Construction of a Prognostic Score for Ultrasound Evaluation of the Transobturator Sling for Stress Urinary Incontinence
Abstract
:1. Introduction
- Position of the sling with respect to the urethra (proximal, middle, or distal third) both at rest and in Valsalva.
- Distance between the sling and the posterior urethral wall is considered adequate if between 3–5 mm (in 2D transperineal). With a high-frequency probe, it is possible to accurately calculate the distance between the sling and the urethral light.
- Sling shape (at rest and Valsalva). The tapes usually have a flat shape at rest, determined by their shape parallel to the urethral lumen, and they deform into a “C” shape in Valsalva in relation to the tension caused by the increase in intra-abdominal pressure.
- Concordance of the urethral movement with that of the sling during the Valsalva (urethral kinking).
- The symmetry of the sling and its arms in the cross-section or corona. It allows assessment of the extrusion or winding of the sling arms.
2. Materials and Methods
3. Results
3.1. Descriptive Study
3.2. Bivariate Analysis of the Sonographic Parameters
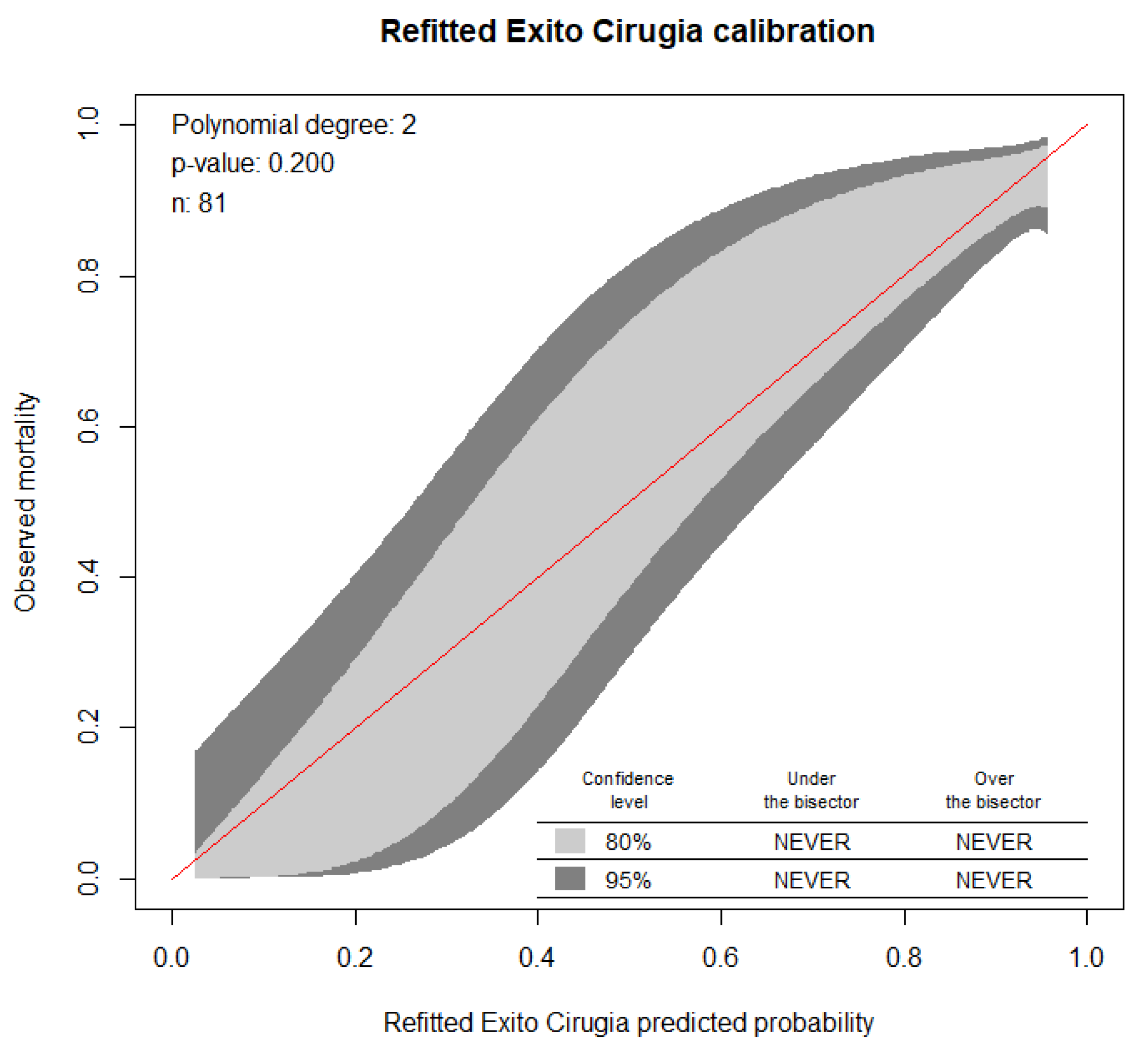
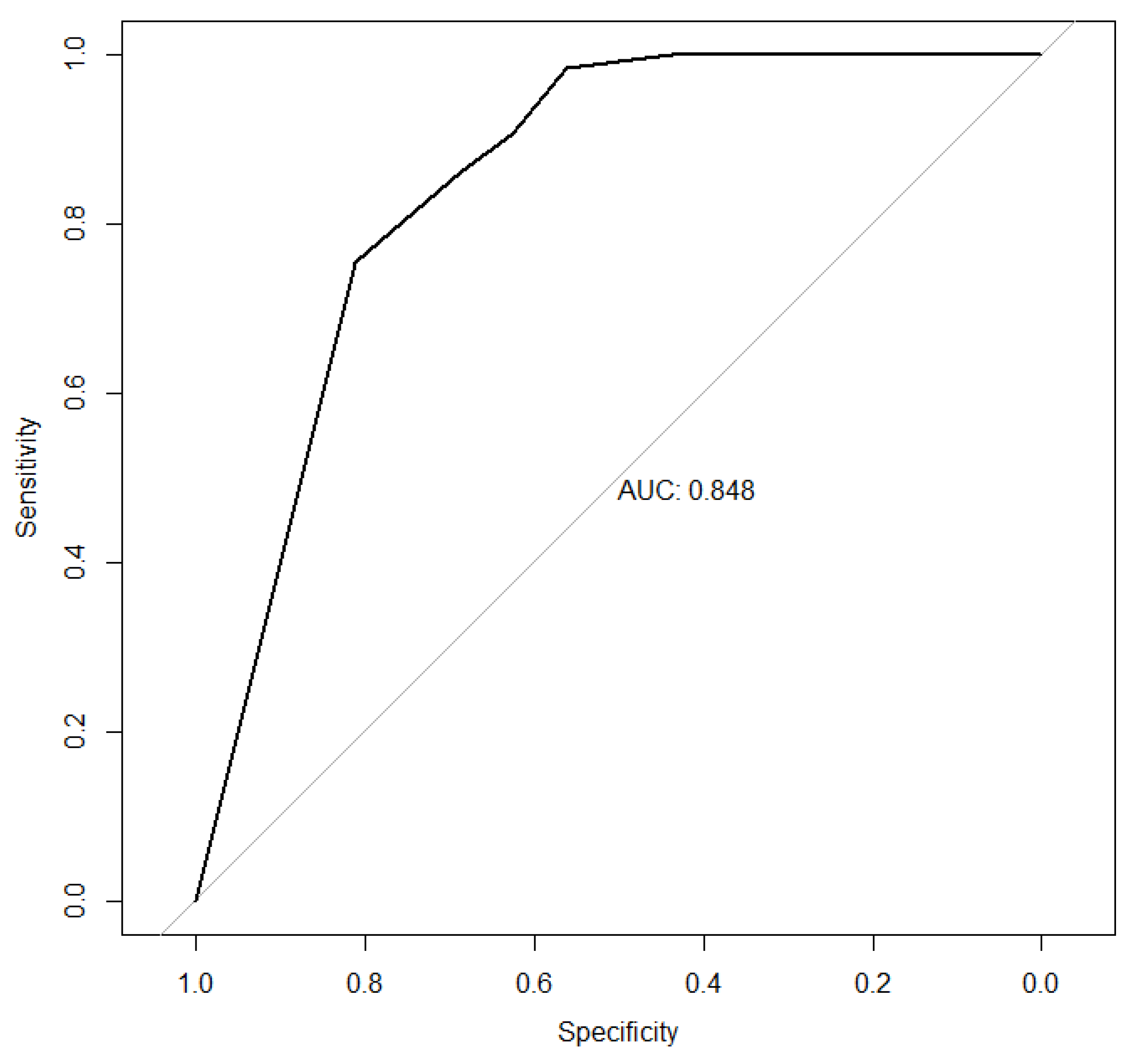
3.3. Predictive Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Batmani, S.; Jalali, R.; Mohammadi, M.; Bokaee, S. Prevalence and factors related to urinary incontinence in older adults women worldwide: A comprehensive systematic review and meta-analysis of observational studies. BMC Geriatr. 2021, 21, 29. [Google Scholar] [CrossRef]
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; Van Kerrebroeck, P.; Victor, A.; Wein, A. The standardisation of terminology in lower urinary tract function: Report from the standardisation sub-committee of the international continence society. Urology 2003, 61, 37–49. [Google Scholar] [CrossRef]
- Haylen, B.T.; De Ridder, D.; Freeman, R.M.; Swift, S.E.; Berghmans, B.; Lee, J.; Monga, A.; Petri, E.; Rizk, D.E.; Sand, P.K.; et al. An international urogynecological association (iuga)/international continence society (ics) joint report on the terminology for female pelvic floor dysfunction. Int. Urogynecol. J. 2010, 21, 5–26. [Google Scholar] [CrossRef] [PubMed]
- Robles, J.E. La incontinencia urinaria. An. Sist. Sanit. Navar. 2006, 29, 219–231. Available online: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1137-66272006000300006&lng=es&nrm=iso&tlng=es (accessed on 15 July 2021). (In Spanish). [CrossRef] [Green Version]
- Kirchin, V.; Page, T.; Keegan, P.E.; Atiemo, K.O.M.; Cody, J.D.; McClinton, S.; Aluko, P. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst. Rev. 2017, 2017, 28738443. [Google Scholar] [CrossRef] [PubMed]
- Berek, J.S.; Kraus, L.; Professor, L.; Berek, D.L. Berek & Novak’s Gynecology; Wolters Kluwer: Philadelphia, PA, USA, 2020. [Google Scholar]
- Hilton, P. Operations for urinary incontinence. In Bonney’s Gynaecological Surgery, 12th ed.; de Barros Lopes, A., Spirtos Nick, M., Hilton, P., Monaghan John, M., Eds.; John Wiley & Sons, Ltd.: Chichester, UK, 2018; pp. 193–230. [Google Scholar]
- Aygül, C.; Özyurt, R.; Aytek Şık, B.; Kumbasar, S. Evaluation of the efficacy of transobturator tape surgery in the treatment of stress urinary incontinence using urodynamics and questionnaires. J. Turk. Soc. Obstet. Gynecol. 2016, 13, 172–177. [Google Scholar] [CrossRef]
- López, M.A.; Albarracín, A.; Lauroba, P.; Sanjuan, A. Banda libre de tensión transobturadora en el tratamiento de la incontinencia urinaria femenina. Cinco años de experiencia en un hospital comarcal. Clín. Investig. Ginecol. Obstet. 2013, 40, 253–258. [Google Scholar] [CrossRef]
- Staack, A.; Vitale, J.; Ragavendra, N.; Rodríguez, L.V. Translabial ultrasonography for evaluation of synthetic mesh in the vagina. Urology 2014, 83, 68–74. [Google Scholar] [CrossRef]
- Manonai, J.; Rostaminia, G.; Denson, L.; Shobeiri, S.A. Clinical and ultrasonographic study of patients presenting with transvaginal mesh complications. Neurourol. Urodyn. 2016, 35, 407–411. [Google Scholar] [CrossRef]
- Chantarasorn, V.; Shek, K.L.; Dietz, H.P. Sonographic appearance of transobturator slings: Implications for function and dysfunction. Int. Urogynecol. J. 2011, 22, 493–498. [Google Scholar] [CrossRef]
- Jiménez Cidre, M.Á.; López-Fando Lavalle, L.; Quicios Dorado, C.; Castro Guerín, C.D.; Fraile Poblador, A.; Mayayo Dehesa, T. Ecografía en el diagnóstico de la incontinencia urinaria femenina. Arch. Españoles Urol. (Ed. Impresa) 2006, 59, 431–439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dietz, H.P. Pelvic floor ultrasound: A review. Am. J. Obstet. Gynecol. 2016, 202, 321–334. [Google Scholar] [CrossRef] [PubMed]
- Dietz, H.P.; Hoyte, L.P.J.; Steensma, A.B. Atlas of Pelvic Floor Ultrasound; Springer: London, UK, 2008. [Google Scholar] [CrossRef]
- Hegde, A.; Nogueiras, M.; Aguilar, V.C.; Davila, G.W. Dynamic assessment of sling function on transperineal ultrasound: Does it correlate with outcomes 1 year following surgery? Int. Urogynecol. J. 2017, 28, 857–864. [Google Scholar] [CrossRef]
- Wermuth, D.E.; Sheridan, A.; Oliver, J.; Glanc, P.; Khatri, G.; Bagley, A.; Patel, N. Translabial ultrasound for assessment of synthetic midurethral sling complications. Ultrasound Q. 2021, 37, 237–243. [Google Scholar] [CrossRef]
- Skorupska, K.A.; Miotla, P.; Kubik-Komar, A.; Skorupski, P.; Rechberger, T. Development and validation of the polish version of the urogenital distress inventory short form and the incontinence impact questionnaire short form. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 215, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Nattino, G.; Lemeshow, S.; Phillips, G.; Finazzi, S.; Bertolini, G. Assessing the calibration of dichotomous outcome models with the calibration belt. Stata J. Promot. Commun. Stat. Stata 2017, 17, 1003–1014. [Google Scholar] [CrossRef] [Green Version]
- Kilinc, M.F.; Yildiz, Y.; Hascicek, A.M.; Doluoglu, O.G.; Tokat, E. Long-term postoperative follow-up results of transobturator autologous rectus fascial sling versus transobturator tension-free vaginal tapes for female stress urinary incontinence: Randomized controlled clinical trial. Neurourol. Urodyn. 2021, 41, 281–289. [Google Scholar] [CrossRef]
- Sabadell, J.; Montero-Armengol, A.; Salicrú, S.; Catalán-Martínez, M.; Gil-Moreno, A.; Poza, J.L. Long-term outcomes of transobturator suburethral tapes for female stress urinary incontinence. Neurourol. Urodyn. 2021, 124, 973–981. [Google Scholar] [CrossRef]
- Illiano, E.; Trama, F.; Li Marzi, V.; Mancini, V.; Carrieri, G.; Ruvolo, C.C.; Califano, G.; Fabi, C.; Brancorsini, S.; Costantini, E. Translabial ultrasound: A non-invasive technique for assessing “technical errors” after tot failure. Int. Urogynecol. J. 2021. [Google Scholar] [CrossRef]
- Kociszewski, J.; Rautenberg, O.; Perucchini, D.; Eberhard, J.; Geissbühler, V.; Hilgers, R.; Viereck, V. Tape functionality: Sonographic tape characteristics and outcome after tvt incontinence surgery. Neurourol. Urodyn. 2008, 27, 485–490. [Google Scholar] [CrossRef]
- Taithongchai, A.; Sultan, A.H.; Wieczorek, P.A.; Thakar, R. Clinical application of 2d and 3d pelvic floor ultrasound of mid-urethral slings and vaginal wall mesh. Int. Urogynecol. J. 2019, 30, 1401–1411. [Google Scholar] [CrossRef]
- Duckett, J.; Thakar, R.; Shah, V.; Stephenson, J.; Balachandran, A. The use of imaging for synthetic midurethral slings. J. Ultrasound Med. 2020, 39, 1497–1506. [Google Scholar] [CrossRef] [PubMed]
- Apaza Valencia, J. Evaluación del suelo pélvico mediante ecografía introital. Rev. Peru. Ginecol. Obstet. 2016, 62, 235–246. [Google Scholar] [CrossRef]
- Ramírez-Ley, C.R.; Ramírez-Lucero, C.F.; Arias-Rosales, E.C. Ultrasonido en la evaluación de la incontinencia urinaria femenina no neurológica. Rev. Mex. Urol. 2011, 71, 319–324. [Google Scholar]
- Tan, Y.H.; Frazer, M.I.; Hughes, I.; Wong, V. Correlation between translabial ultrasound parameters and outcomes in retropubic mid-urethral slings: Can we predict success? World J. Urol. 2021, 39, 163–168. [Google Scholar] [CrossRef]

| Parameter | Media ± S.D. | n/N y% |
|---|---|---|
| Age | 51.71 ± 10.57 | |
| Obesity | 36/81 (44%) | |
| History of depression/anxiety | 18/81 (22%) | |
| Parity | 2.33 ± 1.16 | |
| Multiparity | 62/81 (76.54%) | |
| Childbirth >4000 g | 12/81 (14.81%) | |
| Cesarean deliveries | 2/81 (2.47%) | |
| Pre-surgical clinical | ||
| Stress UI | 52/81 (64.2%) | |
| Mixed UI | 29/81 (35.8%) | |
| No clinic | 0/81 (0%) | |
| Post-Surgical clinical | ||
| Stress UI | 6/81 (7.41%) | |
| Mixed UI | 10/81 (12.35%) | |
| Urgency | 16/81 (19.75%) | |
| No clinic | 49/81 (60.49%) | |
| Post-surgery ICIQ-IU | 11.13 ± 11.79 | |
| Ultrasound Parameter | Value | Non-Clinical Stress UI (n = 33) | Clinical Stress UI (n = 9) | Total |
|---|---|---|---|---|
| Distance to posterior urethral wall (p < 0.001) | <5 mm | 61 (93.8%) | 8 (50%) | 69 (85.2%) |
| >5 mm | 4 (6.2%) | 8 (50%) | 12 (14.8%) | |
| Position at rest (p = 0.04) | Not proximal | 65 (100%) | 14 (87.5%) | 79 (97.5%) |
| Proximal | 0 (0%) | 2 (12.5%) | 2 (2.5%) | |
| Form at rest (p < 0.001) | In C | 5 (7.7%) | 8 (50%) | 13 (16.1%) |
| Flat | 60 (92.3%) | 8 (50%) | 68 (84%) | |
| Form in Valsalva (p = 0.24) | In C | 57 (87.7%) | 12 (75%) | 69 (85.2%) |
| Flat | 8 (12.3%) | 4 (25%) | 12 (14.8%) | |
| Resting length—Valsalva (p = 0.17) | <15 mm | 63 (96.9%) | 14 (87.5%) | 77 (95.1%) |
| 15–25 mm | 2 (3.1%) | 2 (12.5%) | 4 (4.9%) | |
| Increased posterior urethrovesical angle (Valsalva—rest) (p = 0.21) | <15° | 58 (89.2%) | 12 (75%) | 70 (86.4%) |
| >15° | 7 (10.8%) | 4 (25%) | 11 (13.6%) | |
| Symmetry (p = 0.0083) | Asymmetric | 8 (12.3%) | 7 (43.8%) | 15 (18.5%) |
| Symmetrical | 57 (87.7%) | 9 (56.2%) | 66 (81.5%) | |
| Urethral concordance (p = 0.04) | Yes | 65 (100%) | 14 (87.5%) | 79 (97.5%) |
| No | 0 (0%) | 2 (12.5%) | 2 (2.5%) |
| Parameter | OR | IC 95% | p-Value |
|---|---|---|---|
| Distance sling to posterior urethral wall < 5 mm | 10.84 | 2.20–63.11 | 0.004 |
| Flat shape of the sling at rest | 11.63 | 2.41–66.24 | 0.003 |
| Sling symmetry | 6.95 | 1.48–36.96 | 0.016 |
| Clinical Stress UI | Non-Clinical Stress UI | Total | ||
|---|---|---|---|---|
| Clinic | YES | 16 (100%) | 0 (0%) | 16 (19.8%) |
| NO | 0 (0%) | 65 (100%) | 65 (80.2%) | |
| Score | 0–1 points | 9 (56.2%) | 2 (3.1%) | 11 (13.6%) |
| 2–3 points | 7 (43.8%) | 63 (96.9%) | 81 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cristina, E.-G.; Lorena, S.-M.; Rita, P.-G.; Santiago, G.-M.E.; Salvador, J.-L.J. Construction of a Prognostic Score for Ultrasound Evaluation of the Transobturator Sling for Stress Urinary Incontinence. J. Clin. Med. 2022, 11, 1296. https://doi.org/10.3390/jcm11051296
Cristina E-G, Lorena S-M, Rita P-G, Santiago G-ME, Salvador J-LJ. Construction of a Prognostic Score for Ultrasound Evaluation of the Transobturator Sling for Stress Urinary Incontinence. Journal of Clinical Medicine. 2022; 11(5):1296. https://doi.org/10.3390/jcm11051296
Chicago/Turabian StyleCristina, Espada-Gonzalez, Sabonet-Morente Lorena, Perez-Gonzalez Rita, Gonzalez-Mesa Ernesto Santiago, and Jimenez-Lopez Jesus Salvador. 2022. "Construction of a Prognostic Score for Ultrasound Evaluation of the Transobturator Sling for Stress Urinary Incontinence" Journal of Clinical Medicine 11, no. 5: 1296. https://doi.org/10.3390/jcm11051296
APA StyleCristina, E.-G., Lorena, S.-M., Rita, P.-G., Santiago, G.-M. E., & Salvador, J.-L. J. (2022). Construction of a Prognostic Score for Ultrasound Evaluation of the Transobturator Sling for Stress Urinary Incontinence. Journal of Clinical Medicine, 11(5), 1296. https://doi.org/10.3390/jcm11051296








