Different Kinetics of HBV-DNA and HBsAg in HCV Coinfected Patients during DAAs Therapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Treatment Regimen
2.3. Assays
2.4. Statistics
3. Results
3.1. Clinical and Virological Features
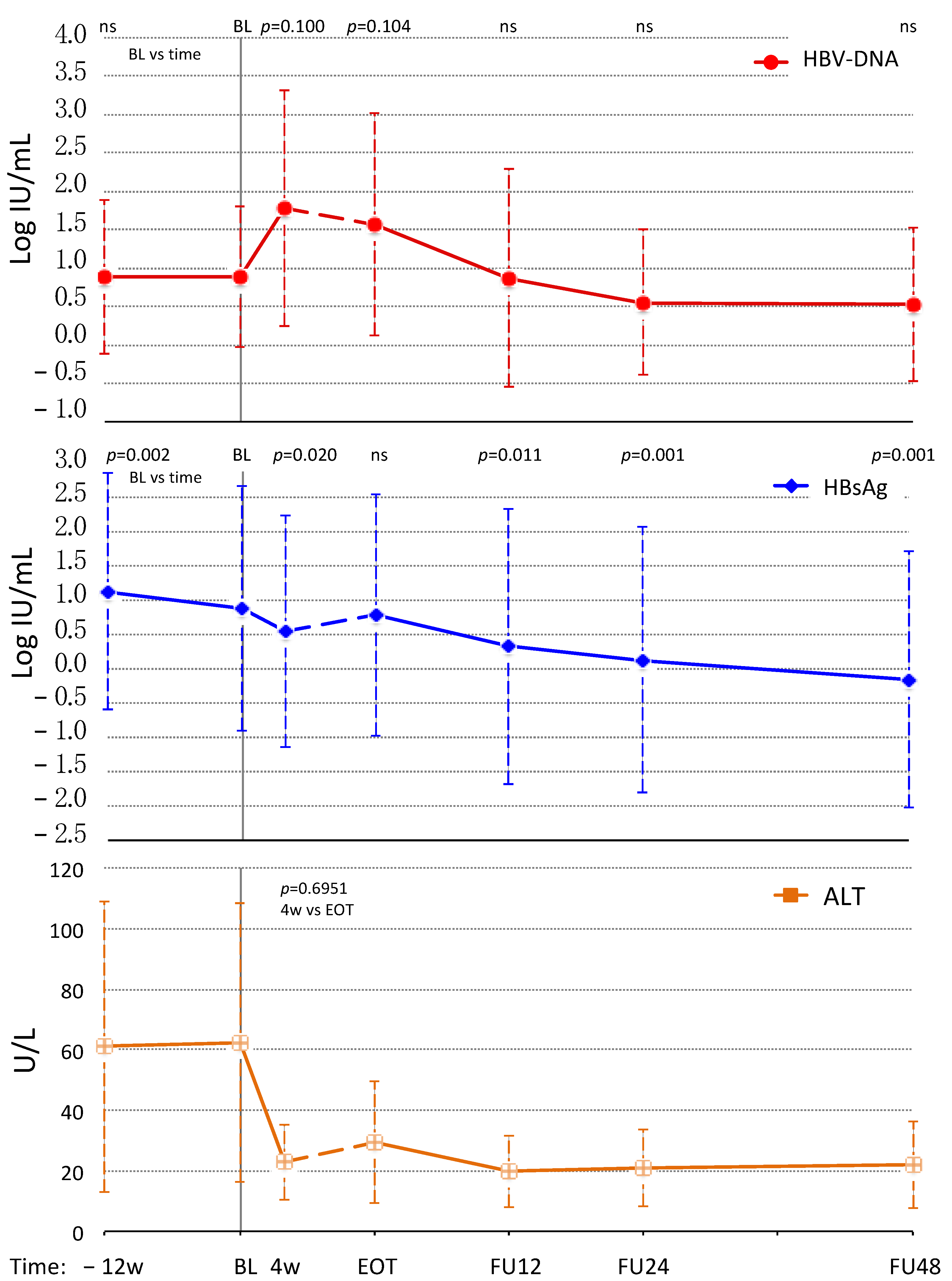
3.2. HBV-DNA and HBsAg Kinetics
3.2.1. HBeAg Negative Infection
3.2.2. HBeAg Negative Chronic Hepatitis B
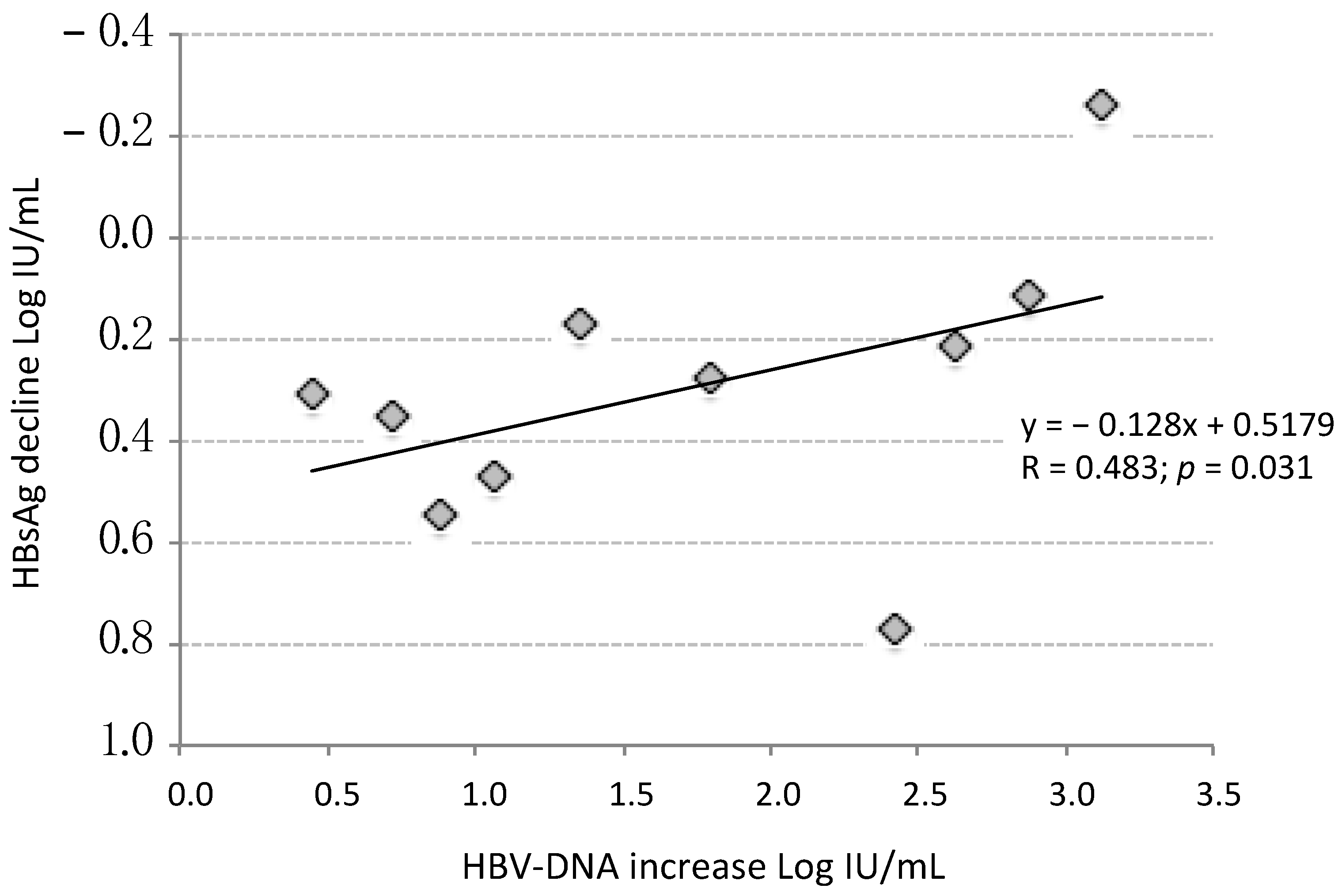
3.2.3. Factors Influencing HBsAg Decline during DAAs
3.2.4. Interferon Gamma Inducible Protein 10 during DAAs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Progress Report on HIV, Viral Hepatitis and Sexually Transmitted Infections. 2021. Available online: https://www.who.int/publications/i/item/9789240027077 (accessed on 28 February 2022).
- Bellecave, P.; Gouttenoire, J.; Gajer, M.; Brass, V.; Koutsoudakis, G.; Blum, H.E.; Bartenschlager, R.; Nassal, M.; Moradpour, D. Hepatitis B and C virus coinfection: A novel model system reveals the absence of direct viral interference. Hepatology 2009, 50, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Shih, Y.-F.; Liu, C.-J. Hepatitis C Virus and Hepatitis B Virus Co-Infection. Viruses 2020, 12, 741. [Google Scholar] [CrossRef] [PubMed]
- Wiegand, S.; Jaroszewicz, J.; Potthoff, A.; zu Siederdissen, C.H.; Maasoumy, B.; Deterding, K.; Manns, M.; Wedemeyer, H.; Cornberg, M. Dominance of hepatitis C virus (HCV) is associated with lower quantitative hepatitis B surface antigen and higher serum interferon-γ-induced protein 10 levels in HBV/HCV-coinfected patients. Clin. Microbiol. Infect. 2015, 21, 710.e1–710.e9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, K.; Lai, X.; Song, J.; He, L.; Wang, L.; Ou, G.; Tian, X.; Wang, L.; Deng, J.; Zhang, J.; et al. A novel cell culture model reveals the viral interference during hepatitis B and C virus coinfection. Antivir. Res. 2021, 189, 105061. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Uchida, T.; Xia, Y.; Umarova, R.; Liu, C.-J.; Chen, P.-J.; Gaggar, A.; Suri, V.; Mücke, M.M.; Vermehren, J.; et al. Diminished hepatic IFN response following HCV clearance triggers HBV reactivation in coinfection. J. Clin. Investig. 2020, 130, 3205–3220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tseng, C.W.; Wu, S.F.; Chen, C.Y.; Ho, Y.C.; He, Y.T.; Tseng, K.C. Characteristics of regulatory T-cell function in patients with chronic hepatitis B and C coinfection. J. Viral Hepat. 2020, 27, 800–809. [Google Scholar] [CrossRef] [Green Version]
- Murai, K.; Hikita, H.; Kai, Y.; Kondo, Y.; Fukuoka, M.; Fukutomi, K.; Doi, A.; Yamai, T.; Nakabori, T.; Fukuda, R.; et al. Hepatitis C virus infection suppresses hepatitis B virus replication via the RIG-I-like helicase pathway. Sci. Rep. 2020, 10, 941. [Google Scholar] [CrossRef]
- Heim, M.H.; Thimme, R. Innate and adaptive immune responses in HCV infections. J. Hepatol. 2014, 61, S14–S25. [Google Scholar] [CrossRef] [Green Version]
- Belperio, P.S.; Shahoumian, T.A.; Mole, L.A.; Backus, L.I. Evaluation of hepatitis B reactivation among 62,920 veterans treated with oral hepatitis C antivirals. Hepatology 2017, 66, 27–36. [Google Scholar] [CrossRef] [Green Version]
- Calvaruso, V.; Ferraro, D.; Licata, A.; Bavetta, M.G.; Petta, S.; Bronte, F.; Colomba, G.M.E.; Craxì, A.; Di Marco, V. HBV reactivation in patients with HCV/HBV cirrhosis on treatment with direct-acting antivirals. J. Viral Hepat. 2018, 25, 72–79. [Google Scholar] [CrossRef]
- Serper, M.; Forde, K.A.; Kaplan, D.E. Rare clinically significant hepatic events and hepatitis B reactivation occur more frequently following rather than during direct-acting antiviral therapy for chronic hepatitis C: Data from a national US cohort. J. Viral Hepat. 2018, 25, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Mücke, M.M.; I Backus, L.; Mücke, V.T.; Coppola, N.; Preda, C.M.; Yeh, M.-L.; Tang, L.S.Y.; Belperio, P.S.; Wilson, E.; Yu, M.-L.; et al. Hepatitis B virus reactivation during direct-acting antiviral therapy for hepatitis C: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2018, 3, 172–180. [Google Scholar] [CrossRef]
- Bersoff-Matcha, S.J.; Cao, K.; Jason, M.; Ajao, A.; Jones, S.C.; Meyer, T.; Brinker, A. Hepatitis B Virus Reactivation Associated with Direct-Acting Antiviral Therapy for Chronic Hepatitis C Virus: A Review of Cases Reported to the U.S. Food and Drug Administration Adverse Event Reporting System. Ann. Intern. Med. 2017, 166, 792. [Google Scholar] [CrossRef] [PubMed]
- Sastre, L.; Ruiz, P.; Costa, J.; Forns, X. Severe hepatitis B reactivation during direct-acting antiviral treatment in “the absence” of hepatitis B surface antigen. Int. J. Infect. Dis. 2019, 79, 47–49. [Google Scholar] [CrossRef] [Green Version]
- Yeh, M.-L.; Huang, C.-I.; Huang, C.-F.; Hsieh, M.-H.; Liu, T.-W.; Lin, Y.-H.; Liang, P.-C.; Hsieh, M.-Y.; Lin, Z.-Y.; Chen, S.-C.; et al. Pretreatment Hepatitis B Viral Load Predicts Long-Term Hepatitis B Response After Anti-Hepatitis C Therapy in Hepatitis B/C Dual-Infected Patients. J. Infect. Dis. 2019, 219, 1224–1233. [Google Scholar] [CrossRef]
- Yeh, M.-L.; Huang, C.-F.; Huang, C.-I.; Holmes, J.A.; Hsieh, M.-H.; Tsai, Y.-S.; Liang, P.-C.; Tsai, P.-C.; Hsieh, M.-Y.; Lin, Z.-Y.; et al. Hepatitis B-related outcomes following direct-acting antiviral therapy in Taiwanese patients with chronic HBV/HCV co-infection. J. Hepatol. 2020, 73, 62–71. [Google Scholar] [CrossRef] [Green Version]
- Pawlotsky, J.M.; Negro, F.; Aghemo, A.; Berenguer, M.; Dalgard, O.; Dusheiko, G.; Marra, F.; Puoti, M.; Wedemeyer, H.; European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: Final update of the series. J. Hepatol. 2020, 73, 1170–1218. [Google Scholar] [CrossRef]
- AASLD-IDSA Hepatitis C Guidance Panel. Hepatitis C Guidance 2019 Update: American Association for the Study of Liver Diseases–Infectious Diseases Society of America Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection AASLD-IDSA Hepatitis C Guidance Panel. Hepatology 2019, 71, 686–721. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, A. Drafting Committee for Hepatitis Management Guidelines, the Japan Society of Hepatology Japan Society of Hepatology guidelines for the management of hepatitis C virus infection: 2019 update. Hepatol. Res. 2020, 50, 791–816. [Google Scholar] [CrossRef]
- Roy, A.; De, A.; Singh, V. DAAs and HBV/HCV coinfection: Glimmer of light and a few shades of grey. J. Hepatol. 2020, 73, 461. [Google Scholar] [CrossRef]
- Balagopal, A.; Thio, C.L. When viruses collide: Hepatitis B virus reactivation after hepatitis C treatment. J. Clin. Investig. 2020, 130, 2823–2826. [Google Scholar] [CrossRef]
- Carlin, A.F.; Aristizabal, P.; Song, Q.; Wang, H.; Paulson, M.S.; Stamm, L.M.; Schooley, R.T.; Wyles, D.L. Temporal dynamics of inflammatory cytokines/chemokines during sofosbuvir and ribavirin therapy for genotype 2 and 3 hepatitis C infection. Hepatology 2015, 62, 1047–1058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oliveri, F.; Surace, L.; Cavallone, D.; Colombatto, P.; Ricco, G.; Salvati, N.; Coco, B.; Romagnoli, V.; Gattai, R.; Salvati, A.; et al. Long-term outcome of inactive and active, low viraemic HBe, Ag-negative-hepatitis B virus infection: Benign course towards HBs, Ag clearance. Liver Int. 2017, 37, 1622–1631. [Google Scholar] [CrossRef] [PubMed]
- Zhou, K.; Wahed, A.S.; Cooper, S.; Di Bisceglie, A.M.; Fontana, R.J.; Ghany, M.G.; Khalili, M.; Lok, A.S.; Perrillo, R.; Lee, W.M.; et al. Phase Transition Is Infrequent Among North American Adults With e-Antigen-Negative Chronic Hepatitis B and Low-Level Viremia. Am. J. Gastroenterol. 2019, 114, 1753–1763. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-J.; Yang, H.-I.; Su, J.; Jen, C.-L.; You, S.-L.; Lu, S.-N.; Huang, G.-T.; Iloeje, U.H.; REVEAL-HBV Study Group. Risk of Hepatocellular Carcinoma across a Biological Gradient of Serum Hepatitis B Virus DNA Level. JAMA 2006, 295, 65–73. [Google Scholar] [CrossRef] [Green Version]
- Tsay, P.K.; Tai, D.I.; Chen, Y.M.; Yu, C.P.; Wan, S.Y.; Shen, Y.J.; Lin, D.Y. Impact of gender, viral transmission and aging in the preva-lence of hepatitis B surface antigen. Chang Gung Med. J. 2009, 32, 155–164. [Google Scholar]
- Liaw, Y.-F.; Brunetto, M.R.; Hadziyannis, S. The natural history of chronic HBV infection and geographical differences. Antivir. Ther. 2010, 15 (Suppl. S3), 25–33. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.-H.; Chen, P.-J.; Yeh, S.-H. Gender disparity in chronic hepatitis B: Mechanisms of sex hormones. J. Gastroenterol. Hepatol. 2015, 30, 1237–1245. [Google Scholar] [CrossRef] [Green Version]
- Sato, S.; Tsuzura, H.; Kita, Y.; Ikeda, Y.; Kabemura, D.; Sato, S.; Amano, N.; Yatagai, N.; Murata, A.; Shimada, Y.; et al. Hepatitis B Surface Antigen Decline during Sofosbuvir and Ribavirin Therapy in Hepatitis B Inactive Carriers Who Were Co-infected with Hepatitis C. Intern. Med. 2021, 60, 3569–3572. [Google Scholar] [CrossRef]
- Ledipasvir/Sofosbuvir for Hepatitis B Virus Infection (APOSTLE). Available online: https://clinicaltrials.gov/ct2/show/NCT03312023 (accessed on 22 January 2022).
- Urbani, S.; Boni, C.; Amadei, B.; Fisicaro, P.; Cerioni, S.; Valli, M.A.; Missale, G.; Ferrari, C. Acute phase HBV-specific T cell responses associated with HBV persistence after HBV/HCV coinfection. Hepatology 2005, 41, 826–831. [Google Scholar] [CrossRef]
- Martin, B.; Hennecke, N.; Lohmann, V.; Kayser, A.; Neumann-Haefelin, C.; Kukolj, G.; Böcher, W.-O.; Thimme, R. Restoration of HCV-specific CD8+ T cell function by interferon-free therapy. J. Hepatol. 2014, 61, 538–543. [Google Scholar] [CrossRef] [PubMed]
- Ahlenstiel, G.; Titerence, R.H.; Koh, C.; Edlich, B.; Feld, J.J.; Rotman, Y.; Ghany, M.G.; Hoofnagle, J.H.; Liang, T.J.; Heller, T.; et al. Natural Killer Cells Are Polarized Toward Cytotoxicity in Chronic Hepatitis C in an Interferon-Alfa–Dependent Manner. Gastroenterology 2010, 138, 325–335.e2. [Google Scholar] [CrossRef] [Green Version]
- Serti, E.; Chepa-Lotrea, X.; Kim, Y.J.; Keane, M.; Fryzek, N.; Liang, T.J.; Ghany, M.; Rehermann, B. Successful Interferon-Free Therapy of Chronic Hepatitis C Virus Infection Normalizes Natural Killer Cell Function. Gastroenterology 2015, 149, 190–200.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cornberg, M.; Pischke, S.; Müller, T.; Behrendt, P.; Piecha, F.; Benckert, J.; Todt, D.; Steinmann, E.; Papkalla, A.; von Karpowitz, M.; et al. Sofosbuvir monotherapy fails to achieve HEV RNA elimination in patients with chronic hepatitis E—The Hep, Net Sof, E pilot study. J. Hepatol. 2020, 73, 696–699. [Google Scholar] [CrossRef] [PubMed]
- Sofia, M.J.; Link, J.O. Harvoni: A Combination Therapy for Curing HCV. In Comprehensive Medicinal Chemistry III; Chackalamannil, S., Rotella, D., Ward, S.E., Eds.; Elsevier: Amsterdam, The Netherlands, 2017; Volume 8, pp. 558–582. ISBN 9780128032015. [Google Scholar] [CrossRef]
- Feng, J.Y.; Xu, Y.; Barauskas, O.; Perry, J.K.; Ahmadyar, S.; Stepan, G.; Yu, H.; Babusis, D.; Park, Y.; Mc Cutcheon, K.; et al. Role of Mitochondrial RNA Polymerase in the Toxicity of Nucleotide Inhibitors of Hepatitis C Virus. Antimicrob. Agents Chemother. 2016, 60, 806–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Parameter | Units | Overall | ENI | CHB (NAs) | p Value |
|---|---|---|---|---|---|
| Subjects | Number | 23 | 15 | 8 | |
| Gender | Males | 17 (73.9%) | 11 (73.3%) | 6 (75%) | 1.00 |
| Age | years | 57.1 (36.1–81.7) | 62.1 (41.0–81.7) | 54.8 (36.1–65.9) | 0.093 |
| LS | kPa | 10.5 (5.3–38.5) | 10.5 (5.3–38.5) | 15.7 (6.6–35.0) | 0.495 |
| ALT | U/L | 45 (9–161) | 51 (9–161) | 44 (16–96) | 0.495 |
| HCV-RNA | Log IU/mL | 6.2 (3.7–7.7) | 6.2 (3.7-7.7) | 6.0 (4.9–6.7) | 0.561 |
| Genotype | 1a | 4 (17.4%) | 2 (13.3%) | 2 (25.0%) | nd |
| 1b | 7 (30.4%) | 5 (33.3%) | 2 (25.0%) | nd | |
| 2 | 3 (13.0%) | 3 (20.0%) | 0 | nd | |
| 3 | 7 (30.4%) | 5 (33.3%) | 2 (25.0%) | nd | |
| 4 | 2 (8.7%) | 0 | 2 (25.0%) | nd | |
| HBsAg | IU/mL | 34.37 (0.10–17,915.0) | 6.61 (0.10–17,915.0) | 213.19 (16.88–4165.7) | 0.028 |
| HBV-DNA | Detected * | 7 (30.4%) | 7 (46.7%) | 0 | nd |
| HBV-DNA | IU/mL ** | 31 (10–599) | 31 (10–599) | n.a. | nd |
| Genotype | B | 1 (4.3%) | 0 | 1 (12.5%) | nd |
| D | 8 (34.8%) | 4 (26.7%) | 4 (50.0%) | nd | |
| n.a. | 14 (60.9%) | 11 (73.3%) | 3 (37.5%) | nd |
| Category | Log HBsAg Maximum Decline Median (Range) | Mann–Whitney U Test p Value | Log HBsAg >0.4 Decline Number (%) | Chi Square p Value | |
|---|---|---|---|---|---|
| Patients | Overall | 0.30 (−0.26–0.91) | 7/22 (31.8) | ||
| Gender | Males | 0.27 (−0.26–0.91) | 0.042 | 3/16 (18.7) | 0.032 |
| Females | 0.48 (0.27–0.60) | 4/6 (66.7) | |||
| HBV phase | ENI | 0.29 (−0.26–0.77) | 0.610 | 5/14 (66.7) | 0.604 |
| CHB | 0.32 (0.13–0.91) | 2/8 (35.7) | |||
| Fibrosis | F0–F2 | 0.21 (−0.26–0.42) | 0.105 | 1/7 (14.3) | 0.228 |
| F3–F4 | 0.35 (−0.11–0.91) | 6/15 (20.0) | |||
| DAAs | SOF | 0.36 (0.08–0.91) | 0.045 | 6/13 (46.2%) | 0.083 |
| NO SOF | 0.22 (−0.26–0.55) | 1/9 (11.1%) |
| Parameter | BL | Week 4 | EOT | EOF | |
|---|---|---|---|---|---|
| HBsAg | Log IU/mL | 2.09 ± 1.56 | 1.82 ± 1.54 | 1.76 ± 1.70 | 1.84 ± 1.68 |
| BL vs time | p value | <0.001 | 0.002 | 0.062 | |
| IP-10 | Log pg/mL | 2.35 ± 0.30 | 1.66 ± 0.57 | 1.75 ± 0.49 | 1.69 ± 0.55 |
| BL vs time | p value | <0.001 | <0.001 | 0.003 | |
| IP-10 ENI | Log pg/mL | 2.46 ± 0.34 | 1.84 ± 0.51 | 1.82 ± 0.56 | 1.76 ± 0.55 |
| IP-10 CHB | Log pg/mL | 2.22 ± 0.22 | 1.45 ± 0.61 | 1.68 ± 0.45 | 1.63 ± 0.61 |
| ENI vs CHB | p value | 0.221 | 0.284 | 0.159 | 0.729 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colombatto, P.; Palmisano, E.; Ricco, G.; Cavallone, D.; Oliveri, F.; Coco, B.; Salvati, A.; Romagnoli, V.; Surace, L.; Vatteroni, M.; et al. Different Kinetics of HBV-DNA and HBsAg in HCV Coinfected Patients during DAAs Therapy. J. Clin. Med. 2022, 11, 1406. https://doi.org/10.3390/jcm11051406
Colombatto P, Palmisano E, Ricco G, Cavallone D, Oliveri F, Coco B, Salvati A, Romagnoli V, Surace L, Vatteroni M, et al. Different Kinetics of HBV-DNA and HBsAg in HCV Coinfected Patients during DAAs Therapy. Journal of Clinical Medicine. 2022; 11(5):1406. https://doi.org/10.3390/jcm11051406
Chicago/Turabian StyleColombatto, Piero, Elena Palmisano, Gabriele Ricco, Daniela Cavallone, Filippo Oliveri, Barbara Coco, Antonio Salvati, Veronica Romagnoli, Lidia Surace, Marialinda Vatteroni, and et al. 2022. "Different Kinetics of HBV-DNA and HBsAg in HCV Coinfected Patients during DAAs Therapy" Journal of Clinical Medicine 11, no. 5: 1406. https://doi.org/10.3390/jcm11051406
APA StyleColombatto, P., Palmisano, E., Ricco, G., Cavallone, D., Oliveri, F., Coco, B., Salvati, A., Romagnoli, V., Surace, L., Vatteroni, M., Pistello, M., Virdis, A., Bonino, F., & Brunetto, M. R. (2022). Different Kinetics of HBV-DNA and HBsAg in HCV Coinfected Patients during DAAs Therapy. Journal of Clinical Medicine, 11(5), 1406. https://doi.org/10.3390/jcm11051406









