Dissemination of Chest Compression-Only Cardiopulmonary Resuscitation by Bystanders for Out-of-Hospital Cardiac Arrest in Students: A Nationwide Investigation in Japan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design of SPIRITS
2.2. Study Subjects
2.3. Data Collection and Outcome Measures
2.4. Statistical Analysis
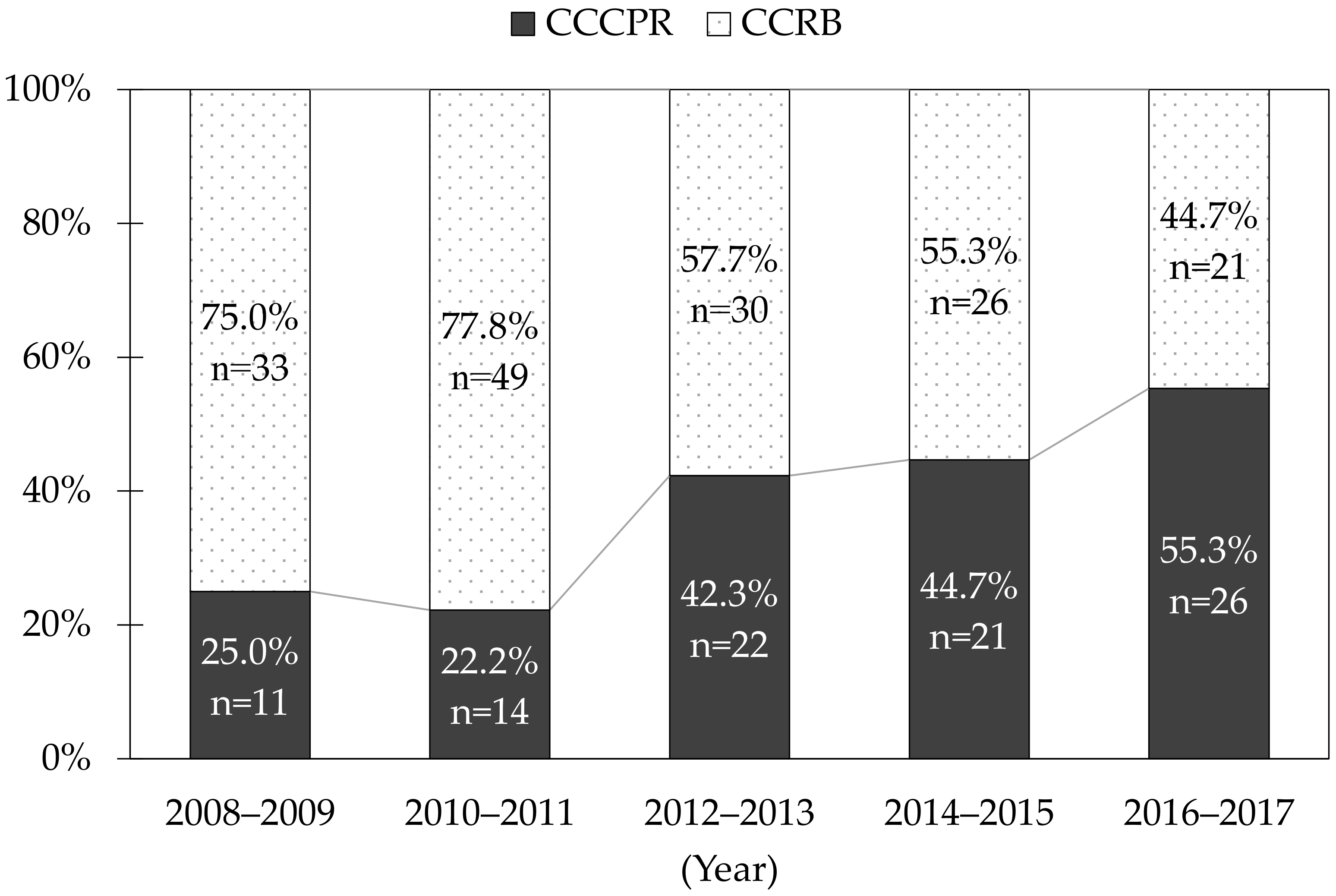
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Atkins, D.L.; Berger, S. Improving outcomes from out-of-hospital cardiac arrest in young children and adolescents. Pediatr. Cardiol. 2012, 33, 474–483. [Google Scholar] [CrossRef]
- Hazinski, M.F.; Nolan, J.P.; Aickin, R.; Bhanji, F.; Billi, J.E.; Callaway, C.W.; Castren, M.; de Caen, A.R.; Ferrer, J.M.; Finn, J.C.; et al. Circulation 2015-Part 1: Executive summary: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 2015, 132, S2–S39. [Google Scholar] [CrossRef] [PubMed]
- Nishiyama, C.; Iwami, T.; Kawamura, T.; Ando, M.; Yonemoto, N.; Hiraide, A.; Nonogi, H. Effectiveness of simplified chest compression-only CPR training for the general public: A randomized controlled trial. Resuscitation 2008, 79, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Ringh, M.; Jonsson, M.; Svensson, L.; Herlitz, J.; Claesson, A.; Djärv, T.; Nordberg, P.; Forsberg, S.; Rubertsson, S.; et al. Survival in Out-of-Hospital Cardiac Arrest after Standard Cardiopulmonary Resuscitation or Chest Compressions Only before Arrival of Emergency Medical Services: Nationwide Study during Three Guideline Periods. Circulation 2019, 139, 2600–2609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bobrow, B.J.; Spaite, D.W.; Berg, R.A.; Stolz, U.; Sanders, A.B.; Kern, K.B.; Vadeboncoeur, T.F.; Clark, L.L.; Gallagher, J.V.; Stapczynski, J.S.; et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA 2010, 304, 1447–1454. [Google Scholar] [CrossRef] [Green Version]
- Iwami, T.; Kitamura, T.; Kiyohara, K.; Kawamura, T. Dissemination of chest compression-only cardiopulmonary resuscitation and survival after out-of-hospital cardiac arrest. Circulation 2015, 132, 415–422. [Google Scholar] [CrossRef] [Green Version]
- Kitamura, T.; Kiyohara, K.; Nishiyama, C.; Kiguchi, T.; Kobayashi, D.; Kawamura, T.; Iwami, T. Chest compression-only versus conventional cardiopulmonary resuscitation for bystander-witnessed out-of-hospital cardiac arrest of medical origin: A propensity score-matched cohort from 143,500 patients. Resuscitation 2018, 126, 29–35. [Google Scholar] [CrossRef]
- Ong, M.E.; Ng, F.S.; Anushia, P.; Tham, L.P.; Leong, B.S.; Ong, V.Y.; Tiah, L.; Lim, S.H.; Anantharaman, V. Comparison of chest compression only and standard cardiopulmonary resuscitation for out-of-hospital cardiac arrest in Singapore. Resuscitation 2008, 78, 119–126. [Google Scholar] [CrossRef]
- Rea, T.D.; Fahrenbruch, C.; Culley, L.; Donohoe, R.T.; Hambly, C.; Innes, J.; Bloomingdale, M.; Subido, C.; Romines, S.; Eisenberg, M.S. CPR with chest compression alone or with rescue breathing. N. Engl. J. Med. 2010, 363, 423–433. [Google Scholar] [CrossRef] [Green Version]
- Svensson, L.; Bohm, K.; Castrèn, M.; Pettersson, H.; Engerström, L.; Herlitz, J.; Rosenqvist, M. Compression-only CPR or standard CPR in out-of-hospital cardiac arrest. N. Engl. J. Med. 2010, 363, 434–442. [Google Scholar] [CrossRef] [Green Version]
- Javaudin, F.; Raiffort, J.; Desce, N.; Baert, V.; Hubert, H.; Montassier, E.; Le Cornec, C.; Lascarrou, J.B.; Le Bastard, Q.; GR-RéAC. Neurological Outcome of Chest Compression-Only Bystander CPR in Asphyxial and Non-Asphyxial Out-Of-Hospital Cardiac Arrest: An Observational Study. Prehosp. Emerg. Care 2021, 25, 812–821. [Google Scholar] [CrossRef]
- Zhan, L.; Yang, L.J.; Huang, Y.; He, Q.; Liu, G.J. Continuous chest compression versus interrupted chest compression for cardiopulmonary resuscitation of non-asphyxial out-of-hospital cardiac arrest. Cochrane Database Syst. Rev. 2017, 3, CD010134. [Google Scholar] [CrossRef]
- Bielski, K.; Smereka, J.; Chmielewski, J.; Pruc, M.; Chirico, F.; Gasecka, A.; Litvinova, N.; Jaguszewski, M.J.; Nowak-Starz, G.; Rafique, Z.; et al. Meta-analysis of chest compression-only versus conventional cardiopulmonary resuscitation by bystanders for adult with out-of-hospital cardiac arrest. Cardiol. J. 2021. [Google Scholar] [CrossRef]
- Naim, M.Y.; Griffis, H.M.; Berg, R.A.; Bradley, R.N.; Burke, R.V.; Markenson, D.; McNally, B.F.; Nadkarni, V.M.; Song, L.; Vellano, K.; et al. Compression-only versus rescue-breathing cardiopulmonary resuscitation after pediatric out-of-hospital cardiac arrest. J. Am. Coll. Cardiol. 2021, 78, 1042–1052. [Google Scholar] [CrossRef]
- Kitamura, T.; Iwami, T.; Kawamura, T.; Nagao, K.; Tanaka, H.; Nadkarni, V.M.; Berg, R.A.; Hiraide, A. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: A prospective, nationwide, population-based cohort study. Lancet 2010, 375, 1347–1354. [Google Scholar] [CrossRef] [Green Version]
- Goto, Y.; Funada, A.; Goto, Y. Conventional versus chest-compression-only cardiopulmonary resuscitation by bystanders for children with out-of-hospital cardiac arrest. Resuscitation 2018, 122, 126–134. [Google Scholar] [CrossRef]
- Young, K.D.; Gausche-Hill, M.; McClung, C.D.; Lewis, R.J. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics 2004, 114, 157–164. [Google Scholar] [CrossRef]
- Fukuda, T.; Ohashi-Fukuda, N.; Kobayashi, H.; Gunshin, M.; Sera, T.; Kondo, Y.; Yahagi, N. Conventional versus compression-only versus no-bystander cardiopulmonary resuscitation for pediatric out-of-hospital cardiac arrest. Circulation 2016, 134, 2060–2070. [Google Scholar] [CrossRef]
- Nitta, M.; Iwami, T.; Kitamura, T.; Nadkarni, V.M.; Berg, R.A.; Shimizu, N.; Ohta, K.; Nishiuchi, T.; Hayashi, Y.; Hiraide, A.; et al. Utstein Osaka Project. Age-specific differences in outcomes after out-of-hospital cardiac arrests. Pediatrics 2011, 128, e812–e820. [Google Scholar] [CrossRef] [Green Version]
- Mitamura, H.; Iwami, T.; Mitani, Y.; Takeda, S.; Takatsuki, S. Aiming for zero deaths: Prevention of sudden cardiac death in schools-statement from the AED Committee of the Japanese Circulation Society. Circ. J. 2015, 79, 1398–1401. [Google Scholar] [CrossRef] [Green Version]
- Matsui, S.; Kitamura, T.; Sado, J.; Kiyohara, K.; Kobayashi, D.; Kiguchi, T.; Nishiyama, C.; Okabayashi, S.; Shimamoto, T.; Matsuyama, T.; et al. Location of arrest and survival from out-of-hospital cardiac arrest among children in the public-access defibrillation era in Japan. Resuscitation 2019, 140, 150–158. [Google Scholar] [CrossRef]
- Ministry of Education, Culture, Sports, Science and Technology. Elementary and Secondary Education Bureau. Elementary and Secondary Education Planning Division. Available online: http://www.mext.go.jp/component/a_menu/education/detail/__icsFiles/afieldfile/2017/03/24/1289307_12.pdf (accessed on 10 December 2021).
- Kiyohara, K.; Sado, J.; Kitamura, T.; Ayusawa, M.; Nitta, M.; Iwami, T.; Nakata, K.; Sato, Y.; Kojimahara, N.; Yamaguchi, N.; et al. Epidemiology of pediatric out-of-hospital cardiac arrest at school- an investigation of a nationwide registry in Japan. Circ. J. 2018, 82, 1026–1032. [Google Scholar] [CrossRef] [Green Version]
- Kiyohara, K.; Kitamura, T.; Ayusawa, M.; Nitta, M.; Iwami, T.; Nakata, K.; Matsui, S.; Sobue, T.; Kitamura, Y.; SPIRITS investigators. Incidence, characteristics, and outcomes of pediatric out-of-hospital cardiac arrest in nursery schools and kindergartens in Japan. J. Cardiol. 2020, 76, 549–556. [Google Scholar] [CrossRef]
- Kiyohara, K.; Sado, J.; Kitamura, T.; Ayusawa, M.; Nitta, M.; Iwami, T.; Nakata, K.; Sobue, T.; Kitamura, Y. Public-access automated external defibrillation and bystander-initiated cardiopulmonary resuscitation in schools: A nationwide investigation in Japan. Europace 2019, 21, 451–458. [Google Scholar] [CrossRef]
- Japan Sport Council. School Safety Departament. Available online: https://www.jpnsport.go.jp/anzen/anzen_school/toukei/tabid/80/Default.aspx (accessed on 10 December 2021).
- Jacobs, I.; Nadkarni, V.; Bahr, J.; Berg, R.A.; Billi, J.E.; Bossaert, L.; Cassan, P.; Coovadia, A.; D’Este, K.; Finn, J.; et al. International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update and simplification of the Utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 2004, 110, 3385–3397. [Google Scholar] [CrossRef]
- Cummins, R.O.; Chamberlain, D.A.; Abramson, N.S.; Allen, M.; Baskett, P.J.; Becker, L.; Bossaert, L.; Delooz, H.H.; Dick, W.F.; Eisenberg, M.S.; et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: The Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation 1991, 84, 960–975. [Google Scholar] [CrossRef] [Green Version]
- Bardai, A.; Berdowski, J.; van der Werf, C.; Blom, M.T.; Ceelen, M.; van Langen, I.M.; Tijssen, J.G.; Wilde, A.A.; Koster, R.W.; Tan, H.L. Incidence, causes, and outcomes of out-of-hospital cardiac arrest in children. A comprehensive, prospective, population-based study in the Netherlands. J. Am. Coll. Cardiol. 2011, 57, 1822–1828. [Google Scholar] [CrossRef] [Green Version]
- Japan Resuscitation Council. JRC Resuscitation Guideline 2020. Pediatric Life Support. Available online: https://www.japanresuscitationcouncil.org/wp-content/uploads/2021/03/PLS%E3%82%AA%E3%83%B3%E3%83%A9%E3%82%A4%E3%83%B3%E7%89%88ver1.4.pdf (accessed on 10 December 2021).
- Japan Resuscitation Council. JRC Resuscitation Guideline 2010. Education, Implementation, and Teams. Available online: https://minds.jcqhc.or.jp/docs/minds/Res/Ch.7_EIT.pdf (accessed on 10 December 2021).
- Nord, A.; Svensson, L.; Karlsson, T.; Claesson, A.; Herlitz, J.; Nilsson, L. Increased survival from out-of-hospital cardiac arrest when off duty medically educated personnel perform CPR compared with laymen. Resuscitation 2017, 120, 88–94. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Labour and Welfare. Vital Statistics of Japan. Available online: http://www.e-stat.go.jp/SG1/estat/List.do?lid=000001138000 (accessed on 10 December 2021).
- Anderson, B.R.; Vetter, V.L. Return to play? Practical considerations for young athletes with cardiovascular disease. Br. J. Sports Med. 2009, 43, 690–695. [Google Scholar] [CrossRef]
- Campbell, R.M.; Berger, S.; Drezner, J. Sudden cardiac arrest in children and young athletes: The importance of a detailed personal and family history in the pre-participation evaluation. Br. J. Sports Med. 2009, 43, 336–341. [Google Scholar] [CrossRef]
- Liberthson, R.R. Sudden death from cardiac causes in children and young adults. N. Engl. J. Med. 1996, 334, 1039–1044. [Google Scholar] [CrossRef] [PubMed]
- Section on Cardiology and Cardiac Surgery. Pediatric sudden cardiac arrest. Pediatrics 2012, 129, e1094–e1102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Topjian, A.A.; Raymond, T.T.; Atkins, D.; Chan, M.; Duff, J.P.; Joyner, B.L., Jr.; Lasa, J.J.; Lavonas, E.J.; Levy, A.; Mahgoub, M.; et al. Pediatric Basic and Advanced Life Support Collaborators. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S469–S523. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Total | Type of Bystander-CPR | p-Value | ||||
|---|---|---|---|---|---|---|---|
| CCCPR | CCRB | ||||||
| n = 253 | n = 94 | n = 159 | |||||
| Patient characteristics | |||||||
| Male | 197 | (77.9%) | 79 | (84.0%) | 118 | (74.2%) | 0.069 |
| Education level | 0.050 | ||||||
| Elementary school (age, years: median 10, range 6–12) | 43 | (17.0%) | 9 | (9.6%) | 34 | (21.4%) | |
| Junior high school (age, years: median 14, range 12–15) | 80 | (31.6%) | 31 | (33.0%) | 49 | (30.8%) | |
| High school/technical college (age, years: median 17, range 15–19) | 130 | (51.4%) | 54 | (57.4%) | 76 | (47.8%) | |
| VF as first documented rhythm | 209 | (82.6%) | 80 | (85.1%) | 129 | (81.1%) | 0.420 |
| Cardiac origin | 228 | (90.1%) | 88 | (93.6%) | 140 | (88.1%) | 0.152 |
| Arrest witnessed by bystanders | 226 | (89.3%) | 85 | (90.4%) | 141 | (88.7%) | 0.664 |
| Situation at the time of arrest | 0.892 | ||||||
| Health and physical education class | 108 | (42.7%) | 41 | (43.6%) | 67 | (42.1%) | |
| Other classes | 25 | (9.9%) | 8 | (8.5%) | 17 | (10.7%) | |
| Athletic club activity | 90 | (35.6%) | 35 | (37.2%) | 55 | (34.6%) | |
| Other situations | 30 | (11.9%) | 10 | (10.6%) | 20 | (12.6%) | |
| Location of arrest | 0.583 | ||||||
| School yard | 139 | (54.9%) | 48 | (51.1%) | 91 | (57.2%) | |
| Gymnasium/Pool | 77 | (30.4%) | 31 | (33.0%) | 46 | (28.9%) | |
| Classroom | 21 | (8.3%) | 10 | (10.6%) | 11 | (6.9%) | |
| Other locations | 16 | (6.3%) | 5 | (5.3%) | 11 | (6.9%) | |
| AED pad application by bystanders | 217 | (85.8%) | 82 | (87.2%) | 135 | (84.9%) | 0.608 |
| Dispatcher instruction | 121 | (47.8%) | 48 | (51.1%) | 73 | (45.9%) | 0.428 |
| Survival outcomes | |||||||
| Prehospital ROSC | 126 | (49.8%) | 53 | (56.4%) | 73 | (45.9%) | 0.107 |
| 30-day survival | 146 | (57.7%) | 57 | (60.6%) | 89 | (56.0%) | 0.468 |
| CPC 1 or 2 | 124 | (49.0%) | 50 | (53.2%) | 74 | (46.5%) | 0.307 |
| Factors | CPC 1 or 2 | Univariable Analysis | Multivariable Analysis | |||
|---|---|---|---|---|---|---|
| n/N | (%) | Crude OR | (95% CI) | Adjusted OR | (95% CI) | |
| Type of bystander-CPR | ||||||
| CCCPR | 50/94 | (53.2%) | 1.31 | (0.78–2.18) | 1.23 | (0.67–2.28) |
| CCRB | 74/159 | (46.5%) | ref. | ref. | ||
| Sex | ||||||
| Male | 103/197 | (52.3%) | 1.83 | (0.99–3.36) | 0.96 | (0.41–2.25) |
| Female | 21/56 | (37.5%) | ref. | ref. | ||
| Education level | ||||||
| Elementary school | 12/43 | (27.9%) | 0.38 | (0.18–0.80) | 1.08 | (0.33–3.46) |
| Junior high school | 46/80 | (57.5%) | 1.31 | (0.75–2.30) | 1.26 | (0.66–2.42) |
| High school/technical college | 66/130 | (50.8%) | ref. | ref. | ||
| First documented rhythm | ||||||
| VF | 121/209 | (57.9%) | 18.79 | (5.64–62.64) | 10.67 | (2.57–44.33) |
| Non-VF | 3/44 | (6.8%) | ref. | ref. | ||
| Origin of arrest | ||||||
| Cardiac origin | 121/228 | (53.1%) | 8.29 | (2.41–28.49) | 1.19 | (0.20–7.27) |
| Non-cardiac origin | 3/25 | (12.0%) | ref. | ref. | ||
| Witness of arrest | ||||||
| Witnessed by bystanders | 115/226 | (50.9%) | 2.07 | (0.89–4.81) | 1.61 | (0.51–5.10) |
| Not witnessed | 9/27 | (33.3%) | ref. | ref. | ||
| Situation at the time of arrest | ||||||
| Health and physical education class | 70/108 | (64.8%) | ref. | ref. | ||
| Other classes | 3/25 | (12.0%) | 0.07 | (0.02–0.26) | 0.21 | (0.04–1.03) |
| Athletic club activity | 46/90 | (51.1%) | 0.57 | (0.32–1.01) | 0.48 | (0.25–0.93) |
| Other situations | 5/30 | (16.7%) | 0.11 | (0.04–0.31) | 0.33 | (0.09–1.19) |
| Location of arrest | ||||||
| School yard | 73/139 | (52.5%) | ref. | ref. | ||
| Gymnasium/pool | 48/77 | (62.3%) | 1.50 | (0.85–2.64) | 1.70 | (0.86–3.33) |
| Classroom | 1/21 | (4.8%) | 0.05 | (0.01–0.35) | 0.22 | (0.02–2.36) |
| Other locations | 2/16 | (12.5%) | 0.13 | (0.03–0.59) | 0.32 | (0.05–1.93) |
| AED pad application by bystanders | ||||||
| Yes | 116/217 | (53.5%) | 4.02 | (1.75–9.22) | 3.32 | (1.24–8.86) |
| No | 8/36 | (22.2%) | ref. | ref. | ||
| Dispatcher instruction | ||||||
| Yes | 62/121 | (51.2%) | 1.19 | (0.72–1.94) | 1.38 | (0.76–2.50) |
| No | 62/132 | (47.0%) | ref. | ref. | ||
| Type of Bystander-CPR | Prehospital ROSC | 30-Day Survival | CPC 1 or 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n/N | (%) | p-Value | n/N | (%) | p-Value | n/N | (%) | p-Value | |||
| First documented rhythm | VF | CCCPR | 53/80 | (66.3%) | 0.054 | 57/80 | (71.3%) | 0.140 | 50/80 | (62.5%) | 0.288 |
| CCRB | 68/129 | (52.7%) | 79/129 | (61.2%) | 71/129 | (55.0%) | |||||
| Non-VF | CCCPR | 0/14 | (0.0%) | 0.105 | 0/14 | (0.0%) | 0.014 | 0/14 | (0.0%) | 0.220 | |
| CCRB | 5/30 | (16.7%) | 10/30 | (33.3%) | 3/30 | (10.0%) | |||||
| Origin Of arrest | Cardiac origin | CCCPR | 51/88 | (58.0%) | 0.202 | 56/88 | (63.6%) | 0.386 | 49/88 | (55.7%) | 0.531 |
| CCRB | 69/140 | (49.3%) | 81/140 | (57.9%) | 72/140 | (51.4%) | |||||
| Non-cardiac origin | CCCPR | 2/6 | (33.3%) | 0.539 | 1/6 | (16.7%) | 0.258 | 1/6 | (16.7%) | 0.687 | |
| CCRB | 4/19 | (21.1%) | 8/19 | (42.1%) | 2/19 | (10.5%) | |||||
| Witness of arrest | Witnessed by bystanders | CCCPR | 52/85 | (61.2%) | 0.028 | 54/85 | (63.5%) | 0.314 | 48/85 | (56.5%) | 0.192 |
| CCRB | 65/141 | (46.1%) | 80/141 | (56.7%) | 67/141 | (47.5%) | |||||
| Not witnessed | CCCPR | 1/9 | (11.1%) | 0.083 | 3/9 | (33.3%) | 0.411 | 2/9 | (22.2%) | 0.386 | |
| CCRB | 8/18 | (44.4%) | 9/18 | (50.0%) | 7/18 | (38.9%) | |||||
| Education level | Elementary school | CCCPR | 5/9 | (55.6%) | 0.269 | 5/9 | (55.6%) | 0.440 | 4/9 | (44.4%) | 0.214 |
| CCRB | 12/34 | (35.3%) | 14/34 | (41.2%) | 8/34 | (23.5%) | |||||
| Junior high school | CCCPR | 18/31 | (58.1%) | 0.428 | 19/31 | (61.3%) | 0.580 | 17/31 | (54.8%) | 0.702 | |
| CCRB | 24/49 | (49.0%) | 33/49 | (67.3%) | 29/49 | (59.2%) | |||||
| High school/ Technical college | CCCPR | 30/54 | (55.6%) | 0.440 | 33/54 | (61.1%) | 0.506 | 29/54 | (53.7%) | 0.573 | |
| CCRB | 37/76 | (48.7%) | 42/76 | (55.3%) | 37/76 | (48.7%) | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kiyohara, K.; Kitamura, Y.; Ayusawa, M.; Nitta, M.; Iwami, T.; Nakata, K.; Sobue, T.; Kitamura, T. Dissemination of Chest Compression-Only Cardiopulmonary Resuscitation by Bystanders for Out-of-Hospital Cardiac Arrest in Students: A Nationwide Investigation in Japan. J. Clin. Med. 2022, 11, 928. https://doi.org/10.3390/jcm11040928
Kiyohara K, Kitamura Y, Ayusawa M, Nitta M, Iwami T, Nakata K, Sobue T, Kitamura T. Dissemination of Chest Compression-Only Cardiopulmonary Resuscitation by Bystanders for Out-of-Hospital Cardiac Arrest in Students: A Nationwide Investigation in Japan. Journal of Clinical Medicine. 2022; 11(4):928. https://doi.org/10.3390/jcm11040928
Chicago/Turabian StyleKiyohara, Kosuke, Yuri Kitamura, Mamoru Ayusawa, Masahiko Nitta, Taku Iwami, Ken Nakata, Tomotaka Sobue, and Tetsuhisa Kitamura. 2022. "Dissemination of Chest Compression-Only Cardiopulmonary Resuscitation by Bystanders for Out-of-Hospital Cardiac Arrest in Students: A Nationwide Investigation in Japan" Journal of Clinical Medicine 11, no. 4: 928. https://doi.org/10.3390/jcm11040928
APA StyleKiyohara, K., Kitamura, Y., Ayusawa, M., Nitta, M., Iwami, T., Nakata, K., Sobue, T., & Kitamura, T. (2022). Dissemination of Chest Compression-Only Cardiopulmonary Resuscitation by Bystanders for Out-of-Hospital Cardiac Arrest in Students: A Nationwide Investigation in Japan. Journal of Clinical Medicine, 11(4), 928. https://doi.org/10.3390/jcm11040928







