Head Lice Infestation in Schoolchildren, in Poland—Is There a Chance for Change?
Abstract
1. Introduction
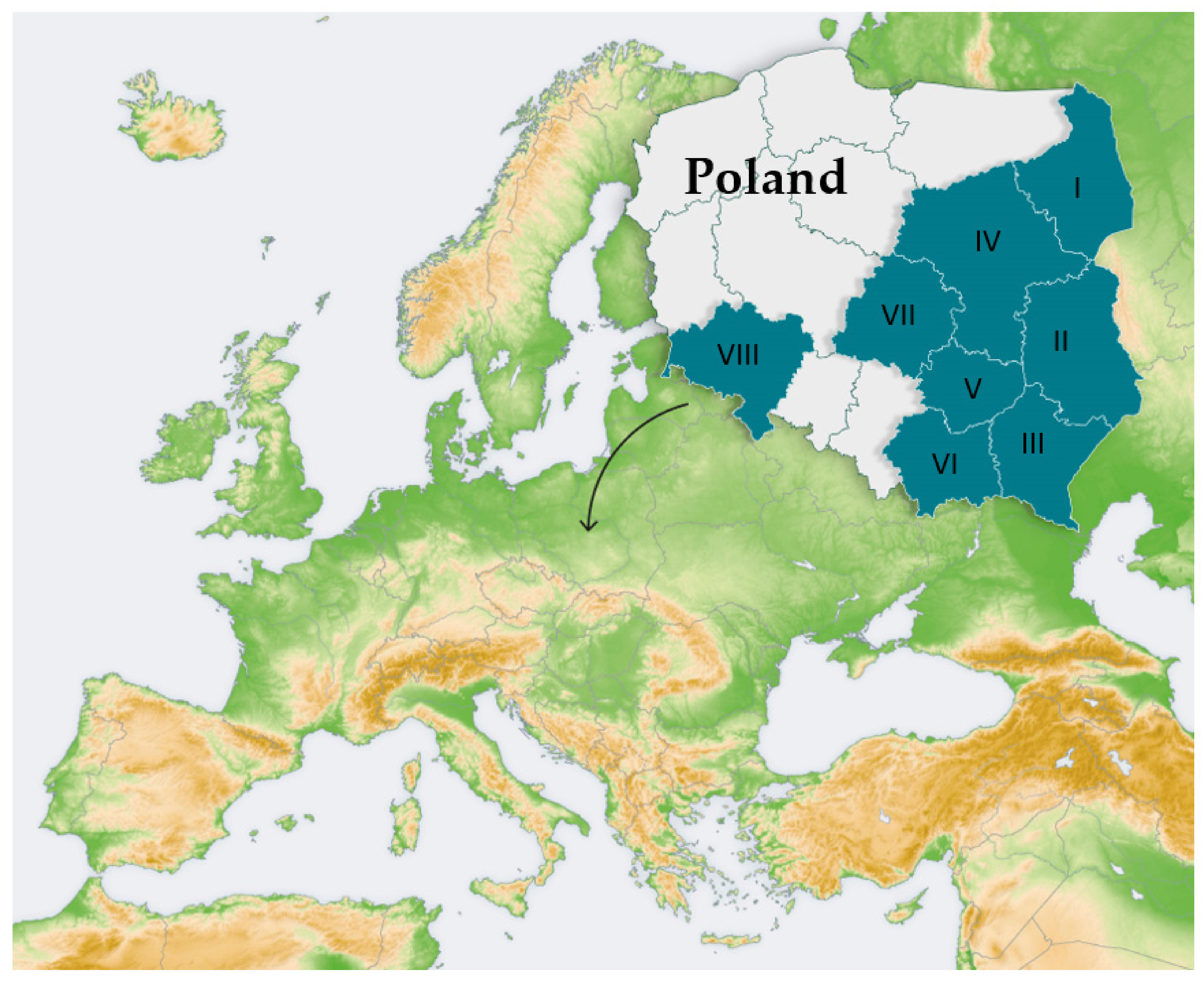
2. Materials and Methods
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Donaldson, A.L.; Hardstaff, J.L.; Harris, J.P.; Vivancos, R.; O’Brien, S.J. School-based surveillance of acute infectious disease in children: A systematic review. BMC Infect. Diss. 2021, 21, 744. [Google Scholar] [CrossRef] [PubMed]
- Falagas, M.E.; Matthaiou, D.K.; Rafailidis, P.I.; Panos, G.; Pappas, G. Worldwide Prevalence of Head Lice. Emerg. Infect. Dis. 2008, 14, 1493–1494. [Google Scholar] [CrossRef] [PubMed]
- Boutellis, A.; Abi-Rached, L.; Raoult, D. The origin and distribution of human lice in the world. Infect. Genet. Evol. 2014, 23, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.-W.; Chuang, T.-W.; Huang, Y.-C.; Chou, C.-M.; Chiang, C.-L.; Lee, F.-P.; Hsu, Y.-T.; Lin, J.-W.; Briand, K.; Tu, C.-Y.; et al. Intestinal parasitic infections: Current prevalence and risk factors among schoolchildren in capital area of the Republic of Marshall Islands. Acta Trop. 2017, 176, 242–248. [Google Scholar] [CrossRef]
- Donaldson, A.L.; Harris, J.P.; Vivancos, R.; O’Brien, S.J. Risk factors associated with outbreaks of seasonal infectious disease in school settings, England, UK. Epidemiol. Infect. 2020, 148, e287. [Google Scholar] [CrossRef]
- Dogra, S.; Kumar, B. Epidemiology of Skin Diseases in School Children: A Study from Northern India. Pediatr. Dermatol. 2003, 20, 470–473. [Google Scholar] [CrossRef]
- Heukelbach, J.; Feldmeier, H. Ectoparasites—The underestimated realm. Lancet 2004, 363, 889–891. [Google Scholar] [CrossRef]
- Hatam-Nahavandi, K.; Ahmadpour, E.; Pashazadeh, F.; Dezhkam, A.; Zarean, M.; Rafiei-Sefiddashti, R.; Salimi-Khorashad, A.; Hosseini-Teshnizi, S.; Hazratian, T.; Otranto, D. Pediculosis capitis among school-age students worldwide as an emerging public health concern: A systematic review and meta-analysis of past five decades. Parasitol. Res. 2020, 119, 3125–3143. [Google Scholar] [CrossRef]
- Izri, A.; Chosidow, O. Efficacy of machine laundering to eradicate head lice: Recommendations to decontaminate washable clothes, linens, and fomites. Clin. Infect. Dis. 2006, 42, e9–e10. [Google Scholar] [CrossRef]
- Burkhart, C.N.; Burkhart, C.G. Fomite transmission in head lice. J. Am. Acad. Dermatol. 2007, 56, 1044–1047. [Google Scholar] [CrossRef]
- Meister, L.; Ochsendorf, F. Head Lice. Dtsch. Aerzteblatt Online 2016, 113, 763–772. [Google Scholar] [CrossRef] [PubMed]
- Habedank, B. Lause—Biologie, medizinische Bedeutung und Bekämpfung. In Krank Durch ArthroPoden, Denisia, Vol 30; Aspock, H., Ed.; Biologiezentrum/Oberostereichische Landesmuseen: Linz, Austria, 2010; pp. 655–672. [Google Scholar]
- Medina, Á.; López, D.; Vásquez, L.R. Pediculosis capitis grave en una niña inscrita en una guardería. Biomédica 2019, 39, 631–638. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jones, J.E. Signs and symptoms of parasitic diseases. Prim. Care Clin. Off. Pract. 1991, 18, 1–12. [Google Scholar] [CrossRef]
- Jamani, S.; Rodríguez, C.; Rueda, M.M.; Matamoros, G.; Canales, M.; Bearman, G.; Stevens, M.; Sanchez, A. Head lice infestations in rural Honduras: The need for an integrated approach to control neglected tropical diseases. Int. J. Dermatol. 2018, 58, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Murray, E.S.; Torrey, S.B. Virulence of Rickettsia prowazeki for head lice. Ann. N. Y. Acad. Sci. 1975, 266, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Previte, D.J.; Yoon, K.S.; Murenzi, E.; Koehler, J.E.; Pittendrigh, B.R.; Lee, S.H.; Clark, J.M. Comparison of the proliferation and excretion of Bartonella quintana between body and head lice following oral challenge. Insect Mol. Biol. 2017, 26, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Amanzougaghene, N.; Fenollar, F.; Raoult, D.; Mediannikov, O. Where are we with human lice? A review of the current state of knowledge. Front. Cell. Infect. Microbiol. 2020, 9, 474. [Google Scholar] [CrossRef]
- Bartosik, K.; Buczek, A.; Zając, Z.; Kulisz, J. Head pediculosis in schoolchildren in the eastern region of the European Union. Ann. Agric. Environ. Med. 2015, 22, 599–603. [Google Scholar] [CrossRef]
- Wegner, Z.; Racewicz, M.; Stańczak, J. Occurrence of pediculosis capitis in a population of children from Gdańsk, Sopot, Gdynia and the vicinities. APPlied Parasitol. 1994, 35, 219–225. [Google Scholar]
- Izdebska, J.N.; Kozina, P.; Cierocka, K.; Mierzyński, Ł. Human lice Pediculus humanus and pediculosis in the past and present—Occurrence, diagnostics and controlling. In Stawonogi: Na początku nowego wieku; Buczek, A., Błaszak, C., Eds.; Koliber: Lublin, Poland, 2018; pp. 151–159. [Google Scholar]
- Szewczyk, K. Wszawica głowowa u dzieci i młodzieży-rola pielęgniarki szkolnej w jej zwalczaniu. In Medyczne i Behawioralne Uwarunkowania Stanu Zdrowia; Truszkowski, W., Ed.; STANU ZDROWIA: Olsztyn, Poland, 2019; pp. 24–32. [Google Scholar]
- Sawicka, B.; Mikulak, E.; Gliniewicz, A. Occurrence of head pediculosis and its control in children’s homes in selected provinces of Poland in the years 2007–2009. Prz. Epidemiol. 2011, 65, 669–674. [Google Scholar]
- Bartosik, K.; Tytuła, A.; Zając, Z.; Buczek, W.; Jasztal-Kniażuk, A.; Błaszkiewicz, P.S.; Borzęcki, A. Scabies and pediculosis in penitentiary institutions in poland—A study of ectoparasitoses in confinement conditions. Int. J. Environ. Res. Public Health 2020, 17, 6086. [Google Scholar] [CrossRef] [PubMed]
- Tytuła, A.; Bartosik, K.; Jasztal-Kniażuk, A.; Buczek, W.; Błaszkiewicz, A.; Borzęcka-Sapko, A. Analysis of the prevalence of pediculosis and scabies in orphanages and refugee shelters in south-eastern Poland. J. Educ. Health Sport 2019, 9, 493–500. [Google Scholar]
- Araújo, A.; Ferreira, L.F.; Guidon, N.; Maues da Serra Freire, N.; Reinhard, K.J.; Dittmar, K. Ten thousand years of head lice infection. Parasitol. Today 2000, 16, 269. [Google Scholar] [CrossRef]
- Drali, R.; Mumcuoglu, K.; Raoult, D. Human lice in paleoentomology and paleomicrobiology. Microbiol. Spectr. 2016, 4, PoH-0005-2014. [Google Scholar] [CrossRef] [PubMed]
- Rukke, B.A.; Birkemoe, T.; Soleng, A.; Lindstedt, H.H.; Ottesen, P. Head lice in Norwegian households: Actions taken, costs and knowledge. PLoS ONE 2012, 7, e32686. [Google Scholar]
- Sánchez-Casas, R.M.; Fernández-Salas, I.; Laguna-Aguilar, M.; Rodríguez-Rojas, J.J.; Medina-Ponce, M.L.; Díaz-González, E.E. Pediculosis affects Mexican children from different socioeconomic status equally: A cross-sectional study. J. Trop. Pediatrics 2020, 67. [Google Scholar] [CrossRef]
- Morsy, T.A.; el-Ela, R.G.; Morsy, A.T.; Nassar, M.M.; Khalaf, S.A. Two contagious ectoparasites in orphanage children in Nasr City, Cairo. J. Egypt. Soc. Parasitol. 2000, 30, 727–734. [Google Scholar]
- Mimouni, D.; Grotto, I.; Haviv, J.; Gdalevich, M.; Huerta, M.; Shpilberg, O. Secular trends in the epidemiology of pediculosis capitis and pubis among Israeli soldiers: A 27-year follow-up. Int. J. Dermatol. 2001, 40, 637–639. [Google Scholar] [CrossRef]
- Tappeh, K.H.; Chavshin, A.; Hajipirloo, H.M.; Khashaveh, S.; Hanifian, H.; Bozorgomid, A.; Mohammadi, M.; Gharabag, D.J.; Azizi, H. Pediculosis capitis among primary school children and related risk factors in Urmia, the main city of west Azarbaijan, Iran. J. Arthropod Borne Dis. 2012, 6, 79–85. [Google Scholar]
- Lesshafft, H.; Baier, A.; Guerra, H.; Terashima, A.; Feldmeier, H. Prevalence and Risk Factors Associated with Pediculosis Capitis in an Impoverished Urban Community in Lima, Peru. J. Glob. Infect. Dis. 2013, 5, 138–143. [Google Scholar] [CrossRef]
- Saraswat, n.; Shankar, P.; Chopra, A.; Mitra, B.; Kumar, S. Risk Factors Associated with Head Lice Infestation in Rural Pediatric Patients. Indian Dermatol. Online J. 2020, 11, 25–28. [Google Scholar] [PubMed]
- Willems, S.; Lapeere, H.; Haedens, N.; Pasteels, I.; Naeyaert, J.M.; De Maeseneer, J. The importance of socio-economic status and individual characteristics on the prevalence of head lice in schoolchildren. Eur. J. Dermatol. 2005, 15, 387–392. [Google Scholar] [PubMed]
- Dehghanzadeh, R.; Asghari-Jafarabadi, M.; Salimian, S.; Asl Hashemi, A.; Khayatzadeh, S. Impact of family ownerships, individual hygiene, and residential environments on the prevalence of pediculosis capitis among schoolchildren in urban and rural areas of northwest of Iran. Parasitol. Res. 2015, 114, 4295–4303. [Google Scholar] [CrossRef]
- Birkemoe, T.; Lindstedt, H.H.; Ottesen, P.; Soleng, A.; Næss, Ø.; Rukke, B.A. Head lice predictors and infestation dynamics among primary school children in Norway. Fam. Pract. 2015, 33, 23–29. [Google Scholar] [CrossRef]
- Heukelbach, J.; Ugbomoiko, U.S. Knowledge, attitudes and practices regarding head lice infestations in rural Nigeria. J. Infect. Dev. Ctries 2011, 5, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Sidoti, E.; Bonura, F.; Paolini, G.; Tringali, G. A survey on knowledge and perceptions regarding head lice on a sample of teachers and students in primary schools of north and south of Italy. J. Prev. Med. Hyg. 2009, 50, 141–149. [Google Scholar] [PubMed]
- Kwok, K.; Ghrear, S.; Li, V.; Haddock, T.; Coleman, P.; Birch, S.A.J. Children can learn new facts equally well from interactive media versus face to face instruction. Front. Psychol. 2016, 07, 1603. [Google Scholar] [CrossRef] [PubMed]
- Yingklang, M.; Sengthong, C.; Haonon, O.; Dangtakot, R.; Pinlaor, P.; Sota, C.; Pinlaor, S. Effect of a health education program on reduction of pediculosis in school girls at Amphoe Muang, Khon Kaen Province, Thailand. PLoS ONE 2018, 13, e0198599. [Google Scholar]
- Feinstein, L.; Sabates, R.; Anderson, T.M.; Sorhaindo, A.; Hammond, C. What are the effects of education on health? In Measuring the Effects of Education on Health and Civic Engagement: Proceedings of the Copenhagen Symposium; OECD: Paris, France, 2016; pp. 171–354. [Google Scholar]
- Silva, L.; de Alencar, R.A.; Madeira, N.G. Survey assessment of parental perceptions regarding head lice. Int. J. Dermatol. 2008, 47, 249–255. [Google Scholar] [CrossRef]
- Parison, J.C.; Canyon, D. Head lice and the impact of knowledge, attitudes and practices—A social science overview. In Management and Control of Head Lice Infestations; Heukelbach, J., Ed.; UNI-MED Verlag AG: Bremen, Germany, 2010; pp. 98–103. [Google Scholar]
- Speare, R.; Buettner, P.G. Head lice in pupils of a primary school in Australia and implications for control. Int. J. Dermatol. 1999, 38, 285–290. [Google Scholar] [CrossRef]
- Toloza, A.C.; Ascunce, M.S.; Reed, D.; Picollo, M.I. Geographical distribution of pyrethroid resistance allele frequency in head lice (Phthiraptera: Pediculidae) from Argentina. J. Med. Entomol. 2014, 51, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Kaul, N.; Palma, K.G.; Silagy, S.S.; Goodman, J.J.; Toole, J. North American efficacy and safety of a novel pediculicide rinse, isopropyl myristate 50% (Resultz). J. Cutan. Med. Surg. 2007, 11, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Kalari, H.; Soltani, A.; Azizi, K.; Faramarzi, H.; Moemenbellah-Fard, M.D. Comparative efficacy of three pediculicides to treat head lice infestation in primary school girls: A randomised controlled assessor blind trial in rural Iran. BMC Dermatol. 2019, 19, 13. [Google Scholar] [CrossRef] [PubMed]
- Gunning, K.; Kiraly, B.; Pippitt, K. Lice and Scabies: Treatment Update. Am. Fam. Physician 2019, 99, 635–642. [Google Scholar]
- Mumcuoglu, K.Y.; Friger, M.; Ioffe-Uspensky, I.; Ben-Ishai, F.; Miller, J. Louse comb versus direct visual examination for the diagnosis of head louse infestations. Pediatr. Dermatol. 2001, 18, 9–12. [Google Scholar] [CrossRef]
- Mumcuoglu, K.Y.; Pollack, R.J.; Reed, D.L.; Barker, S.C.; Gordon, S.; Toloza, A.C.; Picollo, M.I.; Taylan-Ozkan, A.; Chosidow, O.; Habedank, B. International recommendations for an effective control of head louse infestations. Int. J. Dermatol. 2021, 60, 272–280. [Google Scholar] [CrossRef]
- Mumcuoglu, K.Y. Head lice in drawings of kindergarten children. Isr. J. Psychiatry Relat. Sci. 1991, 28, 25–32. [Google Scholar]
- Kartashova, O.V.; Lobuteva, L.A.; Zakharova, O.V.; Lobuteva, A.V.; Goykhman, A.A. Medical and social factors of pediculosis. Open Access Maced. J. Med. Sci. 2019, 7, 3240–3244. [Google Scholar] [CrossRef]
- Hurst, S.K.; Dotson, J.A.W.; Butterfield, P.; Corbett, C.F.; Oneal, G. Stigma resulting from head lice infestation: A concept analysis and implications for public health. Nurs. Forum 2020, 55, 252–258. [Google Scholar] [CrossRef]
- Ibarra, J.; Fry, F.; Wickenden, C.; Jenner, M.; Franks, A. The impact of well-developed preventative strategies on the eradication of head lice. Perspect. Public Health 2009, 129, 165–173. [Google Scholar] [CrossRef]
- Bednarek, A.; Bednarz, M. Health behaviours of boys and girls at younger school age. Med. Ogólna Nauk. Zdr. 2013, 19, 305–312. [Google Scholar]
- Mazur, J. (Ed.) Health and Health Behavior of Schoolchildren in Poland and the Background of Selected Sociodemographic Determinants. HBSC 2014 Research Results; Mother and Child Institute: Warsaw, Poland, 2015. [Google Scholar]

| Location of School | n | Number of Schoolchildren | H | p | ||||
|---|---|---|---|---|---|---|---|---|
| M | SD | Mdn | Min. | Max. | ||||
| Rural school | 50 | 133.2 | 100.8 | 97.5 | 16 | 452 | 73.33 | <0.0001 |
| Suburban school | 13 | 270.5 | 191.4 | 212.0 | 120 | 830 | ||
| Urban school | 105 | 491.8 | 268.4 | 476.0 | 44 | 1300 | ||
| Were Any Cases of Head Lice Reported in The School in 2014–2018? | Location | χ2 | df | p | |||||
|---|---|---|---|---|---|---|---|---|---|
| Rural School n = 50 | Suburban School n = 13 | Urban School n = 105 | |||||||
| n | % | n | % | n | % | ||||
| No | 12 | 24.0 | 1 | 7.7 | 8 | 7.6 | 7.87 | 2 | 0.0196 |
| Yes | 38 | 76.0 | 12 | 92.3 | 97 | 92.4 | |||
| How often Are the Educational Activities Carried Out? | The Solution to the Pediculosis Capitis Issue in Your School Was… | p | |||||
|---|---|---|---|---|---|---|---|
| Easy/Quite Easy n = 70 | Difficult/Quite Difficult n = 62 | Difficult To Say n = 23 | |||||
| n | % | n | % | n | % | ||
| 1 × per school year | 26 | 37.1 | 21 | 33.9 | 5 | 21.7 | 0.3768 |
| 1 × per semester | 12 | 17.1 | 23 | 37.1 | 8 | 34.8 | 0.0245 |
| When the problem occurs | 48 | 68.6 | 40 | 64.5 | 16 | 69.6 | 0.8528 |
| Is The School Supported by Other Institutions in Pediculosis Control? 1 | n | % [N = 168] * |
|---|---|---|
| Provincial Department of Education | 14 | 8.3 |
| Sanitary-Epidemiological Station | 65 | 38.7 |
| Ministry | 0 | 0.0 |
| Other | 15 | 8.9 |
| No | 61 | 36.3 |
| Total responses | 155 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bartosik, K.; Janczaruk, M.; Zając, Z.; Sędzikowska, A.; Kulisz, J.; Woźniak, A.; Jasztal-Kniażuk, A.; Kulbaka, E.; Tytuła, A. Head Lice Infestation in Schoolchildren, in Poland—Is There a Chance for Change? J. Clin. Med. 2022, 11, 783. https://doi.org/10.3390/jcm11030783
Bartosik K, Janczaruk M, Zając Z, Sędzikowska A, Kulisz J, Woźniak A, Jasztal-Kniażuk A, Kulbaka E, Tytuła A. Head Lice Infestation in Schoolchildren, in Poland—Is There a Chance for Change? Journal of Clinical Medicine. 2022; 11(3):783. https://doi.org/10.3390/jcm11030783
Chicago/Turabian StyleBartosik, Katarzyna, Marzena Janczaruk, Zbigniew Zając, Aleksandra Sędzikowska, Joanna Kulisz, Aneta Woźniak, Anita Jasztal-Kniażuk, Ewa Kulbaka, and Andrzej Tytuła. 2022. "Head Lice Infestation in Schoolchildren, in Poland—Is There a Chance for Change?" Journal of Clinical Medicine 11, no. 3: 783. https://doi.org/10.3390/jcm11030783
APA StyleBartosik, K., Janczaruk, M., Zając, Z., Sędzikowska, A., Kulisz, J., Woźniak, A., Jasztal-Kniażuk, A., Kulbaka, E., & Tytuła, A. (2022). Head Lice Infestation in Schoolchildren, in Poland—Is There a Chance for Change? Journal of Clinical Medicine, 11(3), 783. https://doi.org/10.3390/jcm11030783









