Accuracy of a Computer-Aided Dynamic Navigation System in the Placement of Zygomatic Dental Implants: An In Vitro Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
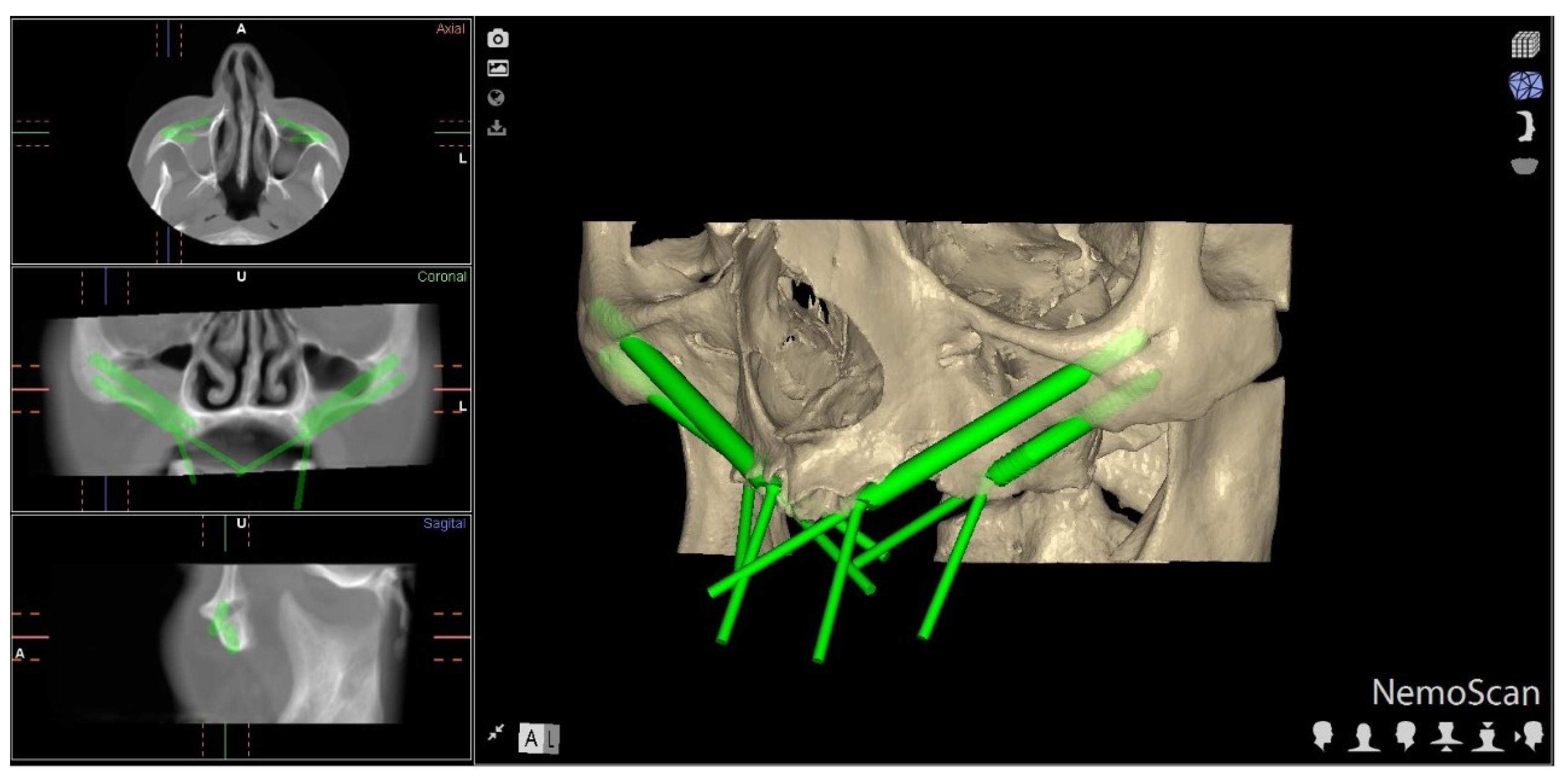
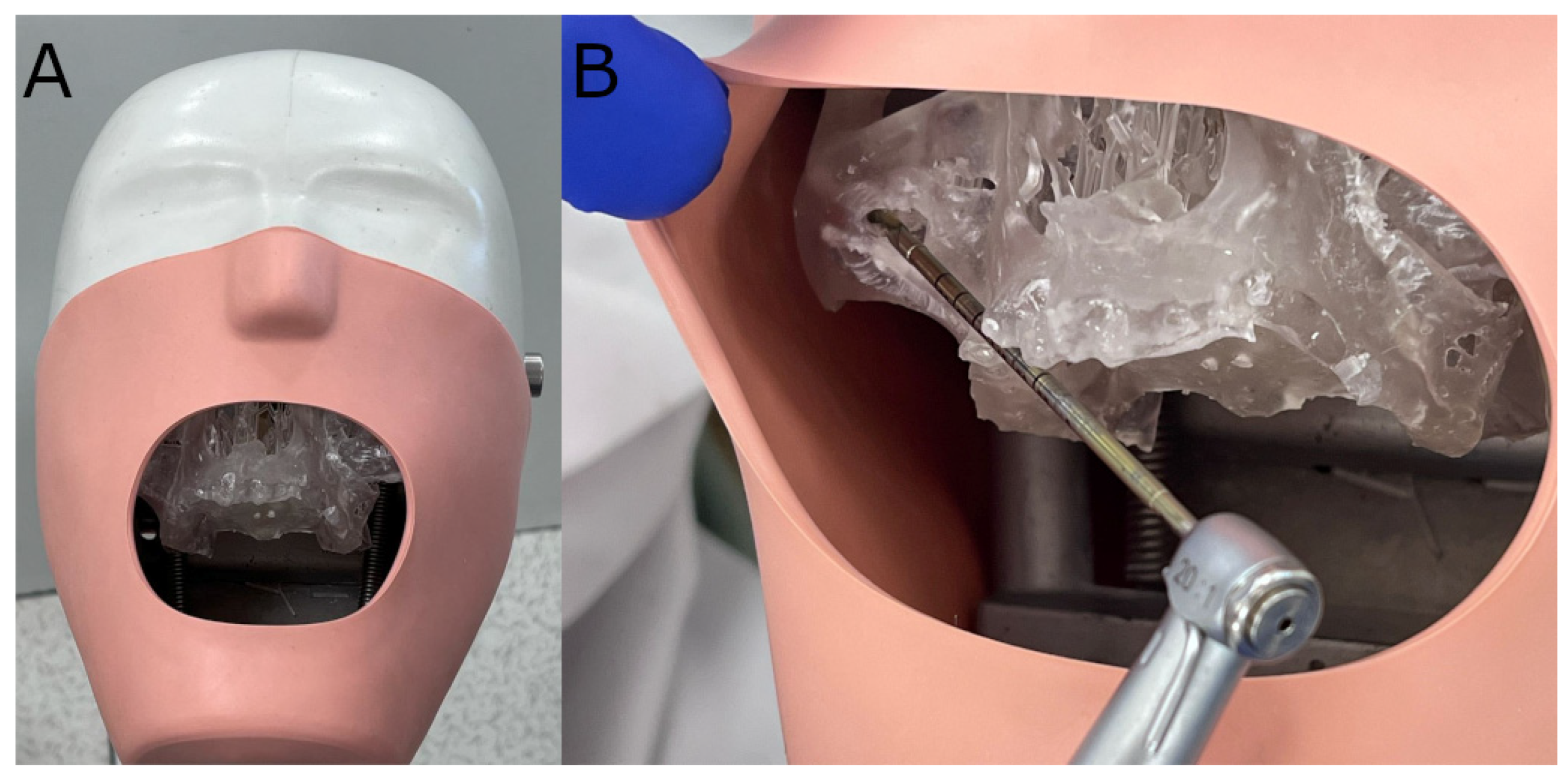
2.2. Experimental Procedure
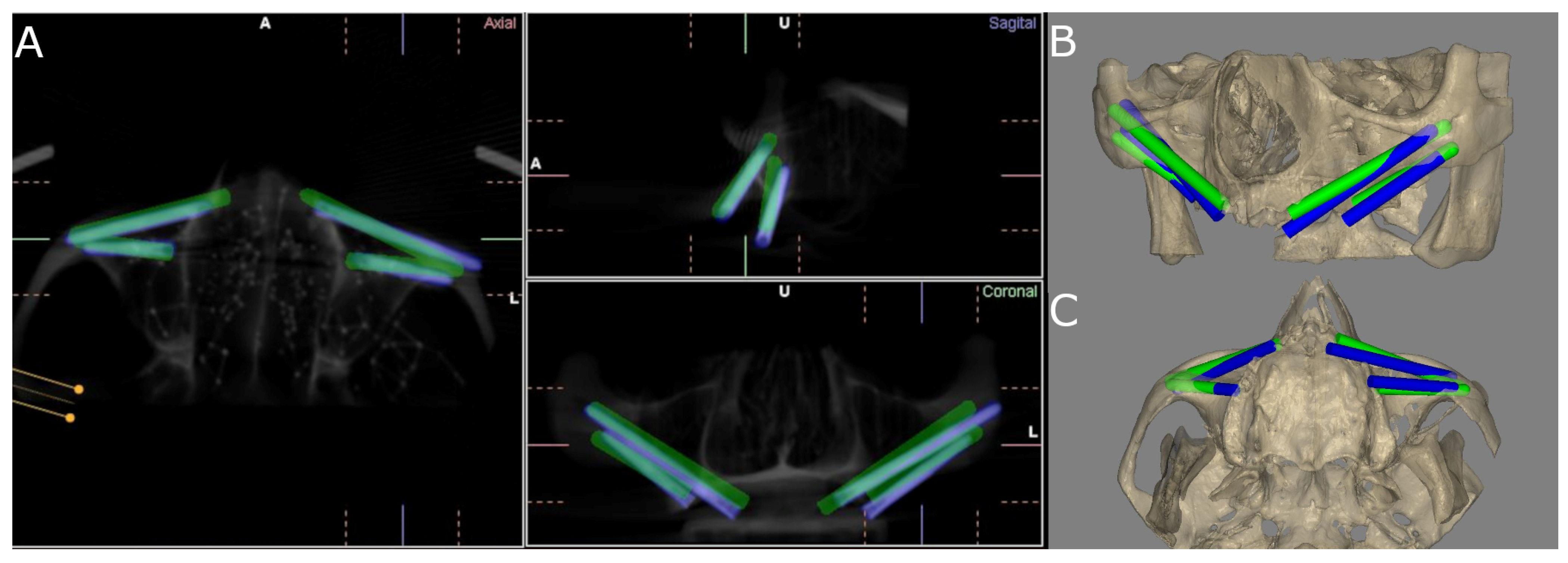
2.3. Measurement Procedure
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bidra, A.S.; Jacob, R.F.; Taylor, T.D. Classification of maxillectomy defects: A systematic review and criteria necessary for a universal description. J. Prosthet. Dent. 2012, 107, 261–270. [Google Scholar] [CrossRef]
- Rosenstein, J.; Dym, H. Zygomatic Implants: A Solution for the Atrophic Maxilla. Dent. Clin. N. Am. 2020, 64, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Davó, R.; Felice, P.; Pistilli, R.; Barausse, C.; Marti-Pages, C.; Ferrer-Fuertes, A.; Ippolito, D.R.; Esposito, M. Immediately loaded zygomatic implants vs. conventional dental implants in augmented atrophic maxillae: 1-year post-loading results from a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 145–161. [Google Scholar] [PubMed]
- Gutiérrez Muñoz, D.; Obrador Aldover, C.; Zubizarreta-Macho, Á.; González Menéndez, H.; Lorrio Castro, J.; Peñarrocha-Oltra, D.; Montiel-Company, J.M.; Hernández Montero, S. Survival Rate and Prosthetic and Sinus Complications of Zygomatic Dental Implants for the Rehabilitation of the Atrophic Edentulous Maxilla: A Systematic Review and Meta-Analysis. Biology 2021, 10, 601. [Google Scholar] [CrossRef] [PubMed]
- Brånemark, P.I.; Gröndahl, K.; Ohrnell, L.O.; Nilsson, P.; Petruson, B.; Svensson, B.; Engstrand, P.; Nannmark, U. Zygoma fixture in the management of advanced atrophy of the maxilla: Technique and long-term results. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2004, 38, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; Nobre Mde, A.; Lopes, I. A new approach to rehabilitate the severely atrophic maxilla using extramaxillary anchored implants in immediate function: A pilot study. J. Prosthet. Dent. 2008, 100, 354–366. [Google Scholar] [CrossRef]
- Omami, G.; Al Yafi, F. Should Cone Beam Computed Tomography Be Routinely Obtained in Implant Planning? Dent. Clin. N. Am. 2019, 63, 363–379. [Google Scholar] [CrossRef]
- Zhou, W.; Fan, S.; Wang, F.; Huang, W.; Jamjoom, F.Z.; Wu, Y. A novel extraoral registration method for a dynamic navigation system guiding zygomatic implant placement in patients with maxillectomy defects. Int. J. Oral Maxillofac. Surg. 2021, 50, 116–120. [Google Scholar] [CrossRef]
- Chana, H.; Smith, G.; Bansal, H.; Zahra, D. A Retrospective Cohort Study of the Survival Rate of 88 Zygomatic Implants Placed Over an 18-year Period. Int. J. Oral Maxillofac. Implants 2019, 34, 461–470. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implants Res. 2018, 16, 416–435. [Google Scholar] [CrossRef] [Green Version]
- Stefanelli, L.V.; DeGroot, B.S.; Lipton, D.I.; Mandelaris, G.A. Accuracy of a Dynamic Dental Implant Navigation System in a Private Practice. Int. J. Oral Maxillofac. Implants 2019, 34, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wang, F.; Huang, W.; Fan, S. Real-Time Navigation in Zygomatic Implant Placement: Workflow. Oral Maxillofac. Surg. Clin. N. Am. 2019, 31, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Mediavilla Guzmán, A.; Riad Deglow, E.; Zubizarreta-Macho, Á.; Agustín-Panadero, R.; Hernández Montero, S. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Navigation for Dental Implant Placement: An In Vitro Study. J. Clin. Med. 2019, 8, 2123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.K.; Yuh, D.Y.; Huang, R.Y.; Fu, E.; Tsai, C.F.; Chiang, C.Y. Accuracy of Implant Placement with a Navigation System, a Laboratory Guide, and Freehand Drilling. Int. J. Oral Maxillofac. Implants 2018, 33, 1213–1218. [Google Scholar] [CrossRef]
- Gargallo-Albiol, J.; Barootchi, S.; Salomó-Coll, O.; Wang, H.L. Advantages and disadvantages of implant navigation surgery. A systematic review. Ann. Anat. 2019, 225, 1–10. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; Pontes, A.E.; Piattelli, A.; Iezzi, G. Primary Stability of Dental Implants in Low-Density (10 and 20 pcf) Polyurethane Foam Blocks: Conical vs. Cylindrical Implants. Int. J. Environ. Res. Public Health 2020, 17, 2617. [Google Scholar] [CrossRef] [Green Version]
- Hung, K.F.; Wang, F.; Wang, H.W.; Zhou, W.J.; Huang, W.; Wu, Y.Q. Accuracy of a real-time surgical navigation system for the placement of quad zygomatic implants in the severe atrophic maxilla: A pilot clinical study. Clin. Implant Dent. Relat. Res. 2017, 19, 458–465. [Google Scholar] [CrossRef]
- Xiaojun, C.; Ming, Y.; Yanping, L.; Yiqun, W.; Chengtao, W. Image guided oral implantology and its application in the placement of zygoma implants. Comput. Methods Programs Biomed. 2009, 93, 162–173. [Google Scholar] [CrossRef]
- Chen, X.; Wu, Y.; Wang, C. Application of a surgical navigation system in the rehabilitation of maxillary defects using zygoma implants: Report of one case. Int. J. Oral Maxillofac. Implants 2011, 26, e29–e34. [Google Scholar]
- Hung, K.; Huang, W.; Wang, F.; Wu, Y. Real-Time Surgical Navigation System for the Placement of Zygomatic Implants with Severe Bone Deficiency. Int. J. Oral Maxillofac. Implants 2016, 31, 1444–1449. [Google Scholar] [CrossRef] [Green Version]
- Jorba-García, A.; Figueiredo, R.; González-Barnadas, A.; Camps-Font, O.; Valmaseda-Castellón, E. Accuracy and the role of experience in dynamic computer guided dental implant surgery: An in-vitro study. Med. Oral Patol. Oral Cir. Bucal. 2019, 24, e76–e83. [Google Scholar] [CrossRef] [PubMed]
- Brief, J.; Edinger, D.; Hassfeld, S.; Eggers, G. Accuracy of image-guided implantology. Clin. Oral Implants Res. 2005, 16, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Aydemir, C.A.; Arısan, V. Accuracy of dental implant placement via dynamic navigation or the freehand method: A split-mouth randomized controlled clinical trial. Clin. Oral Implants Res. 2020, 31, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Schneider, D.; Ganeles, J.; Wismeijer, D.; Zwahlen, M.; Hämmerle, C.H.; Tahmaseb, A. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implants 2009, 24, 92–109. [Google Scholar]
- Gunkel, A.R.; Freysinger, W.; Thumfart, W.F. Experience with various 3-dimensional navigation systems in head and neck surgery. Arch. Otolaryngol. Head Neck Surg. 2000, 126, 390–395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.G.; Lee, W.J.; Lee, S.S.; Heo, M.S.; Huh, K.H.; Choi, S.C.; Kim, T.I.; Yi, W.J. An advanced navigational surgery system for dental implants completed in a single visit: An in vitro study. J. Craniomaxillofac. Surg. 2015, 43, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Tahmaseb, A.; Wismeijer, D.; Coucke, W.; Derksen, W. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 25–42. [Google Scholar] [CrossRef] [Green Version]
- Jorba-García, A.; González-Barnadas, A.; Camps-Font, O.; Figueiredo, R.; Valmaseda-Castellón, E. Accuracy assessment of dynamic computer-aided implant placement: A systematic review and meta-analysis. Clin Oral Investig. 2021, 25, 2479–2494. [Google Scholar] [CrossRef]
- Block, M.S.; Emery, R.W.; Lank, K.; Ryan, J. Implant Placement Accuracy Using Dynamic Navigation. Int. J. Oral Maxillofac. Implants 2017, 32, 92–99. [Google Scholar] [CrossRef]
- Kaewsiri, D.; Panmekiate, S.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. The accuracy of static vs. dynamic computer-assisted implant surgery in single tooth space: A randomized controlled trial. Clin. Oral Implants Res. 2019, 30, 505–514. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Oliveira, D.R.; Custódio, A.L. Accuracy evaluation of computed tomography-derived stereolithographic surgical guides in zygomatic implant placement in human cadavers. J. Oral Implantol. 2010, 36, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Vrielinck, L.; Politis, C.; Schepers, S.; Pauwels, M.; Naert, I. Image-based planning and clinical validation of zygoma and pterygoid implant placement in patients with severe bone atrophy using customized drill guides. Preliminary results from a prospective clinical follow-up study. Int. J. Oral Maxillofac. Surg. 2003, 32, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Ramezanzade, S.; Yates, J.; Tuminelli, F.J.; Keyhan, S.O.; Yousefi, P.; Lopez-Lopez, J. Zygomatic implants placed in atrophic maxilla: An overview of current systematic reviews and meta-analysis. Maxillofac. Plast. Reconstr. Surg. 2021, 43, 1. [Google Scholar] [CrossRef] [PubMed]
- Lan, K.; Wang, F.; Huang, W.; Davó, R.; Wu, Y. Quad Zygomatic Implants: A Systematic Review and Meta-analysis on Survival and Complications. Int. J. Oral Maxillofac. Implants 2021, 36, 21–29. [Google Scholar] [CrossRef] [PubMed]


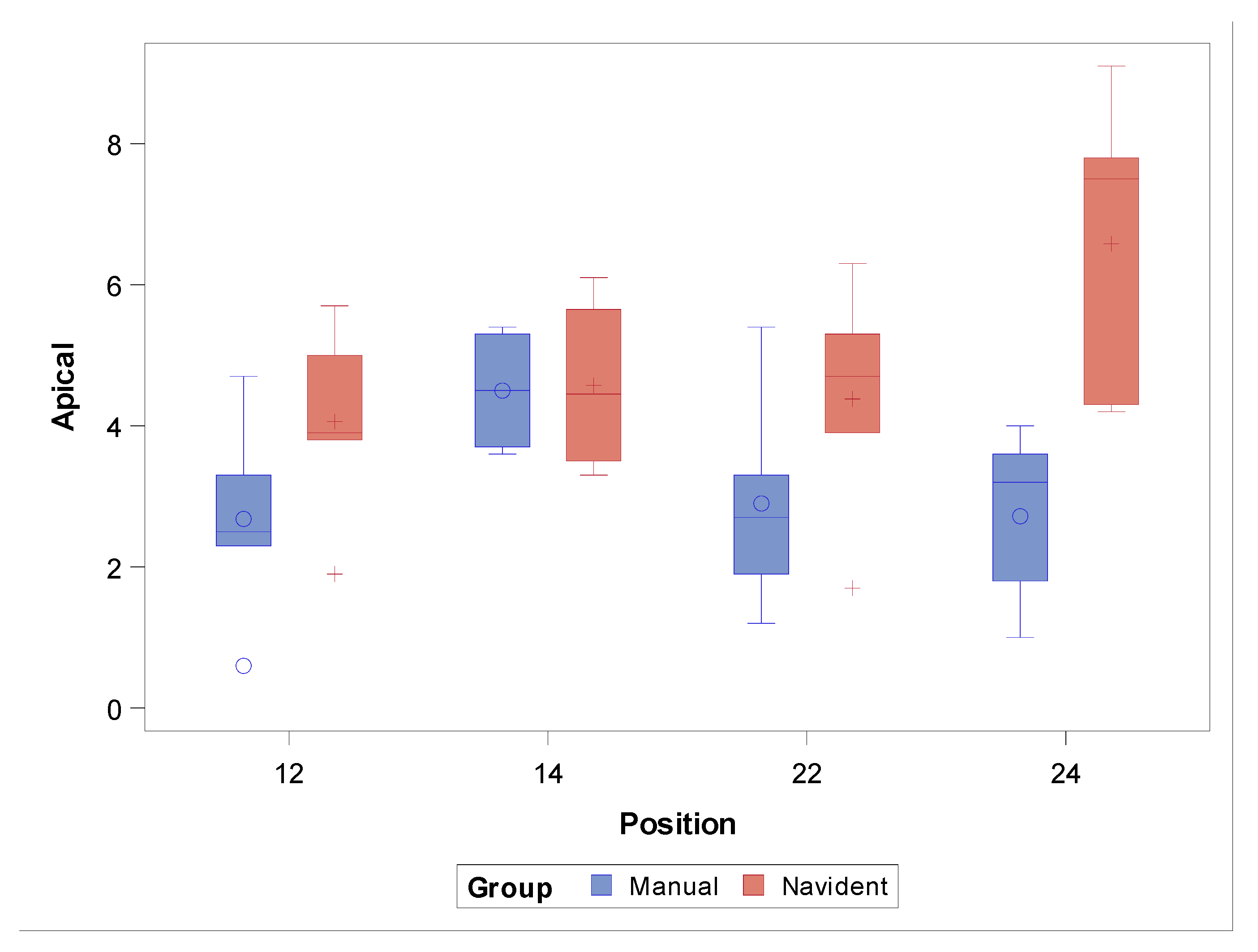
| n | Mean | Median | SD | Lower 95% CL for Mean | Upper 95% CL for Mean | Minimum | Maximum | ||
|---|---|---|---|---|---|---|---|---|---|
| CORONAL | NI | 19 | 5.43 a | 5.70 | 2.13 | 4.41 | 6.46 | 1.60 | 10.50 |
| FHI | 20 | 4.75 a | 4.35 | 1.58 | 4.01 | 5.48 | 2.20 | 7.80 | |
| APICAL | NI | 19 | 4.92 a | 4.70 | 1.89 | 4.00 | 5.83 | 1.70 | 9.10 |
| FHI | 20 | 3.20 b | 3.30 | 1.45 | 2.52 | 3.88 | 0.60 | 5.40 | |
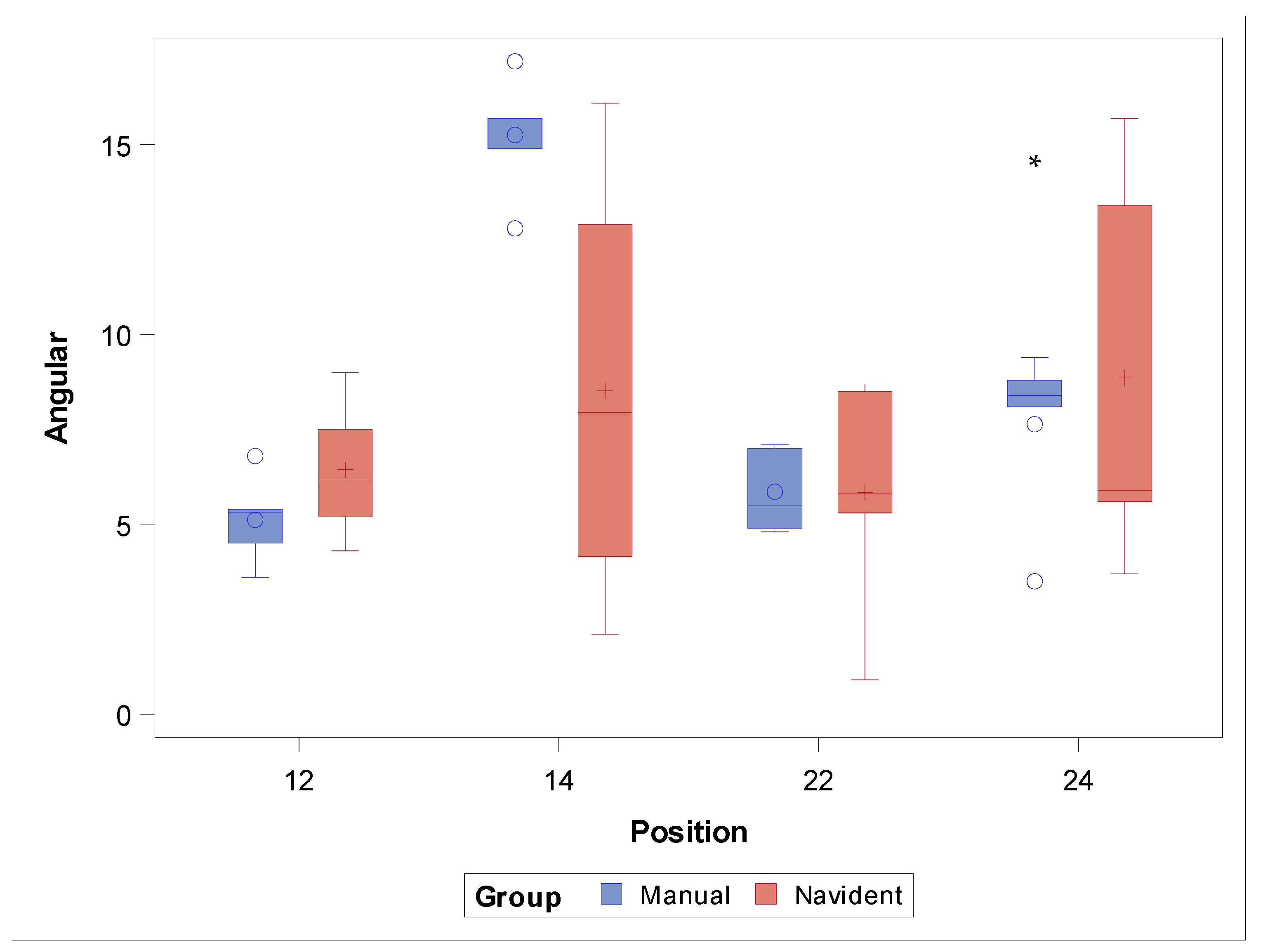
| ANGULAR | NI | 19 | 7.36 a | 6.20 | 4.12 | 5.37 | 9.34 | 0.90 | 16.10 |
| FHI | 20 | 8.47 b | 7.05 | 4.40 | 6.41 | 10.53 | 3.50 | 17.20 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González Rueda, J.R.; García Ávila, I.; de Paz Hermoso, V.M.; Riad Deglow, E.; Zubizarreta-Macho, Á.; Pato Mourelo, J.; Montero Martín, J.; Hernández Montero, S. Accuracy of a Computer-Aided Dynamic Navigation System in the Placement of Zygomatic Dental Implants: An In Vitro Study. J. Clin. Med. 2022, 11, 1436. https://doi.org/10.3390/jcm11051436
González Rueda JR, García Ávila I, de Paz Hermoso VM, Riad Deglow E, Zubizarreta-Macho Á, Pato Mourelo J, Montero Martín J, Hernández Montero S. Accuracy of a Computer-Aided Dynamic Navigation System in the Placement of Zygomatic Dental Implants: An In Vitro Study. Journal of Clinical Medicine. 2022; 11(5):1436. https://doi.org/10.3390/jcm11051436
Chicago/Turabian StyleGonzález Rueda, Juan Ramón, Irene García Ávila, Víctor Manuel de Paz Hermoso, Elena Riad Deglow, Álvaro Zubizarreta-Macho, Jesús Pato Mourelo, Javier Montero Martín, and Sofía Hernández Montero. 2022. "Accuracy of a Computer-Aided Dynamic Navigation System in the Placement of Zygomatic Dental Implants: An In Vitro Study" Journal of Clinical Medicine 11, no. 5: 1436. https://doi.org/10.3390/jcm11051436
APA StyleGonzález Rueda, J. R., García Ávila, I., de Paz Hermoso, V. M., Riad Deglow, E., Zubizarreta-Macho, Á., Pato Mourelo, J., Montero Martín, J., & Hernández Montero, S. (2022). Accuracy of a Computer-Aided Dynamic Navigation System in the Placement of Zygomatic Dental Implants: An In Vitro Study. Journal of Clinical Medicine, 11(5), 1436. https://doi.org/10.3390/jcm11051436








