Impact of COVID-19-Related Lockdown on Delivery and Perinatal Outcomes: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Setting
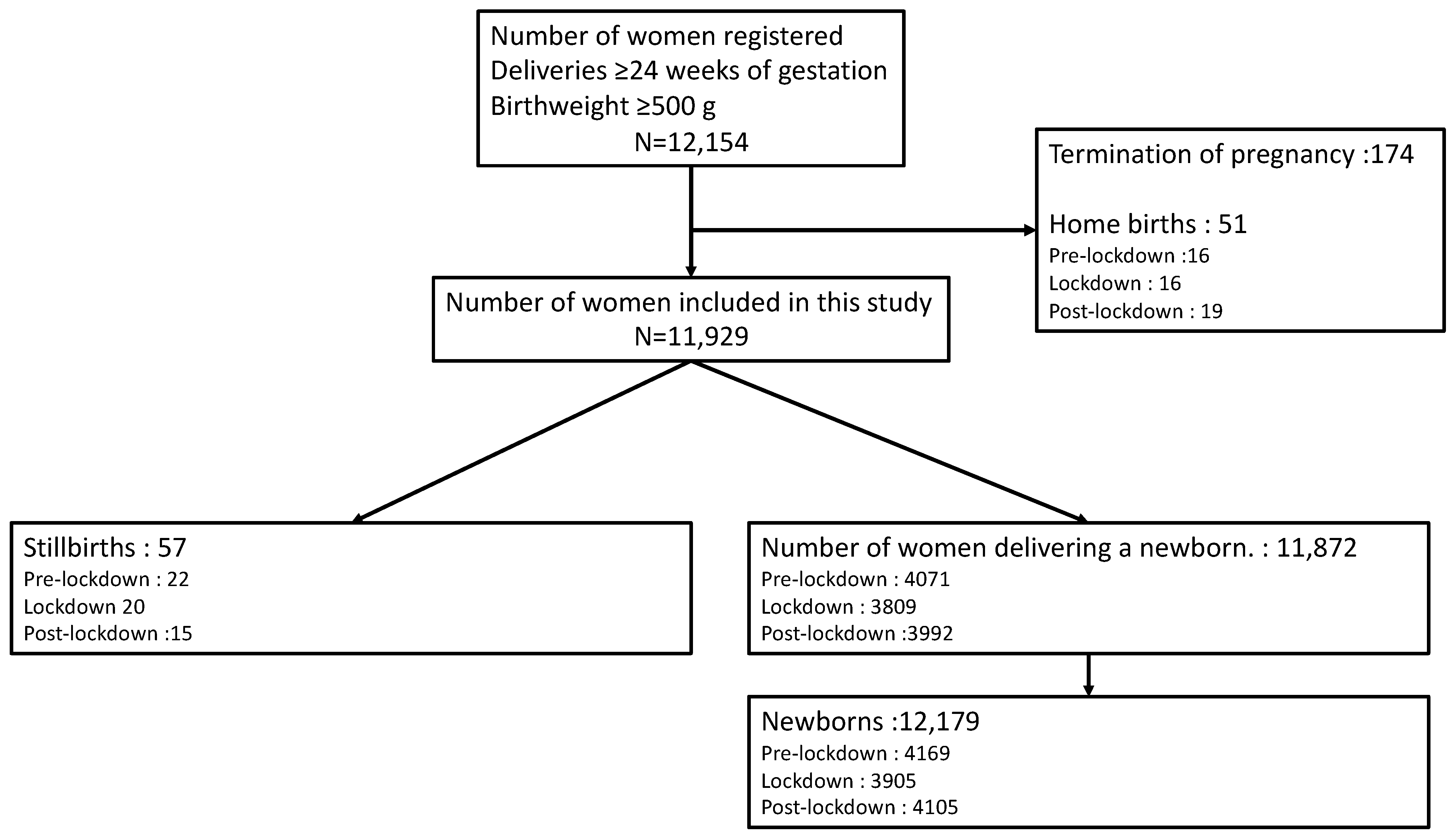
2.2. Study Design
2.3. Data Collection
2.4. Outcomes
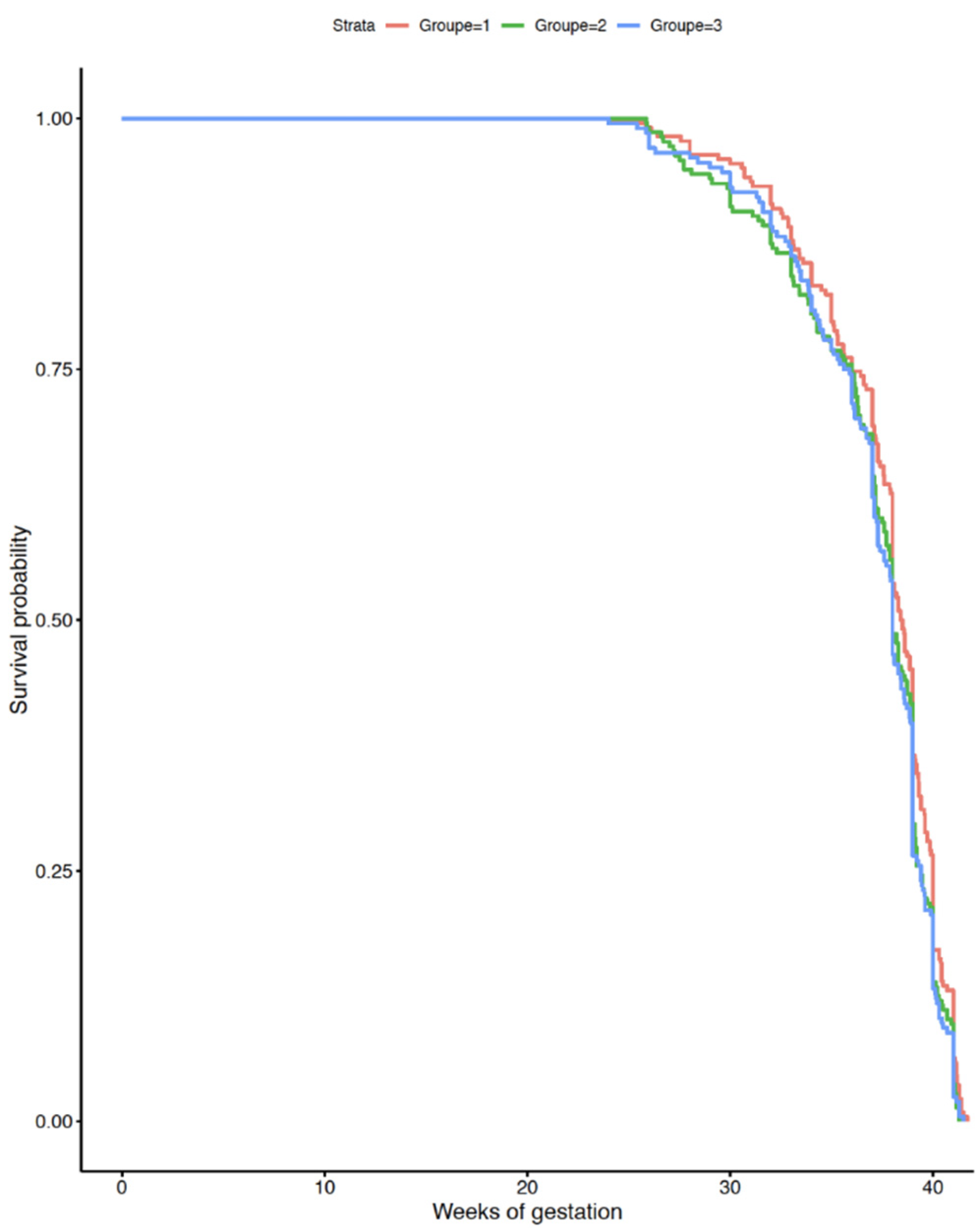
2.5. Statistical Analysis
2.6. Ethics
3. Results
4. Discussion
4.1. Main Findings
4.2. Clinical Interpretation
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-openingremarks-at-the-media-briefing-on-covid-19—11-march-2020 (accessed on 12 March 2020).
- DÉCRET DU n° 2020-260 DU 16 MARS 2020 PORTANT RÉGLEMENTATION DES DÉPLACEMENTS DANS LE CADRE DE LA LUTTE CONTRE LA PROPAGATION DU VIRUS COVID-19. Available online: https://www.legifrance.gouv.fr/jorf/id/JORFTEXT000041728476?r=2JghG4TgkV (accessed on 8 May 2020).
- IllicoMed. CORONAVIRUS (Statistiques Février 2020): LES INQUIÉTUDES ET LES RÉACTIONS DES FRANÇAIS—Illicomed & IFOP. Available online: https://www.illicomed.com/coronavirus-statistiques/ (accessed on 8 May 2020).
- Rasmussen, S.A.; Smulian, J.C.; Lednicky, J.A.; Wen, T.S.; Jamieson, D.J. Coronavirus Disease 2019 (COVID-19) and pregnancy: What obstetricians need to know. Am. J. Obstet. Gynecol. 2020, 222, 415–426. [Google Scholar] [CrossRef]
- Santé Publique France. COVID-19: POINTS ÉPIDÉMIOLOGIQUES HEBDOMADAIRES NATONIAUX ET RÉGIONAUX. Available online: https://www.santepubliquefrance.fr/dossiers/coronavirus-covid-19/coronavirus-chiffres-cles-et-evolution-de-la-covid-19-en-france-et-dans-le-monde#block-266156 (accessed on 20 July 2020).
- Garabedian, C.; Dupuis, N.; Vayssière, C.; Bussières, L.; Ville, Y.; Renaudin, B.; Dugave, L.; Winer, N.; Banaszkiewicz, N.; Rozenberg, P.; et al. Impact of COVID-19 Lockdown on Preterm Births, Low Birthweights and Stillbirths: A Retrospective Cohort Study. J. Clin. Med. 2021, 10, 5649. [Google Scholar] [CrossRef]
- Mesnier, J.; Cottin, Y.; Coste, P.; Ferrari, E.; Schiele, F.; Lemesle, G.; Thuaire, C.; Angoulvant, D.; Cayla, G.; Bouleti, C.; et al. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: A registry study. Lancet Public Health 2020, 5, e536–e542. [Google Scholar] [CrossRef]
- Wood, S. The Mystery of the Missing STEMIs during the COVID-19 Pandemic. Available online: https://www.tctmd.com/news/mystery-missing-stemis-during-covid-19-pandemic (accessed on 11 April 2020).
- Rudilosso, S.; Laredo, C.; Vera, V.; Vargas, M.; Renú, A.; Llull, L.; Obach, V.; Amaro, S.; Urra, X.; Torres, F.; et al. Acute Stroke Care Is at Risk in the Era of COVID-19: Experience at a Comprehensive Stroke Center in Barcelona. Stroke 2020, 51, 1991–1995. [Google Scholar] [CrossRef]
- Vouga, M.; Favre, G.; Martinez-Perez, O.; Pomar, L.; Acebal, L.F.; Abascal-Saiz, A.; Vila Hernandez, M.R.; Hcini, N.; Lambert, V.; Carles, G.; et al. Maternal outcomes and risk factors for COVID-19 severity among pregnant women. Sci. Rep. 2021, 11, 13898. [Google Scholar] [CrossRef]
- Di Mascio, D.; Khalil, A.; Saccone, G.; Rizzo, G.; Buca, D.; Liberati, M.; Vecchiet, J.; Napi, L.; Scambia, G.; Berghella, V.; et al. Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. MFM 2020, 2, 100107. [Google Scholar] [CrossRef]
- Nayak, M.K.; Panda, S.K.; Panda, S.S.; Rath, S.; Ghosh, A.; Mohakud, N.K. Neonatal outcomes of pregnant women with COVID-19 in a developing country setup. Pediatrics Neonatol. 2021, 62, 499–505. [Google Scholar] [CrossRef]
- Ranjbar, F.; Allahqoli, L.; Ahmadi, S.; Mousavi, R.; Gharacheh, M.; Eshraghi, N.; Alkatout, I. Changes in pregnancy outcomes during the COVID-19 lockdown in Iran. BMC Pregnancy Childbirth 2021, 21, 577. [Google Scholar] [CrossRef]
- Goyal, M.; Singh, P.; Singh, K.; Shekhar, S.; Agrawal, N.; Misra, S. The effect of the COVID-19 pandemic on maternal health due to delay in seeking health care: Experience from a tertiary center. Int. J. Gynecol. Obstet. 2021, 152, 231–235. [Google Scholar] [CrossRef]
- Ashich, K.C.; Gurung, R.; Kinney, M.V.; Sunny, A.K.; Moinuddin, M.; Basnet, O.; Paudel, P.; Bhattarai, P.; Subedi, K.; Shrestha, M.P.; et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: A prospective observational study. Lancet Glob. Health 2020, 8, e1273–e1281. [Google Scholar]
- Alshaikh, B.; Cheung, P.-Y.; Soliman, N.; Brundler, M.-A.; Yusuf, K. Impact of Lockdown Measures during COVID-19 Pandemic on Pregnancy and Preterm Birth. Am. J. Perinatol. 2021. [Google Scholar] [CrossRef]
- Kugelman, N.; Lavie, O.; Assaf, W.; Cohen, N.; Sagi-Dain, L.; Bardicef, M.; Kedar, R.; Damti, A.; Segev, Y. Changes in the obstetrical emergency department profile during the COVID-19 pandemic. J. Matern. Fetal Neonatal Med. 2020, 1–7. [Google Scholar] [CrossRef]
- Li, M.; Yin, H.; Jin, Z.; Zhang, H.; Leng, B.; Luo, Y.; Zhao, Y. Impact of Wuhan lockdown on the indications of cesarean delivery and newborn weights during the epidemic period of COVID-19. PLoS ONE 2020, 15, e0237420. [Google Scholar] [CrossRef]
- Rolnik, D.L.; Matheson, A.; Liu, Y.; Chu, S.; Mcgannon, C.; Mulcahy, B.; Malhotra, A.; Palmer, K.R.; Hodges, R.J.; Mol, B.W. Impact of COVID-19 pandemic restrictions on pregnancy duration and outcome in Melbourne, Australia. Ultrasound Obstet. Gynecol. 2021, 58, 677–687. [Google Scholar] [CrossRef]
- Betrán, A.P.; Temmerman, M.; Kingdon, C.; Mohiddin, A.; Opiyo, N.; Torloni, M.R.; Zhang, J.; Musana, O.; Wanyonyi, S.Z.; Gülmezoglu, A.M.; et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet 2018, 392, 1358–1368. [Google Scholar] [CrossRef]
- Dahlke, J.D.; Mendez-Figueroa, H.; Maggio, L.; Sperling, J.D.; Chauhan, S.P.; Rouse, D.J. The Case for Standardizing Cesarean Delivery Technique: Seeing the Forest for the Trees. Obstet. Gynecol. 2020, 136, 972–980. [Google Scholar] [CrossRef]
- Liu, X.; Chen, M.; Wang, Y.; Sun, L.; Zhang, J.; Shi, Y.; Wang, J.; Zhang, H.; Sun, G.; Baker, P.N.; et al. Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID-19 outbreak: A cross-sectional study. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 1229–1240. [Google Scholar] [CrossRef]
- Cao-Lei, L.; Dancause, K.N.; Elgbeili, G.; Laplante, D.P.; Szyf, M.; King, S. Pregnant women’s cognitive appraisal of a natural disaster affects their children’s BMI and central adiposity via DNA methylation: Project Ice Storm. Early Hum. Dev. 2016, 103, 189–192. [Google Scholar] [CrossRef]
- Merlot, E.; Couret, D.; Otten, W. Prenatal stress, fetal imprinting and immunity. Brain Behav. Immun. 2008, 22, 42–51. [Google Scholar] [CrossRef]
- Cruz-Lemini, M.; Ferriols Perez, E.; de la Cruz Conty, M.; Caño Aguilar, A.; Encinas Pardilla, M.; Prats Rodríguez, P.; Muner Hernandez, M.; Forcen Acebal, L.; Pintado Recarte, P.; Medina Mallen, M.d.C.; et al. Obstetric Outcomes of SARS-CoV-2 Infection in Asymptomatic Pregnant Women. Viruses 2021, 13, 112. [Google Scholar] [CrossRef]
- Du, M.; Yang, J.; Han, N.; Liu, M.; Liu, J. Association between the COVID-19 pandemic and the risk for adverse pregnancy outcomes: A cohort study. BMJ Open 2021, 11, e047900. [Google Scholar] [CrossRef]
- D’Antonio, F.; Sen, C.; Mascio, D.D.; Galindo, A.; Villalain, C.; Herraiz, I.; Arisoy, R.; Ovayolu, A.; Eroğlu, H.; Guerra Canales, M.; et al. Maternal and perinatal outcomes in high vs low risk-pregnancies affected by SARS-COV-2 infection (Phase-2): The WAPM (World Association of Perinatal Medicine) working group on COVID-19. Am. J. Obstet. Gynecol. MFM 2021, 3, 100329. [Google Scholar]
- Mullins, E.; Hudak, M.L.; Banerjee, J.; Getzlaff, T.; Townson, J.; Barnette, K.; Playle, R.; Perry, A.; Bourne, T.; Lees, C.C.; et al. Pregnancy and neonatal outcomes of COVID-19: Co-reporting of common outcomes from PAN-COVID and AAP SONPM registries. Ultrasound Obstet. Gynecol. 2021, 57, 573–581. [Google Scholar] [CrossRef]

| Pre-Lockdown (n = 4093) | Lockdown (n = 3829) | Post-Lockdown (n = 4007) | P1 | P2 | |
|---|---|---|---|---|---|
| Maternal age, median (Q1,Q3) | 31.8 (28.0–35.4) | 31.8 (28.1–35.5) | 31.8 (28.1–35.5) | 0.28 | 0.35 |
| <35 years old, % (n) | 72.9 (2985) | 71.9 (2756) | 71.5 (2867) | ||
| 35–40 years old, % (n) | 20.2 (827) | 20.7 (793) | 21.4 (859) | ||
| ≥40 years old, % (n) | 6.8 (281) | 7.3 (280) | 7.0 (281) | ||
| Nullipara, % (n) | 49.7 (1960) | 50.8 (1877) | 50.6 (1947) | 0.31 | 0.83 |
| Multiple pregnancies, % (n) | 3.2 (133) | 3.0 (115) | 3.3 (132) | 0.57 | 0.50 |
| BMI (kg/m2) | 0.82 | 0.42 | |||
| <18.5 | 2.8 (103) | 2.8 (99) | 3.0 (108) | ||
| 18.5–25 | 59.8 (2227) | 58.7 (2062) | 60.5 (2199) | ||
| 26–30 | 22.9 (855) | 23.7 (832) | 22.4 (814) | ||
| >30 | 14.4 (536) | 14.7 (516) | 14.1 (514) | ||
| Diabetes with insulin, % (n) | 8.9 (364) | 7.7 (288) | 8.8 (365) | 0.17 | 0.09 |
| Hypertensive disorders, % (n) | 5.4 (220) | 5.6 (216) | 5.1 (204) | 0.71 | 0.30 |
| Active smoking, % (n) | 11.3 (368) | 10.2 (310) | 10.1 (322) | 0.23 | 0.91 |
| Gestational age at delivery, WG, median (Q1,Q3) | 39.3 (38.2–40.3) | 39.3 (38–40) | 39.3 (38.2–40.3) | 0.66 | 0.27 |
| <37+0 WG, % (n) | 10.6 (435) | 10.7 (435) | 10.0 (402) | 0.93 | 0.34 |
| ≥41 WG, % (n) | 9.2 (377) | 8.9 (340) | 9.2 (367) | 0.17 | 0.23 |
| Pre-Lockdown (n = 4169) | Lockdown (n = 3905) | Post-Lockdown (n = 4105) | P1 | P2 | |
|---|---|---|---|---|---|
| Onset of labor | 0.19 | 0.06 | |||
| Spontaneous labor, % (n) | 59.6 (2370) | 57.9 (2138) | 56.0 (2166) | ||
| Labor induction, % (n) | 28.0 (1111) | 28.4 (1049) | 30.1 (1166) | ||
| Pre-labor CD, % (n) | 12.4 (493) | 13.6 (503) | 13.8 (533) | ||
| Overall CD, % (n) | 23.6 (968) | 24.8 (946) | 24.3 (973) | 0.28 | 0.68 |
| Operative vaginal delivery *, % (n) | 16.6 (519) | 17.6 (506) | 18.8 (571) | 0.35 | 0.21 |
| Perineal tear *, % (n) | 1.1 (35) | 1.0 (30) | 1.3 (40) | 0.86 | 0.37 |
| Postpartum Hemorrhage > 1 L, % (n) | 3.1 (125) | 3.1 (119) | 3.2 (130) | 0.94 | 0.78 |
| Transfusion, % (n) | 0.9 (37) | 1.1 (41) | 0.9 (34) | 0.52 | 0.51 |
| Stillbirth, % (n) | 0.5 (22) | 0.5 (20) | 0.4 (15) | 0.81 | 0.41 |
| 1 min Apgar score < 7, % (n) | 8.4 (337) | 9.4 (351) | 9.1 (356) | 0.13 | 0.66 |
| 5 min Apgar score < 7, % (n) | 1.8 (74) | 2.4 (90) | 2.3 (91) | 0.09 | 0.86 |
| Umbilical artery pH, % (n) | 0.41 | 0.53 | |||
| ≥7.20 | 76.0 (3104) | 76.2 (2,934) | 77.3 (3148) | ||
| 7.10–7.19 | 19.4 (793) | 18.8 (724) | 17.9 (729) | ||
| 7.00–7.09 | 3.5 (144) | 4.2 (160) | 4.1 (168) | ||
| <7.0 | 1.0 (41) | 0.9 (33) | 0.7 (27) | ||
| NICU admission, % (n) | 11.5 (478) | 12.7 (495) | 12.3 (503) | 0.10 | 0.59 |
| Neonatal death, % (n) | 0.4 (16) | 0.3 (11) | 0.4 (18) | 0.54 | 0.32 |
| Pre-Lockdown vs. Lockdown | Post-Lockdown vs. Lockdown | |
|---|---|---|
| CD rate * | 1.06 [0.95–1.18] | 1.02 [0.92–1.14] |
| Severe postpartum hemorrhage ** | 1.01 [0.76–1.28] | 0.95 [0.74–1.23] |
| Perineal tear ** | 1.01 [0.66–1.56] | 0.81 [0.53–1.21] |
| Maternal transfusion ** | 1.14 [0.73–1.80] | 1.04 [0.65–1.64] |
| Apgar score 5 min < 7 ** | 1.33 [0.97–1.84] | 0.93 [0.69–1.27] |
| pH < 7.10 ** | 1.10 [0.88–1.36] | 1.04 [0.82–1.23] |
| NICU admission | 1.15 [0.99–1.33] | 0.96 [0.83–1.10] |
| Neonatal death | 0.86 [0.37–1.82] | 1.62 [0.77–3.56] |
| Stillbirth * | 0.81 [0.39–1.37] | 1.05 [0.52–2.12] |
| Pre-Lockdown (n = 3481) | Lockdown (n = 3187) | Post-Lockdown (n = 3332) | P1 | P2 | |
|---|---|---|---|---|---|
| CD, % (n) | 13.5 (467) | 13.6 (432) | 12.9 (429) | 0.67 | 0.47 |
| Operative vaginal delivery, % (n) | 14.4 (499) | 15.1 (480) | 16.0 (533) | 0.34 | 0.22 |
| Perineal tear, % (n) | 1.1 (38) | 1.0 (31) | 1.4 (46) | 0.84 | 0.50 |
| Postpartum hemorrhage, % (n) | 2.6 (89) | 2.7 (85) | 3.0 (99) | 0.77 | 0.17 |
| Maternal transfusion, % (n) | 0.9 (32) | 1.0 (33) | 0.9 (30) | 0.73 | 0.66 |
| 5-min Apgar score < 7, % (n) | 1.4 (48) | 1.6 (51) | 1.8 (60) | 0.53 | 0.60 |
| Arterial pH ≤ 7.10, % (n) | 4.6 (157) | 5.0 (158) | 5.0 (167) | 0.17 | 0.93 |
| NICU admission, % (n) | 8.1 (284) | 9.0 (288) | 9.2 (310) | 0.23 | 0.77 |
| Neonatal death, % (n) | 0.3 (12) | 0.2 (7) | 0.3 (11) | 0.46 | 0.54 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quibel, T.; Winer, N.; Bussières, L.; Vayssière, C.; Deruelle, P.; Defrance, M.; Rozenberg, P.; Bouyer, J.; Dupuis, N.; Renaudin, B.; et al. Impact of COVID-19-Related Lockdown on Delivery and Perinatal Outcomes: A Retrospective Cohort Study. J. Clin. Med. 2022, 11, 756. https://doi.org/10.3390/jcm11030756
Quibel T, Winer N, Bussières L, Vayssière C, Deruelle P, Defrance M, Rozenberg P, Bouyer J, Dupuis N, Renaudin B, et al. Impact of COVID-19-Related Lockdown on Delivery and Perinatal Outcomes: A Retrospective Cohort Study. Journal of Clinical Medicine. 2022; 11(3):756. https://doi.org/10.3390/jcm11030756
Chicago/Turabian StyleQuibel, Thibaud, Norbert Winer, Laurence Bussières, Christophe Vayssière, Philippe Deruelle, Manon Defrance, Patrick Rozenberg, Jean Bouyer, Ninon Dupuis, Benoit Renaudin, and et al. 2022. "Impact of COVID-19-Related Lockdown on Delivery and Perinatal Outcomes: A Retrospective Cohort Study" Journal of Clinical Medicine 11, no. 3: 756. https://doi.org/10.3390/jcm11030756
APA StyleQuibel, T., Winer, N., Bussières, L., Vayssière, C., Deruelle, P., Defrance, M., Rozenberg, P., Bouyer, J., Dupuis, N., Renaudin, B., Dugave, L., Banaszkiewicz, N., Garabedian, C., & Ville, Y. (2022). Impact of COVID-19-Related Lockdown on Delivery and Perinatal Outcomes: A Retrospective Cohort Study. Journal of Clinical Medicine, 11(3), 756. https://doi.org/10.3390/jcm11030756






