Comparison of the Effect of MFAT and MFAT + PRP on Treatment of Hip Osteoarthritis: An Observational, Intention-to-Treat Study at One Year
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Statistical Methods
2.2.1. Reproducibility of Analysis and Replicability of Results
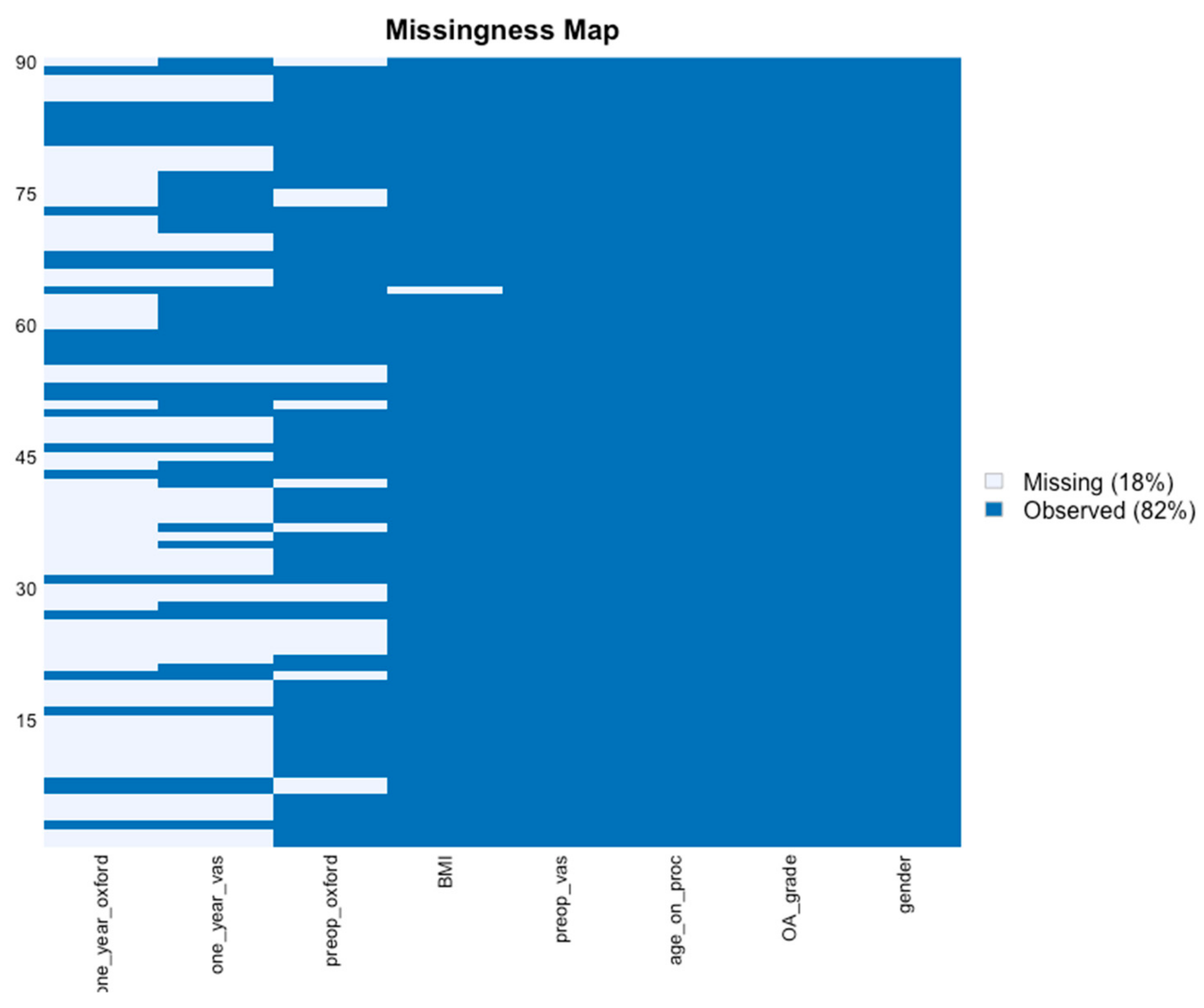
2.2.2. Missing Values
2.2.3. Study Flow Chart
2.3. Patients
2.4. Harvesting Adipose Tissue
2.5. Preparation of PRP
2.6. Injection Protocol
2.7. Responder Classification
3. Results
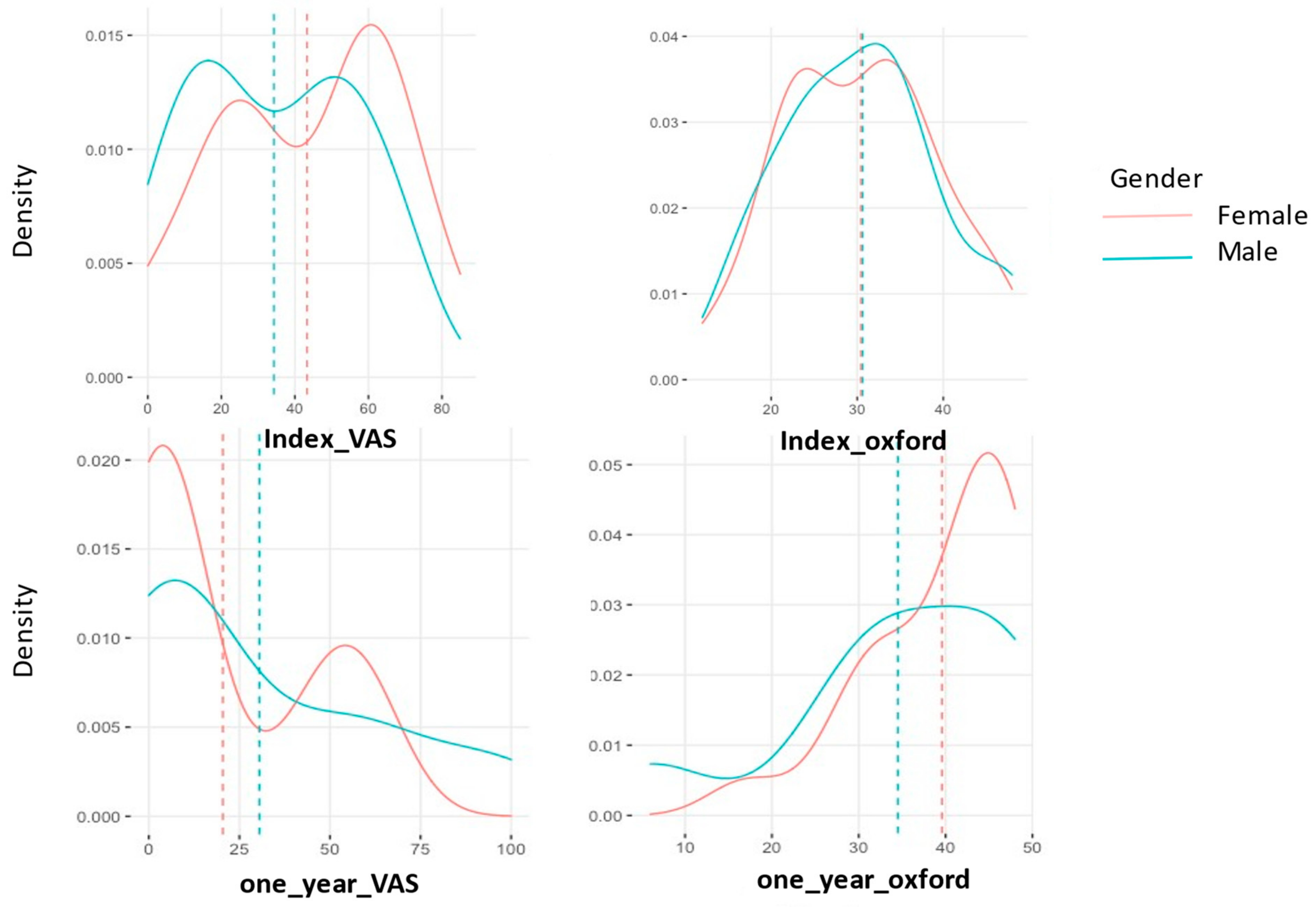
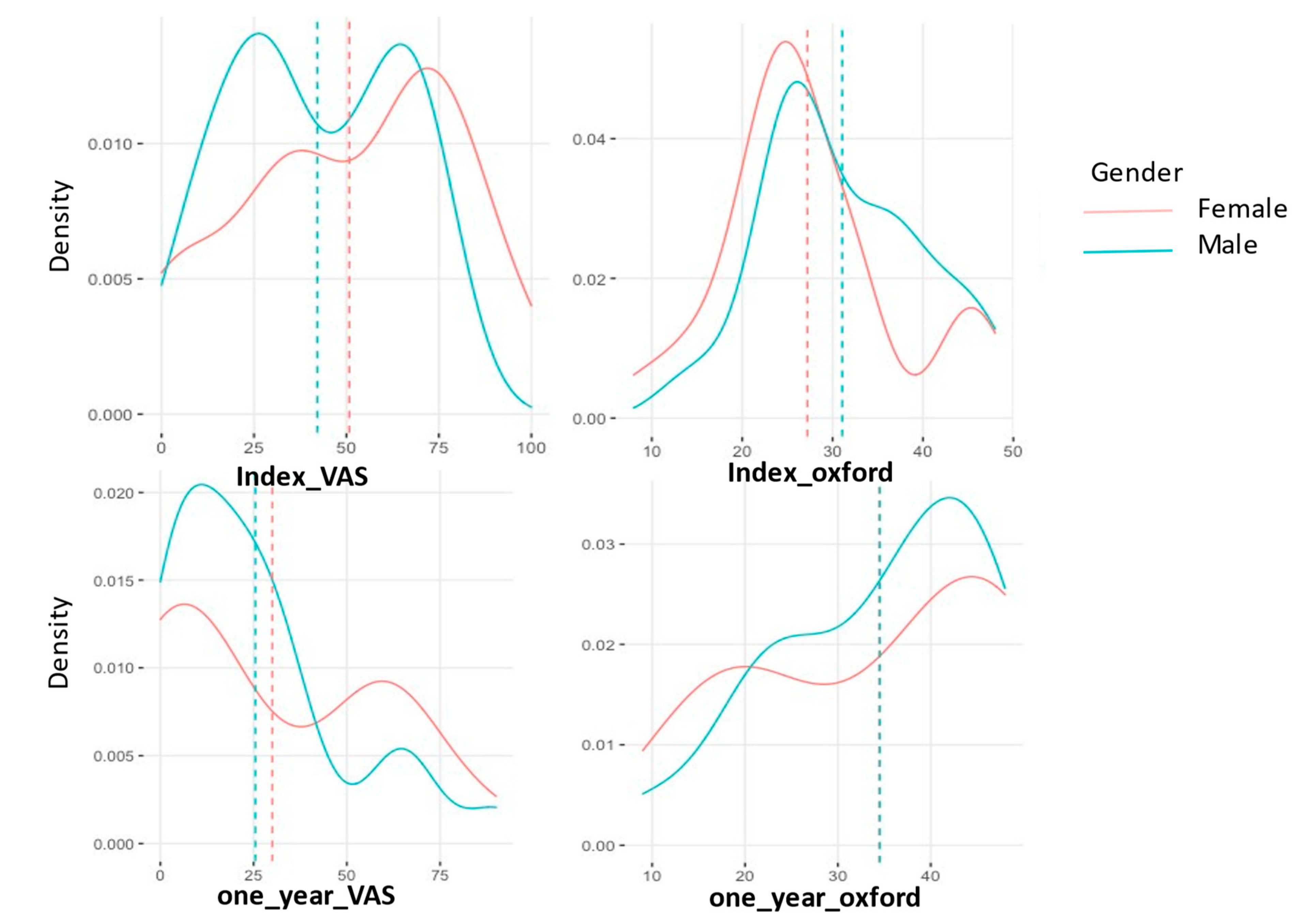
3.1. General Outcomes
3.2. Response to Treatment
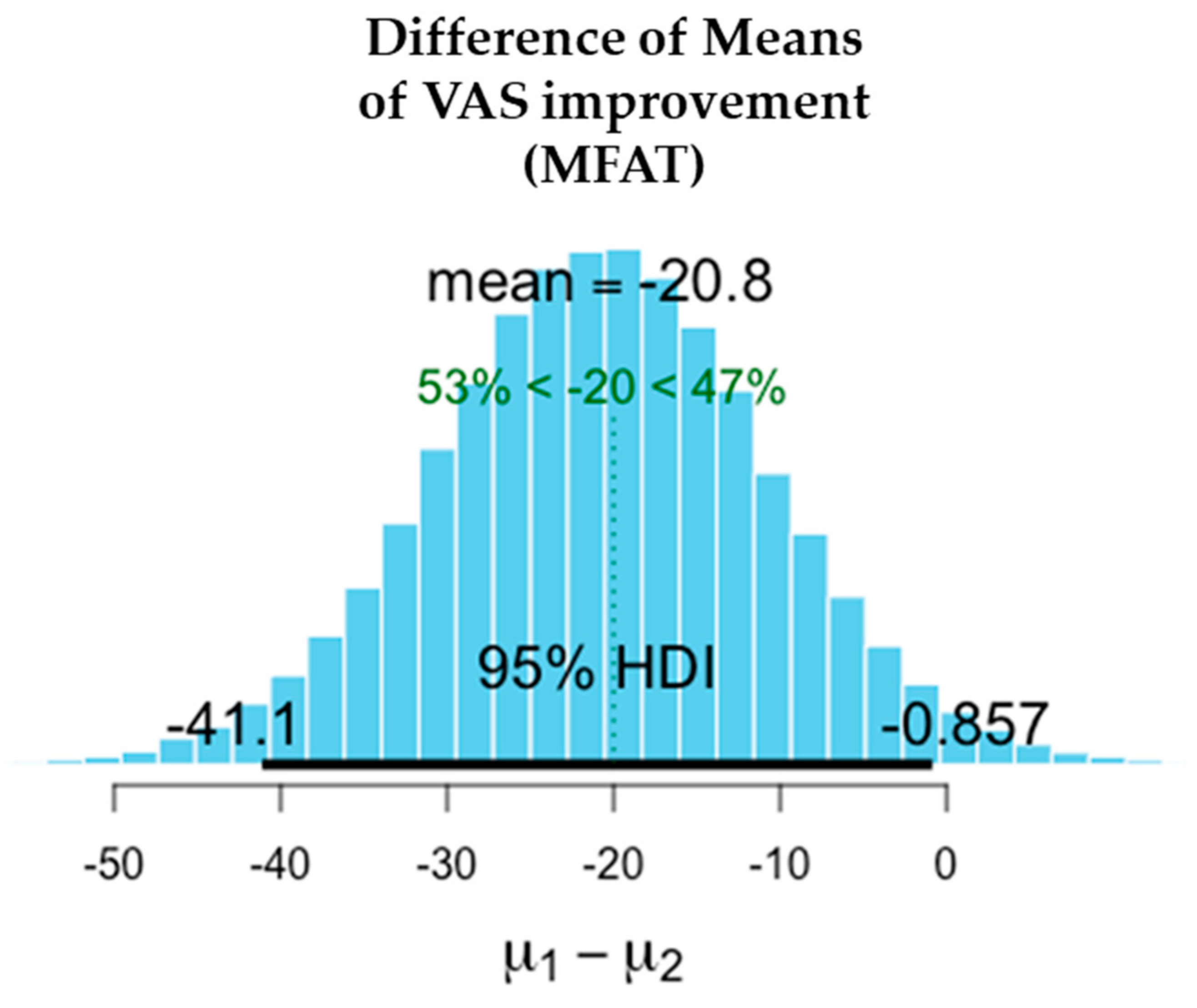
3.2.1. VAS
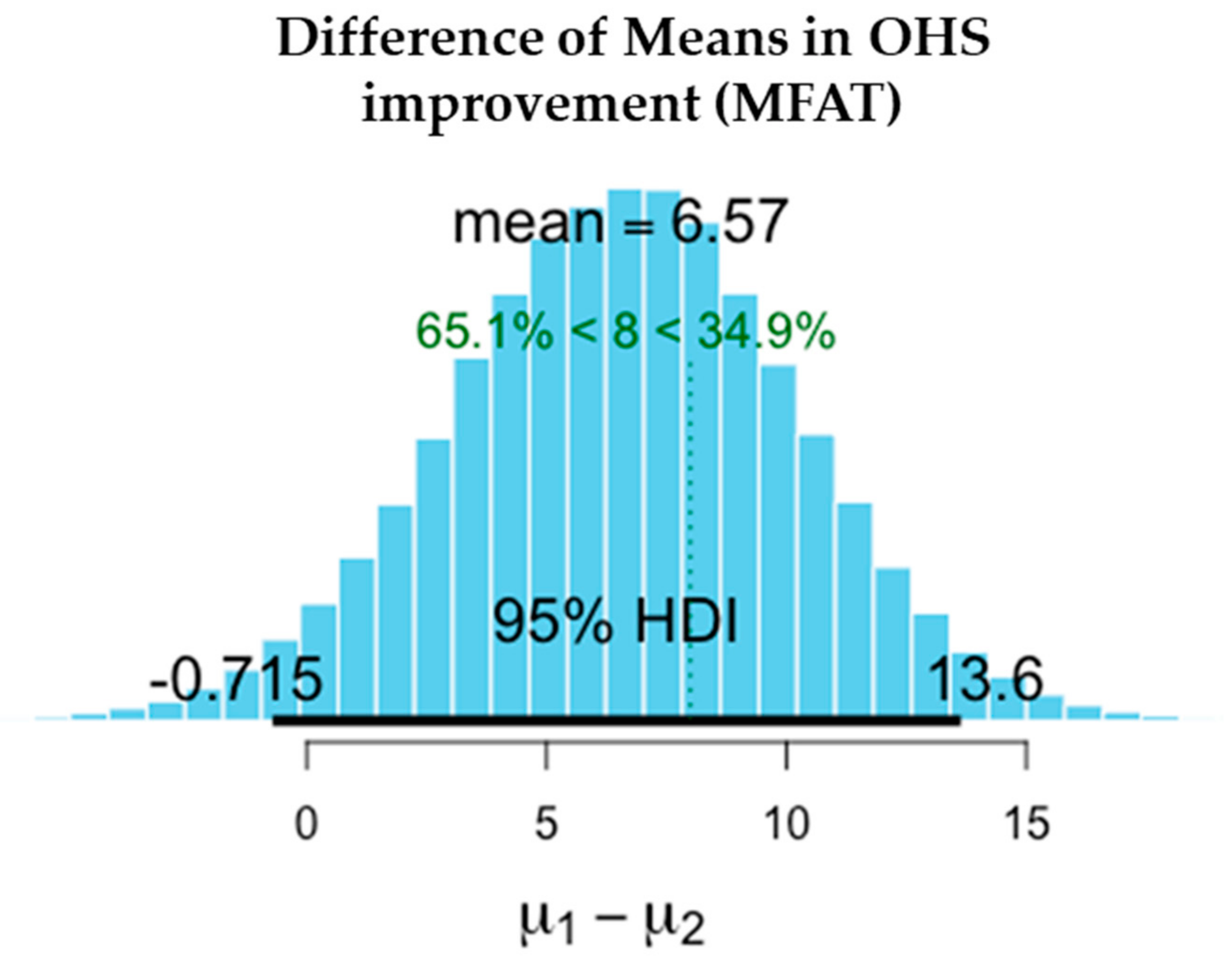
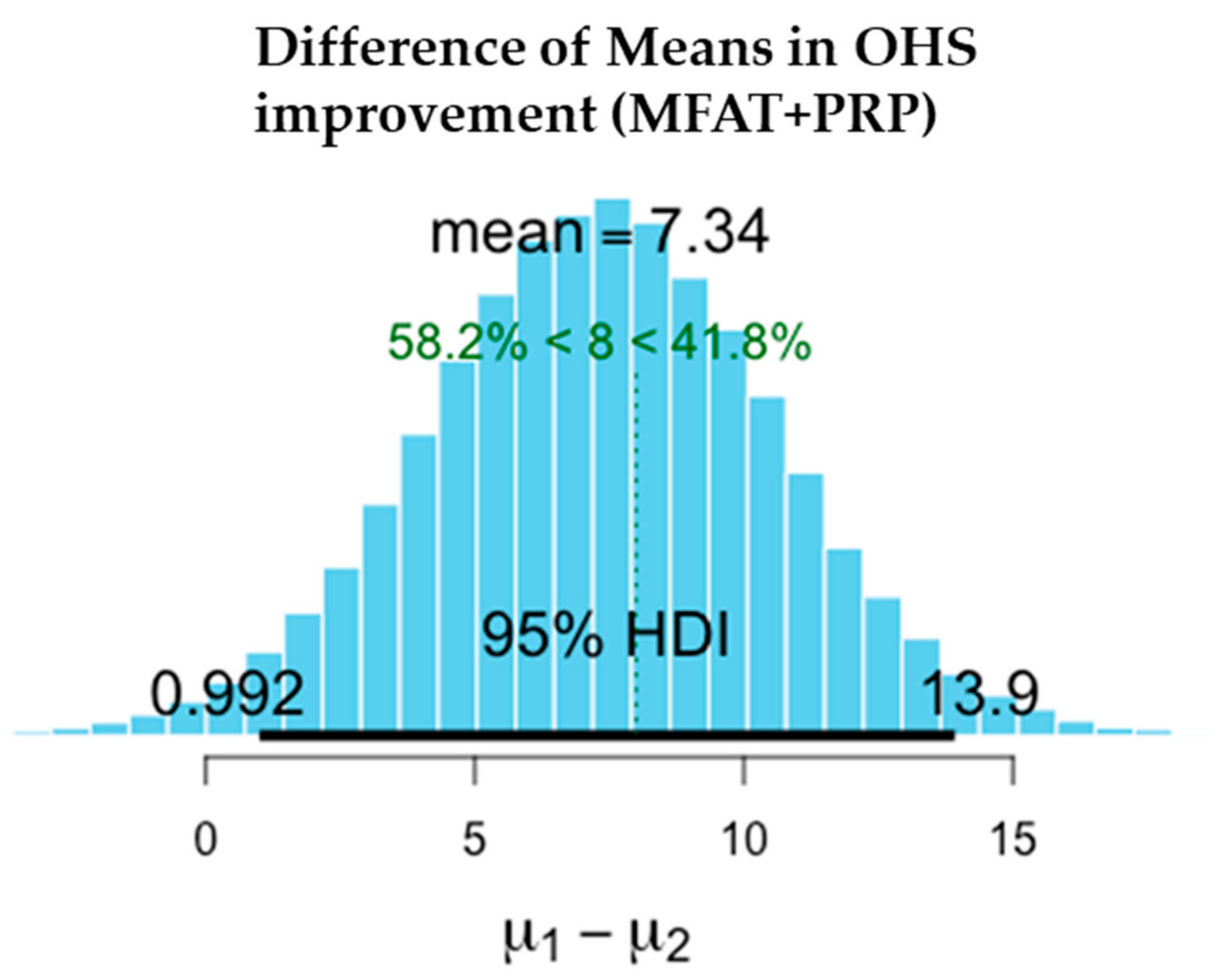
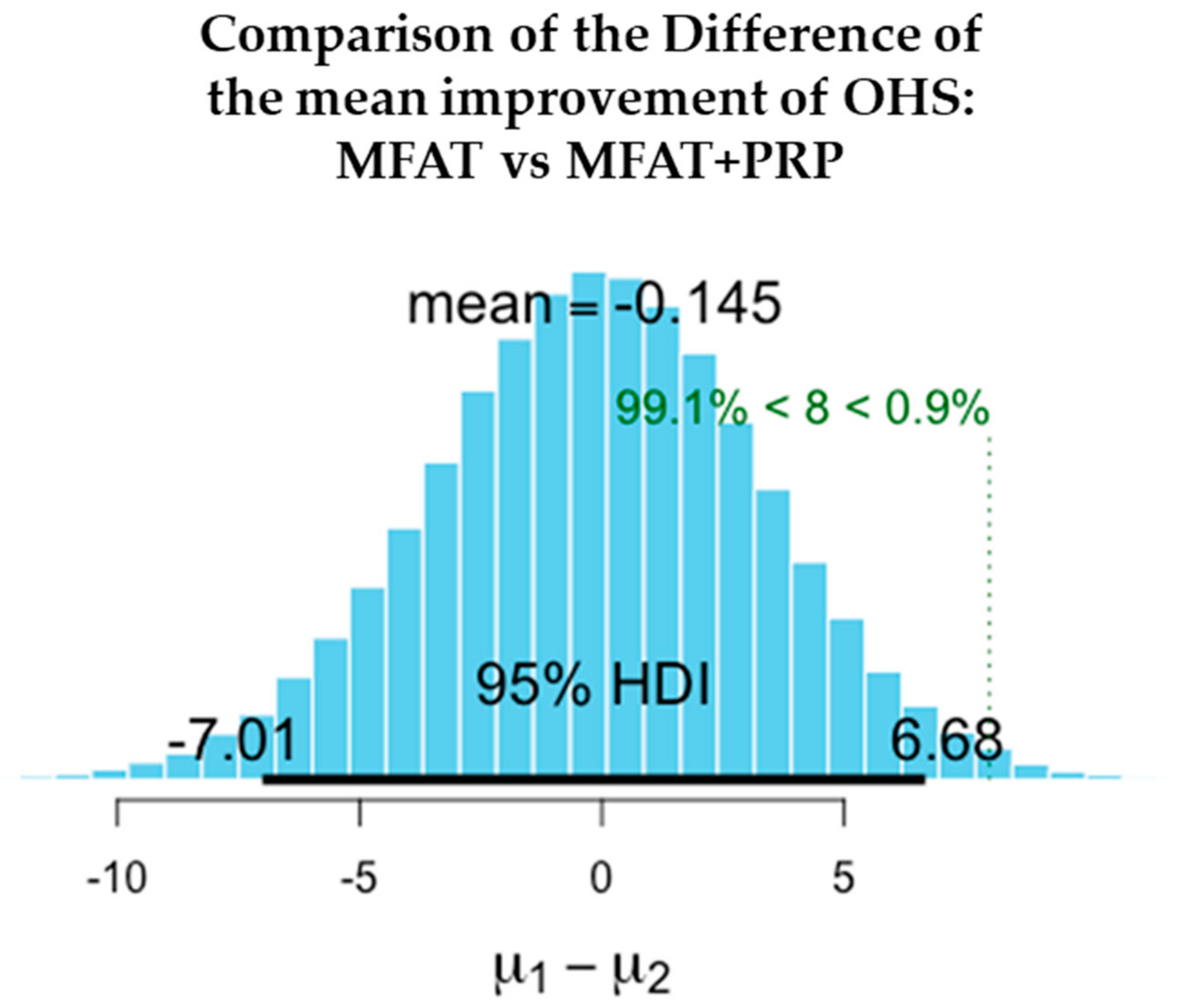
3.2.2. OHS
3.3. Complications
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Murphy, N.J.; Eyles, J.P.; Hunter, D.J. Hip Osteoarthritis: Etiopathogenesis and Implications for Management. Adv. Ther. 2016, 33, 1921–1946. [Google Scholar] [CrossRef] [PubMed]
- National Joint Registry. 17th Annual Report 2020. Available online: https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2017th%20Annual%20Report%202020.pdf (accessed on 14 December 2021).
- Evans, J.T.; Evans, J.P.; Walker, R.W.; Blom, A.W.; Whitehouse, M.R.; Sayers, A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019, 393, 647–654. [Google Scholar] [CrossRef]
- Patel, A.; Pavlou, G.; Mújica-Mota, R.E.; Toms, A.D. The epidemiology of revision total knee and hip arthroplasty in England and Wales: A comparative analysis with projections for the United States. A study using the National Joint Registry dataset. Bone Jt. J. 2015, 97, 1076–1081. [Google Scholar] [CrossRef] [PubMed]
- Runhaar, J.; Özbulut, Ö.; Kloppenburg, M.; Boers, M.; Bijlsma, J.W.J.; Bierma-Zeinstra, S.M.A. Diagnostic criteria for early hip osteoarthritis; first steps, based on the CHECK study. Rheumatology 2021, 60, 5158–5164. [Google Scholar] [CrossRef]
- Rhon, D.I.; Greenlee, T.A.; Sissel, C.D.; Reiman, M.P. The two-year incidence of hip osteoarthritis after arthroscopic hip surgery for femoroacetabular impingement syndrome. BMC Musculoskelet. Disord. 2019, 20, 266. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, D.R.; Chen, J.W.; Lall, A.C.; Kyin, C.; Walker-Santiago, R.; Shapira, J.; Rosinsky, P.J.; Domb, B.G. Microfracture in Hip Arthroscopy. Keep It Simple! Arthrosc. Tech. 2019, 8, e1063–e1067. [Google Scholar] [CrossRef]
- Green, C.J.; Beck, A.; Wood, D.; Zheng, M.H. The biology and clinical evidence of microfracture in hip preservation surgery. J. Hip Preserv. Surg. 2016, 3, 108–123. [Google Scholar] [CrossRef]
- Dallich, A.A.; Rath, E.; Atzmon, R.; Radparvar, J.R.; Fontana, A.; Sharfman, Z.; Amar, E. Chondral lesions in the hip: A review of relevant anatomy, imaging and treatment modalities. J. Hip Preserv. Surg. 2019, 6, 3–15. [Google Scholar] [CrossRef]
- Medina-Porqueres, I.; Ortega-Castillo, M.; Muriel-Garcia, A. Effectiveness of platelet-rich plasma in the management of hip osteoarthritis: A systematic review and meta-analysis. Clin. Rheumatol. 2021, 40, 53–64. [Google Scholar] [CrossRef]
- Gazendam, A.; Ekhtiari, S.; Bozzo, A.; Phillips, M.; Bhandari, M. Intra-articular saline injection is as effective as corticosteroids, platelet-rich plasma and hyaluronic acid for hip osteoarthritis pain: A systematic review and network meta-analysis of randomised controlled trials. Br. J. Sports Med. 2021, 55, 256–261. [Google Scholar] [CrossRef]
- Zhu, C.; Wu, W.; Qu, X. Mesenchymal stem cells in osteoarthritis therapy: A review. Am. J. Transl. Res. 2021, 13, 448–461. [Google Scholar] [PubMed]
- Ivone, A.; Fioruzzi, A.; Jannelli, E.; Castelli, A.; Ghiara, M.; Ferranti Calderoni, E.; Fontana, A. Micro-fragmented Adipose Tissue Transplantation (MATT) for the treatment of acetabular delamination. A two years follow up comparison study with microfractures. Acta Biomed. 2019, 90, 69–75. [Google Scholar]
- Heidari, N.; Noorani, A.; Slevin, M.; Cullen, A.; Stark, L.; Olgiati, S.; Zerbi, A.; Wilson, A. Patient-Centered Outcomes of Microfragmented Adipose Tissue Treatments of Knee Osteoarthritis: An Observational, Intention-to-Treat Study at Twelve Months. Stem. Cells Int. 2020, 2020, 8881405. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef]
- Louis, M.L.; Gravier Dumonceau, R.; Jouve, E.; Cohen, M.; Djouri, R.; Richardet, N.; Jourdan, E.; Giraudo, L.; Dumoulin, C.; Grimaud, F.; et al. Intra Articular Injection Of Autologous Microfat And Platelet-Rich Plasma In The Treatment Of Knee Osteoarthritis: A Double Blind Randomized Comparative Study. Arthroscopy 2021, 37, 3125–3137. [Google Scholar] [CrossRef]
- Zhang, H.F.; Wang, C.G.; Li, H.; Huang, Y.T.; Li, Z.J. Intra-articular platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: A meta-analysis. Drug Des. Dev. Ther. 2018, 12, 445–453. [Google Scholar] [CrossRef]
- Kruschke, J.K. Bayesian estimation supersedes the t test. J. Exp. Psychol. Gen. 2013, 142, 573–603. [Google Scholar] [CrossRef]
- Jokura, Y.; Yano, K.; Watanabe, N.; Yamato, M. Bayesian statistics and clinical trial designs for human cells and tissue products for regulatory approval. Regen. Ther. 2016, 5, 86–95. [Google Scholar] [CrossRef][Green Version]
- Kruschke, J.K. Doing Bayesian Data Analysis: A Tutorial with R, JAGS, and Stan, 2th ed.; Elsevier: Amsterdam, The Netherlands, 2014; pp. 1–759. [Google Scholar]
- Sánchez, M.; Fiz, N.; Azofra, J.; Usabiaga, J.; Aduriz Recalde, E.; Garcia Gutierrez, A.; Albillos, J.; Gárate, R.; Aguirre, J.J.; Padilla, S.; et al. A randomized clinical trial evaluating plasma rich in growth factors (PRGF-Endoret) versus hyaluronic acid in the short-term treatment of symptomatic knee osteoarthritis. Arthroscopy 2012, 28, 1070–1078. [Google Scholar] [CrossRef]
- Anitua, E.; Prado, R.; Nurden, A.T.; Nurden, P. Characterization of Plasma Rich in Growth Factors (PRGF): Components and formulations. In Platelet Rich Plasma in Orthopaedics and Sports Medicine; Anitua, E., Cugat, R., Sánchez, M., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 29–45. [Google Scholar]
- Haefeli, M.; Elfering, A. Pain assessment. Eur. Spine J. 2006, 15 (Suppl. S1), S17–S24. [Google Scholar] [CrossRef]
- Murray, D.W.; Fitzpatrick, R.; Rogers, K.; Pandit, H.; Beard, D.J.; Carr, A.J.; Dawson, J. The use of the Oxford hip and knee scores. J. Bone Jt. Surg. Br. 2007, 89, 1010–1014. [Google Scholar] [CrossRef]
- Harris, K.; Dawson, J.; Gibbons, E.; Lim, C.R.; Beard, D.J.; Fitzpatrick, R.; Price, A.J. Systematic review of measurement properties of patient-reported outcome measures used in patients undergoing hip and knee arthroplasty. Patient Relat. Outcome Meas. 2016, 7, 101–108. [Google Scholar] [CrossRef]
- Danoff, J.R.; Goel, R.; Sutton, R.; Maltenfort, M.G.; Austin, M.S. How Much Pain Is Significant? Defining the Minimal Clinically Important Difference for the Visual Analog Scale for Pain After Total Joint Arthroplasty. J. Arthroplasty 2018, 33, S71–S75.e2. [Google Scholar] [CrossRef]
- Beard, D.J.; Harris, K.; Dawson, J.; Doll, H.; Murray, D.W.; Carr, A.J.; Price, A.J. Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J. Clin. Epidemiol. 2015, 68, 73–79. [Google Scholar] [CrossRef]
- Manktelow, A.R.; Gehrke, T.; Haddad, F.S. Hip surgery—State of the art: Totally Hip 2017: Gothenburg. Bone Jt. J. 2017, 99, 1–2. [Google Scholar] [CrossRef]
- Aiyer, R.; Noori, S.; Schirripa, F.; Schirripa, M.; Aboud, T.; Jain, S.; Gulati, A.; Puttanniah, V.; Gungor, S.; Hunter, C. Treatment of knee osteoarthritic pain with platelet-rich plasma: A systematic review of clinical studies. Pain Manag. 2021, 11, 419–431. [Google Scholar] [CrossRef]
- Alessandri, G.; Pessina, A.; Paroni, R.; Bercich, L.; Paino, F.; Dei Cas, M.; Cadei, M.; Caruso, A.; Schiariti, M.; Restelli, F.; et al. Single-Shot Local Injection of Microfragmented Fat Tissue Loaded with Paclitaxel Induces Potent Growth Inhibition of Hepatocellular Carcinoma in Nude Mice. Cancers 2021, 13, 5505. [Google Scholar] [CrossRef]
- Lopa, S.; Colombini, A.; Moretti, M.; de Girolamo, L. Injective mesenchymal stem cell-based treatments for knee osteoarthritis: From mechanisms of action to current clinical evidences. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2003–2020. [Google Scholar] [CrossRef]
- Schiavone Panni, A.; Vasso, M.; Braile, A.; Toro, G.; De Cicco, A.; Viggiano, D.; Lepore, F. Preliminary results of autologous adipose-derived stem cells in early knee osteoarthritis: Identification of a subpopulation with greater response. Int. Orthop. 2019, 43, 7–13. [Google Scholar] [CrossRef]
- Smith, O.J.; Kanapathy, M.; Khajuria, A.; Prokopenko, M.; Hachach-Haram, N.; Mann, H.; Mosahebi, A. Systematic review of the efficacy of fat grafting and platelet-rich plasma for wound healing. Int. Wound J. 2018, 15, 519–526. [Google Scholar] [CrossRef]
- Kim, S.H.; Park, E.S.; Kim, T.H. Rejuvenation Using Platelet-rich Plasma and Lipofilling for Vaginal Atrophy and Lichen Sclerosus. J. Menopausal. Med. 2017, 23, 63–68. [Google Scholar] [CrossRef]
- Garcia, F.L.; Williams, B.T.; Polce, E.M.; Heller, D.B.; Aman, Z.S.; Nwachukwu, B.U.; Nho, S.J.; Chahla, J. Preparation Methods and Clinical Outcomes of Platelet-Rich Plasma for Intra-articular Hip Disorders: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Orthop. J. Sports Med. 2020, 8, 2325967120960414. [Google Scholar] [CrossRef]
- Kraeutler, M.J.; Houck, D.A.; Garabekyan, T.; Miller, S.L.; Dragoo, J.L.; Mei-Dan, O. Comparing Intra-articular Injections of Leukocyte-Poor Platelet-Rich Plasma Versus Low-Molecular Weight Hyaluronic Acid for the Treatment of Symptomatic Osteoarthritis of the Hip: A Double-Blind, Randomized Pilot Study. Orthop. J. Sports Med. 2021, 9, 2325967120969210. [Google Scholar] [CrossRef]
- Anitua, E.; Sánchez, M.; Nurden, A.T.; Zalduendo, M.M.; de la Fuente, M.; Azofra, J.; Andía, I. Platelet-released growth factors enhance the secretion of hyaluronic acid and induce hepatocyte growth factor production by synovial fibroblasts from arthritic patients. Rheumatology 2007, 46, 1769–1772. [Google Scholar] [CrossRef]
- Dall’Oca, C.; Breda, S.; Elena, N.; Valentini, R.; Samaila, E.M.; Magnan, B. Mesenchymal Stem Cells injection in hip osteoarthritis: Preliminary results. Acta Biomed. 2019, 90, 75–80. [Google Scholar]
- Guo, B.; Sawkulycz, X.; Heidari, N.; Rogers, R.; Liu, D.; Slevin, M. Characterisation of Novel Angiogenic and Potent Anti-Inflammatory Effects of Micro-Fragmented Adipose Tissue. Int. J. Mol. Sci. 2021, 22, 3271. [Google Scholar] [CrossRef]
- Vezzani, B.; Shaw, I.; Lesme, H.; Yong, L.; Khan, N.; Tremolada, C.; Péault, B. Higher Pericyte Content and Secretory Activity of Microfragmented Human Adipose Tissue Compared to Enzymatically Derived Stromal Vascular Fraction. Stem. Cells Transl. Med. 2018, 7, 876–886. [Google Scholar] [CrossRef]
- Olsson, D.C.; Teixeira, B.L.; Jeremias, T.D.S.; Réus, J.C.; De Luca Canto, G.; Porporatti, A.L.; Trentin, A.G. Administration of mesenchymal stem cells from adipose tissue at the hip joint of dogs with osteoarthritis: A systematic review. Res. Vet. Sci. 2021, 135, 495–503. [Google Scholar] [CrossRef]
- Soler, R.; Orozco, L.; Munar, A.; Huguet, M.; López, R.; Vives, J.; Coll, R.; Codinach, M.; Garcia-Lopez, J. Final results of a phase I-II trial using ex vivo expanded autologous Mesenchymal Stromal Cells for the treatment of osteoarthritis of the knee confirming safety and suggesting cartilage regeneration. Knee 2016, 23, 647–654. [Google Scholar] [CrossRef]
- Bukulmez, H.; Matthews, A.L.; Sullivan, C.M.; Chen, C.; Kraay, M.J.; Elston, R.C.; Moskowitz, R.W.; Goldberg, V.M.; Warman, M.L. Hip joint replacement surgery for idiopathic osteoarthritis aggregates in families. Arthritis Res. Ther. 2006, 8, R25. [Google Scholar] [CrossRef]
- Lindner, C.; Thiagarajah, S.; Wilkinson, J.M.; Panoutsopoulou, K.; Day-Williams, A.G.; Cootes, T.F.; Wallis, G.A. Investigation of association between hip osteoarthritis susceptibility loci and radiographic proximal femur shape. Arthritis Rheumatol. 2015, 67, 2076–2084. [Google Scholar] [CrossRef]
- Maillefert, J.F.; Gueguen, A.; Monreal, M.; Nguyen, M.; Berdah, L.; Lequesne, M.; Mazieres, B.; Vignon, E.; Dougados, M. Sex differences in hip osteoarthritis: Results of a longitudinal study in 508 patients. Ann. Rheum. Dis. 2003, 62, 931–934. [Google Scholar] [CrossRef]
- Fossett, E.; Khan, W.S. Optimising human mesenchymal stem cell numbers for clinical application: A literature review. Stem. Cells Int. 2012, 2012, 465259. [Google Scholar] [CrossRef]




| Gender | Treatment | No. of Patients | Mean Age on Procedure (SD) | Mean BMI on Procedure (SD) |
|---|---|---|---|---|
| FEMALE | MFAT | 36 | 65 (13) | 26 (7) |
| MALE | 21 | 56 (10) | 31 (7) | |
| FEMALE | MFAT + PRP | 37 | 60 (8) | 26 (4) |
| MALE | 53 | 60 (11) | 27 (5) |
| Gender | OA Grade | MFAT | MFAT + PRP |
|---|---|---|---|
| FEMALE | 1 | 6 | 6 |
| 2 | 11 | 7 | |
| 3 | 12 | 6 | |
| 4 | 7 | 18 | |
| MALE | 1 | 5 | 8 |
| 2 | 1 | 9 | |
| 3 | 5 | 10 | |
| 4 | 10 | 26 | |
| TOTAL | 57 | 90 |
| Treatment | Patient Reported Outcome | Super-Responder | Responder | TOTAL Responders | TOTAL Non-Responder | Lost to Follow-Up | Total |
|---|---|---|---|---|---|---|---|
| MFAT | VAS | 14 | 8 | 22 | 13 | 22 | 57 |
| OHS | 11 | 11 | 22 | 5 | 30 | ||
| MFAT + PRP | VAS | 20 | 12 | 32 | 12 | 46 | 90 |
| OHS | 11 | 4 | 15 | 8 | 67 |
| Measure | Outcome | Treatment | Difference of the Means | 95% Credible Interval of the Difference of the Means | |
|---|---|---|---|---|---|
| VAS | Pain reduction (−) | MFAT | −20.771 | −41.117 | −0.857 |
| MFAT + PRP | −12.767 | −28.882 | +3.543 | ||
| OHS | Function Improvement (+) | MFAT | +6.568 | −0.715 | +13.640 |
| MFAT + PRP | +7.339 | +0.993 | +13.920 | ||
| Treatment | Conversion to THR | OA Grade | ||
|---|---|---|---|---|
| KL 2 | KL 3 | KL 4 | ||
| MFAT | 10 | 0 | 4 | 6 |
| MFAT + PRP | 10 | 1 | 2 | 7 |
| Measure | Outcome | Treatment | Difference of the Means | 95% Credible Interval of the Difference of the Means | |
|---|---|---|---|---|---|
| VAS | Difference in pain reduction (mean) | µ1–µ2 | −9.190 | −27.610 | 9.291 |
| OHS | Difference in functional improvement (+) | µ1–µ2 | −0.145 | −7.011 | 6.677 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heidari, N.; Slevin, M.; Zeinolabediny, Y.; Meloni, D.; Olgiati, S.; Wilson, A.; Noorani, A.; Azamfirei, L. Comparison of the Effect of MFAT and MFAT + PRP on Treatment of Hip Osteoarthritis: An Observational, Intention-to-Treat Study at One Year. J. Clin. Med. 2022, 11, 1056. https://doi.org/10.3390/jcm11041056
Heidari N, Slevin M, Zeinolabediny Y, Meloni D, Olgiati S, Wilson A, Noorani A, Azamfirei L. Comparison of the Effect of MFAT and MFAT + PRP on Treatment of Hip Osteoarthritis: An Observational, Intention-to-Treat Study at One Year. Journal of Clinical Medicine. 2022; 11(4):1056. https://doi.org/10.3390/jcm11041056
Chicago/Turabian StyleHeidari, Nima, Mark Slevin, Yasmin Zeinolabediny, Davide Meloni, Stefano Olgiati, Adrian Wilson, Ali Noorani, and Leonard Azamfirei. 2022. "Comparison of the Effect of MFAT and MFAT + PRP on Treatment of Hip Osteoarthritis: An Observational, Intention-to-Treat Study at One Year" Journal of Clinical Medicine 11, no. 4: 1056. https://doi.org/10.3390/jcm11041056
APA StyleHeidari, N., Slevin, M., Zeinolabediny, Y., Meloni, D., Olgiati, S., Wilson, A., Noorani, A., & Azamfirei, L. (2022). Comparison of the Effect of MFAT and MFAT + PRP on Treatment of Hip Osteoarthritis: An Observational, Intention-to-Treat Study at One Year. Journal of Clinical Medicine, 11(4), 1056. https://doi.org/10.3390/jcm11041056







