Abstract
Elderly patients (over age 85) are increasingly treated in Intensive Care Units (ICU), despite doctors’ reluctance to accept these frail patients. There are only few studies describing the relevance of treatments for this group of patients in ICU. One of these studies defined an age of 85 or over as the essential admittance criterion. Exclusion criteriwere low autonomy before admittance or an inability to answer the phone. Epidemiological data, history, lifestyle, and autonomy (ADL score of six items) were recorded during admission to the ICU and by phone interviews six months later. Eight French ICUs included 239 patients aged over 85. The most common diagnostics were non-cardiogenic lung disease (36%), severe sepsis/septic shock (29%), and acute pulmonary oedem (28%). Twenty-three percent of patients were dependent at the time of their admission. Seventy-one percent of patients were still alive when released from ICU, and 52% were still alive after 6 months. Among the patients which were non-dependent before hospitalization, 17% became dependent. The only prognostic criterifound were the SAPS II score on admission and the place of residence before admission (nursing home or family environment had poor prognosis). Although the prognosis of these elderly patients was good after hospitalization in ICU, it should be noted that the population was carefully selected as having few comorbidities or dependence. No triage critericould be suggested.
1. Introduction
Elderly people (aged over 85) represent an increasingly large part of the French population (2.89% in 2014 and 3.11% in 2016 [1]), and the number of elderly patients treated in intensive care units is also increasing as in many other countries [2]. Whether right or wrong, these patients are often considered as frail, having multiple diseases, and being unable to benefit from the intensive care contributions. Even if more and more elderly patients are admitted into our units, there is still great reluctance to accept these patients, although it is unsupported by any evidence. Whether this depends on the units or even the individuals shows that this decision is not based on any rationale [3].
Age is risk factor for intensive care patients [4], but does threshold really exist? This wariness has been reinforced by several studies. One paper [5], in particular, showed catastrophic one-year survival rate (less than 3%) for patients aged over 85 years hospitalized in ICU for hemodynamic failure. Interestingly, the threshold seems to be around the age of 85. This first impression has been confirmed by several recent studies which estimate that patients are even older [6,7].
However, all these studies focus only on survival. Only one recent study [8] estimates the quality of life in one year after ICY stay for patients older than 75. Without any obvious data, many doctors are afraid that these patients will only survive at the cost of significant decrease of their autonomy. This belief is not supported by any studies on patients aged over 75 or 80 years [2,9,10,11]. This age group (75–84) is now well accepted in our units. However, information on elderly patients is missing. For this reason, we conducted study with 6-month follow-up on dependence and survival of the eldest patients.
2. Methods
This multicentric, prospective, observational cohort study included all patients aged 85 or older who were referred to French hospitals (one university hospital and seven non-university hospitals) for ICU treatment from 1 January 2015 to 31 December 2016, followed by an admission to ICU up to six months later. The ethics committee (CPP Ile de France 1) issued positive opinion, as did the National Commission for Information Technology and Freedom (CNIL). According to French laws, an information document related to observation studies and requesting its approval had to be handed to each patient or relatives upon admission to ICU. The inclusion criteriused were patients’ age (85 or older) and admission to the ICU. During triage, no department had protocol or recommendation to assist the physician. The decision to admit the patient was the sole responsibility of the ICU physician. Patients can be admitted into ICU from another department, emergency, or directly from their home after support by the mobile emergency service.
The non-inclusion criteriwere bedridden patients already very dependent before admission to the ICU, patients who did not speak French or have neurological disease (dementia, etc.) or psychiatric disease preventing them from being interviewed after 6-month period, patients having no phone number nor contact information, and those having no social security coverage. The exclusion criteriwere the inability to reach the patient or relative after 6-month period. The main key point was the change of autonomy status before intensive care and six months later. Autonomy was assessed by the ADL (Activities of Daily Living [12]) score of six items (Table 1), validated by the geriatrics department, completed with datprovided by the patient or relative. The result is score of zero to six, and an ADL score of less than three was considered as marker of dependence. The secondary key points were survival and any change of residence location. In addition to the ADL score and the residence location before and six months after admission, datcollected were the main antecedents, the Knaus score [13] that describes baseline health status of the patients, the mode of admission to the ICU, the length of hospitalization, the SAPS II score, the main treatments used, the possible existence of withheld or withdrawn life-sustaining therapy decision (WOLST) [14], and death in the ICU. The phone numbers of the patient or relatives, including those of an attending physician or the nursing home, were recorded. Six months later, we used phone interview to get more information about residence location, autonomy, and their overall health status feelings compared to before their intensive care stay.

Table 1.
ADL Score (Katz and Akpom, [12]).
The optimal sample size was considered as being 157 patients for this purely descriptive study on very large total population, including an error margin of 10% and confidence level of 95%.
Quantitative variables were expressed as the mean (standard deviation) when following Gaussian distribution or median (interquartile range 25–75%) and were compared using the Student T or Mann–Whitney U test, respectively. Factorial analysis was carried out to describe variability. Qualitative variables were expressed as frequencies (95% confidence interval) calculated by angular transformation and were compared using the Chi-square or Fisher’s exact probability test for categorical variables. Datwas tested for normality using the Shapiro-Wilk test. Hazard ratios with 95% CI were used to report the results. The time variable was defined as the number of days from ICU triage. The variables were included in Cox’s regression analysis or logistic regression because all were associated with p < 0.2 on univariate analysis. All tests were two-sided with 5% significance and performed using R software [15] (using tidyverse [16] and epiDisplay [17] packages).
3. Results
The eight centers enrolled total of 245 patients from 1 January 2015 to 31 December 2016 (Figure 1). Three patients were excluded (dementia). Datafter 6 months could not be collected for another 3 patients. Therefore, the usable sample was reduced to 239 cases.
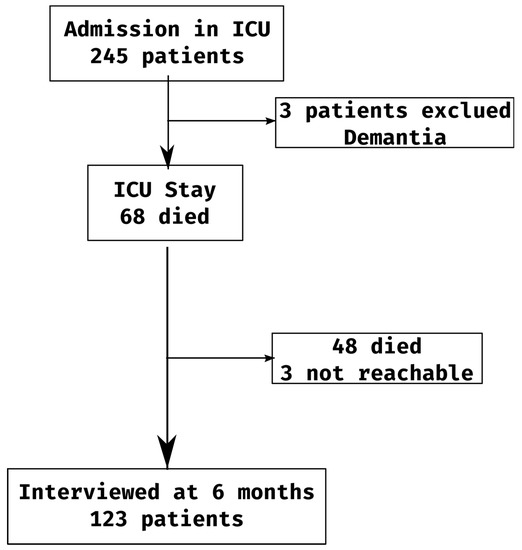
Figure 1.
Flow-chart.
The baseline clinical characteristics of the study population are shown in Table 2. There were various admission diagnostics, but the most frequent were acute non-cardiogenic respiratory failure (36%), severe sepsis/septic shock (29%), and acute pulmonary oedem (28%). total of 51 (21.4%) patients were only hospitalized in continuing care unit (part of the ICU without invasive ventilation, dialysis, or other heavy techniques). total of 214 patients (89%) were not dependent (ADL Score > 2) before hospitalization in the ICU. total of 68 (28.6%) patients died in the ICU. Death in the ICU was linked to the severity at admission time, but not to age, autonomy before admission, length of hospitalization, nor the treatments used.

Table 2.
Summary of the population before and during ICU stay.
4. At Six Months
Total of 123 patients (52.3%) were still alive after six months (Figure 2). In addition to the SAPS II score, the predictive factors (for survival) used were the patients origin and their residence location before hospitalization, the worst case being the nursing home and living with family. Only the score SAPS, the dependence before hospitalization, and neurological disease appear to be related to the dependance (Table 3 and Table 4).

Figure 2.
Survival curve {TC “”3”\1 4}.

Table 3.
Dependency six months after ICU stay: risk factors.

Table 4.
Log-binomial regression modeling risk factors for dependence six month later.
As far as the ADL score, only items 1 (personal care) and 5 (continence) changed (Table 5, Figure 3). Among the 88 patients being non-dependent before intensive care and still living after six months, 15 (16.7% (9.9; 26)) of them became dependent. One question dealt with their overall feeling of the change of their quality of life over these six months. One third of the patients answered that they felt better, one third did not notice any difference, and one third felt worse.

Table 5.
ADL score before ICU state and six months later {TC “”2”\1 4}; n (%).

Figure 3.
Comparison of the ADL score before the stay in ICU versus six months after.
Total of 53 patients (22%) went through decision to withhold or withdraw life-sustaining treatment (WOLST). No advance directives have been found for any patient. These patients were not older, not hospitalized more often, nor had more serious medical history. The ADL score showed greater dependence (26.4% versus 14.1%—p = 0.003) before the admission for patients for whom WOLST decision had been issued. The mortality rate of patients having undergone procedure to withhold or withdraw life-sustaining therapy was 66% (eight were alive at six months) compared to 17.8% for other patients (p < 0.0001). Hospitalization in the ICU was longer. After six months, mortality was 84.9% versus 36.8% (p < 0.0001).
5. Discussion
The results showed significant early mortality rate (40% of deaths after 30 days), but, after six months, the survival rate was close to 50%. Early mortality in the hospital was similar to what was found in other studies based on similar populations, which confirmed the quality of our sample [8,18,19,20]. More importantly, autonomy was preserved: 60% of the patients having maximum ADL score before hospitalization had the same score after six months, and less than 10% became dependent (ADL score < 3).
The assessment of the autonomy status after six months is not an easy task. The ADL score has been chosen because of its simplicity, which is also its limitation. In order to be able to interview patients by phone, simple score had to be retained. The SF36 score [21], for instance, which is much more complete and well validated, would have been unusable by phone. Therefore, this study is limited to patient autonomy and not quality of life, which is much more complex task to define and approach.
The definition of an ICU varies widely from one country to another, as does the profile of admitted patient types and the seriousness of their status, as well as hospital organization, which makes it hard to assimilate published articles.
Understanding the outcome at 6 months of elderly patients following stay in the ICU could guide the physician in deciding upon the admission of patient to the ICU. If age over 85 is not clear prognostic factor, comorbidities and general condition, as vague as this notion may be, are probably more significant elements. The small size of our sample did not allow the definition of patient groups or simple referral criteria. The residence location before hospitalization was statistically linked to survival and autonomy, but, in reality, it cannot be used: patients living with their family can also be perfectly autonomous or very dependent. Patients living in nursing homes were probably over-selected on admission and, therefore, not particularly representative of this population.
The concept of frailness has recently been introduced in studies focused on patients aged 75 to 85 [22] to define class of non-disabled patients but at high risk of degradation after major hospitalization, (intensive care, surgery, etc.) and on mortality. However, no simple index usable in an emergency department has been validated to date, except the frailness score CSH [23]. However, more than 60% of patients aged 85 and above are classified as “frail” [11,24]. Therefore, these indices are not particularly discriminating for this age group. Criteriusually used (e.g., CFS score [25]) are too complex to collect in an emergency department when deciding to admit to the ICU (walking speed, muscle strength, etc.). Nevertheless, this is an interesting concept which could help refine the triage of patients upon admission.
This study does not show any new criterifor the decision to admit an elderly patient to the ICU. In the service, decisions regarding the continuation of care or the level of commitment in these patients could be based in part on the SAPSII score.
6. Conclusions
The positive results in terms of survival rate and autonomy six months after hospitalization in the ICU of patients aged over 85 support an easier admission of these patients. However, these positive results are obtained at the cost of very severe triage, the rules for which still need to be defined.
Author Contributions
P.M.: data retrieval, statistical analysis, writing; B.G.: data retrieval, writing; F.F., S.E., G.P.: data retrieval. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of CPP Ile de France #1 (CHRD0514, 28 October 2014. ClinicalTrials.gov Identifier: NCT02849756.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request from Philippe Michel.
Acknowledgments
This work was carried out with the assistance of the Clinical Research Support Unit of the R. Dubos hospital (Pontoise—France).
Conflicts of Interest
The authors declare no conflict of interest.
References
- INSEE. Série 001641607 Démographie—Population au début du mois—France (Inclus Mayotte Partir de 2014); Insee: Paris, France, 2016. [Google Scholar]
- Bagshaw, S.M.; Webb, S.A.R.; Delaney, A.; George, C.; Pilcher, D.; Hart, G.K.; Bellomo, R. Very old patients admitted to intensive care in Australiand New Zealand:multi-centre cohort analysis. Crit. Care 2009, 13, R45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guidet, B.; De Lange, D.; Christensen, S.; Moreno, R.; Fjølner, J.; Dumas, G.; Flaatten, H. Attitudes of physicians towards the care of critically ill elderly patients—European survey. ACTA Anaesthesiol. Scand. 2017, 62, 207–219. [Google Scholar] [CrossRef]
- Gayat, E.; Cariou, A.; Deye, N.; Vieillard-Baron, A.; Jaber, S.; Damoisel, C.; Lu, Q.; Monnet, X.; Rennuit, I.; Azoulay, E.; et al. Determinants of long-term outcome in ICU survivors: Results from the FROG-ICU study. Crit. Care 2018, 22, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biston, P.; Aldecoa, C.; Devriendt, J.; Madl, C.; Chochrad, D.; Vincent, J.-L.; De Backer, D. Outcome of elderly patients with circulatory failure. Intensiv. Care Med. 2014, 40, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Sprung, C.L.; Artigas, A.; Kesecioglu, J.; Pezzi, A.; Wiis, J.; Pirracchio, R.; Baras, M.; Edbrooke, D.L.; Pesenti, A.; Bakker, J.; et al. The Eldicus prospective, observational study of triage decision making in European intensive care units. Part II: Intensive care benefit for the elderly. Crit. Care Med. 2012, 40, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Khouli, H.; Astua, A.; Dombrowski, W.; Ahmad, F.; Homel, P.; Shapiro, J.; Singh, J.; Nallamothu, R.; Mahbub, H.; Eden, E.; et al. Changes in health-related quality of life and factors predicting long-term outcomes in older adults admitted to intensive care units. Crit. Care Med. 2011, 39, 731–737. [Google Scholar] [CrossRef]
- Demiselle, J.; Duval, G.; Hamel, J.-F.; Renault, A.; Bodet-Contentin, L.; Martin-Lefèvre, L.; Vivier, D.; Villers, D.; Lefèvre, M.; Robert, R.; et al. Determinants of hospital and one-year mortality among older patients admitted to intensive care units: Results from the multicentric SENIOREcohort. Ann. Intensiv. Care 2021, 11, 35. [Google Scholar] [CrossRef]
- Tabah, A.; Philippart, F.; Timsit, J.F.; Willems, V.; Français, A.; Leplège, A.; Carlet, J.; Bruel, C.; Misset, B.; Garrouste-Orgeas, M. Quality of life in patients aged 80 or over after ICU discharge. Crit. Care 2010, 14, R2. [Google Scholar] [CrossRef] [Green Version]
- de Rooij, S.E.; Govers, A.C.; Korevaar, J.C.; Giesbers, A.W.; Levi, M.; de Jonge, E. Cognitive, Functional, and Quality-of-Life Outcomes of Patients Aged 80 and Older Who Survived at Least 1 Year After Planned or Unplanned Surgery or Medical Intensive Care Treatment. J. Am. Geriatr. Soc. 2008, 56, 816–822. [Google Scholar] [CrossRef]
- Flaatten, H.; De Lange, D.W.; Morandi, A.; Andersen, F.H.; Artigas, A.; Bertolini, G.; Boumendil, A.; Cecconi, M.; Christensen, S.; Faraldi, L.; et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥80 years). Intensive Care Med. 2017, 43, 1820–1828. [Google Scholar] [CrossRef]
- Katz, S.; Akpom, C.A. Index of ADL. Med. Care 1976, 14, 116–118. [Google Scholar] [CrossRef]
- Knaus, W.A.; Zimmerman, J.E.; Wagner, D.P.; Draper, E.A.; Lawrence, D.E. APACHE—Acute physiology and chronic health evaluation: Physiologically based classification system. Crit. Care Med. 1981, 9, 591–597. [Google Scholar] [CrossRef]
- Levin, P.D.; Sprung, C.L. End of life decisions in intensive care. Intensive Care Med. 1999, 25, 893–895. [Google Scholar] [CrossRef]
- R Core Team. R: Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Wickham, H. Tidyverse: Easily Install and Load the ‘Tidyverse’. 2017; R package, version 1.2.1. [Google Scholar]
- Chongsuvivatwong, V. epidisplay: Epidemiological DatDisplay Package. 2018; R package, version 3.5.0.1. [Google Scholar]
- Andersen, F.H.; Flaatten, H.; Klepstad, P.; Follestad, T.; Strand, K.; Krüger, A.J.; Hahn, M.; Buskop, C.; Rime, A.K.; Kvåle, R. Long-Term Outcomes After ICU Admission Triage in Octogenarians. Crit. Care Med. 2017, 45, e363–e371. [Google Scholar] [CrossRef] [PubMed]
- Roch, A.; Wiramus, S.; Pauly, V.; Forel, J.-M.; Guervilly, C.; Gainnier, M.; Papazian, L. Long-term outcome in medical patients aged 80 or over following admission to an intensive care unit. Crit. Care 2011, 15, R36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sacanella, E.; Joan Manel Pérez-Castejón, J.M.N.; Masanés, F.; Navarro, M.; Castro, P. New sorting aid tools are emerging from both the adaptations of existing scores and the notion of fragility. Eur. Geriatr. Med. 2011, 15, R105. [Google Scholar]
- Brazier, J.E.; Harper, R.; Jones, N.M.; O’cathain, A.; Thomas, K.J.; Usherwood, T.; Westlake, L. Validating the SF-36 health survey questionnaire: New outcome measure for primary care. Br. Med. J. 1992, 305, 160–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patrizio, E.; Bergamaschini, L.C.; Cesari, M. Developing Frailty Index from routinely collected datin the Emergency Department among of hospitalized patients. Eur. Geriatr. Med. 2019, 10, 727–732. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.W.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. Global clinical measure of fitness and frailty in elderly people. CMAJ 2005, 173, 489–495. [Google Scholar] [CrossRef] [Green Version]
- Fronczek, J.; Polok, K.; de Lange, D.W.; Jung, C.; Beil, M.; Rhodes, A.; Fjalner, J.; Górka, J.; Andersen, F.H.; Artigas, A.; et al. Relationship between the Clinical Frailty Scale and short-term mortality in patients ≥80 years old acutely admitted to the ICU: Prospective cohort study. Crit. Care 2021, 25, 231. [Google Scholar] [CrossRef]
- Le Maguet, P.; Roquilly, A.; Lasocki, S.; Asehnoune, K.; Carise, E.; Martin, M.S.; Mimoz, O.; LE Gac, G.; Somme, D.; Cattenoz, C.; et al. Prevalence and impact of frailty on mortality in elderly ICU patients: Prospective, multicenter, observational study. Intensive Care Med. 2014, 40, 674–682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).