Minimally Invasive versus Full Sternotomy SAVR in the Era of TAVR: An Institutional Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Data Collection
2.3. Surgical Procedure
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Svensson, L.G.; Tuzcu, M.; Kapadia, S.; Blackstone, E.H.; Roselli, E.E.; Gillinov, A.M.; Sabik, J.F.; Lytle, B.W. A comprehensive review of the PARTNER trial. J. Thorac. Cardiovasc. Surg. 2013, 145, S11–S16. [Google Scholar] [CrossRef] [Green Version]
- Reardon, M.J.; Van Mieghem, N.M.; Popma, J.J.; Kleiman, N.S.; Søndergaard, L.; Mumtaz, M.; Adams, D.H.; Deeb, G.M.; Maini, B.; Gada, H.; et al. Surgical or Transcatheter Aortic-Valve Replacement in Intermediate-Risk Patients. N. Engl. J. Med. 2017, 376, 1321–1331. [Google Scholar] [CrossRef]
- Tsigkas, G.; Despotopoulos, S.; Makris, A.; Koniari, I.; Armylagos, S.; Davlouros, P.; Hahalis, G. Transcatheter versus surgical aortic valve replacement in severe, symptomatic aortic stenosis. J. Geriatr. Cardiol. 2018, 15, 76–85. [Google Scholar] [CrossRef]
- Nishimura, R.A.; Otto, C.M.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Guyton, R.A.; O’Gara, P.T.; Ruiz, C.E.; Skubas, N.J.; Sorajja, P.; et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: A report of the American college of cardiology/American heart association task force on practice guidelines. J. Am. Coll. Cardiol. 2014, 63, e57–e185. [Google Scholar] [CrossRef] [Green Version]
- Autschbach, R.; Walther, T. Conventional Aortic Valve Replacement: Standard Therapy in the 1990s and the Development of Minimally Invasive Approaches. Thorac. Cardiovasc. Surg. 2017, 65, S183–S186. [Google Scholar] [CrossRef] [PubMed]
- Cosgrove, D.M., III; Sabik, J.F. Minimally Invasive Approach for Aortic Valve Operations. Ann. Thorac. Surg. 1996, 62, 596–597. [Google Scholar] [CrossRef]
- Kirmani, B.H.; Jones, S.G.; Malaisrie, S.C.; Chung, D.A.; Williams, R.J. Limited versus full sternotomy for aortic valve replacement. Cochrane Database Syst. Rev. 2017, 2017, CD011793. [Google Scholar] [CrossRef] [PubMed]
- Gilmanov, D.; Bevilacqua, S.; Murzi, M.; Cerillo, A.G.; Gasbarri, T.; Kallushi, E.; Miceli, A.; Glauber, M. Minimally Invasive and Conventional Aortic Valve Replacement: A Propensity Score Analysis. Ann. Thorac. Surg. 2013, 96, 837–843. [Google Scholar] [CrossRef]
- Glauber, M.; Ferrarini, M.; Miceli, A. Minimally invasive aortic valve surgery: State of the art and future directions. Ann. Cardiothorac. Surg. 2015, 4, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Khoshbin, E.; Prayaga, S.; Kinsella, J.; Sutherland, F.W.H. Mini-sternotomy for aortic valve replacement reduces the length of stay in the cardiac intensive care unit: Meta-analysis of randomised controlled trials. BMJ Open 2011, 1, e000266. [Google Scholar] [CrossRef] [Green Version]
- Mihaljevic, T.; Cohn, L.H.; Unic, D.; Aranki, S.F.; Couper, G.S.; Byrne, J.G. One Thousand Minimally Invasive Valve Operations: Early and late results. Ann. Surg. 2004, 240, 529–534. [Google Scholar] [CrossRef]
- Semsroth, S.; Gothe, R.M.; Raith, Y.R.; De Brabandere, K.; Hanspeter, E.; Kilo, J.; Kofler, M.; Müller, L.; Ruttman-Ulmer, E.; Grimm, M. Comparison of Two Minimally Invasive Techniques and Median Sternotomy in Aortic Valve Replacement. Ann. Thorac. Surg. 2017, 104, 877–883. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, M.L.; Mckellar, S.; Sundt, T.M.; Schaff, H. Ministernotomy versus conventional sternotomy for aortic valve replacement: A systematic review and meta-analysis. J. Thorac. Cardiovasc. Surg. 2009, 137, 670–679.e5. [Google Scholar] [CrossRef] [Green Version]
- Murtuza, B.; Pepper, J.R.; DeL Stanbridge, R.; Jones, C.; Rao, C.; Darzi, A.; Athanasiou, T. Minimal Access Aortic Valve Replacement: Is It Worth It? Ann. Thorac. Surg. 2008, 85, 1121–1131. [Google Scholar] [CrossRef] [PubMed]
- Phan, K.; Xie, A.; DI Eusanio, M.; Yan, T.D. A Meta-Analysis of Minimally Invasive Versus Conventional Sternotomy for Aortic Valve Replacement. Ann. Thorac. Surg. 2014, 98, 1499–1511. [Google Scholar] [CrossRef]
- Nezafati, M.H.; Kahrom, M.; Nezafati, P. Minimally Invasive Aortic Valve Surgery. SMGroup 2016, 1–17. [Google Scholar]
- Nair, S.K.; Sudarshan, C.D.; Thorpe, B.S.; Singh, J.; Pillay, T.; Catarino, P.; Valchanov, K.; Codispoti, M.; Dunning, J.; Abu-Omar, Y.; et al. Mini-Stern Trial: A randomized trial comparing mini-sternotomy to full median sternotomy for aortic valve replacement. J. Thorac. Cardiovasc. Surg. 2018, 156, 2124–2132.e31. [Google Scholar] [CrossRef]
- Olds, A.; Saadat, S.; Azzolini, A.; Dombrovskiy, V.; Odroniec, K.; Lemaire, A.; Ghaly, A.; Lee, L.Y. Improved operative and recovery times with mini-thoracotomy aortic valve replacement. J. Cardiothorac. Surg. 2019, 14, 91. [Google Scholar] [CrossRef] [Green Version]
- Ghanta, R.K.; Lapar, D.J.; Kern, J.A.; Kron, I.L.; Speir, A.M.; Fonner, E.; Quader, M.; Ailawadi, G. Minimally invasive aortic valve replacement provides equivalent outcomes at reduced cost compared with conventional aortic valve replacement: A real-world multi-institutional analysis. J. Thorac. Cardiovasc. Surg. 2015, 149, 1060–1065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabata, M.; Umakanthan, R.; Cohn, L.H.; Bolman, R.M., III; Shekar, P.S.; Chen, F.Y.; Couper, G.S.; Aranki, S.F. Early and late outcomes of 1000 minimally invasive aortic valve operations. Eur. J. Cardio-Thoracic Surg. 2008, 33, 537–541. [Google Scholar] [CrossRef] [Green Version]
- Aris, A.; Cámara, M.L.; Montiel, J.; Delgado, L.J.; Galán, J.; Litvan, H. Ministernotomy versus median sternotomy for aortic valve replacement: A prospective, randomized study. Ann. Thorac. Surg. 1999, 67, 1583–1587. [Google Scholar] [CrossRef]
- Bethencourt, D.M.; Le, J.; Rodriguez, G.; Kalayjian, R.W.; Thomas, G.S. Minimally Invasive Aortic Valve Replacement via Right Anterior Minithoractomy and Central Aortic Cannulation A 13-Year Experience. Innovations 2017, 12, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Neely, R.C.; Boskovski, M.T.; Gosev, I.; Kaneko, T.; McGurk, S.; Leacche, M.; Cohn, L.H. Minimally invasive aortic valve replacement versus aortic valve replacement through full sternotomy: The Brigham and Women’s Hospital experience. Ann. Cardiothorac. Surg. 2015, 4, 38–48. [Google Scholar] [CrossRef] [PubMed]
| Surgical Approach | |||
|---|---|---|---|
| FS (n = 60) | MI (n = 53) | p-Value | |
| Patients, n (%) | 60 (53.1) | 53 (46.9) | |
| Age, y (SD) | 58.7 (13.19) | 60.89 (11.73) | 0.353 |
| BMI, (SD) | 30.68 (6.89) | 29.04 (4.56) | 0.136 |
| Gender | 1 | ||
| Male, n (%) | 39 (65) | 34 (64.15) | |
| Female, n (%) | 21 (35) | 19 (35.85) | |
| Primary Diagnosis | 0.477 | ||
| AS, n (%) | 48 (80) | 46 (86.79) | |
| AI, n (%) | 12 (20) | 7 (13.21) | |
| Preoperative LVEF (SD) | 57.7 (10.87) | 59.72 (10.4) | 0.316 |
| Diabetes, n (%) | 20 (33.3) | 6 (11.32) | 0.01 |
| Hypertension, n (%) | 33 (55) | 27 (50.94) | 0.81 |
| CAD, n (%) | 9 (15) | 5 (9.43) | 0.542 |
| Hyperlipidemia, n (%) | 26 (43.33) | 25 (47.17) | 0.826 |
| Renal Failure, n (%) | 4 (6.67) | 3 (5.66) | 1 |
| CHF, n (%) | 4 (6.67) | 3 (5.66) | 1 |
| Cerebrovascular Disease, n (%) | 0 (0) | 0 (0) | |
| Previous Stroke, n (%) | 4 (6.67) | 3 (5.66) | 1 |
| Current Smoker, n (%) | 5 (8.33) | 6 (11.32) | 0.828 |
| Previous Smoker, n (%) | 22 (36.67) | 15 (28.3) | 0.456 |
| BAV, n (%) | 27 (45) | 33 (62.26) | 0.1 |
| Surgical Approach | p-Value | ||
|---|---|---|---|
| FS | MI | ||
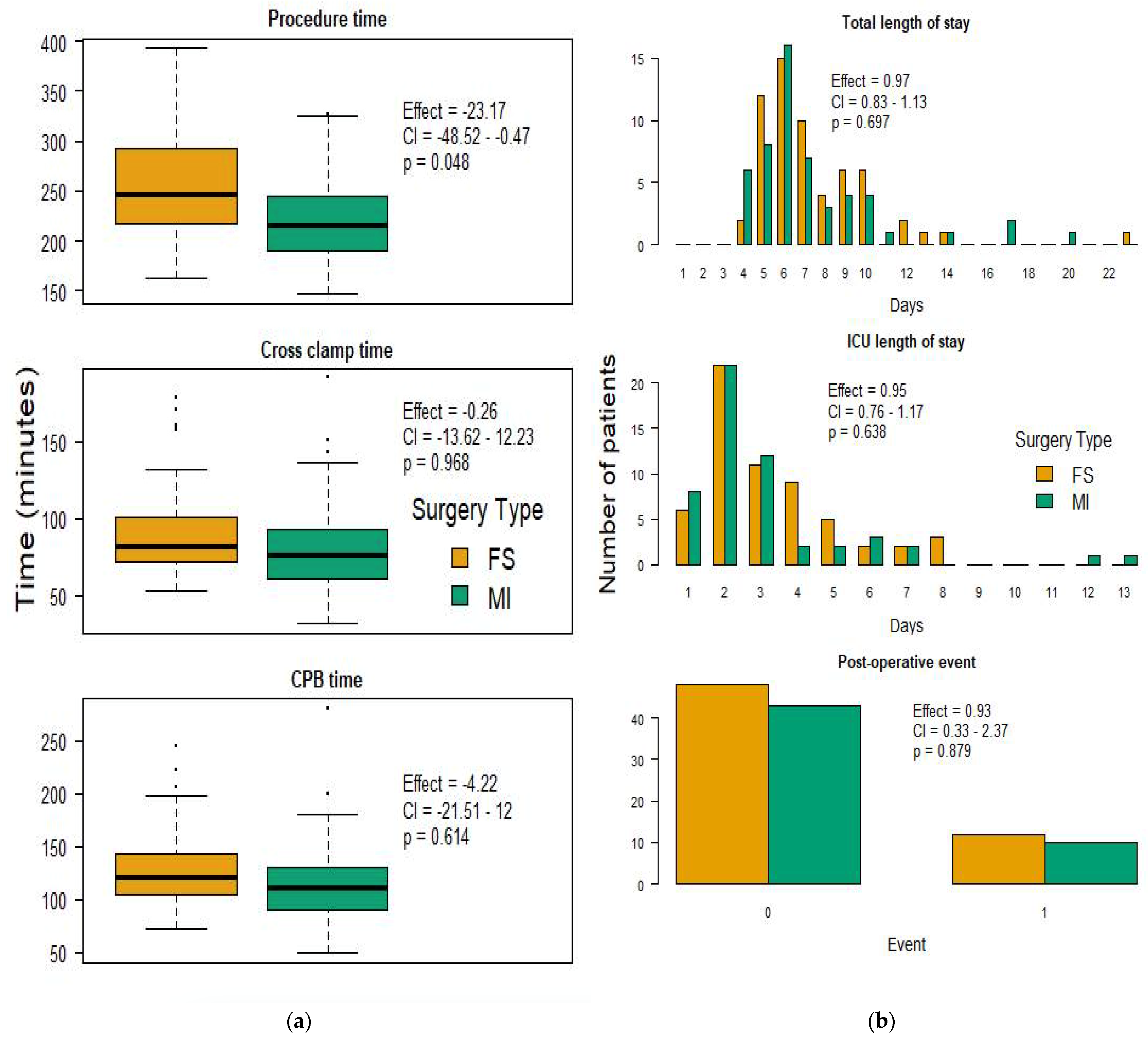
| Procedure length (min), median (IQR) | 247 (217.25–292) | 216 (190–244) | 0.048 |
| CPB time (min), median (IQR) | 120 (104–142.25) | 111 (90–131) | 0.613 |
| Cross-clamp time (min), median (IQR) | 82 (72–101) | 76 (61–93) | 0.968 |
| Mean aortic gradient, median (IQR) | 11 (9–13.6) | 10.7 (9.15–13.73) | 0.712 |
| ICU LOS (days), median (IQR) | 3 (2–4) | 2 (2–3) | 0.636 |
| Total hospital LOS (days), median (IQR) | 7 (6–9) | 6 (5–8) | 0.697 |
| Aortic valve reintervention, n (%) | 1 (1.67) | 3 (5.66) | 0.280 |
| Atrial fibrillation, n (%) | 15 (25) | 18 (33.96) | 0.297 |
| Postoperative event, n (%) | 12 (20) | 10 (18.87) | 0.879 |
| Stroke, n (%) | 0 (0) | 2 (3.77) | 0.422 |
| Bleeding requiring transfusion, n (%) | 6 (10) | 0 (0) | 0.052 |
| Deep sternal wound infection, n (%) | 1 (1.67) | 0 (0) | 1 |
| Acute kidney injury, n (%) | 3 (5) | 2 (3.77) | 1 |
| 30-day readmission, n (%) | 8 (13.33) | 6 (11.32) | 0.97 |
| 30-day mortality, n (%) | 0 (0) | 1 (1.89) | 0.95 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilson, T.W.; Horns, J.J.; Sharma, V.; Goodwin, M.L.; Kagawa, H.; Pereira, S.J.; McKellar, S.H.; Selzman, C.H.; Glotzbach, J.P. Minimally Invasive versus Full Sternotomy SAVR in the Era of TAVR: An Institutional Review. J. Clin. Med. 2022, 11, 547. https://doi.org/10.3390/jcm11030547
Wilson TW, Horns JJ, Sharma V, Goodwin ML, Kagawa H, Pereira SJ, McKellar SH, Selzman CH, Glotzbach JP. Minimally Invasive versus Full Sternotomy SAVR in the Era of TAVR: An Institutional Review. Journal of Clinical Medicine. 2022; 11(3):547. https://doi.org/10.3390/jcm11030547
Chicago/Turabian StyleWilson, Tyler W., Joshua J. Horns, Vikas Sharma, Matthew L. Goodwin, Hiroshi Kagawa, Sara J. Pereira, Stephen H. McKellar, Craig H. Selzman, and Jason P. Glotzbach. 2022. "Minimally Invasive versus Full Sternotomy SAVR in the Era of TAVR: An Institutional Review" Journal of Clinical Medicine 11, no. 3: 547. https://doi.org/10.3390/jcm11030547
APA StyleWilson, T. W., Horns, J. J., Sharma, V., Goodwin, M. L., Kagawa, H., Pereira, S. J., McKellar, S. H., Selzman, C. H., & Glotzbach, J. P. (2022). Minimally Invasive versus Full Sternotomy SAVR in the Era of TAVR: An Institutional Review. Journal of Clinical Medicine, 11(3), 547. https://doi.org/10.3390/jcm11030547






