Pulmonary Tuberculosis and Risk of Lung Cancer: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
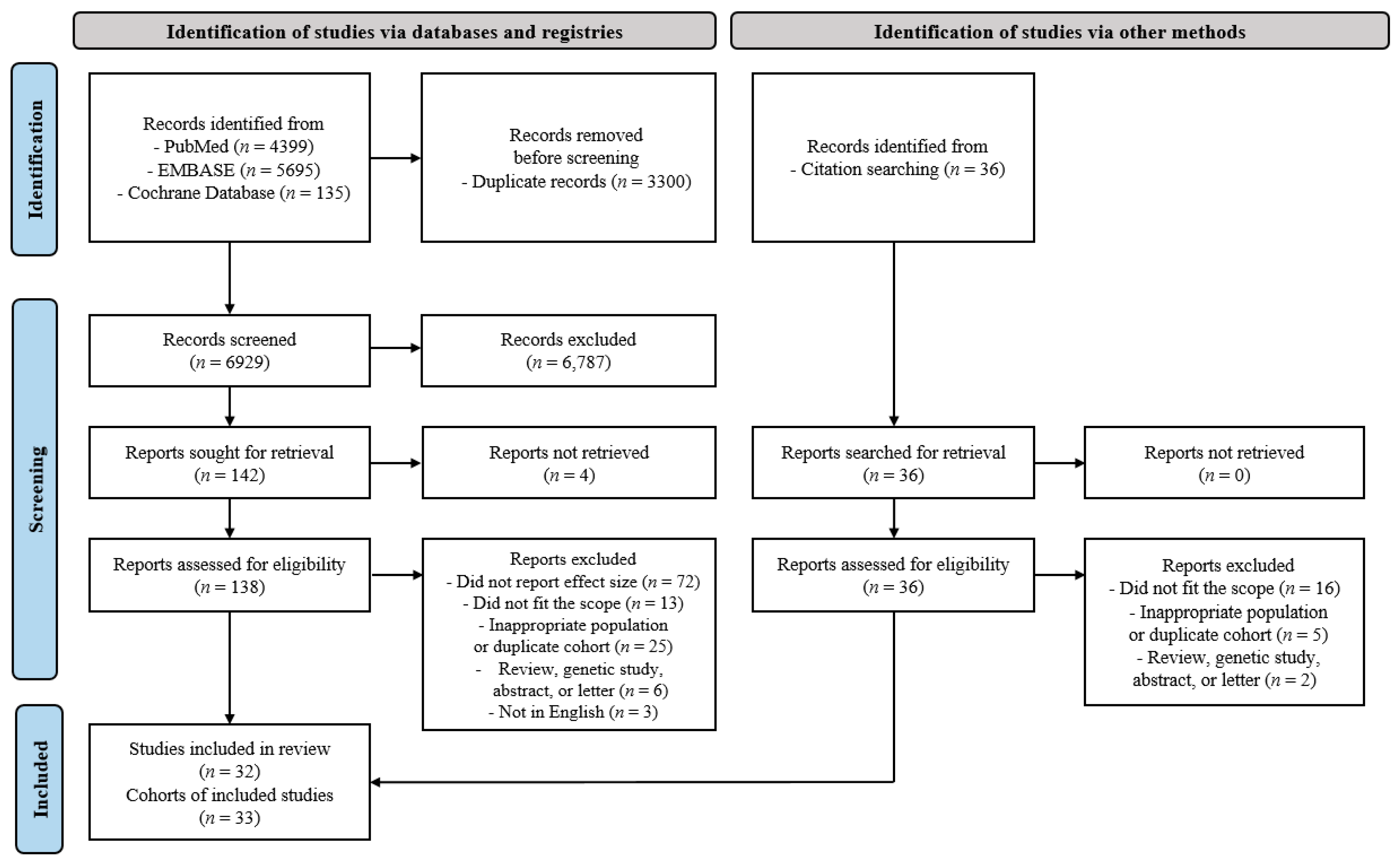
2. Materials and Methods
2.1. Literature Search Strategy and Eligibility Criteria
2.2. Diagnosis of TB and Lung Cancer
2.3. Data Extraction
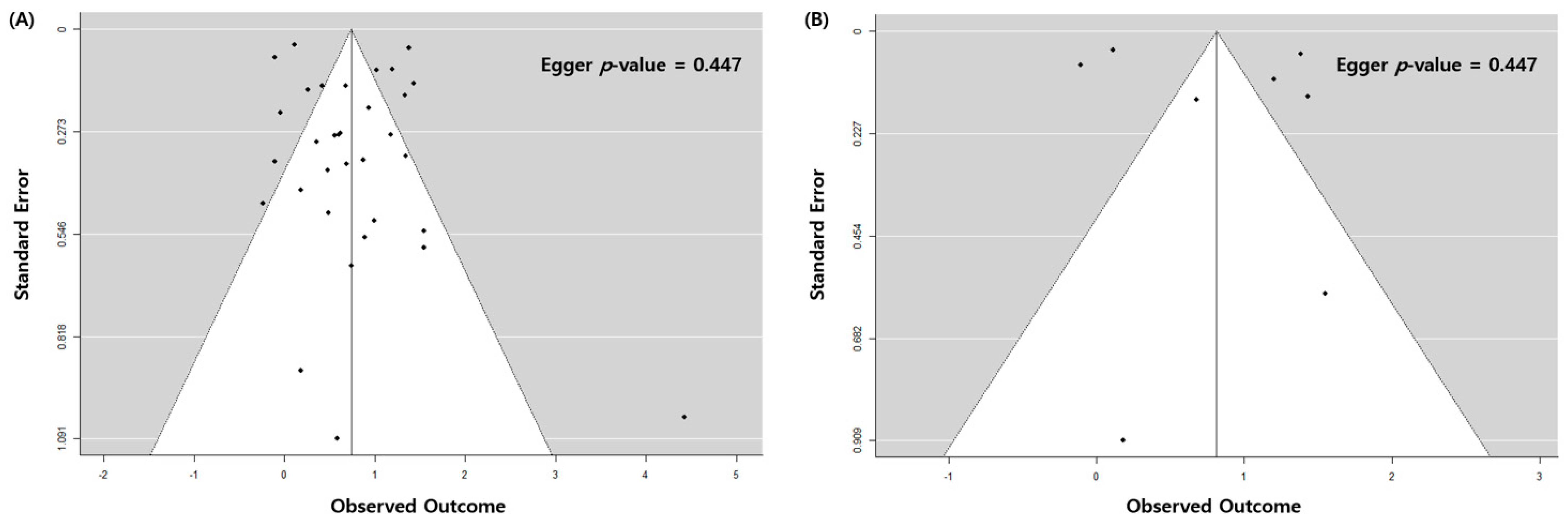
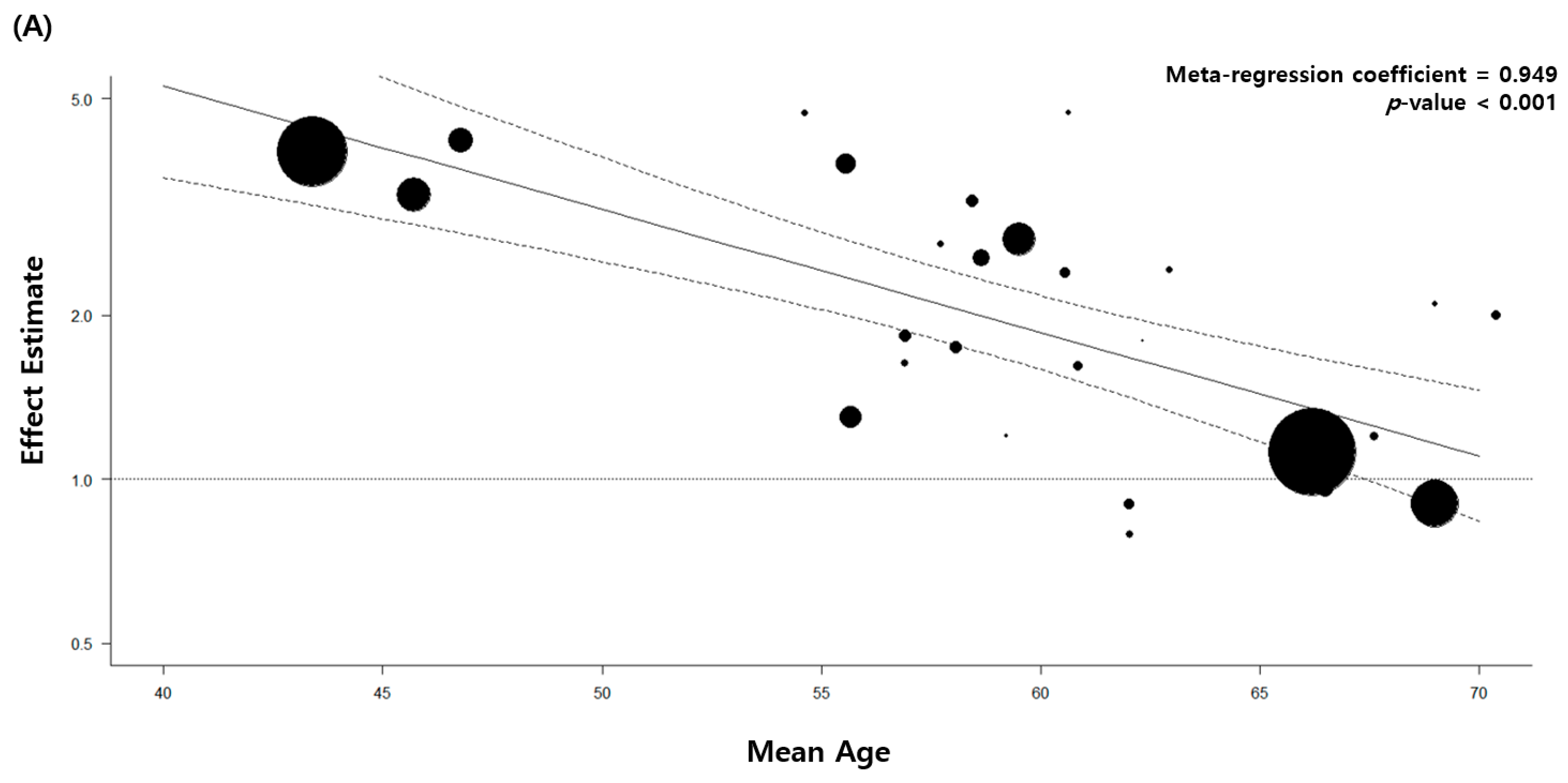
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Literature
3.2. Pulmonary TB and Risk of Lung Cancer with All Eligible Studies
3.3. Pulmonary TB and Risk of Lung Cancer with High-Quality Studies
3.4. Stratified and Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Report on Cancer: Setting Priorities, Investing Wisely and Providing Care for All; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Doll, R.; Hill, A.B. Smoking and Carcinoma of the Lung. Br. Med. J. 1950, 2, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Wynder, E.L.; Graham, E.A. Etiologic Factors-in Bronchiogenic Carcinoma with Special Reference to Industrial Exposures. Report of Eight Hundred Fifty-Seven Proved Cases. AMA Arch. Ind. Hyg. Occup. Med. 1951, 4, 221–235. [Google Scholar] [PubMed]
- Adler, I. Primary Malignant Growths of the Lungs and Bronchi; Longmans, Green & Co.: London, UK, 1912. [Google Scholar]
- Gorlova, O.Y.; Zhang, Y.; Schabath, M.B.; Lei, L.; Zhang, Q.; Amos, C.I.; Spitz, M.R. Never Smokers and Lung Cancer Risk: A Case-Control Study of Epidemiological Factors. Int. J. Cancer 2006, 118, 1798–1804. [Google Scholar] [CrossRef] [PubMed]
- Barta, J.A.; Powell, C.A.; Wisnivesky, J.P. Global Epidemiology of Lung Cancer. Ann. Glob. Health 2019, 85, 8. [Google Scholar] [CrossRef] [PubMed]
- Coussens, L.M.; Werb, Z. Inflammation and Cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef]
- Brenner, D.R.; Boffetta, P.; Duell, E.J.; Bickeböller, H.; Rosenberger, A.; McCormack, V.; Muscat, J.E.; Yang, P.; Wichmann, H.-E.; Brueske-Hohlfeld, I.; et al. Previous Lung Diseases and Lung Cancer Risk: A Pooled Analysis From the International Lung Cancer Consortium. Am. J. Epidemiol. 2012, 176, 573–585. [Google Scholar] [CrossRef]
- Brenner, D.R.; McLaughlin, J.R.; Hung, R.J. Previous Lung Diseases and Lung Cancer Risk: A Systematic Review and Meta-Analysis. PLoS ONE 2011, 6, e17479. [Google Scholar] [CrossRef]
- Leung, C.Y.; Huang, H.-L.; Rahman, M.; Nomura, S.; Abe, S.K.; Saito, E.; Shibuya, K. Cancer Incidence Attributable to Tuberculosis in 2015: Global, Regional, and National Estimates. BMC Cancer 2020, 20, 1–13. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; Connell, D.O.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (Nos) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.Ohri.Ca/programs/clinical_epidemiology/oxford.Asp (accessed on 1 December 2020).
- The World Bank. World Bank Country and Lending Groups. Available online: https://datahelpdesk.Worldbank.Org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 1 December 2020).
- World Health Organization. Tuberculosis Data. Available online: https://www.Who.Int/teams/global-tuberculosis-programme/data (accessed on 1 December 2020).
- DerSimonian, R.; Laird, N. Meta-Analysis in Clinical Trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying Heterogeneity in a Meta-Analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing. In R Foundation for Statistical Computing; R Core Team: Vienna, Austria, 2021. [Google Scholar]
- Viechtbauer, W. Conducting Meta-Analyses in R with the Metafor Package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- Kim, H.; Kim, H.Y.; Goo, J.M.; Kim, Y. Lung Cancer CT Screening and Lung-Rads in a Tuberculosis-Endemic Country: The Korean Lung Cancer Screening Project (K-LUCAS). Radiology 2020, 296, 181–188. [Google Scholar] [CrossRef] [PubMed]
- An, S.J.; Kim, Y.J.; Han, S.S.; Heo, J. Effects of Age on the Association between Pulmonary Tuberculosis and Lung Cancer in a South Korean Cohort. J. Thorac. Dis. 2020, 12, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Oh, C.-M.; Roh, Y.-H.; Lim, D.; Kong, H.-J.; Cho, H.; Hwangbo, B.; Won, Y.-J.; Jung, K.-W.; Oh, K. Pulmonary Tuberculosis is Associated with Elevated Risk of Lung Cancer in Korea: The Nationwide Cohort Study. J. Cancer 2020, 11, 1899–1906. [Google Scholar] [CrossRef]
- Yang, L.; Lu, X.; Deng, J.; Zhou, Y.; Huang, N.; Qiu, F.; Yang, X.; Yang, R.; Fang, W.; Ran, P.; et al. Risk Factors Shared by COPD and Lung Cancer and Mediation Effect of COPD: Two Center Case–Control Studies. Cancer Causes Control 2014, 26, 11–24. [Google Scholar] [CrossRef]
- Yang, T.-Y.; Lin, W.-M.; Lin, C.-L.; Sung, F.-C.; Kao, C.-H. Correlation between Use of Simvastatin and Lovastatin and Female Lung Cancer Risk: A Nationwide Case-Control Study. Int. J. Clin. Pract. 2014, 69, 571–576. [Google Scholar] [CrossRef]
- Simonsen, D.F.; Farkas, D.K.; Søgaard, M.; Horsburgh, C.R.; Sørensen, H.T.; Thomsen, R.W. Tuberculosis and Risk of Cancer: A Danish Nationwide Cohort Study. Int. J. Tuberc. Lung Dis. 2014, 18, 1211–1219. [Google Scholar] [CrossRef]
- HosgoodIII, H.D.; Chapman, R.S.; He, X.; Hu, W.; Tian, L.; Liu, L.Z.; Lai, H.; Chen, W.; Rothman, N.; Lan, Q. History of Lung Disease and Risk of Lung Cancer in a Population with High Household Fuel Combustion Exposures in Rural China. Lung Cancer 2013, 81, 343–346. [Google Scholar] [CrossRef]
- Bae, J.-M.; Li, Z.-M.; Shin, M.-H.; Kim, D.-H.; Lee, M.-S.; Ahn, Y.-O. Pulmonary Tuberculosis and Lung Cancer Risk in Current Smokers: The Seoul Male Cancer Cohort Study. J. Korean Med. Sci. 2013, 28, 896–900. [Google Scholar] [CrossRef]
- Lo, Y.-L.; Hsiao, C.-F.; Chang, G.-C.; Tsai, Y.-H.; Huang, M.-S.; Su, W.-C.; Chen, Y.-M.; Hsin, C.-W.; Chang, C.-H.; Yang, P.-C.; et al. Risk Factors for Primary Lung Cancer among Never Smokers by Gender in a Matched Case–Control Study. Cancer Causes Control 2012, 24, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Bodmer, M.; Becker, C.; Jick, S.S.; Meier, C.R. Metformin Does Not Alter the Risk of Lung Cancer: A Case–Control Analysis. Lung Cancer 2012, 78, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Shiels, M.S.; Albanes, D.; Virtamo, J.; Engels, E.A. Increased Risk of Lung Cancer in Men with Tuberculosis in the Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study. Cancer Epidemiol. Biomark. Prev. 2011, 20, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.H.; Liao, C.C.; Hsu, W.H.; Chen, H.J.; Liao, W.C.; Muo, C.H.; Sung, F.C.; Chen, C.Y. Increased Lung Cancer Risk among Patients with Pulmonary Tuberculosis: A Population Cohort study. J. Thorac. Oncol. 2011, 6, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Koshiol, J.; Rotunno, M.; Consonni, D.; Pesatori, A.C.; De Matteis, S.; Goldstein, A.M.; Chaturvedi, A.K.; Wacholder, S.; Landi, M.T.; Lubin, J.H.; et al. Lower Risk of Lung Cancer after Multiple Pneumonia Diagnoses. Cancer Epidemiol. Biomark. Prev. 2010, 19, 716–721. [Google Scholar] [CrossRef] [PubMed]
- Park, S.K.; Cho, L.Y.; Yang, J.J.; Park, B.; Chang, S.H.; Lee, K.S.; Kim, H.; Yoo, K.Y.; Lee, C.T. Lung Cancer Risk and Cigarette Smoking, Lung Tuberculosis According to Histologic Type and Gender in a Population Based Case-Control Study. Lung Cancer 2010, 68, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.; Guan, P.; Yin, Z.; Li, X.; He, Q.; Zhou, B. Risk of Lung Cancer following Nonmalignant Respiratory Conditions among Nonsmoking Women Living in Shenyang, Northeast China. J. Womens Health 2009, 18, 1989–1995. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.R.; Yu, I.T.; Chiu, Y.L.; Qiu, H.; Fu, Z.; Goggins, W.; Au, J.S.; Tse, L.A.; Wong, T.W. Previous Pulmonary Disease and Family Cancer History Increase the Risk of Lung Cancer among Hong Kong Women. Cancer Causes Control 2009, 20, 757–763. [Google Scholar] [CrossRef]
- Galeone, C.; Pelucchi, C.; La Vecchia, C.; Negri, E.; Bosetti, C.; Hu, J. Indoor Air Pollution from Solid Fuel Use, Chronic Lung Diseases and Lung Cancer in Harbin, Northeast China. Eur. J. Cancer Prev. 2008, 17, 473–478. [Google Scholar] [CrossRef]
- Ramanakumar, A.V.; Parent, M.E.; Menzies, D.; Siemiatycki, J. Risk of Lung Cancer Following Nonmalignant Respiratory Conditions: Evidence from Two Case-Control Studies in Montreal, Canada. Lung Cancer 2006, 53, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Zatloukal, P.; Kubík, A.; Pauk, N.; Tomásek, L.; Petruzelka, L. Adenocarcinoma of the Lung among Women: Risk Associated with Smoking, Prior Lung Disease, Diet and Menstrual and Pregnancy History. Lung Cancer 2003, 41, 283–293. [Google Scholar] [CrossRef]
- Chan-Yeung, M.; Koo, L.C.; Ho, J.C.; Tsang, K.W.; Chau, W.S.; Chiu, S.W.; Ip, M.S.; Lam, W.K. Risk Factors Associated with Lung Cancer in Hong Kong. Lung Cancer 2003, 40, 131–140. [Google Scholar] [CrossRef]
- Kreuzer, M.; Heinrich, J.; Kreienbrock, L.; Rosario, A.S.; Gerken, M.; Wichmann, H.E. Risk Factors for Lung Cancer among Nonsmoking Women. Int. J. Cancer 2002, 100, 706–713. [Google Scholar] [CrossRef] [PubMed]
- Brenner, A.V.; Wang, Z.; Kleinerman, R.A.; Wang, L.; Zhang, S.; Metayer, C.; Chen, K.; Lei, S.; Cui, H.; Lubin, J.H. Previous Pulmonary Diseases and Risk of Lung Cancer in Gansu Province, China. Int. J. Epidemiol. 2001, 30, 118–124. [Google Scholar] [CrossRef]
- Kreuzer, M.; Gerken, M.; Kreienbrock, L.; Wellmann, J.; Wichmann, H.E. Lung Cancer in Lifetime Nonsmoking Men-Results of a Case-Control Study in Germany. Br. J. Cancer 2001, 84, 134–140. [Google Scholar] [CrossRef]
- Zhou, B.S.; Wang, T.J.; Guan, P.; Wu, J.M. Indoor Air Pollution and Pulmonary Adenocarcinoma among Females: A Case-Control Study in Shenyang, China. Oncol. Rep. 2000, 7, 1253–1259. [Google Scholar] [CrossRef]
- Osann, K.E.; Lowery, J.T.; Schell, M.J. Small Cell Lung Cancer in Women: Risk Associated with Smoking, Prior Respiratory Disease, and Occupation. Lung Cancer 2000, 28, 1–10. [Google Scholar] [CrossRef]
- Mayne, S.T.; Buenconsejo, J.; Janerich, D.T. Previous Lung Disease and Risk of Lung Cancer among Men and Women Nonsmokers. Am. J. Epidemiol. 1999, 149, 13–20. [Google Scholar] [CrossRef]
- Ko, Y.C.; Lee, C.H.; Chen, M.J.; Huang, C.C.; Chang, W.Y.; Lin, H.J.; Wang, H.Z.; Chang, P.Y. Risk Factors for Primary Lung Cancer among Non-Smoking Women in Taiwan. Int. J. Epidemiol. 1997, 26, 24–31. [Google Scholar] [CrossRef]
- Schwartz, A.G.; Yang, P.; Swanson, G.M. Familial Risk of Lung Cancer among Nonsmokers and their Relatives. Am. J. Epidemiol. 1996, 144, 554–562. [Google Scholar] [CrossRef]
- Luo, R.X.; Wu, B.; Yi, Y.N.; Huang, Z.W.; Lin, R.T. Indoor Burning Coal Air Pollution and Lung Cancer—A Case-Control Study in Fuzhou, China. Lung Cancer 1996, 14 (Suppl. 1), S113–S119. [Google Scholar] [CrossRef]
- Wu, A.H.; Fontham, E.T.; Reynolds, P.; Greenberg, R.S.; Buffler, P.; Liff, J.; Boyd, P.; Henderson, B.E.; Correa, P. Previous Lung Disease and Risk of Lung Cancer among Lifetime Nonsmoking Women in the United States. Am. J. Epidemiol. 1995, 141, 1023–1032. [Google Scholar] [CrossRef] [PubMed]
- Alavanja, M.C.; Brownson, R.C.; Boice, J.D., Jr.; Hock, E. Preexisting Lung Disease and Lung Cancer among Nonsmoking Women. Am. J. Epidemiol. 1992, 136, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Wu-Williams, A.H.; Dai, X.D.; Blot, W.; Xu, Z.Y.; Sun, X.W.; Xiao, H.P.; Stone, B.J.; Yu, S.F.; Feng, Y.P.; Ershow, A.G.; et al. Lung Cancer among Women in North-East China. Br. J. Cancer 1990, 62, 982–987. [Google Scholar] [CrossRef] [PubMed]
- Falagas, M.E.; Kouranos, V.D.; Athanassa, Z.; Kopterides, P. Tuberculosis and Malignancy. QJM Int. J. Med. 2010, 103, 461–487. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, M.; Kant, S.; Bhaskar, R. Pulmonary Tuberculosis as Differential Diagnosis of Lung Cancer. South Asian J. Cancer 2012, 1, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Keikha, M.; Esfahani, B.N. The Relationship between Tuberculosis and Lung Cancer. Adv. Biomed. Res. 2018, 7, 58. [Google Scholar] [PubMed]
- Aisenberg, G.M.; Jacobson, K.; Chemaly, R.F.; Rolston, K.V.; Raad, I.I.; Safdar, A. Extrapulmonary Tuberculosis aActive Infection Misdiagnosed as Cancer: Mycobacterium Tuberculosis Disease in Patients at a Comprehensive Cancer Center (2001–2005). Cancer 2005, 104, 2882–2887. [Google Scholar] [CrossRef]
- Wu, C.Y.; Hu, H.Y.; Pu, C.Y.; Huang, N.; Shen, H.C.; Li, C.P.; Chou, Y.J. Pulmonary Tuberculosis Increases the Risk of Lung Cancer: A Population-Based Cohort Study. Cancer 2011, 117, 618–624. [Google Scholar] [CrossRef]
- Wu, J.; Dalal, K. Tuberculosis in Asia and the Pacific: The Role of Socioeconomic Status and Health System Development. Int. J. Prev. Med. 2012, 3, 8–16. [Google Scholar]
- Vermund, S.H.; Yamamoto, N. Co-Infection with Human Immunodeficiency Virus and Tuberculosis in Asia. Tuberculosis 2007, 87, S18–S25. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rintiswati, N.; Mahendradhata, Y.; Subronto, Y.; Varkevisser, C.M.; Van Der Werf, M.J. Journeys to Tuberculosis Treatment: A Qualitative Study of Patients, Families and Communities in Jogjakarta, Indonesia. BMC Public Health 2009, 9, 158. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Tuberculosis Report 2020: Executive Summary; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Alavi-Naini, R.; Sharifi-Mood, B.; Metanat, M. Association between Tuberculosis and Smoking. Int. J. High Risk Behav. Addict. 2012, 1, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.Y.; Li, X.L.; Yu, X.S.; Guan, P.; Yin, Z.H.; He, Q.C.; Zhou, B.S. Facts and Fiction of the Relationship between Preexisting Tuberculosis and Lung Cancer Risk: A Systematic Review. Int. J. Cancer 2009, 125, 2936–2944. [Google Scholar] [CrossRef]
- Nalbandian, A.; Yan, B.S.; Pichugin, A.; Bronson, R.T.; Kramnik, I. Lung Carcinogenesis Induced by Chronic Tuberculosis Infection: The Experimental Model and Genetic Control. Oncogene 2009, 28, 1928–1938. [Google Scholar] [CrossRef] [PubMed]
- Su, V.Y.; Yen, Y.F.; Pan, S.W.; Chuang, P.H.; Feng, J.Y.; Chou, K.T.; Chen, Y.M.; Chen, T.J.; Su, W.J. Latent Tuberculosis Infection and the Risk of Subsequent Cancer. Medicine 2016, 95, e2352. [Google Scholar] [CrossRef]
- Roberts, T.; Beyers, N.; Aguirre, A.; Walzl, G. Immunosuppression during Active Tuberculosis is Characterized by Decreased Interferon-γ Production and CD25 Expression with Elevated Forkhead Box P3, Transforming Growth Factor-β, and Interleukin-4 mRNA Levels. J. Infect. Dis. 2007, 195, 870–878. [Google Scholar] [CrossRef] [PubMed]
- Adams, L.B.; Dinauer, M.C.; Morgenstern, D.E.; Krahenbuhl, J.L. Comparison of the Roles of Reactive Oxygen and Nitrogen Intermediates in the Host Response to Mycobacterium Tuberculosis Using Transgenic Mice. Tuber. Lung Dis. 1997, 78, 237–246. [Google Scholar] [CrossRef]
- da Silva, A.L.G.; Bresciani, M.J.; Karnopp, T.E.; Weber, A.F.; Ellwanger, J.H.; Henriques, J.A.P.; Valim, A.R.d.M.; Possuelo, L.G. DNA Damage and Cellular Abnormalities in Tuberculosis, Lung Cancer and Chronic Obstructive Pulmonary Disease. Multidiscip. Respir. Med. 2015, 10, 38. [Google Scholar] [CrossRef]
- Woo, S.J.; Kim, Y.; Jung, H.; Lee, J.J.; Hong, J.Y. Tuberculous Fibrosis Enhances Tumorigenic Potential via the NOX4-Autophagy Axis. Cancers 2021, 13, 687. [Google Scholar] [CrossRef]
- Chai, Q.; Lu, Z.; Liu, Z.; Zhong, Y.; Zhang, F.; Qiu, C.; Li, B.; Wang, J.; Zhang, L.; Pang, Y.; et al. Lung Gene Expression Signatures Suggest Pathogenic Links and Molecular Markers for Pulmonary Tuberculosis, Adenocarcinoma and Sarcoidosis. Commun. Biol. 2020, 3, 604. [Google Scholar] [CrossRef] [PubMed]
- Hwang, I.K.; Paik, S.S.; Lee, S.H. Impact of Pulmonary Tuberculosis on the EGFR Mutational Status and Clinical Outcome in Patients with Lung Adenocarcinoma. Cancer Res. Treat. 2019, 51, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Reid, M.J.; Arinaminpathy, N.; Bloom, A.; Bloom, B.R.; Boehme, C.; Chaisson, R.; Chin, D.P.; Churchyard, G.; Cox, H.; Ditiu, L. Building a Tuberculosis-Free World: The Lancet Commission on Tuberculosis. Lancet 2019, 393, 1331–1384. [Google Scholar] [CrossRef]



| First Author, Year | Country | No. of Participants | No. of pul. TB | No. of Lung Cancer | Characteristics of Patients | Diagnostic Method of pul. TB | Study Design | Cohort | Adjusted Covariates |
|---|---|---|---|---|---|---|---|---|---|
| Kim et al. 2020 [19] | South Korea | 11,394 | 1509 | 65 | Smokers | Low dose CT | Prospective cohort | Population-based | Age, sex, smoking status, smoking burden, family history of lung cancer, nodule count per CT scan, and comorbidities (pulmonary fibrosis and emphysema) |
| An et al. 2020 [20] | South Korea | 22,656 | 3776 | 194 | General population | ICD-10 codes (A15, A16, A19) | Case-control | Population-based | Age, sex, smoking status, and income level |
| Oh et al. 2020 [21] | South Korea | 20,252 | 2640 | 65 | General population, aged ≥40 years | Medical history and chest X-ray | Retrospective cohort | Population-based | Age, sex, education, income level, smoking status, BMI, and physical activity |
| Yang et al. 2015 [22] | China | 3238 | 199 | 1559 | General population | Interview | Case-control | Hospital-based | Age, sex, BMI, education, smoking status, smoking burden, exposure to passive smoking, occupational exposure to metallic toxicant, housing ventilation, intakes of cured meat and vegetables or fruit, and emphysema |
| Yang et al. 2015 [23] | Taiwan | 34,658 | 1455 | 17,329 | Women | ICD-9 codes (010–012, 018) | Case-control | Population-based | Age, income level, employment, and comorbidities (asthma, COPD, hypertension, and stroke) |
| Simonsen et al. 2014 [24] | Denmark | 11,472 | 11,472 | 390 | General population | ICD-8 codes (011, 012) and ICD-10 codes (A15, A16) | Retrospective cohort | Population-based | Age, sex, comorbidities, and patients’ country of origin |
| Hosgood et al. 2013 [25] | China | 996 | 26 | 498 | General population | Interview | Case-control | Population-based | Sex, education, family history of lung cancer, occupation, smoking status, exposure to passive smoking, and exposure to household heating and cooking fume |
| Bae et al. 2013 [26] | South Korea | 7009 | 658 | 93 | Men | Questionnaire | Prospective cohort | Population-based | Age and intake of coffee and tomato |
| Lo et al. 2013 [27] | Taiwan | 3080 | 127 | 1540 | Never smokers | Interview | Case-control | Hospital-based | Age and education |
| Bodmer et al. 2012 [28] | United Kingdom | 91,301 | 1621 | 13,043 | Diabetes patients | UK-based General Practice Research Database (GPRD) | Case-control | Population-based | Age, sex, BMI, smoking, and comorbidities (diabetes and COPD) |
| Shiels et al. 2011 [29] | Finland | 29,133 | 273 | 3102 | General population | ICD-9 codes (010-012) | Prospective cohort | Population-based | Age and smoking status |
| Yu et al. 2011 [30] | Taiwan | 716,872 | 4480 | 1684 | General population | ICD-9 (011) | Prospective cohort | Population-based | Age, sex, occupation, and comorbidities (hypertension, dyslipidemia, diabetes, and COPD) |
| Koshiol et al. 2010 [31] | Italy | 3968 | 121 | 1890 | General population | Interview | Case-control | Population-based | Age, sex, region, smoking duration, and chronic bronchitis |
| Park et al. 2010 [32] | South Korea | 4916 | 759 | 3781 | General population | Questionnaire and chest X-ray | Case-control | Hospital-based | Age and smoking status |
| Liang et al. 2009 [33] | China | 505 | 21 | 226 | Never smoker, women | Interview | Case-control | Hospital-based | Age, marital status, education, ethnicity, BMI, coal use, exposure to passive smoking, and exposure to coal smoke and cooking fumes |
| Wang et al. 2009 [34] | Hong Kong | 504 | 18 | 212 | Females, aged 30–79 years | Interview | Case-control | Hospital-based | Age, occupation, exposure to cooking, and intakes of vegetables and vitamins |
| Galeone et al. 2008 [35] | China | 654 | 47 | 216 | General population | Interview | Case-control | Hospital-based | Age, sex, region, smoking status, smoking burden, income, family history of lung and other cancers, and occupational exposure to lung carcinogen |
| Ramanakumar et al. 2006 [36] a | Canada | 2461 | 68 | 755 | General population | Interview | Case-control | Population-based | Age, ethnicity, type of respondent, education, income level, and smoking status |
| Ramanakumar et al. 2006 [36] b | Canada | 2746 | 56 | 1205 | General population | Interview | Case-control | Population-based | Age, ethnicity, type of respondent, education, income level, and smoking status |
| Zatloukal, et al. 2003 [37] | Czech Republic | 1990 | 128 | 366 | Women | Questionnaire | Case-control | Hospital-based | Age, region, education, and smoking burden |
| Chan-Yeung et al. 2003 [38] | China | 662 | 72 | 331 | General population | Questionnaire | Case-control | Hospital-based | Smoking burden |
| Kreuzer et al. 2002 [39] | Germany | 769 | 31 | 234 | General population | Interview | Case-control | Population-based | Age and region |
| Brenner et al. 2001 [40] | China | 2651 | 162 | 886 | General population | Interview | Case-control | Population-based | Age, sex, region, and smoking status |
| Kreuzer et al. 2001 [41] | Germany | 861 | 38 | 58 | General population | Confrimed by physician | Case-control | Population-based | Age and region |
| Zhou et al. 2000 [42] | China | 144 | 25 | 72 | Women | Interview | Case-control | Population-based | Age, marital status, education, and BMI |
| Osann et al. 2000 [43] | U.S.A. | 302 | 8 | 98 | Women | Interview | Case-control | Hospital-based | Age, education, and smoking |
| Mayne et al. 1999 [44] | U.S.A. | 874 | 22 | 437 | Non-smokers | Interview | Case-control | Population-based | Smoking, exposure to passive smoking, and comorbidities (emphysema, chronic bronchitis, and asthma) |
| Ko et al. 1997 [45] | Taiwan | 210 | 20 | 105 | General population | Confrimed by physician | Case-control | Hospital-based | Socioeconomic status, region, and education |
| Schwartz et al. 1996 [46] | U.S.A. | 534 | 12 | 257 | Non-smoker, African Americans and Caucasians | Interview | Case-control | Population-based | Age, sex, and ethnicity |
| Luo et al. 1996 [47] | China | 408 | 39 | 102 | General population | Interview | Case-control | Population-based | Age, sex, and ethnicity |
| Wu et al. 1995 [48] | U.S.A. | 1633 | 56 | 397 | Non-smoker, women | Interview | Case-control | Population-based | Age, ethnicity, region, education, comorbidities (lung diseases including asthma, chronic bronchitis, pneumonia, pleurisy, and emphysema) |
| Alavanja et al. 1992 [49] | U.S.A. | 2020 | 34 | 618 | White, non-smoking, women | Interview | Case-control | Population-based | Age and smoking |
| Wu-Williams et al. 1990 [50] | China | 1924 | 186 | 965 | General population | Interview | Case-control | Population-based | Age, education, study area, and smoking status |
| Subgroup | No. of Cohorts * | OR (95% CI) | p-Value | I2 Value (%) | I2 between Subgroups (%) |
|---|---|---|---|---|---|
| All cohorts | 33 | 2.09 (1.62–2.69) | <0.001 | 95 | |
| TB burden of country | |||||
| Low | 18 | 1.77 (1.22–2.56) | 0.003 | 97 | 12 |
| Medium | 6 | 2.48 (1.71–3.58) | <0.001 | 75 | |
| High | 9 | 2.57 (1.68–3.93) | <0.001 | 81 | |
| Region of country | |||||
| East Asia and Pacific | 19 | 2.49 (1.83–3.39) | <0.001 | 93 | 58 |
| Europe and Central Asia | 7 | 1.60 (0.80–3.22) | 0.185 | 98 | |
| North America | 7 | 1.53 (1.11–2.12) | 0.010 | 0 | |
| Economic status of country | |||||
| High-income | 24 | 1.91 (1.41–2.59) | <0.001 | 96 | 20 |
| Upper-middle-income | 9 | 2.57 (1.68–3.93) | <0.001 | 81 | |
| Age | |||||
| Adjusted | 29 | 2.00 (1.54–2.61) | <0.001 | 95 | 14 |
| Not adjusted | 4 | 3.84 (1.21–12.15) | 0.022 | 82 | |
| Sex | |||||
| Adjusted | 22 | 2.23 (1.60–3.11) | <0.001 | 96 | 0 |
| Not adjusted | 11 | 1.90 (1.47–2.46) | <0.001 | 61 | |
| Smoking | |||||
| Adjusted | 22 | 2.03 (1.51–2.73) | <0.001 | 90 | 0 |
| Not adjusted | 11 | 2.19 (1.34–3.59) | 0.002 | 98 | |
| Hypertension | |||||
| Adjusted | 2 | 1.92 (0.66–5.57) | 0.230 | 99 | 0 |
| Not adjusted | 31 | 2.10 (1.62–2.73) | <0.001 | 92 | |
| Diabetes | |||||
| Adjusted | 2 | 1.72 (0.48–6.20) | 0.404 | 99 | 0 |
| Not adjusted | 31 | 2.13 (1.63–2.77) | <0.001 | 94 | |
| Respiratory comorbidities | |||||
| Adjusted | 8 | 1.32 (0.93–1.86) | 0.121 | 94 | 90 |
| Not adjusted | 25 | 2.51 (2.04–3.08) | <0.001 | 78 | |
| Cohort of the study | |||||
| Population-based | 23 | 1.95 (1.41–2.68) | <0.001 | 96 | 0 |
| Hospital-based | 10 | 2.36 (1.85–3.01) | <0.001 | 49 | |
| Study design | |||||
| Prospective cohort study | 4 | 1.96 (1.22–3.15) | 0.005 | 84 | 94 |
| Retrospective cohort study | 2 | 3.95 (3.58–4.36) | <0.001 | 0 | |
| Case-control study | 27 | 1.99 (1.56–2.53) | <0.001 | 89 | |
| Diagnostic method of pulmonary TB | |||||
| Medical record | 8 | 2.26 (1.29–3.94) | 0.004 | 99 | 0 |
| Imaging | 3 | 2.13 (1.16–3.92) | 0.015 | 80 | |
| Self-report or physical examination | 22 | 1.96 (1.56–2.47) | <0.001 | 66 | |
| Subgroup | No. of Studies | OR (95% CI) | p-Value | I2 Value (%) | I2 between Subgroups (%) |
|---|---|---|---|---|---|
| All studies | 8 | 2.26 (1.29–3.94) | 0.004 | 99 | |
| Country of TB burden | |||||
| Low | 7 | 2.04 (1.12–3.73) | 0.020 | 99 | 78 |
| Medium | 1 | 4.18 (3.15–5.55) | <0.001 | - | |
| High | 0 | - | - | - | |
| Region of country | |||||
| East Asia and Pacific | 4 | 2.79 (1.21–6.39) | 0.016 | 98 | 0 |
| Europe and Central Asia | 4 | 1.79 (0.67–4.77) | 0.244 | 99 | |
| North America | 0 | - | - | - |
| Study | Selection | Comparability | Outcome | Quality Score | |||||
|---|---|---|---|---|---|---|---|---|---|
| Adequacy of Case Definition | Degree of Representation of Cases | Selection of Controls | Definition of Controls | Comparability of Cases and Controls on the Basis of Design or Analysis | Confirmation of Exposure | Same Method of Confirmation for Cases and Controls | Non-Response Rate | ||
| An et al. 2020 [20] | * | * | * | * | ** | * | * | * | 9 |
| Yang et al. 2015 [22] | * | * | * | * | ** | * | * | 8 | |
| Yang et al. 2015 [23] | * | * | * | * | * | * | * | * | 8 |
| Hosgood et al. 2013 [25] | * | * | * | * | * | * | * | 7 | |
| Lo et al. 2013 [27] | * | * | * | * | ** | * | * | 8 | |
| Bodmer et al. 2012 [28] | * | * | * | * | ** | * | * | * | 9 |
| Koshiol et al. 2010 [31] | * | * | * | * | ** | * | * | 8 | |
| Park et al. 2010 [32] | * | * | * | * | ** | * | 7 | ||
| Liang et al. 2009 [33] | * | * | * | * | ** | * | * | 8 | |
| Wang et al. 2009 [34] | * | * | * | * | * | * | * | 7 | |
| Galeone et al. 2008 [35] | * | * | * | * | ** | * | * | 8 | |
| Ramanakumar et al. 2006 [36] a | * | * | * | * | ** | * | * | 8 | |
| Ramanakumar et al. 2006 [36] b | * | * | * | * | ** | * | * | 8 | |
| Zatloukal et al. 2003 [37] | * | * | * | * | ** | * | * | 8 | |
| Chan-Yeung et al. 2003 [38] | * | * | * | * | * | * | * | 7 | |
| Kreuzer et al. 2002 [39] | * | * | * | * | * | * | * | 7 | |
| Brenner et al. 2001 [40] | * | * | * | * | ** | * | * | 8 | |
| Kreuzer et al. 2001 [41] | * | * | * | * | * | * | * | * | 8 |
| Zhou et al. 2000 [42] | * | * | * | * | * | * | * | 7 | |
| Osann et al. 2000 [43] | * | * | * | * | ** | * | * | 8 | |
| Mayne et al. 1999 [44] | * | * | * | * | * | * | * | 7 | |
| Ko et al. 1997 [45] | * | * | * | * | * | * | * | 7 | |
| Schwartz et al. 1996 [46] | * | * | * | * | ** | * | * | 8 | |
| Luo et al. 1996 [47] | * | * | * | * | * | * | * | 7 | |
| Wu et al. 1995 [48] | * | * | * | * | ** | * | * | 8 | |
| Alavanja et al. 1992 [49] | * | * | * | * | ** | * | * | 8 | |
| Wu-Williams et al. 1990 [50] | * | * | * | * | ** | * | * | 8 | |
| Selection | Comparability | Outcome | Quality Score | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | Degree of Representation of the Exposed Cohort | Selection of the Non-Exposed Cohort | Confirmation of Exposure | Demonstration That the Current Outcome of Interest Is Absent at the Start of the Study | Comparability of Cohorts Based on Design or Analysis | Assessment of Outcome | Sufficiency of Follow-Up to Detect Outcomes | Adequacy of Follow-Up of Cohorts | |
| Kim et al. 2020 [19] | * | * | * | ** | * | * | 7 | ||
| Oh et al. 2020 [21] | * | * | * | ** | * | * | * | 8 | |
| Simonsen et al. 2014 [24] | * | * | * | * | * | * | * | * | 8 |
| Bae et al. 2013 [26] | * | * | * | ** | * | * | 7 | ||
| Shiels et al. 2011 [29] | * | * | * | * | ** | * | * | * | 9 |
| Yu et al. 2011 [30] | * | * | * | * | * | * | * | 7 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, S.Y.; Kim, J.Y.; Lee, H.S.; Lee, S.; Kim, D.; Kim, S.; Hyun, J.H.; Shin, J.I.; Lee, K.H.; Han, S.H.; et al. Pulmonary Tuberculosis and Risk of Lung Cancer: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 765. https://doi.org/10.3390/jcm11030765
Hwang SY, Kim JY, Lee HS, Lee S, Kim D, Kim S, Hyun JH, Shin JI, Lee KH, Han SH, et al. Pulmonary Tuberculosis and Risk of Lung Cancer: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(3):765. https://doi.org/10.3390/jcm11030765
Chicago/Turabian StyleHwang, Soo Young, Jong Yeob Kim, Hye Sun Lee, Sujee Lee, Dayeong Kim, Subin Kim, Jong Hoon Hyun, Jae Il Shin, Kyoung Hwa Lee, Sang Hoon Han, and et al. 2022. "Pulmonary Tuberculosis and Risk of Lung Cancer: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 3: 765. https://doi.org/10.3390/jcm11030765
APA StyleHwang, S. Y., Kim, J. Y., Lee, H. S., Lee, S., Kim, D., Kim, S., Hyun, J. H., Shin, J. I., Lee, K. H., Han, S. H., & Song, Y. G. (2022). Pulmonary Tuberculosis and Risk of Lung Cancer: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 11(3), 765. https://doi.org/10.3390/jcm11030765







