Mobile Telemedicine Screening for Diabetic Retinopathy Using Nonmydriatic Fundus Photographs in Burgundy: 11 Years of Results
Abstract
:1. Introduction
2. Materials and Methods
2.1. Recruitment and Procedure
2.2. Statistical Analysis
3. Results
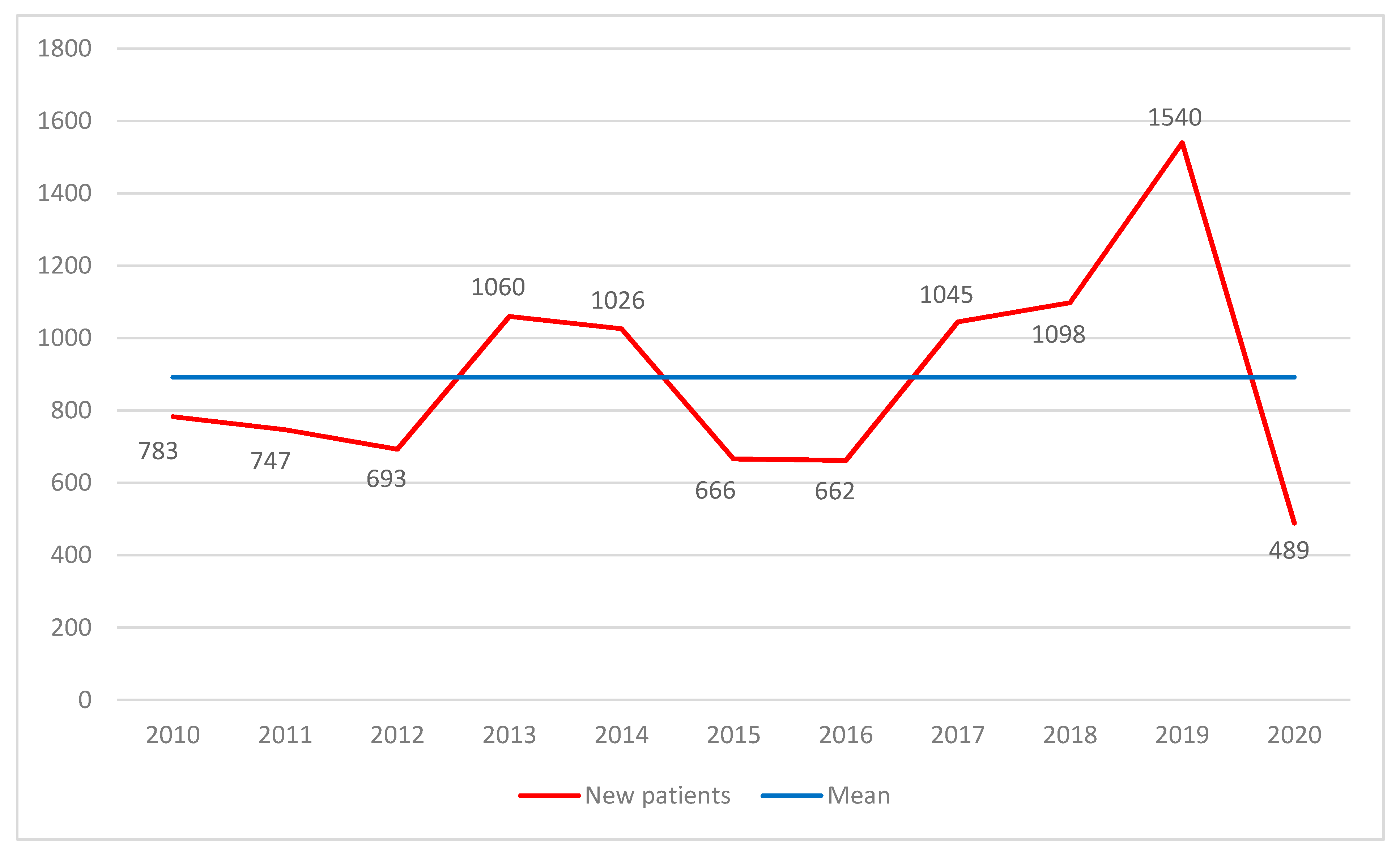
3.1. Description of the Study Population
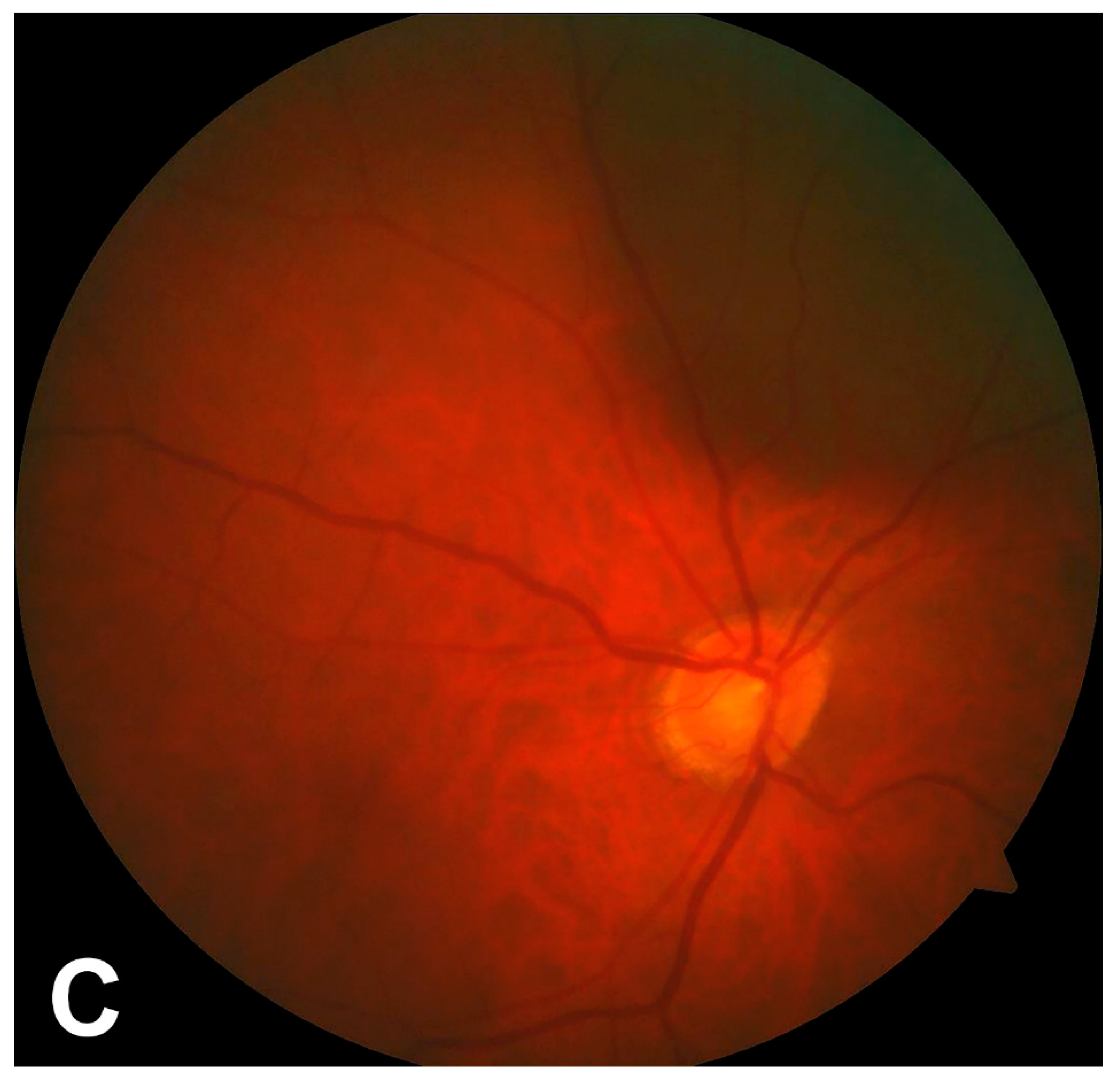
3.2. Screening Results
3.3. Comparison of Patients with and without DR of Any Type
3.4. Differences between Rural and Periurban Areas
3.5. Differences before and after the First Lockdown in France Related to the COVID-19 Pandemic
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Franc, C. Epidemiology of diabetes: Frightening predictions. Med. Sci. 2013, 29, 711–714. [Google Scholar]
- Aiello, L.P.; Avery, R.L.; Arrigg, P.G.; Keyt, B.A.; Jampel, H.D.; Shah, S.T.; Pasquale, L.R.; Thieme, H.; Iwamoto, M.A.; Park, J.E.; et al. Vascular Endothelial Growth Factor in Ocular Fluid of Patients with Diabetic Retinopathy and Other Retinal Disorders. N. Engl. J. Med. 1994, 331, 1480–1487. [Google Scholar] [CrossRef] [PubMed]
- Forbes, J.M.; Cooper, M.E. Mechanisms of Diabetic Complications. Physiol. Rev. 2013, 93, 137–188. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Lo, A.C.Y. Diabetic Retinopathy: Pathophysiology and Treatments. Int. J. Mol. Sci. 2018, 19, 1816. [Google Scholar] [CrossRef] [Green Version]
- Simó-Servat, O.; Hernández, C.; Simó, R. Diabetic Retinopathy in the Context of Patients with Diabetes. Ophthalmic Res. 2019, 62, 211–217. [Google Scholar] [CrossRef]
- Klein, B.E.K. Overview of Epidemiologic Studies of Diabetic Retinopathy. Ophthalmic Epidemiol. 2007, 14, 179–183. [Google Scholar] [CrossRef]
- Yau, J.W.Y.; Rogers, S.L.; Kawasaki, R.; Lamoureux, E.L.; Kowalski, J.W.; Bek, T.; Chen, S.-J.; Dekker, J.M.; Fletcher, A.; Grauslund, J.; et al. Global Prevalence and Major Risk Factors of Diabetic Retinopathy. Diabetes Care 2012, 35, 556–564. [Google Scholar] [CrossRef] [Green Version]
- Vujosevic, S.; Midena, E. Diabetic Retinopathy in Italy: Epidemiology Data and Telemedicine Screening Programs. J. Diabetes Res. 2016, 2016, 3627465. [Google Scholar] [CrossRef]
- Vujosevic, S.; Aldington, S.; Silva, P.; Hernández, C.; Scanlon, P.; Peto, T.; Simó, R. Screening for diabetic retinopathy: New perspectives and challenges. Lancet Diabetes Endocrinol. 2020, 8, 337–347. [Google Scholar] [CrossRef]
- Rosenfeld, P.J.; Brown, D.M.; Heier, J.S.; Boyer, D.S.; Kaiser, P.K.; Chung, C.Y.; Kim, R.Y.; for the MARINA Study Group. Ranibizumab for neovascular age-related macular degeneration. N. Engl. J. Med. 2006, 355, 1419–1431. [Google Scholar] [CrossRef] [Green Version]
- Massin, P.; Aubert, J.-P.; Erginay, A.; Bourovitch, J.; BenMehidi, A.; Audran, G.; Bernit, B.; Jamet, M.; Collet, C.; Laloi-Michelin, M.; et al. Screening for diabetic retinopathy: The first telemedical approach in a primary care setting in France. Diabetes Metab. 2004, 30, 451–457. [Google Scholar] [CrossRef]
- Massin, P.; Aubert, J.; Eschwege, E.; Erginay, A.; Bourovitch, J.; BenMehidi, A.; Nougarède, M.; Bouée, S.; Fagnani, F.; Tcherny, M.; et al. Evaluation of a screening program for diabetic retinopathy in a primary care setting Dodia (Dépistage ophtalmologique du diabète) study. Diabetes Metab. 2005, 31, 153–162. [Google Scholar] [CrossRef]
- Lenoble, P.; Kheliouen, M.; Bourderont, D.; Klinger, V.; Nasica, X.; Benseddik, Y.; Holl, P. Dépistage de la rétinopathie diabétique par télédiagnostic dans le Haut-Rhin. J. Fr. Ophtalmol. 2009, 32, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.M.; Kaiser, P.; Michels, M.; Soubrane, G.; Heier, J.S.; Kim, R.Y.; Sy, J.P.; Schneider, S.; for the ANCHOR Study Group. Ranibizumab versus Verteporfin for Neovascular Age-Related Macular Degeneration. N. Engl. J. Med. 2006, 355, 1432–1444. [Google Scholar] [CrossRef] [Green Version]
- Massin, P.; Chabouis, A.; Erginay, A.; Viens-Bitker, C.; Lecleire-Collet, A.; Meas, T.; Guillausseau, P.-J.; Choupot, G.; André, B.; Denormandie, P. OPHDIAT©: A telemedical network screening system for diabetic retinopathy in the Île-de-France. Diabetes Metab. 2008, 34, 227–234. [Google Scholar] [CrossRef]
- Massin, P.; Angioi-Duprez, K.; Bacin, F.; Cathelineau, B.; Cathelineau, G.; Chaine, G.; Coscas, G.; Flament, J.; Sahel, J.-A.; Turut, P.; et al. Recommendations of the ALFEDIAM (French Association for the Study of Diabetes and Metabolic Diseases) for the screening and surveillance of diabetic retinopathy. J. Fr. Ophtalmol. 1997, 20, 302–310. [Google Scholar]
- Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs—An extension of the modified Airlie House classification. ETDRS report number 10. In Ophthalmology; 1991; 98, (Suppl. S5), pp. 786–806. [Google Scholar] [CrossRef]
- Aiello, L.P.; Odia, I.; Glassman, A.R.; Melia, M.; Jampol, L.M.; Bressler, N.M.; Kiss, S.; Silva, P.S.; Wykoff, C.C.; Sun, J.K.; et al. Comparison of Early Treatment Diabetic Retinopathy Study Standard 7-Field Imaging with Ultrawide-Field Imaging for Determining Severity of Diabetic Retinopathy. JAMA Ophthalmol. 2019, 137, 65–73. [Google Scholar] [CrossRef] [Green Version]
- Wat, N.; Wong, R.L.; Wong, I.Y. Associations between diabetic retinopathy and systemic risk factors. Hong Kong Med. J. 2016, 22, 589–599. [Google Scholar] [CrossRef] [Green Version]
- Schulze-Döbold, C.; Erginay, A.; Robert, N.; Chabouis, A.; Massin, P. Ophdiat®: Five-year experience of a telemedical screening programme for diabetic retinopathy in Paris and the surrounding area. Diabetes Metab. 2012, 38, 450–457. [Google Scholar] [CrossRef]
- Soulié-Strougar, M.; Charles, A.; Métral, P.; Quercia, P.; Souchier, M.; Chirpaz, L.; Bron, A.; Creuzot-Garcher, C. Screening diabetic retinopathy in Burgundy with an itinerant nonmydriatic camera. J. Fr. Ophtalmol. 2007, 30, 121–126. [Google Scholar] [CrossRef]
- Sasso, F.C.; Pafundi, P.C.; Gelso, A.; Bono, V.; Costagliola, C.; Marfella, R.; Sardu, C.; Rinaldi, L.; Galiero, R.; Acierno, C.; et al. Telemedicine for screening diabetic retinopathy: The NO BLIND Italian multicenter study. Diabetes Metab. Res. Rev. 2019, 35, e3113. [Google Scholar] [PubMed]
- Keel, S.; Xie, J.; Foreman, J.; Taylor, H.R.; Dirani, M. Prevalence and characteristics of choroidal nevi: The Australian National Eye Health Survey. Clin. Exp. Ophthalmol. 2018, 46, 777–782. [Google Scholar] [CrossRef] [Green Version]
- Chien, J.L.; Sioufi, K.; Surakiatchanukul, T.; Shields, J.A.; Shields, C.L. Choroidal nevus: A review of prevalence, features, genetics, risks, and outcomes. Curr. Opin. Ophthalmol. 2017, 28, 228–237. [Google Scholar] [CrossRef]
- Sumich, P.; Mitchell, P.; Wang, J.J. Choroidal nevi in a white population: The Blue Mountains Eye Study. Arch. Ophthalmol. 1998, 116, 645–650. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colijn, J.M.; Buitendijk, G.H.S.; Prokofyeva, E.; Alves, D.; Cachulo, M.L.; Khawaja, A.P.; Cougnard-Gregoire, A.; Merle, B.M.J.; Korb, C.; Erke, M.G.; et al. Prevalence of Age-Related Macular Degeneration in Europe: The Past and the Future. Ophthalmology 2017, 124, 1753–1763. [Google Scholar] [CrossRef] [Green Version]
- Bron, A.; Baudouin, C.; Nordmann, J.P.; Rouland, J.F.; Thomas, F.; Bean, K.; De Clercq, B.; Bénétos, A.; de Gendre, A.S.; Lefebvre, S. Prevalence of intraocular hypertension and glaucoma in a nonselected French population. J. Fr. Ophtalmol. 2006, 29, 635–641. [Google Scholar] [CrossRef]
- Galiero, R.; Pafundi, P.C.; Nevola, R.; Rinaldi, L.; Acierno, C.; Caturano, A.; Salvatore, T.; Adinolfi, L.E.; Costagliola, C.; Sasso, F.C. The Importance of Telemedicine during COVID-19 Pandemic: A Focus on Diabetic Retinopathy. J. Diabetes Res. 2020, 2020, 9036847. [Google Scholar] [CrossRef]
- Sasso, F.C.; Pafundi, P.C.; Gelso, A.; Bono, V.; Costagliola, C.; Marfella, R.; Sardu, C.; Rinaldi, L.; Galiero, R.; Acierno, C.; et al. High HDL cholesterol: A risk factor for diabetic retinopathy? Findings from NO BLIND study. Diabetes Res. Clin. Pract. 2019, 150, 236–244. [Google Scholar] [CrossRef]
- Sasso, F.; Pafundi, P.C.; Gelso, A.; Bono, V.; Costagliola, C.; Marfella, R.; Sardu, C.; Rinaldi, L.; Galiero, R.; Acierno, C.; et al. Relationship between albuminuric CKD and diabetic retinopathy in a real-world setting of type 2 diabetes: Findings from No blind study. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 923–930. [Google Scholar] [CrossRef]
- Mukona, D.M.; Zvinavashe, M. Self- management of diabetes mellitus during the Covid-19 pandemic: Recommendations for a resource limited setting. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1575–1578. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Jayadev, C.; Nittala, M.G.; Velaga, S.B.; Ramachandra, C.A.; Bhaskaranand, M.; Bhat, S.; Solanki, K.; Sadda, S.R. Automated detection of diabetic retinopathy lesions on ultrawidefield pseudocolour images. Acta Ophthalmol. 2018, 96, e168–e173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharafeldin, N.; Kawaguchi, A.; Sundaram, A.; Campbell, S.; Rudnisky, C.; Weis, E.; Tennant, M.T.S.; Damji, K.F. Review of economic evaluations of teleophthalmology as a screening strategy for chronic eye disease in adults. Br. J. Ophthalmol. 2018, 102, 1485–1491. [Google Scholar] [CrossRef] [PubMed]

| Gender | |
|---|---|
| Female | 4154 (40.7) |
| Male | 6066 (59.4) |
| Age (years) a | 68.5 (±11.2) |
| Attending ophthalmologist | 3744 (36.5) |
| Type of diabetes | |
| Type 1 | 355 (3.5) |
| Type 2 | 8993 (88.0) |
| Unknown | 877 (8.5) |
| Treatment of diabetes | |
| Oral antidiabetics | 9063 (88.7) |
| Insulin | 1762 (17.2) |
| Treatment of high blood pressure | 6557 (64.2) |
| Progression ≥ 1 year | 1146 (11.2) |
| Last check-up more than 2 years before | 4438 (43.4) |
| Number of screenings per patient | |
| 1 | 8321 (81.4) |
| 2 | 1450 (14.2) |
| 3 or more | 449 (4.4) |
| DR Status | |
|---|---|
| No DR | 8209 (80.3) |
| All stages | 1420 (13.9) |
| Mild NPDR | 948 (9.3) |
| Moderate NPDR | 366 (3.6) |
| Severe NPDR | 84 (0.8) |
| PDR | 22 (0.2) |
| Unreadable | 590 (5.8) |
| Other pathologies | |
| Media opacity | 692 (6.8) |
| Late AMD | 347 (3.4) |
| Nevus | 287 (2.8) |
| CRVO | 20 (0.2) |
| OHT | 799 (7.8) |
| Papillary anomaly | 418 (4.1) |
| DR Any Type | No DR | p-Value a | |
|---|---|---|---|
| Number | 1420 | 8210 | |
| Age (years) b | 68.5 (±11.3) | 68.3 (±11.2) | 0.44 |
| Gender c | 841 (59.2) | 4859 (59.0) | 0.98 |
| Attending ophthalmologist c | 474 (33.4) | 3041 (37.0) | <0.01 |
| HbA1c (%) b | 7.44 (±1.4) | 6.99 (±1.1) | <0.001 |
| Progression of diabetes b | 13.76 (±10.9) | 9.31 (±8.9) | <0.001 |
| Time since last check-up b | 3.47 (±3.3) | 3.68 (±3.7) | 0.04 |
| Type of diabetes b,d, 8851 patients | |||
| Type 1 | 73 (6.1) | 258 (3.4) | <0.001 |
| Type 2 | 1129 (93.9) | 7391 (96.6) | - |
| Treatment of diabetes b | |||
| Oral antidiabetics | 1181 (83.2) | 7380 (89.9) | <0.001 |
| Insulin | 490 (34.5) | 1295 (15.8) | <0.001 |
| Other pathologies b | |||
| Media opacity | 96 (6.8) | 527 (6.4) | 0.63 |
| Late AMD | 46 (3.2) | 294 (3.6) | 0.52 |
| Naevus | 31 (2.2) | 253 (3.1) | 0.07 |
| CRVO | 2 (0.1) | 19 (0.2) | 0.76 |
| OHT | 131 (9.2) | 615 (7.4) | 0.02 |
| ONH anomaly | 72 (5.1) | 337 (4.1) | 0.10 |
| Rural Townships | Suburban Townships | p-Value a | |
|---|---|---|---|
| 2753 | 1230 | - | |
| Age (years) b | 73.1 (±11.2) | 74.5 (±11.2) | <0.001 |
| Males c | 1630 (59.2) | 738 (60.0) | 0.64 |
| Attending ophthalmologist c | 910 (33.1) | 440 (35.8) | 0.09 |
| HbA1c (%) b | 7.1 (±1.2) | 7.0 (±1.1) | 0.06 |
| Treatment of diabetes c | |||
| Oral antidiabetics | 2471 (89.8) | 1106 (89.9) | 0.88 |
| Insulin | 467 (17.0) | 235 (19.1) | 0.10 |
| DR status c | |||
| No DR | 2379 (86.4) | 1040 (84.6) | 0.12 |
| Mild NPDR | 220 (8.0) | 123 (10.0) | 0.04 |
| Moderate NPDR | 78 (2.8) | 42 (3.4) | 0.32 |
| Severe NPDR | 14 (0.5) | 8 (0.7) | 0.58 |
| PDR | 11 (0.4) | 2 (0.2) | 0.37 |
| Unreadable c | 51 (1.9) | 15 (1.2) | 0.15 |
| Other pathologies c | |||
| Media opacity | 265 (9.6) | 106 (8.6) | 0.31 |
| Late AMD | 118 (4.3) | 40 (3.3) | 0.12 |
| Nevus | 140 (5.1) | 48 (3.9) | 0.10 |
| CRVO | 8 (0.3) | 3 (0.2) | 1.00 |
| OHT | 190 (6.9) | 102 (8.3) | 0.12 |
| ONH anomaly | 117 (4.3) | 52 (4.2) | 0.97 |
| Rural Townships | Suburban Townships | Odds Ratio | p-Value a | |
|---|---|---|---|---|
| Age (years) b | 73.1 (±11.3) | 74.5 (±11.2) | 0.24 (0.11; 0.51) | <0.001 |
| Males c | 1630 (59.2) | 738 (60.0) | 0.95 (0.83; 1.09) | 0.46 |
| HbA1c (%) b | 7.1 (±1.2) | 7.0 (±1.1) | 1.10 (1.00; 1.22) | 0.06 |
| Insulin c | 467 (17.0) | 235 (19.1) | 0.83 (0.69; 1.00) | 0.05 |
| Attending ophthalmologist c | 910 (33.1) | 440 (35.8) | 0.88 (0.77; 1.02) | 0.09 |
| No DR c | 2379 (86.4) | 1040 (84.6) | 0.71 (0.40; 1.27) | 0.24 |
| Mild NPDR c | 220 (8.0) | 123 (10.0) | 0.79 (0.54; 1.14) | 0.20 |
| Before Lockdown | After Lockdown | p-Value a | |
|---|---|---|---|
| 367 | 441 | ||
| Age (years) b | 70.3 (±11.7) | 69.1 (±10.2) | 0.04 |
| Males c | 212 (57.8) | 271 (61.5) | 0.31 |
| HbA1c (%) b | 7.1 (±1.2) | 6.9 (±1.0) | 0.28 |
| Progression of diabetes (years) b | 11.9 (±10.4) | 11.2 (±9.6) | 0.37 |
| Insulin-dependent c | 71 (20.5) | 69 (16.8) | 0.22 |
| DR status c | 0.56 | ||
| No DR | 325 (88.5) | 393 (89.1) | - |
| Mild NPDR | 29 (7.9) | 37 (8.4) | - |
| Moderate NPDR | 7 (1.9) | 9 (2.0) | - |
| Severe NPDR | 5 (1.4) | 2 (0.5) | - |
| PDR | 1 (0.3) | 0 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charlot, A.; Baudin, F.; Tessier, M.; Lebrize, S.; Hurand, V.; Megroian, D.; Arnould, L.; Ben-Ghezala, I.; Bron, A.M.; Gabrielle, P.-H.; et al. Mobile Telemedicine Screening for Diabetic Retinopathy Using Nonmydriatic Fundus Photographs in Burgundy: 11 Years of Results. J. Clin. Med. 2022, 11, 1318. https://doi.org/10.3390/jcm11051318
Charlot A, Baudin F, Tessier M, Lebrize S, Hurand V, Megroian D, Arnould L, Ben-Ghezala I, Bron AM, Gabrielle P-H, et al. Mobile Telemedicine Screening for Diabetic Retinopathy Using Nonmydriatic Fundus Photographs in Burgundy: 11 Years of Results. Journal of Clinical Medicine. 2022; 11(5):1318. https://doi.org/10.3390/jcm11051318
Chicago/Turabian StyleCharlot, Anthony, Florian Baudin, Mélanie Tessier, Sarah Lebrize, Victoire Hurand, Déborah Megroian, Louis Arnould, Inès Ben-Ghezala, Alain Marie Bron, Pierre-Henry Gabrielle, and et al. 2022. "Mobile Telemedicine Screening for Diabetic Retinopathy Using Nonmydriatic Fundus Photographs in Burgundy: 11 Years of Results" Journal of Clinical Medicine 11, no. 5: 1318. https://doi.org/10.3390/jcm11051318
APA StyleCharlot, A., Baudin, F., Tessier, M., Lebrize, S., Hurand, V., Megroian, D., Arnould, L., Ben-Ghezala, I., Bron, A. M., Gabrielle, P.-H., & Creuzot-Garcher, C. (2022). Mobile Telemedicine Screening for Diabetic Retinopathy Using Nonmydriatic Fundus Photographs in Burgundy: 11 Years of Results. Journal of Clinical Medicine, 11(5), 1318. https://doi.org/10.3390/jcm11051318







