Albumin Binds COVID-19 Spike 1 Subunit and Predicts In-Hospital Survival of Infected Patients—Possible Alteration by Glucose
Abstract
:1. Introduction
2. Materials and Methods
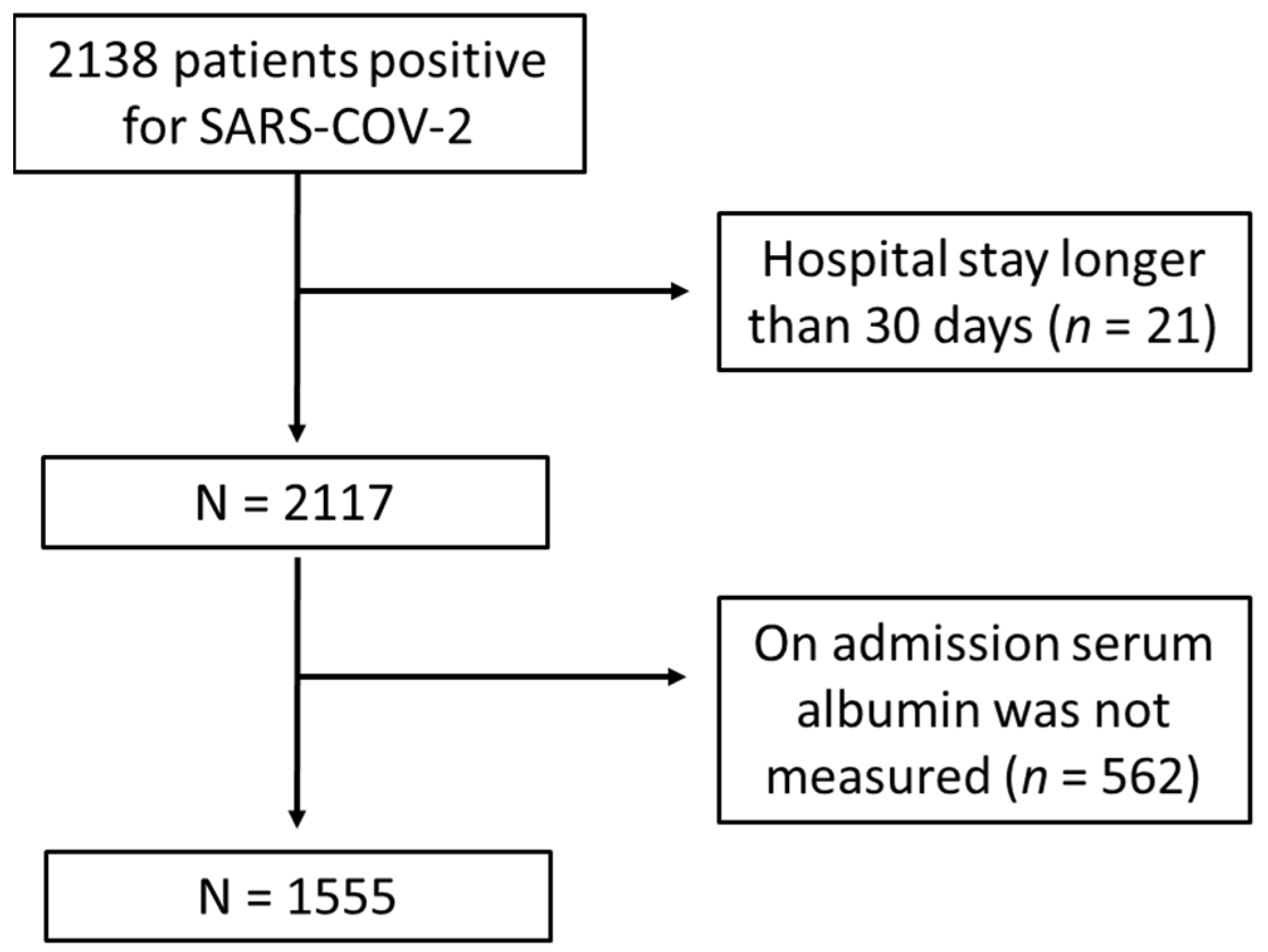
2.1. Study Population
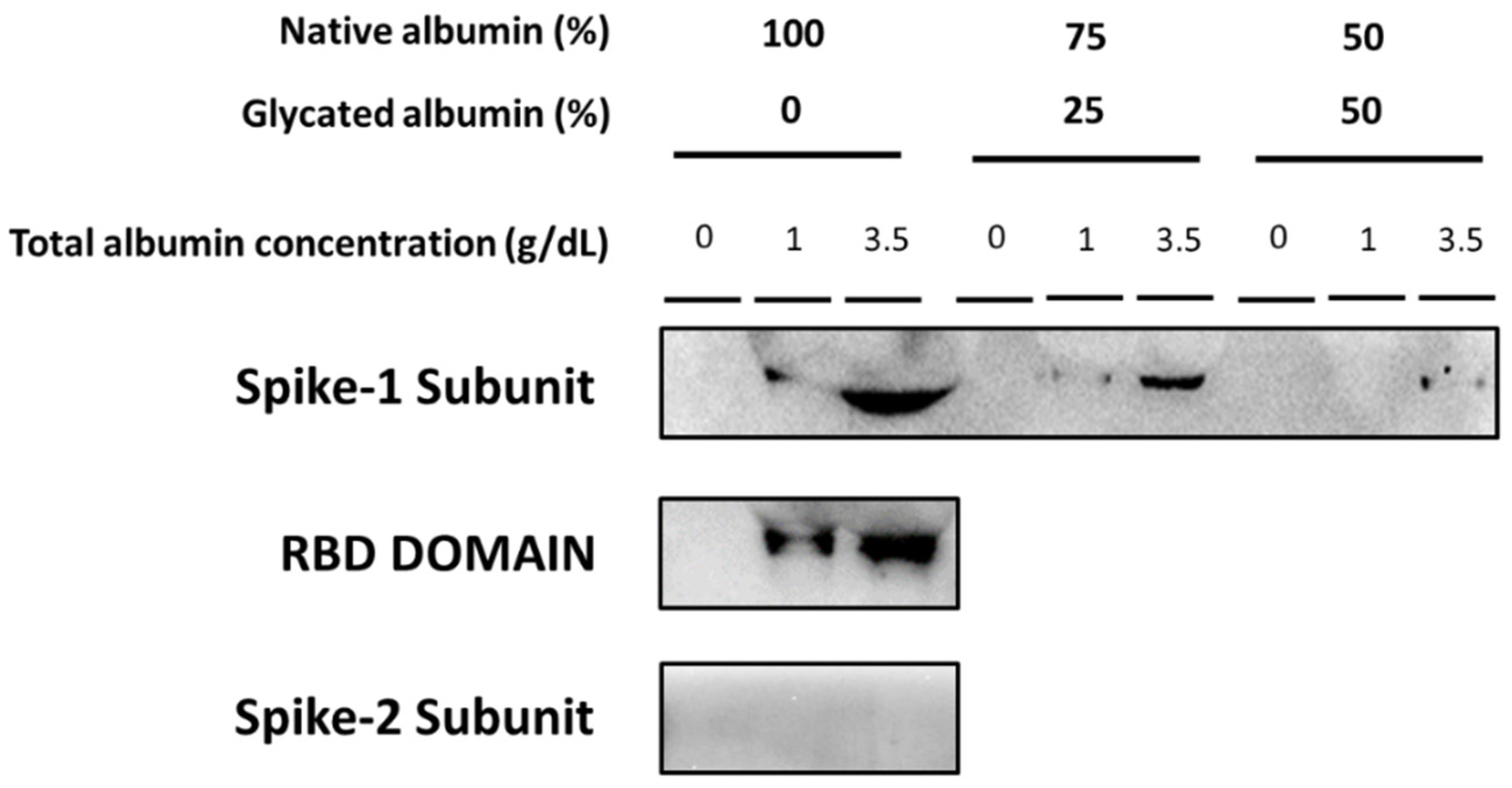
2.2. Interaction between Native and Glycated Albumin with SARS-CoV-2 Spike Protein Subunits
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Associations with In-Hospital All-Cause Mortality
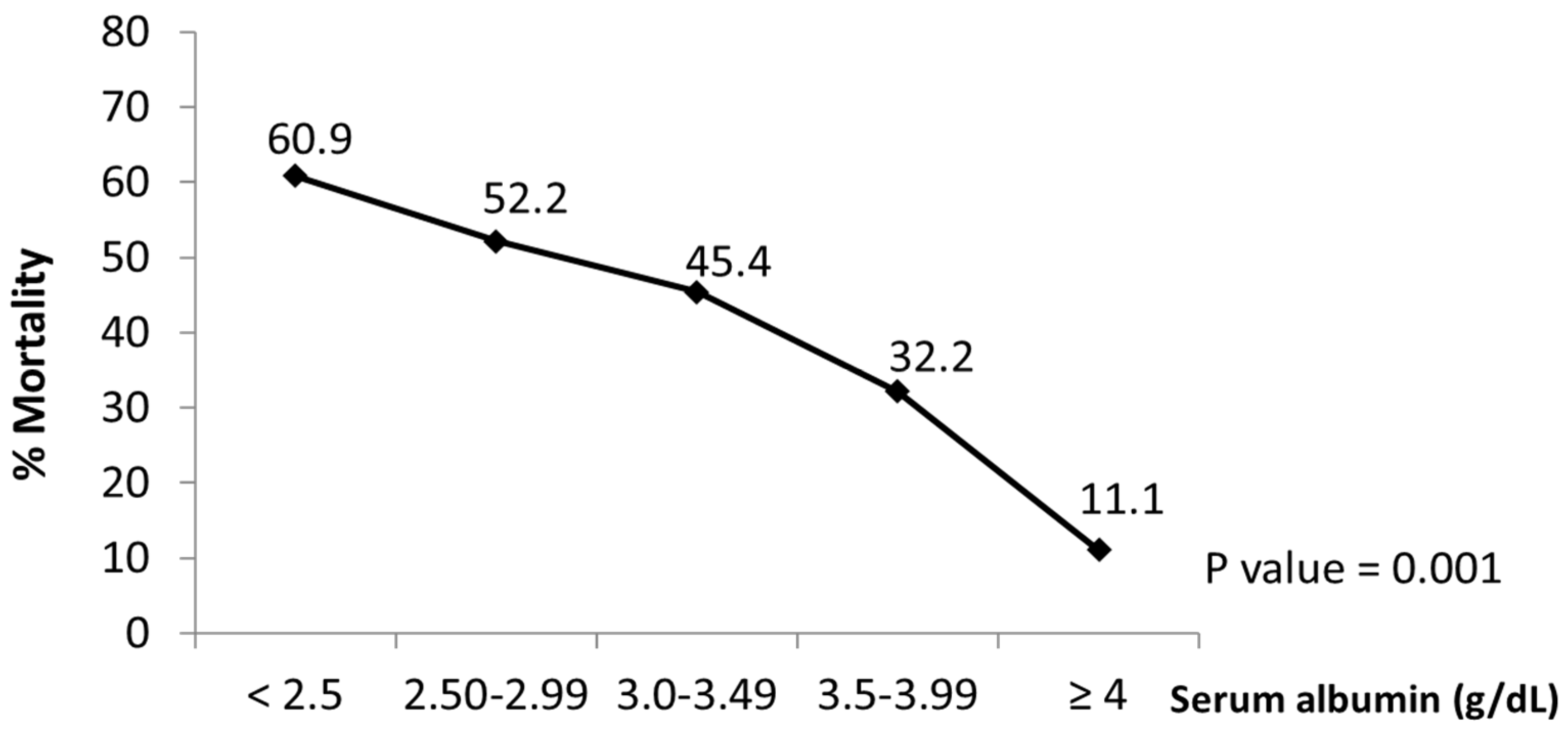
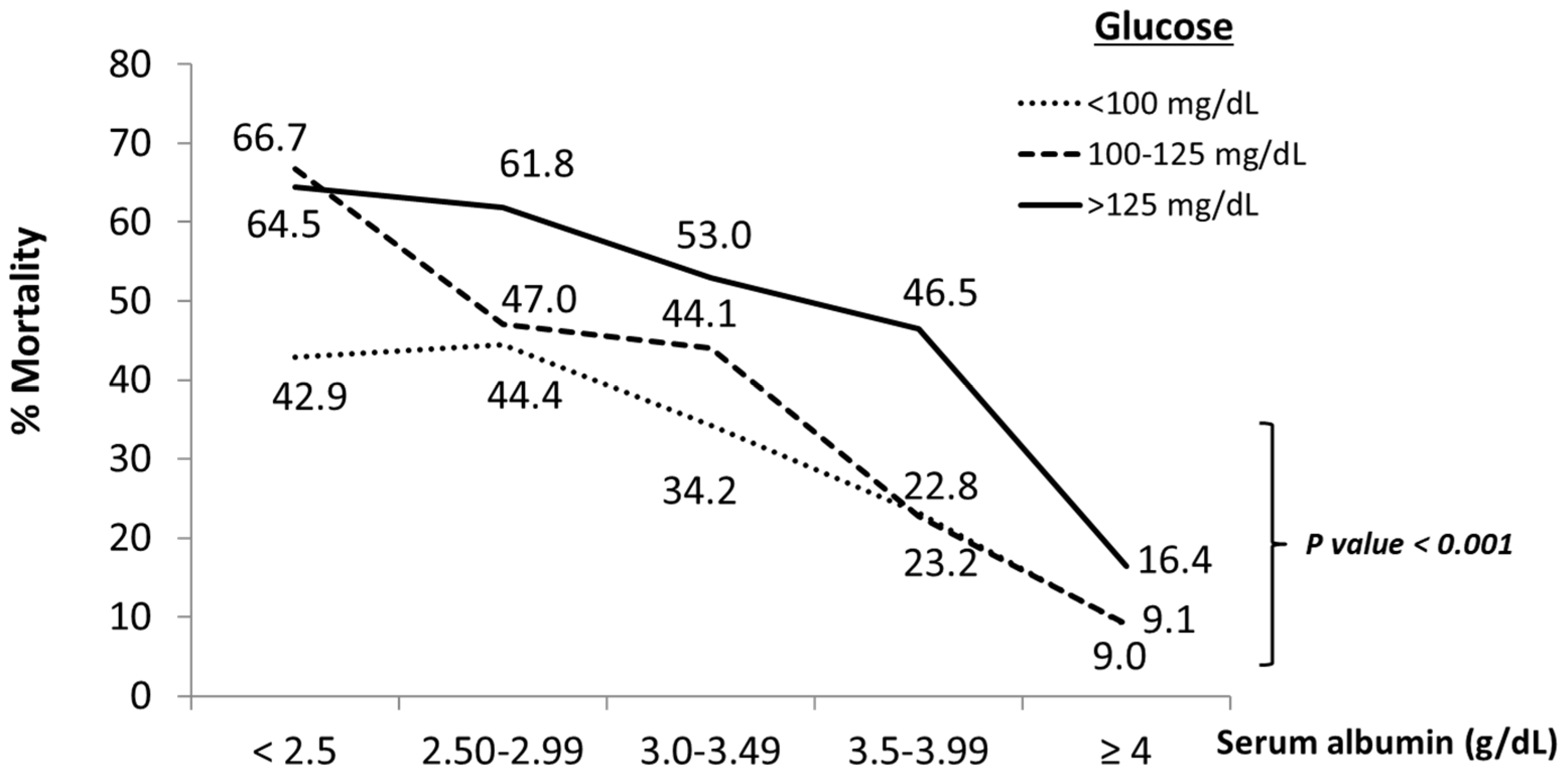
3.3. Relationship between On-Admission Serum Albumin Levels and In-Hospital Mortality
3.4. Binding of SARS-CoV-2 Spike Subunits to Albumin
4. Discussion
5. Comments and Study Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oettl, K.; Birner-Gruenberger, R.; Spindelboeck, W.; Stueger, H.P.; Dorn, L.; Stadlbauer, V.; Putz-Bankuti, C.; Krisper, P.; Graziadei, I.; Vogel, W.; et al. Oxidative albumin damage in chronic liver failure: Relation to albumin binding capacity, liver dysfunction and survival. J. Hepatol. 2013, 59, 978–983. [Google Scholar] [CrossRef]
- Lu, X.; Yao, G.; Tian, Y.F. The interaction between native serum albumin and hepatitis B virus. Arch. Virol. 1988, 98, 163–170. [Google Scholar] [PubMed]
- Fuhrman, M.; Charney, P.; Mueller, C.M. Hepatic proteins and nutrition assessment. J. Am. Diet. Assoc. 2004, 104, 1258–1264. [Google Scholar] [CrossRef] [PubMed]
- Ishida, S.; Hashimoto, I.; Seike, T.; Abe, Y.; Nakaya, Y.; Nakanishi, H. Serum albumin levels correlate with inflammation rather than nutrition supply in burns patients: A retrospective study. J. Med. Investig. 2014, 61, 361–368. [Google Scholar] [CrossRef] [Green Version]
- Vincent, J.L.; Dubois, M.J.; Navickis, R.J.; Wilkes, M.M. Hypoalbuminemia in acute illness: Is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann. Surg. 2003, 237, 319–334. [Google Scholar] [CrossRef] [PubMed]
- Challen, R.; Brooks-Pollock, E.; Read, J.M.; Dyson, L.; Tsaneva-Atanasova, K.; Danon, L. Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: Matched cohort study. BMJ 2021, 372, n579. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Cheng, A.; Kumar, R.; Fang, Y.; Chen, G.; Zhu, Y.; Lin, S. Hypoalbuminemia predicts the outcome of COVID-19 independent of age and co-morbidity. J. Med. Virol. 2020, 92, 2152–2158. [Google Scholar] [CrossRef]
- Li, J.; Li, M.; Zheng, S.; Li, M.; Zhang, M.; Sun, M.; Li, X.; Deng, A.; Cai, Y.; Zhang, H. Plasma albumin levels predict risk for nonsurvivors in critically ill patients with COVID-19. Biomark. Med. 2020, 14, 827–837. [Google Scholar] [CrossRef]
- Arasteh, A.; Farahi, S.; Habibi-Rezaei, M.; Moosavi-Movahedi, A.A. Glycated albumin: An overview of the In Vitro models of an In Vivo potential disease marker. J. Diabetes Metab. Disord. 2014, 13, 49. [Google Scholar] [CrossRef] [Green Version]
- Blache, D.; Bourdon, E.; Salloignon, P.; Lucchi, G.; Ducoroy, P.; Petit, J.-M.; Verges, B.; Lagrost, L. Glycated Albumin with Loss of Fatty Acid Binding Capacity Contributes to Enhanced Arachidonate Oxygenation and Platelet Hyperactivity: Relevance in Patients with Type 2 Diabetes. Diabetes 2015, 64, 960–972. [Google Scholar] [CrossRef] [Green Version]
- Carrasco-Sánchez, F.J.; López-Carmona, M.D.; Martínez-Marcos, F.J.; Pérez-Belmonte, L.M.; Hidalgo-Jiménez, A.; Buonaiuto, V.; Suárez Fernández, C.; Freire, C.S.J.; Luordo, D.; Pesqueira, F.P.M.; et al. Admission hyperglycaemia as a predictor of mortality in patients hospitalized with COVID-19 regardless of diabetes status: Data from the Spanish SEMI-COVID-19 Registry. Ann. Med. 2021, 53, 103–116. [Google Scholar] [CrossRef]
- Di Fiore, F.; Lecleire, S.; Pop, D.; Rigal, O.; Hamidou, H.; Paillot, B.; Ducrotte, P.; Lerebours, E.; Michel, P. Baseline nutritional status is predictive of response to treatment and survival in patients treated by definitive chemoradiotherapy for a locally advanced esophageal cancer. Am. J. Gastroenterol. 2007, 102, 2557–2563. [Google Scholar] [CrossRef]
- Ishizuka, M.; Nagata, H.; Takagi, K.; Horie, T.; Kubota, K. Inflammation-Based Prognostic Score Is a Novel Predictor of Postoperative Outcome in Patients with Colorectal Cancer. Ann. Surg. 2007, 246, 1047–1051. [Google Scholar] [CrossRef]
- Dosch, S.F.; Mahajan, S.D.; Collins, A.R. SARS coronavirus spike protein-induced innate immune response occurs via activation of the NF-kappaB pathway in human monocyte macrophagesinvitro. Virus Res. 2009, 142, 19–27. [Google Scholar] [CrossRef]
- Buzhdygan, T.P.; DeOre, B.J.; Baldwin-Leclair, A.; Bullock, T.A.; McGary, H.M.; Khan, J.A.; Razmpour, R.; Hale, J.F.; Galie, P.A.; Potula, R. Andrews AM, Ramirez SH. The SARS-CoV-2 spike protein alters barrier function in 2D static and 3D microfluidic in-vitro models of the human blood-brain barrier. Neurobiol. Dis. 2020, 146, 105131. [Google Scholar] [CrossRef]
- Mesas, A.E.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Cabrera, M.A.S.; De Andrade, S.M.; Sequí-Dominguez, I.; Martínez-Vizcaíno, V. Predictors of in-hospital COVID-19 mortality: A comprehensive systematic review and meta-analysis exploring differences by age, sex and health conditions. PLoS ONE 2020, 15, e0241742. [Google Scholar] [CrossRef]
- Kuderer, N.M.; Choueiri, T.K.; Shah, D.P.; Shyr, Y.; Rubinstein, S.M.; Rivera, D.R.; Shete, S.; Hsu, C.Y.; Desai, A.; de Lima Lopes, G., Jr.; et al. COVID-19 and Cancer Consortium. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet 2020, 395, 1907–1918. [Google Scholar]
- Viana-Llamas, M.C.; Arroyo-Espliguero, R.; Silva-Obregón, J.A.; Uribe-Heredia, G.; Núñez-Gil, I.; García-Magallón, B.; Torán-Martínez, C.G.; Castillo-Sandoval, A.; Díaz-Caraballo, E.; Rodríguez-Guinea, I.; et al. Hypoalbuminemia on admission in COVID-19 infection: An early predictor of mortality and adverse events. A retrospective observational study. Med. Clin. 2021, 156, 428–436. [Google Scholar] [CrossRef]
- Ceriello, A.; De Nigris, V.; Prattichizzo, F. Why is hyperglycaemia worsening COVID -19 and its prognosis? Diabetes Obes. Metab. 2020, 22, 1951–1952. [Google Scholar] [CrossRef]
- Aziz, M.; Fatima, R.; Lee-Smith, W.; Assaly, R. The association of low serum albumin level with severe COVID-19: A systematic review and meta-analysis. Crit. Care 2020, 24, 255. [Google Scholar] [CrossRef]
- Kheir, M.; Saleem, F.; Wang, C.; Mann, A.; Chua, J. Higher albumin levels on admission predict better prognosis in patients with confirmed COVID-19. PLoS ONE 2021, 16, e0248358. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zheng, L.; Liu, L.; Zhao, M.; Xiao, J.; Zhao, Q. Liver impairment in COVID-19 patients: A retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver Int. 2020, 40, 2095–2103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moshage, H.J.; Janssen, J.A.; Franssen, J.H.; Hafkenscheid, J.C.; Yap, S.H. Study of the molecular mechanism of decreased liver synthesis of albumin in inflammation. J. Clin. Investig. 1987, 79, 1635–1641. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Li, C.; Wang, Z.; Wang, H.; Zhou, N.; Jiang, J. Decreased serum albumin level indicates poor prognosis of COVID-19 patients: Hepatic injury analysis from 2623 hospitalized cases. Sci. China Life Sci. 2020, 63, 1678–1687. [Google Scholar] [CrossRef]
- Fleck, A.; Hawker, F.; Wallace, P.; Raines, G.; Trotter, J.; Ledingham, I.; Calman, K. Increased vascular permeability: A major cause of hypoalbuminaemia in disease and injury. Lancet 1985, 1, 781–784. [Google Scholar] [CrossRef]
- Soeters, P.B.; Wolfe, R.R.; Shenkin, A. Hypoalbuminemia: Pathogenesis and Clinical Significance. J. Parenter. Enter. Nutr. 2019, 43, 181–193. [Google Scholar] [CrossRef] [Green Version]
- Sharifpour, M.; Rangaraju, S.; Liu, M.; Alabyad, D.; Nahab, F.B.; Creel-Bulos, C.M.; Jabaley, C.S.; on behalf of the Emory COVID-19 Quality & Clinical Research Collaborative. C-Reactive protein as a prognostic indicator in hospitalized patients with COVID-19. PLoS ONE 2020, 15, e0242400. [Google Scholar] [CrossRef]
- Wang, L. C-reactive protein levels in the early stage of COVID-19. Méd. Mal. Infect. 2020, 50, 332–334. [Google Scholar] [CrossRef]
- Gajahi, S.A.; Catan, A.; Giraud, P.; Assouan, K.S.; Guerin-Dubourg, A.; Debussche, X.; Le Moullec, N.; Bourdon, E.; Bravo, S.B.; Paradela-Dobarro, B.; et al. Glycation of human serum albumin impairs binding to the glucagon-like peptide-1 analogue liraglutide. J. Biol. Chem. 2018, 293, 4778–4791. [Google Scholar] [CrossRef] [Green Version]
- Song, S.O.; Hwang, Y.-C.; Ahn, K.J.; Cha, B.S.; Song, Y.D.; Lee, D.W.; Lee, B.-W. Clinical Characteristics of Patients Responding to Once-Daily Basal Insulin Therapy in Korean Subjects with Type 2 Diabetes. Diabetes Ther. 2015, 6, 547–558. [Google Scholar] [CrossRef] [Green Version]
- Atassi, M.Z.; Sakata, S.; Sakata, S. Immune recognition of serum albumin. XVI. Role of adjuvant in the autoimmune response to mouse serum albumin. Mol. Immunol. 1982, 19, 1509–1512. [Google Scholar] [CrossRef]
- Wilde, B.; Katsounas, A. Immune Dysfunction and Albumin-Related Immunity in Liver Cirrhosis. Mediat. Inflamm. 2019, 2019, 7537649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krishnan, S.; Nordqvist, H.; Ambikan, A.T.; Gupta, S.; Sperk, M.; Svensson-Akusjärvi, S.; Mikaeloff, F.; Benfeitas, R.; Saccon, E.; Ponnan, S.M.; et al. Metabolic Perturbation Associated With COVID-19 Disease Severity and SARS-CoV-2 Replication. Mol. Cell Proteom. 2021, 20, 100159. [Google Scholar] [CrossRef] [PubMed]
- Kermali, M.; Khalsa, R.K.; Pillai, K.; Ismail, Z.; Harky, A. The role of biomarkers in diagnosis of COVID-19–A systematic review. Life Sci. 2020, 254, 117788. [Google Scholar] [CrossRef]
| Variables | Categories | COVID-19 Population n = 1555 N (%) | |
|---|---|---|---|
| Age groups (years) | 18–49 | 287 (18.5) | |
| 50–69 | 494 (31.8) | ||
| 70–84 | 405 (26.0) | ||
| ≥85 | 369 (23.7) | ||
| Gender | Male | 898 (57.7) | |
| Female | 657 (42.3) | ||
| Diseases | Hypertension | No | 767 (49.3) |
| Yes | 788 (50.7) | ||
| Dyslipidemia | No | 986 (63.4) | |
| Yes | 569 (36.6) | ||
| Diabetes mellitus | No | 1157 (74.4) | |
| Yes | 398 (25.6) | ||
| Active cancer | No | 1442 (92.7) | |
| Yes | 113 (7.3) | ||
| COPD | No | 1400 (90.0) | |
| Yes | 155 (10.0) | ||
| ICU admission | No | 1381 (88.8) | |
| Yes | 174 (11.2) | ||
| Outcome | Discharged | 1052 (67.7) | |
| Death | 503 (32.3) | ||
| Variables | Categories | Death | p Value | ||
|---|---|---|---|---|---|
| Not n = 1052 N (%) | Yes n = 503 N (%) | ||||
| Age groups (years) | 18–49 | 272 (94.8) | 15 (5.2) | <0.001 | |
| 50–69 | 424 (85.5) | 70 (14.2) | |||
| 70–84 | 228 (56.3) | 177 (43.7) | |||
| ≥85 | 128 (34.7) | 241 (65.3) | |||
| Gender | Male | 598 (66.6) | 300 (33.4) | 0.296 | |
| Female | 454 (69.1) | 203 (30.9) | |||
| Diseases | |||||
| Hypertension | No | 595 (77.6) | 172 (22.4) | <0.001 | |
| Yes | 457 (58.0) | 331 (42.0) | |||
| Dyslipidemia | No | 713 (72.3) | 273 (27.7) | <0.001 | |
| Yes | 339 (59.6) | 230 (40.4) | |||
| Diabetes mellitus | No | 826 (71.4) | 331 (28.6) | <0.001 | |
| Yes | 226 (56.8) | 172 (43.2) | |||
| Active cancer | No | 1009 (70.0) | 433 (30.0) | <0.001 | |
| Yes | 43 (38.1) | 70 (61.9) | |||
| COPD | No | 979 (69.9) | 421 (30.1) | <0.001 | |
| Yes | 73 (47.1) | 82 (52.9) | |||
| ICU admission | No | 975 (70.6) | 46 (29.4) | <0.001 | |
| Yes | 77 (44.3) | 97 (55.7) | |||
| at Admission Parameters | |||||
| Albumin (g/dL) | <3.5 | 304 (50.9) | 293 (49.1) | <0.001 | |
| ≥3.5 | 748 (78.1) | 210 (21.9) | |||
| Glucose (mg/dL) | <100 | 232 (74.8) | 78 (25.2) | <0.001 | |
| 100–125 | 387 (72.9) | 144 (27.1) | |||
| >125 | 363 (57.0) | 274 (43.0) | |||
| C-Reactive Protein (mg/dL) | ≤0.5 | 30 (71.4) | 12 (28.6) | 0.391 | |
| >0.5 | 439 (64.9) | 237 (35.1) | |||
| Variables | Categories | Crude | Age Adjusted | Full Adjusted * | |||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | p Value | OR (95%CI) | p Value | OR (95%CI) | p Value | ||
| Age groups | 18–49 | 1 | NA | NA | 1 | ||
| 50–69 | 2.99 (1.68–5.34) | <0.001 | 1.85 (0.97–3.52) | 0.060 | |||
| 70–84 | 14.07 (8.07–24.53) | <0.001 | 11.70 (6.09–22.52) | <0.001 | |||
| ≥85 | 34.14 (19.45–59.90) | <0.001 | 40.63 (20.86–79.15) | <0.001 | |||
| Gender | Male | 1 | 0.296 | 1 | <0.001 | 1 | |
| Female | 0.891 (0.72–1.11) | 0.618 (0.48–0.80) | 0.74 (0.56–0.99) | 0.041 | |||
| Active Cancer | No | 1 | 1 | 1 | |||
| Yes | 3.79 (2.55–5.64) | <0.001 | 3.33 (2.13–5.21) | <0.001 | 3.87 (2.34–6.42) | <0.001 | |
| Dyslipidemia | No | 1 | 1 | 1 | |||
| Yes | 1.77 (1.42–2.20) | <0.001 | 1.07 (0.83–1.37) | 0.601 | 1.06 (0.79–1.43) | 0.688 | |
| Diabetes | No | 1 | 1 | 1 | |||
| Yes | 1.90 (1.50–2.40) | <0.001 | 1.20 (0.92–1.57) | 0.179 | 1.03 (0.75–1.42) | 0.866 | |
| Hypertension | No | 1 | 1 | 1 | |||
| Yes | 2.50 (2.00–3.12) | <0.001 | 0.79 (0.60–1.04) | 0.100 | 0.86 (0.62–1.19) | 0.368 | |
| COPD | No | 1 | 1 | 1 | |||
| Yes | 2.61 (1.87–3.65) | <0.001 | 1.46 (1.01–2.10) | 0.043 | 1.02 (0.67–1.54) | 0.930 | |
| ICU admissions | No | 1 | 1 | 1 | |||
| Yes | 3.03 (2.20–4.17) | <0.001 | 8.96 (5.94–13.51) | <0.001 | 8.76 (5.68–13.50) | <0.001 | |
| Albumin (g/dL) | <3.5 | 1 | 1 | 1 | |||
| ≥3.5 | 0.29 (0.23–0.36) | <0.001 | 0.44 (0.34–0.56) | <0.001 | 0.48 (0.36–0.62) | <0.001 | |
| Glucose (mg/dL) | <100 | 1 | 1 | 1 | |||
| 100–125 | 1.11 (0.80–1.52) | 0.535 | 1.00 (0.68–1.45) | 0.990 | 1.02 (0.69–1.51) | 0.937 | |
| >125 | 2.24 (1.66–3.03) | <0.001 | 1.63 (1.15–2.32) | 0.006 | 1.56 (1.07–2.29) | 0.022 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zekri-Nechar, K.; Zamorano-León, J.J.; Segura-Fragoso, A.; Alcaide, J.R.; Reche, C.; Andrés-Castillo, A.; Martínez-Martínez, C.H.; Giner, M.; Jiménez-García, R.; López-de-Andrés, A.; et al. Albumin Binds COVID-19 Spike 1 Subunit and Predicts In-Hospital Survival of Infected Patients—Possible Alteration by Glucose. J. Clin. Med. 2022, 11, 587. https://doi.org/10.3390/jcm11030587
Zekri-Nechar K, Zamorano-León JJ, Segura-Fragoso A, Alcaide JR, Reche C, Andrés-Castillo A, Martínez-Martínez CH, Giner M, Jiménez-García R, López-de-Andrés A, et al. Albumin Binds COVID-19 Spike 1 Subunit and Predicts In-Hospital Survival of Infected Patients—Possible Alteration by Glucose. Journal of Clinical Medicine. 2022; 11(3):587. https://doi.org/10.3390/jcm11030587
Chicago/Turabian StyleZekri-Nechar, Khaoula, José J. Zamorano-León, Antonio Segura-Fragoso, José R. Alcaide, Carmen Reche, Alcira Andrés-Castillo, Carlos H. Martínez-Martínez, Manel Giner, Rodrigo Jiménez-García, Ana López-de-Andrés, and et al. 2022. "Albumin Binds COVID-19 Spike 1 Subunit and Predicts In-Hospital Survival of Infected Patients—Possible Alteration by Glucose" Journal of Clinical Medicine 11, no. 3: 587. https://doi.org/10.3390/jcm11030587
APA StyleZekri-Nechar, K., Zamorano-León, J. J., Segura-Fragoso, A., Alcaide, J. R., Reche, C., Andrés-Castillo, A., Martínez-Martínez, C. H., Giner, M., Jiménez-García, R., López-de-Andrés, A., Navarro-Cuellar, C., García-Fernández, M. A., & López-Farré, A. (2022). Albumin Binds COVID-19 Spike 1 Subunit and Predicts In-Hospital Survival of Infected Patients—Possible Alteration by Glucose. Journal of Clinical Medicine, 11(3), 587. https://doi.org/10.3390/jcm11030587








