The Hamburg Spondylodiscitis Assessment Score (HSAS) for Immediate Evaluation of Mortality Risk on Hospital Admission
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics Statement
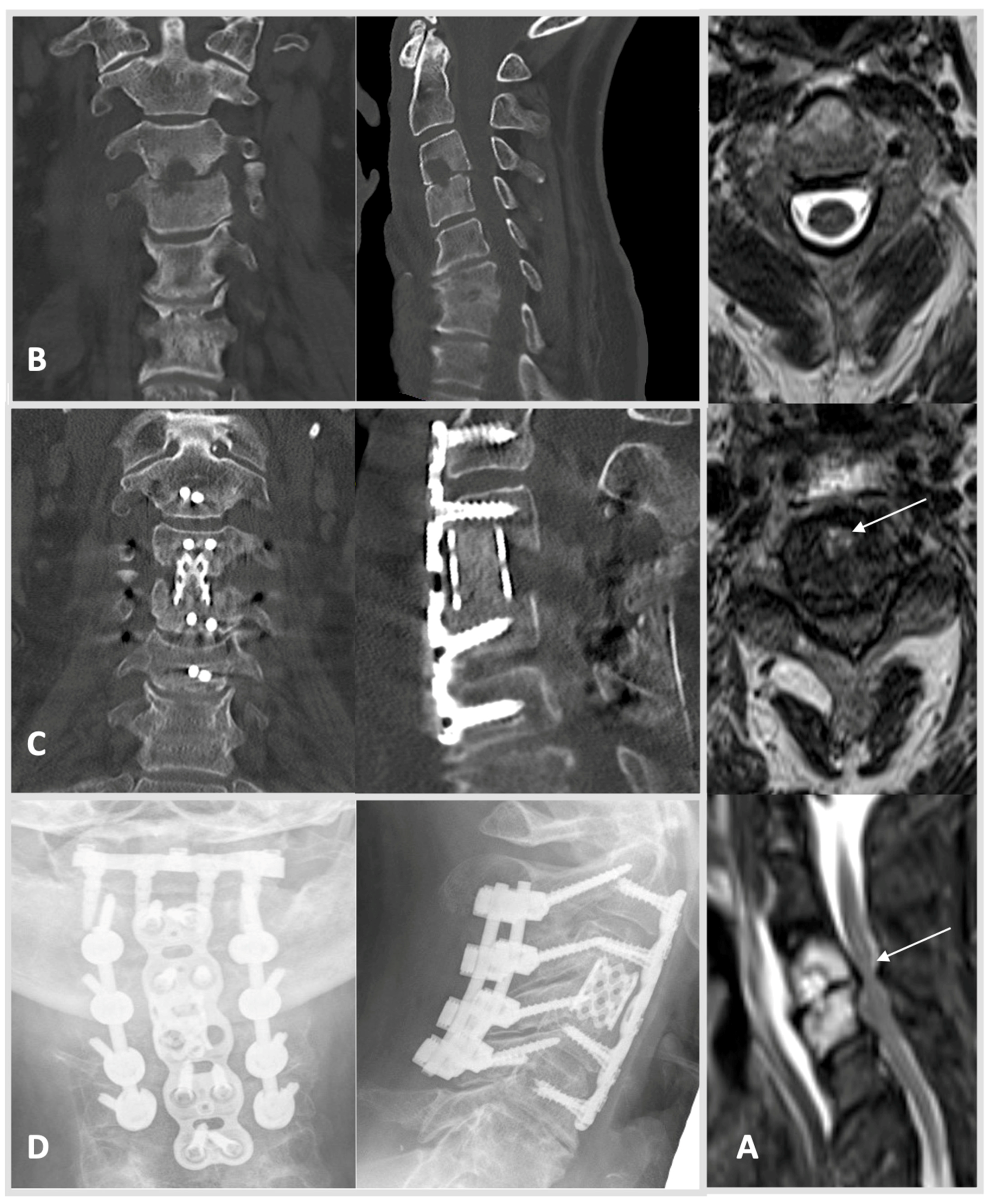
2.2. Diagnosis and Treatment
2.3. Statistical Analysis
3. Results
3.1. Demographic and Disease Characteristics of the Study Cohort
3.2. Course of Treatment
3.3. Complications and In-Hospital Mortality
3.4. Development and Validation of a Clinical Risk Score for Mortality in S Patients
3.5. Limitations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Krogsgaard, M.R.; Wagn, P.; Bengtsson, J. Epidemiology of acute vertebral osteomyelitis in Denmark: 137 cases in Denmark 1978–1982, compared to cases reported to the National Patient Register 1991–1993. Acta Orthop. Scand. 1998, 69, 513–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akiyama, T.; Chikuda, H.; Yasunaga, H.; Horiguchi, H.; Fushimi, K.; Saita, K. Incidence and risk factors for mortality of vertebral osteomyelitis: A retrospective analysis using the Japanese diagnosis procedure combination database. BMJ Open 2013, 3, e002412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kehrer, M.; Pedersen, C.; Jensen, T.G.; Lassen, A. Increasing incidence of pyogenic spondylodiscitis: A 14-year population-based study. J. Infect. 2014, 68, 313–320. [Google Scholar] [CrossRef]
- Sur, A.; Tsang, K.; Brown, M.B.; Tzerakis, N. Management of adult spontaneous spondylodiscitis and its rising incidence. Ann. R. Coll. Surg. Engl. 2015, 97, 451–455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mylona, E.; Samarkos, M.; Kakalou, E.; Fanourgiakis, P.; Skoutelis, A. Pyogenic Vertebral Osteomyelitis: A Systematic Review of Clinical Characteristics. Semin. Arthritis Rheum. 2009, 39, 10–17. [Google Scholar] [CrossRef]
- Berbari, E.F.; Kanj, S.S.; Kowalski, T.J.; Darouiche, R.O.; Widmer, A.F.; Schmitt, S.K.; Hendershot, E.F.; Holtom, P.D.; Huddleston, P.M.; Petermann, G.W.; et al. 2015 Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adults. Clin. Infect. Dis. 2015, 61, e26–e46. [Google Scholar] [CrossRef] [Green Version]
- Widdrington, J.D.; Emmerson, I.; Cullinan, M.; Narayanan, M.; Klejnow, E.; Watson, A.; Ong, E.L.C.; Schmid, M.L.; Price, D.A.; Schwab, U.; et al. Pyogenic Spondylodiscitis: Risk Factors for Adverse Clinical Outcome in Routine Clinical Practice. Med. Sci. 2018, 6, 96. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.; Kowalski, T.J.; Osmon, D.R.; Enzler, M.; Steckelberg, J.M.; Huddleston, P.M.; Nassr, A.; Mandrekar, J.M.; Berbari, E.F. Long-term outcome of pyogenic vertebral osteomyelitis: A cohort study of 260 patients. Open Forum Infect. Dis. 2014, 1, ofu107. [Google Scholar] [CrossRef] [Green Version]
- Hutchinson, C.; Hanger, C.; Wilkinson, T.; Sainsbury, R.; Pithie, A. Spontaneous spinal infections in older people. Intern. Med. J. 2009, 39, 845–848. [Google Scholar] [CrossRef]
- Sobottke, R.; Röllinghoff, M.; Zarghooni, K.; Zarghooni, K.; Schlüter-Brust, K.; Delank, K.-S.; Seifert, H.; Zweig, T.; Eysel, P. Spondylodiscitis in the elderly patient: Clinical mid-term results and quality of life. Arch. Orthop. Trauma Surg. 2009, 130, 1083–1091. [Google Scholar] [CrossRef]
- Kehrer, M.; Pedersen, C.; Jensen, T.G.; Hallas, J.; Lassen, A.T. Increased short- and long-term mortality among patients with infectious spondylodiscitis compared with a reference population. Spine J. 2015, 15, 1233–1240. [Google Scholar] [CrossRef] [PubMed]
- Brummerstedt, M.; Bangstrup, M.; Barfod, T.S. High mortality from pyogenic vertebral osteomyelitis: A retrospective cohort study. Spinal Cord Ser. Cases 2018, 4, 59. [Google Scholar] [CrossRef] [PubMed]
- Viezens, L.; Dreimann, M.; Strahl, A.; Heuer, A.; Koepke, L.-G.; Bay, B.; Waldeyer, C.; Stangenberg, M. Spontaneous spondylodiscitis and endocarditis: Interdisciplinary experience from a tertiary institutional case series and proposal of a treatment algorithm. Neurosurg. Rev. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Herren, C.; Jung, N.; Pishnamaz, M.; Breuninger, M.; Siewe, J.; Sobottke, R. Spondylodiscitis: Diagnosis and Treatment Options. Dtsch. Aerzteblatt Online 2017, 114, 875–882. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sobottke, R.; Seifert, H.; Fätkenheuer, G.; Schmidt, M.; Goßmann, A.; Eysel, P. Current Diagnosis and Treatment of Spondylodiscitis. Dtsch. Aerzteblatt Online 2008, 105, 181–187. [Google Scholar] [CrossRef]
- Homagk, L.; Marmelstein, D.; Homagk, N.; Hofmann, G.O. SponDT (Spondylodiscitis Diagnosis and Treatment): Spondylodiscitis scoring system. J. Orthop. Surg. Res. 2019, 14, 100. [Google Scholar] [CrossRef] [Green Version]
- Herren, C.v.d.H.N.; Dreimann, M. Diagnostik und Therapie der Spondylodiszitis—S2k-Leitlinie. Available online: https://wwwawmforg/en/clinical-practice-guidelines/detail/ll/151-001html (accessed on 24 January 2022).
- Ntalos, D.; Schoof, B.; Thiesen, D.M.; Viezens, L.; Kleinertz, H.; Rohde, H.; Both, A.; Luebke, A.; Strahl, A.; Dreimann, M.; et al. Implementation of a multidisciplinary infections conference improves the treatment of spondylodiscitis. Sci. Rep. 2021, 11, 9515. [Google Scholar] [CrossRef]
- Skaf, G.; Domloj, N.; Fehlings, M.; Bouclaous, C.; Sabbagh, A.; Kanafani, Z.; Kanj, S. Pyogenic spondylodiscitis: An overview. J. Infect. Public Health 2010, 3, 5–16. [Google Scholar] [CrossRef] [Green Version]
- Guerado, E.; Cerván, A.M. Surgical treatment of spondylodiscitis. An update. Int. Orthop. 2012, 36, 413–420. [Google Scholar] [CrossRef] [Green Version]
- Nickerson, E.K.; Sinha, R. Vertebral osteomyelitis in adults: An update. Br. Med. Bull. 2016, 117, 121–138. [Google Scholar] [CrossRef]
- Lener, S.; Hartmann, S.; Barbagallo, G.M.V.; Certo, F.; Thomé, C.; Tschugg, A. Management of spinal infection: A review of the literature. Acta Neurochir. 2018, 160, 487–496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O., III; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Saag, K.G.; Bridges, S.L., Jr.; Akl, E.A.; Bannuru, R.R.; Sullivan, M.C.; Vaysbrot, E.; McNaughton, C.; Osani, M.; Shmerling, R.H.; et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheum. 2016, 68, 1–26. [Google Scholar]
- Pola, E.; Autore, G.; Formica, V.M.; Pambianco, V.; Colangelo, D.; Cauda, R.; Fantoni, M. New classification for the treatment of pyogenic spondylodiscitis: Validation study on a population of 250 patients with a follow-up of 2 years. Eur. Spine J. 2017, 26, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Carragee, E.J. Pyogenic Vertebral Osteomyelitis. JBJS 1997, 79, 874–880. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Pojskić, M.; Carl, B.; Schmöckel, V.; Völlger, B.; Nimsky, C.; Sass, B. Neurosurgical Management and Outcome Parameters in 237 Patients with Spondylodiscitis. Brain Sci. 2021, 11, 1019. [Google Scholar] [CrossRef]
- Blecher, R.; Frieler, S.; Qutteineh, B.; Pierre, C.A.; Yilmaz, E.; Ishak, B.; Von Glinski, A.; Oskouian, R.J.; Kramer, M.; Drexler, M.; et al. Who Needs Surgical Stabilization for Pyogenic Spondylodiscitis? Retrospective Analysis of Non-Surgically Treated Patients. Glob. Spine J. 2021, 2021. [Google Scholar] [CrossRef]
- Zadran, S.; Pedersen, P.H.; Eiskjær, S. Vertebral Osteomyelitis: A Mortality Analysis Comparing Surgical and Conservative Management. Glob. Spine J. 2020, 10, 456–463. [Google Scholar] [CrossRef] [Green Version]
- Krasselt, M.; Baerwald, C.; Petros, S.; Seifert, O. Mortality of Sepsis in Patients with Rheumatoid Arthritis: A Single-Center Retrospective Analysis and Comparison with a Control Group. J. Intensiv. Care Med. 2021, 36, 766–774. [Google Scholar] [CrossRef]
- Stangenberg, M.; Mohme, M.; Mende, K.C.; Thiesen, D.M.; Krätzig, T.; Schoof, B.; Eicker, S.O.; Dreimann, M. Impact of the localization on disease course and clinical management in spondylodiscitis. Int. J. Infect. Dis. 2020, 99, 122–130. [Google Scholar] [CrossRef]
- Kuo, G.; Sun, W.-C.; Lu, Y.-A.; Chen, C.-Y.; Kao, H.-K.; Lin, Y.; Chen, Y.-C.; Hung, C.-C.; Tian, Y.-C.; Hsu, H.-H. Chronic dialysis patients with infectious spondylodiscitis have poorer outcomes than non-dialysis populations. Ther. Clin. Risk Manag. 2018, 14, 257–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fowler, J.V.G.; Justice, A.; Moore, C.; Benjamin, J.D.K.; Woods, C.W.; Campbell, S.; Reller, L.B.; Corey, G.R.; Day, N.P.J.; Peacock, S.J. Risk Factors for Hematogenous Complications of Intravascular Catheter—Associated Staphylococcus aureus Bacteremia. Clin. Infect. Dis. 2005, 40, 695–703. [Google Scholar] [CrossRef]
- Koozi, H.; Lengquist, M.; Frigyesi, A. C-reactive protein as a prognostic factor in intensive care admissions for sepsis: A Swedish multicenter study. J. Crit. Care 2020, 56, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Priest, D.H.; Peacock, J.E. Hematogenous Vertebral Osteomyelitis Due to Staphylococcus aureus in the Adult: Clinical Features and Therapeutic Outcomes. South. Med. J. 2005, 98, 854–862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stangenberg, M.; Mende, K.C.; Mohme, M.; Krätzig, T.; Viezens, L.; Both, A.; Rohde, H.; Dreimann, M. Influence of microbiological diagnosis on the clinical course of spondylodiscitis. Infection 2021, 49, 1017–1027. [Google Scholar] [CrossRef] [PubMed]


| Survival Group Mean (SD) or n (%) | Mortality Group Mean (SD) or n (%) | p-Value | |
|---|---|---|---|
| Age | 64.4 (14.6) | 73.8 (9.9) | <0.001 |
| Body mass index | 28 (19.6) | 26.9 (7.5) | 0.75 |
| ICU stay (in days) | 7.1 (19.5) | 13.3 (11.1) | <0.001 |
| Transfusion (intra- and postoperative) | 1.2 (2.9) | 2.3 (3) | 0.14 |
| Creatinine preoperative | 1.2 (.9) | 2.4 (2.5) | <0.001 |
| Last Creatinine measurement | 1.1 (.9) | 1.8 (1) | <0.001 |
| Hb preoperative | 10.9 (1.9) | 10.1 (1.8) | 0.01 |
| Last Hb measurement | 9.5 (1.5) | 8.4 (1) | <0.001 |
| PCT preoperative | 1.1 (2) | 15.1 (33) | <0.001 |
| Last PCT measurement | 0.4 (.6) | 15.9 (50) | <0.001 |
| Leucocytes preoperative | 10.1 (5.8) | 12.8 (5.5) | 0.003 |
| Last Leucocyte measurement | 7 (2.6) | 19.7 (14.3) | <0.001 |
| Chronic heart disease | 35/50 (70) | 15/50 (30) | 0.001 |
| Chronic kidney failure | 44/65 (67.7) | 21/65 (32.3) | <0.001 |
| Rheumatoid arthritis | 13/22 (59) | 9/22 (41) | <0.001 |
| Acute kidney failure | 55/84 (65.5) | 29/84 (34.5) | <0.001 |
| Acute cardiac decompensation | 23/36 (63.9) | 13/36 (36) | <0.001 |
| Acute liver failure | 2/9 (22) | 7/9 (77.8) | <0.001 |
| Pneumonia | 30/41 (73) | 11/41 (26.8) | 0.028 |
| 95% CI | ||||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | β | SE β | Wald’s χ2 | df | p-Value | OR | Lower | Upper |
| Constant | −7.950 | 2.203 | 10.098 | 1 | <0.001 | 0.001 | NA | NA |
| Age | 0.067 | 0.023 | 8.702 | 1 | 0.003 | 1.069 | 1.023 | 1.118 |
| Heart failure | 0.796 | 0.505 | 2.483 | 1 | 0.115 | 2.217 | 0.824 | 5.967 |
| CKD | 0.440 | 0.484 | 0.824 | 1 | 0.364 | 1.552 | 0.601 | 4.013 |
| RhA | 2.338 | 0.687 | 11.581 | 1 | 0.001 | 10.360 | 2.695 | 39.827 |
| Endocarditis | 0.195 | 0.656 | 0.088 | 1 | 0.767 | 1.215 | 0.336 | 4.395 |
| S. aureus | 1.085 | 0.537 | 4.078 | 1 | 0.043 | 2.959 | 1.032 | 8.481 |
| CNS | 0.624 | 0.690 | 0.817 | 1 | 0.366 | 1.866 | 0.482 | 7.221 |
| Enterobacterales | −0.691 | 1.313 | 0.277 | 1 | 0.599 | 0.501 | 0.038 | 6.572 |
| Enterococcus sp. | 0.975 | 0.943 | 1.069 | 1 | 0.301 | 2.651 | 0.418 | 16.821 |
| Strep. sp. | 0.558 | 1.175 | 0.225 | 1 | 0.635 | 1.746 | 0.175 | 17.471 |
| M. tuberculosis | −13.97 | 40,292 | <0.001 | 1 | 1.0 | 0.000 | 0.000 | - |
| Other germ sp. | 1.893 | 1.112 | 2.902 | 1 | 0.088 | 6.642 | 0.752 | 58.684 |
| Hemoglobin | −0.230 | 0.128 | 3.217 | 1 | 0.073 | 0.795 | 0.618 | 1.022 |
| Leukocyte count | 0.015 | 0.038 | 0.165 | 1 | 0.685 | 1.016 | 0.943 | 1.094 |
| Creatinine | 0.462 | 0.144 | 10.263 | 1 | 0.001 | 1.587 | 1.196 | 2.105 |
| CRP | 0.006 | 0.002 | 7.494 | 1 | 0.006 | 1.006 | 1.002 | 1.010 |
| Test | χ2 | df | p-value | |||||
| Overall model evaluation Omnibus test | 79.55 | 16 | <0.001 | |||||
| Goodness-of-fit test Hosmer–Lemeshow test | 6.2043 | 8 | 0.624 | |||||
| 95% CI | ||||
|---|---|---|---|---|
| Odds Ratio | Lower | Upper | p-Value | |
| Age | ||||
| >72.5 | 3.86 | 1.72 | 8.67 | 0.001 |
| ≤72.5 | 1 | |||
| Rheumatoid arthritis | ||||
| yes | 9.37 | 2.63 | 33.35 | 0.001 |
| no | 1 | |||
| S. aureus infection | ||||
| yes | 2.27 | 1.0 | 5.16 | 0.051 |
| no | 1 | |||
| Creatinine | ||||
| >1.29 | 4.35 | 1.95 | 9.68 | <0.001 |
| ≤1.29 | 1 | |||
| CRP | ||||
| >140.5 | 4.07 | 1.83 | 9.02 | 0.001 |
| ≤140.5 | 1 | |||
| Deceased (n) | Survived (n) | Total (n) | p-Value (χ2) | |
|---|---|---|---|---|
| Low risk (0 points) | 1 | 87 | 88 | <0.001 |
| Moderate risk (1–3 points) | 8 | 113 | 121 | |
| High risk (4–6 points) | 27 | 60 | 87 | |
| Very high risk (7–10 points) | 8 | 3 | 11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heuer, A.; Strahl, A.; Viezens, L.; Koepke, L.-G.; Stangenberg, M.; Dreimann, M. The Hamburg Spondylodiscitis Assessment Score (HSAS) for Immediate Evaluation of Mortality Risk on Hospital Admission. J. Clin. Med. 2022, 11, 660. https://doi.org/10.3390/jcm11030660
Heuer A, Strahl A, Viezens L, Koepke L-G, Stangenberg M, Dreimann M. The Hamburg Spondylodiscitis Assessment Score (HSAS) for Immediate Evaluation of Mortality Risk on Hospital Admission. Journal of Clinical Medicine. 2022; 11(3):660. https://doi.org/10.3390/jcm11030660
Chicago/Turabian StyleHeuer, Annika, André Strahl, Lennart Viezens, Leon-Gordian Koepke, Martin Stangenberg, and Marc Dreimann. 2022. "The Hamburg Spondylodiscitis Assessment Score (HSAS) for Immediate Evaluation of Mortality Risk on Hospital Admission" Journal of Clinical Medicine 11, no. 3: 660. https://doi.org/10.3390/jcm11030660
APA StyleHeuer, A., Strahl, A., Viezens, L., Koepke, L.-G., Stangenberg, M., & Dreimann, M. (2022). The Hamburg Spondylodiscitis Assessment Score (HSAS) for Immediate Evaluation of Mortality Risk on Hospital Admission. Journal of Clinical Medicine, 11(3), 660. https://doi.org/10.3390/jcm11030660






