The Effect of Past Cataract Surgery within the Medium to Long-Term Period on Patients with Dry Eye Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
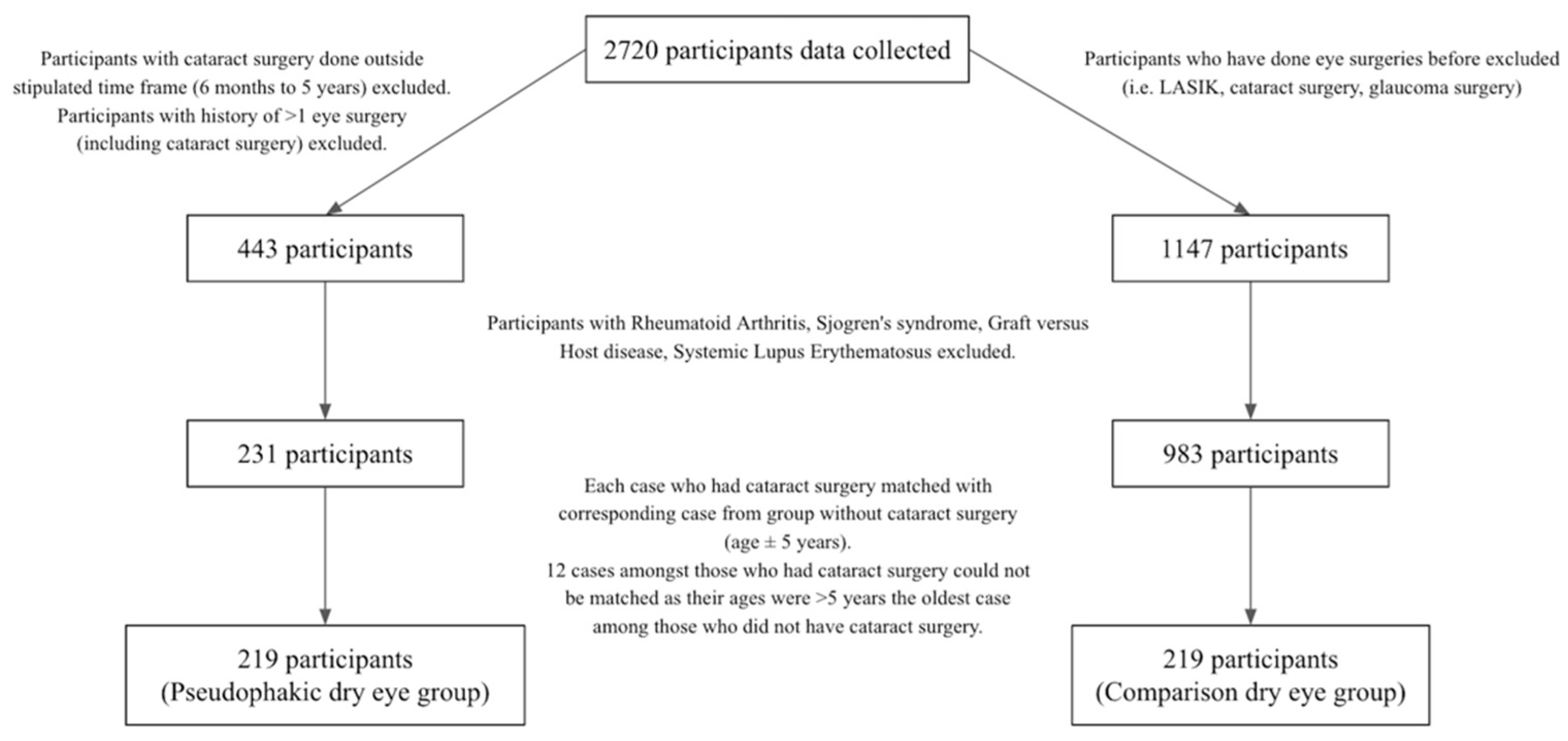
2.2. Participants
2.3. Study Outcomes
2.3.1. Questionnaire
2.3.2. Tear Break-Up Time
2.3.3. Schirmer’s I Test
2.3.4. Meibomian Gland Dysfunction (MGD) Examination
2.3.5. Fluorescein Corneal Staining
2.3.6. Other Clinical Examination
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Summary of Significant Findings
4.2. Comparison with Literature
4.3. Strengths and Weaknesses of Study
4.4. Potential Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tan, A.G.; Kifley, A.; Tham, Y.C.; Shi, Y.; Chee, M.L.; Sabanayagam, C.; Tan, N.Y.Q.; Wong, K.H.; Mitchell, P.; Cumming, R.G.; et al. Six-Year Incidence of and Risk Factors for Cataract Surgery in a Multi-ethnic Asian Population: The Singapore Epidemiology of Eye Diseases Study. Ophthalmology 2018, 125, 1844–1853. [Google Scholar] [CrossRef] [Green Version]
- Day, A.C.; Donachie, P.H.; Sparrow, J.M.; Johnston, R.L. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: Report 1, visual outcomes and complications. Eye 2015, 29, 552–560. [Google Scholar] [CrossRef] [Green Version]
- Addisu, Z.; Solomon, B. Patients’ preoperative expectation and outcome of cataract surgery at jimma university specialized hospital -department of ophthalmology. Ethiop. J. Health Sci. 2011, 21, 47–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taban, M.; Behrens, A.; Newcomb, R.L.; Nobe, M.Y.; Saedi, G.; Sweet, P.M.; McDonnell, P.J. Acute endophthalmitis following cataract surgery: A systematic review of the literature. Arch. Ophthalmol. 2005, 123, 613–620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia-Arumi, J.; Fonollosa, A.; Sararols, L.; Fina, F.; Martínez-Castillo, V.; Boixadera, A.; Zapata, M.A.; Campins, M. Topical anesthesia: Possible risk factor for endophthalmitis after cataract extraction. J. Cataract. Refract. Surg. 2007, 33, 989–992. [Google Scholar] [CrossRef] [PubMed]
- Nowak, M.S.; Grzybowski, A.; Michalska-Małecka, K.; Szaflik, J.P.; Kozioł, M.; Niemczyk, W.; Grabska-Liberek, I. Incidence and Characteristics of Endophthalmitis after Cataract Surgery in Poland, during 2010–2015. Int. J. Environ. Res. Public Health 2019, 16, 2188. [Google Scholar] [CrossRef] [Green Version]
- Rhee, J.; Chan, T.C.; Chow, S.S.; Di Zazzo, A.; Inomata, T.; Shih, K.C.; Tong, L. A Systematic Review on the Association Between Tear Film Metrics and Higher Order Aberrations in Dry Eye Disease and Treatment. Ophthalmol. Ther. 2022, 11, 35–67. [Google Scholar] [CrossRef]
- Teo, C.H.Y.; Ong, H.S.; Liu, Y.C.; Tong, L. Meibomian gland dysfunction is the primary determinant of dry eye symptoms: Analysis of 2346 patients. Ocul. Surf. 2020, 18, 604–612. [Google Scholar] [CrossRef]
- Tong, L.; Lim, L.; Tan, D.; Heng, W.J.; Lim, J.; Chan, C.; Arundhati, A.; Tan, A. Assessment and Management of Dry Eye Disease and Meibomian Gland Dysfunction: Providing a Singapore Framework. Asia Pac. J. Ophthalmol. 2021, 10, 530–541. [Google Scholar] [CrossRef]
- Li, X.M.; Hu, L.; Hu, J.; Wang, W. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea 2007, 26, S16–S20. [Google Scholar] [CrossRef]
- Venugopal KC, K.P. Evaluation of Dryness of Eyes after Manual Small Incision Cataract Surgery with Corneoscleral Tunnel Incision. J. Clin. Diagn. Res. 2012, 6, 1029–1033. [Google Scholar]
- Cho, Y.K.; Kim, M.S. Dry eye after cataract surgery and associated intraoperative risk factors. Korean J. Ophthalmol. 2009, 23, 65–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Congdon, N.G.; Schein, O.D.; von Kulajta, P.; Lubomski, L.H.; Gilbert, D.; Katz, J. Corneal complications associated with topical ophthalmic use of nonsteroidal antiinflammatory drugs. J. Cataract. Refract. Surg. 2001, 27, 622–631. [Google Scholar] [CrossRef]
- Oh, T.; Jung, Y.; Chang, D.; Kim, J.; Kim, H. Changes in the tear film and ocular surface after cataract surgery. Jpn. J. Ophthalmol. 2012, 56, 113–118. [Google Scholar] [CrossRef]
- Khanal, S.; Tomlinson, A.; Esakowitz, L.; Bhatt, P.; Jones, D.; Nabili, S.; Mukerji, S. Changes in corneal sensitivity and tear physiology after phacoemulsification. Ophthalmic Physiol. Opt. 2008, 28, 127–134. [Google Scholar] [CrossRef]
- He, Y.; Li, J.; Zhu, J.; Jie, Y.; Wang, N.; Wang, J. The improvement of dry eye after cataract surgery by intraoperative using ophthalmic viscosurgical devices on the surface of cornea: The results of a consort-compliant randomized controlled trial. Medicine 2017, 96, e8940. [Google Scholar] [CrossRef]
- Gomes, J.A.P.; Azar, D.T.; Baudouin, C.; Efron, N.; Hirayama, M.; Horwath-Winter, J.; Kim, T.; Mehta, J.S.; Messmer, E.M.; Pepose, J.S.; et al. TFOS DEWS II iatrogenic report. Ocul. Surf. 2017, 15, 511–538. [Google Scholar] [CrossRef]
- Camesasca, F.I.; Bianchi, C.; Beltrame, G.; Caporossi, A.; Piovella, M.; Rapisarda, A.; Tassinari, G.; Zeppa, L. Control of inflammation and prophylaxis of endophthalmitis after cataract surgery: A multicenter study. Eur. J. Ophthalmol. 2007, 17, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Song, P.; Sun, Z.; Ren, S.; Yang, K.; Deng, G.; Zeng, Q.; Sun, Y. Preoperative Management of MGD Alleviates the Aggravation of MGD and Dry Eye Induced by Cataract Surgery: A Prospective, Randomized Clinical Trial. Biomed. Res. Int. 2019, 2019, 2737968. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, Y.J.; Park, S.Y.; Jun, I.; Choi, M.; Seo, K.Y.; Kim, E.K.; Kim, T.I. Perioperative Ocular Parameters Associated With Persistent Dry Eye Symptoms After Cataract Surgery. Cornea 2018, 37, 734–739. [Google Scholar] [CrossRef] [PubMed]
- Kasetsuwan, N.; Satitpitakul, V.; Changul, T.; Jariyakosol, S. Incidence and pattern of dry eye after cataract surgery. PLoS ONE 2013, 8, e78657. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, R.M.; Christianson, M.D.; Jacobsen, G.; Hirsch, J.D.; Reis, B.L. Reliability and validity of the Ocular Surface Disease Index. Arch. Ophthalmol. 2000, 118, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Foong, A.W.; Saw, S.M.; Loo, J.L.; Shen, S.; Loon, S.C.; Rosman, M.; Aung, T.; Tan, D.T.; Tai, E.S.; Wong, T.Y. Rationale and methodology for a population-based study of eye diseases in Malay people: The Singapore Malay eye study (SiMES). Ophthalmic Epidemiol. 2007, 14, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Koh, S.; Watanabe, H.; Hosohata, J.; Hori, Y.; Hibino, S.; Nishida, K.; Maeda, N.; Tano, Y. Diagnosing dry eye using a blue-free barrier filter. Am. J. Ophthalmol. 2003, 136, 513–519. [Google Scholar] [CrossRef]
- Korb, D.R.; Blackie, C.A. Meibomian gland diagnostic expressibility: Correlation with dry eye symptoms and gland location. Cornea 2008, 27, 1142–1147. [Google Scholar] [CrossRef]
- Rashid, M.; Thia, Z.Z.; Teo, C.H.Y.; Mamun, S.; Ong, H.S.; Tong, L. Evaluation of Strip Meniscometry and Association with Clinical and Demographic Variables in a Community Eye Study (in Bangladesh). J. Clin. Med. 2020, 9, 3366. [Google Scholar] [CrossRef]
- De Paiva, C.S.; Pflugfelder, S.C. Corneal epitheliopathy of dry eye induces hyperesthesia to mechanical air jet stimulation. Am. J. Ophthalmol. 2004, 137, 109–115. [Google Scholar] [CrossRef]
- Peterson, R.C.; Wolffsohn, J.S. Objective grading of the anterior eye. Optom. Vis. Sci. 2009, 86, 273–278. [Google Scholar] [CrossRef]
- Terry, R.L.; Schnider, C.M.; Holden, B.A.; Cornish, R.; Grant, T.; Sweeney, D.; La Hood, D.; Back, A. CCLRU standards for success of daily and extended wear contact lenses. Optom. Vis. Sci. 1993, 70, 234–243. [Google Scholar] [CrossRef]
- Bruce, A.S. 37—Preliminary Examination. In Contact Lens Practice, 3rd ed.; Efron, N., Ed.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 346–355.e341. [Google Scholar]
- Danjo, Y. Diagnostic usefulness and cutoff value of Schirmer’s I test in the Japanese diagnostic criteria of dry eye. Graefes Arch. Clin. Exp. Ophthalmol. 1997, 235, 761–766. [Google Scholar] [CrossRef]
- Garg, P.; Gupta, A.; Tandon, N.; Raj, P. Dry Eye Disease after Cataract Surgery: Study of its Determinants and Risk Factors. Turk. J. Ophthalmol. 2020, 50, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.W.; Han, S.J.; Nam, S.M.; Kim, T.I.; Kim, E.K.; Seo, K.Y. Meibomian gland dysfunction and tear cytokines after cataract surgery according to preoperative meibomian gland status. Clin. Exp. Ophthalmol. 2016, 44, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Xue, W.; Zhu, M.M.; Zhu, B.J.; Huang, J.N.; Sun, Q.; Miao, Y.Y.; Zou, H.D. Long-term impact of dry eye symptoms on vision-related quality of life after phacoemulsification surgery. Int. Ophthalmol. 2019, 39, 419–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, K.E.; Yoon, S.C.; Ahn, J.M.; Nam, S.M.; Stulting, R.D.; Kim, E.K.; Seo, K.Y. Evaluation of dry eye and meibomian gland dysfunction after cataract surgery. Am. J. Ophthalmol. 2014, 157, 1144–1150.e1141. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.; Rastad, H.; Emamian, M.H.; Fotouhi, A. Meibomian gland dysfunction and its determinants in Iranian adults: A population-based study. Cont. Lens Anterior Eye 2017, 40, 213–216. [Google Scholar] [CrossRef]
- McCarty, C.A.; Bansal, A.K.; Livingston, P.M.; Stanislavsky, Y.L.; Taylor, H.R. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology 1998, 105, 1114–1119. [Google Scholar] [CrossRef]
- Kato, K.; Miyake, K.; Hirano, K.; Kondo, M. Management of Postoperative Inflammation and Dry Eye After Cataract Surgery. Cornea 2019, 38 (Suppl. 1), S25–S33. [Google Scholar] [CrossRef] [PubMed]
- Shibata, Y.; Tanaka, Y.; Tomita, T.; Taogoshi, T.; Kimura, Y.; Chikama, T.; Kihira, K. Evaluation of corneal damage caused by iodine preparations using human corneal epithelial cells. Jpn. J. Ophthalmol. 2014, 58, 522–527. [Google Scholar] [CrossRef]
- Liu, Z.; Luo, L.; Zhang, Z.; Cheng, B.; Zheng, D.; Chen, W.; Lin, Z.; Yang, W.; Liu, Y.; Zhang, M.; et al. Tear film changes after phacoemulsification. Zhonghua Yan Ke Za Zhi 2002, 38, 274–277. (In Chinese) [Google Scholar]
- Hoshi, S.; Tasaki, K.; Hiraoka, T.; Oshika, T. Improvement in Contrast Sensitivity Function after Lacrimal Passage Intubation in Eyes with Epiphora. J. Clin. Med. 2020, 9, 2761. [Google Scholar] [CrossRef]
- Naderi, K.; Gormley, J.; O’Brart, D. Cataract surgery and dry eye disease: A review. Eur. J. Ophthalmol. 2020, 30, 840–855. [Google Scholar] [CrossRef] [PubMed]
| Pseudophakic Dry Eye Group Mean ± Standard Deviation Median (Min, Max) | Comparison Dry Eye Group Mean ± Standard Deviation Median (Min, Max) | p-Value † | |
|---|---|---|---|
| Age (years) | 69.3 ± 7.96 70 (48, 91) | 68.1 ± 4.81 67 (53, 91) | 0.055 |
| Ocular Surface Disease Index score | 31.8 ± 20.9 27.1 (0, 91.7) | 31.4 ± 20.0 28.8 (0, 88.5) | 0.838 |
| Schirmer’s I Test (mm) | 7.51 ± 7.65 6 (0, 37) | 6.51 ± 6.79 5 (0, 35) | 0.145 |
| Tear Break-up Score (seconds) | 2.45 ± 1.59 2 (0, 11) | 2.48 ± 1.92 2 (0, 17) | 0.865 |
| Number of liquid-expressing glands in lower lid | 1.80 ± 2.60 1 (0, 15) | 1.70 ± 2.48 1 (0, 15) | 0.658 |
| Baylor Score Total | 5.16 ± 6.15 3 (0, 25) | 5.63 ± 5.76 4 (0, 21) | 0.394 |
| Superior | 0.398 ± 1.13 0 (0, 5) | 0.361 ± 1.16 0 (0, 4) | 0.692 |
| Inferior | 1.67 ± 1.67 1 (0, 5) | 1.79 ± 1.72 2 (0, 5) | 0.458 |
| Nasal | 0.91 ± 1.49 0 (0, 5) | 1.059 ± 1.49 0 (0, 5) | 0.296 |
| Temporal | 1.18 ± 1.71 0 (0, 5) | 1.31 1 (0, 5) | 0.437 |
| Central | 0.915 ± 1.55 0 (0, 6) | 0.827 ± 1.41 0 (0, 5) | 0.530 |
| Frequency of Symptom in a Week | Pseudophakic Dry Eye Group N (%) | Comparison Dry Eye Group N (%) | p-Value † |
|---|---|---|---|
| Light sensitivity | |||
| <1 ≥1 | 139 80 (36.5%) | 143 76 (34.70%) | 0.690 |
| Grittiness | |||
| <1 ≥1 | 115 104 (47.5%) | 116 103 (47.0%) | 0.924 |
| Burning | |||
| <1 ≥1 | 157 62 (28.2%) | 152 67 (30.6%) | 0.600 |
| Blurring | |||
| <1 ≥1 | 109 110 (50.2%) | 136 83 (37.9%) | 0.009 * |
| Vision fluctuation with blinking | |||
| <1 ≥1 | 148 71 (32.4%) | 155 64 (29.2%) | 0.469 |
| Vision fluctuation with artificial tears | |||
| <1 ≥1 | 141 77 (35.3%) | 138 81 (37.0%) | 0.717 |
| Tearing | |||
| <1 ≥1 | 149 69 (31.7%) | 152 67 (30.6%) | 0.811 |
| Pain | |||
| <1 ≥1 | 194 25 (11.4%) | 194 25 (11.4%) | 1.00 |
| Fatigue | |||
| <1 ≥1 | 113 104 (47.9%) | 113 106 (48.4%) | 0.921 |
| Driving | |||
| <1 ≥1 | 122 97 (44.3%) | 123 96 (43.8%) | 0.923 |
| Television | |||
| <1 ≥1 | 118 101 (46.1%) | 120 99 (45.2%) | 0.848 |
| Wind | |||
| <1 ≥1 | 134 85 (38.8%) | 135 84 (38.4%) | 0.923 |
| Aircon | |||
| <1 ≥1 | 174 45 (20.5%) | 165 54 (24.7%) | 0.304 |
| Frequency of Symptom in a Day | Symptomatic Dry Eyes Prior to Surgery N (%) | No Symptomatic Dry Eyes Prior to Surgery N (%) | p-Value † |
|---|---|---|---|
| Blurred vision | |||
| <1 ≥1 | 44 22 (33.3%) | 115 28 (19.6%) | 0.003 * |
| Pseudophakic Dry Eye Group N (%) | Comparison Dry Eye Group N (%) | p-Value † | |
|---|---|---|---|
| Gender | |||
| Male Female | 55 (24.6%) 169 (75.4%) | 44 (20.1%) 175 (79.9%) | 0.313 |
| Ocular Surface Disease Index (OSDI) score | |||
| <33 ≥33 | 126 92 (42.2%) | 122 97 (44.3%) | 0.659 |
| Corneal sensation Normal Decreased or absent | 213 4 (1.8%) | 213 4 (1.8%) | 1.00 |
| Schirmer’s I Test (mm) | |||
| >8 ≤8 | 77 (34.4%) 141 (65.6%) | 54 (24.7%) 165 (75.3%) | 0.015 * |
| Schirmer’s I Test (mm) | |||
| >8 ≤8 (max. 25 mm) | 67 141 (67.8%) | 47 165 (77.8%) | 0.021 * |
| Tear Break-up Time (seconds) | |||
| ≥5 <5 | 18 200 (91.7%) | 17 202 (92.2%) | 0.794 |
| Meibum character Liquid Viscous or not expressible | 151 61 (28.8%) | 160 54 (25.2%) | 0.411 |
| Follicle grade Superior | |||
| 0 1 2 | 134 60 (27.9%) 21 (9.77%) | 120 73 (34.0%) 22 (10.2%) | 0.427 |
| Inferior | |||
| 0 1 2 | 153 41 (19.1%) 21 (9.78%) | 146 50 (23.0%) 21 (9.68%) | 0.786 |
| Parameters | Model 1 † Odds Ratio (95% Confidence Interval) | Model 2 †† Odds Ratio (95% Confidence Interval) | Model 3 ††† Odds Ratio (95% Confidence Interval) |
|---|---|---|---|
| Cataract surgery status | 1.65 (1.13, 2.42) * | 1.69 (1.15, 2.48) * | 1.66 (1.13, 2.44) * |
| Schirmer’s grade | 1.21 (0.794, 1.84) | 1.18 (0.774, 1.81) | |
| Gender | 1.02 (0.650, 1.63) | ||
| Age | 1.02 (0.983, 1.04) |
| Parameters | Model 1 † Odds Ratio (95% Confidence Interval) | Model 2 †† Odds Ratio (95% Confidence Interval) | Model 3 ††† Odds Ratio (95% Confidence Interval) |
|---|---|---|---|
| Cataract surgery status | 0.625 (0.414, 0.944) * | 0.614 (0.405, 0.931) * | 0.605 (0.398, 0.921) * |
| Blurring grade | 1.16 (0.764, 1.76) | 1.14 (0.744, 1.73) | |
| Gender | 1.47 (0.910, 2.37) | ||
| Age | 1.03 (1.00, 1.06) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siew, L.; Tong, L. The Effect of Past Cataract Surgery within the Medium to Long-Term Period on Patients with Dry Eye Disease. J. Clin. Med. 2022, 11, 972. https://doi.org/10.3390/jcm11040972
Siew L, Tong L. The Effect of Past Cataract Surgery within the Medium to Long-Term Period on Patients with Dry Eye Disease. Journal of Clinical Medicine. 2022; 11(4):972. https://doi.org/10.3390/jcm11040972
Chicago/Turabian StyleSiew, Lei, and Louis Tong. 2022. "The Effect of Past Cataract Surgery within the Medium to Long-Term Period on Patients with Dry Eye Disease" Journal of Clinical Medicine 11, no. 4: 972. https://doi.org/10.3390/jcm11040972
APA StyleSiew, L., & Tong, L. (2022). The Effect of Past Cataract Surgery within the Medium to Long-Term Period on Patients with Dry Eye Disease. Journal of Clinical Medicine, 11(4), 972. https://doi.org/10.3390/jcm11040972






