1. Introduction
Anti-thyroid peroxidase antibodies (TPO-Abs) are known to cause autoimmune thyroiditis. A previous study with three years follow-up of rheumatoid arthritis patients reported a larger carotid intima-media thickness (CIMT) progression in patients TPO-Ab positive than in those TPO-Ab negative. This study also found that TSH levels were higher in TPO-Ab positive patients than in TPO-Ab negative patients [
1].
Subclinical hypothyroidism, defined as increased serum thyroid-stimulating hormone (TSH) concentrations and normal serum free thyroxine levels (free T4), is reported to be positively associated with carotid atherosclerosis [
2]. Therefore, thyroid function could influence the association between TPO-Ab and the progression of atherosclerosis evaluated by CIMT. However, our previous cross-sectional study found a significant positive association between normal TPO-Ab titers (negative) and carotid atherosclerosis (CIMT ≥ 1.1 mm) among euthyroid individuals, defined as having free triiodothyronine (free T3), free T4, and TSH levels with the normal range [
3]. Therefore, independent of thyroid function, high–normal TPO-Ab titers might lead to the development of carotid atherosclerosis.
Atherosclerosis based on CIMT (mm) is an established risk factor for cardiovascular disease [
4,
5,
6]. However, a previous study of 36,984 participants reported no significant associations between yearly CIMT progression (mm/year) and cardiovascular events [
7]. Active arterial wall thickening (CIMT ≥ 0.01 mm/year), which indicates the status of yearly progression of CIMT, is inversely associated with baseline atherosclerosis (CIMT ≥ 1.1 mm), possibly due to the consumption of hematopoietic stem cells (CD34-positive cells) [
8]. CD34-positive cells are known contributors to atherosclerosis; they have been reported to differentiate into macrophages and foam cells [
9].
Since CIMT progression involves the process of endothelial repair, participants with baseline atherosclerosis might have lower endothelial repair activity, resulting in a lower chance of having active arterial wall thickening. Thus, we hypothesized that having a TPO-Ab titer in the normal range is positively associated with baseline atherosclerosis and inversely associated with active arterial wall thickening among euthyroid individuals.
To evaluate this hypothesis, we conducted a prospective study with three years of follow-up (2.8 ± 0.5) of 1069 Japanese individuals aged 40–74 years who participated in an annual health examination in 2014 and had free T3 and free T4 levels in the normal range and negative TPO-Ab titers.
2. Materials and Methods
2.1. Study Population
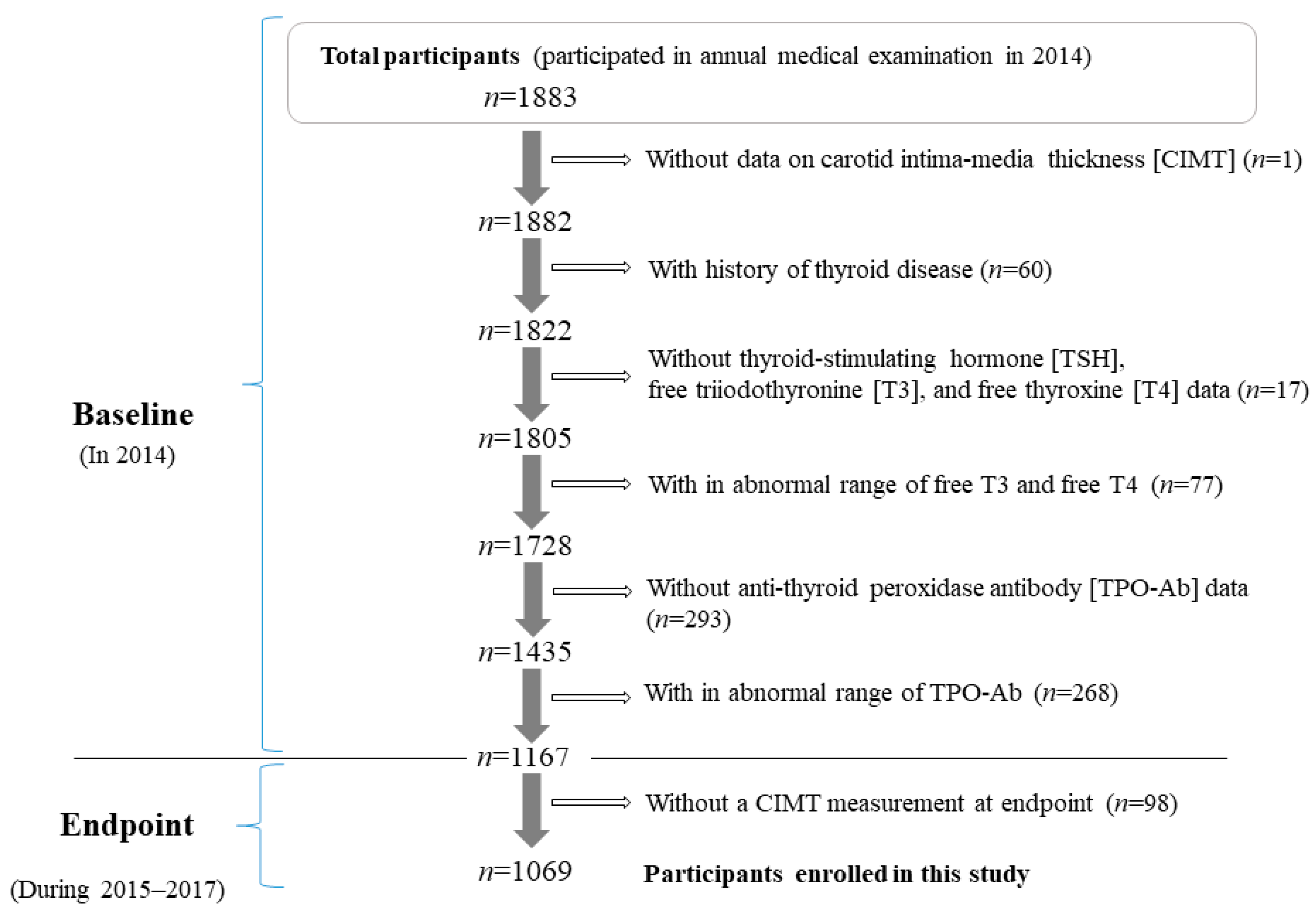
Figure 1 shows the demographics of the study population. The methods related to thyroid function in the present risk survey have been described elsewhere [
3]. The study population comprised 1883 Japanese individuals between the ages of 40 and 74 years from Saza town in western Japan who underwent an annual medical examination in 2014.
One patient without CIMT data (n = 1) was excluded from the present study. To avoid the influence of thyroid disease, participants with a history of thyroid disease (n = 60); participants without thyroid function data on TSH, free T3, and free T4 (n = 17); and participants with abnormal free T3 (normal range: 2.1–4.1 pg/mL) and free T4 (normal range: 1.0–1.7 ng/dL) levels were excluded (n = 77). In addition, participants without TPO-Ab data (n = 293) or abnormal TPO-Ab titers (normal range: <16 IU/mL) (n = 268) were excluded.
Participants who did not undergo an annual medical examination during the follow-up period, 2015–2017 (n = 98) were also excluded. A total of 1069 participants with a mean age of 61.0 years (standard deviation (SD): 8.8 years; range 40–74 years) were included in the study. The follow-up period of this study was 2.8 ± 0.5 years.
Informed consent was obtained from all study participants. This study was approved by the ethics committee of the Nagasaki University Graduate School of Biomedical Sciences (project registration number 14051404). All procedures involving human participants in this study were performed in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki Declaration and its later amendments for comparable ethical standards.
2.2. Data Collection and Laboratory Measurement
Trained interviewers obtained information on clinical characteristics (history of thyroid disease). A fasting blood sample was collected. TSH, free T3, and free T4 levels were measured with chemiluminescent immunoassays at the LSI Medience Corporation (Tokyo, Japan). The normal range for free T3 (2.1–4.1 pg/mL), free T4 (1.0–1.7 ng/dL), and TSH (0.39–4.01 μIU/mL) based on this method were described elsewhere [
10]. TPO-Ab titers were measured using standard procedures (electro chemiluminescence immunoassay) at the LSI Medience Corporation; the normal range (negative) was <16 IU/mL [
10].
An experienced vascular examiner evaluated CIMT of both common carotid arteries using ultrasound inspection equipment: LOGIQ Book XP with a 10-MHz transducer (GE Healthcare, Milwaukee, WI, USA). Maximum values of CIMT in the common carotid arteries were calculated using semi-automated digital edge-detection software (Intimascope; MediaCross, Tokyo, Japan) with a previously described protocol [
11]. Semi-automatically, this software recognized the edges of the internal and external membranes of the artery and determined the distance at a sub-pixel level (estimated to be 0.01 mm) [
12]. We defined active arterial wall thickening as a CIMT increase of ≥0.01 mm/year, as in our previous study [
8]. Furthermore, baseline atherosclerosis was diagnosed as CIMT ≥ 1.1 mm because a normal CIMT value was reported as <1.1 mm in a previous study [
13]. The respective intra-observer variations for CIMT, which were assessed by two examiners, were simple correlation coefficients (r) = 0.91 (
p < 0.01) and r = 0.89 (
p < 0.001), and the inter-observer variation was r = 0.76 (
p < 0.001).
2.3. Statistical Analysis
Characteristics of the study population were expressed as means ± SD except for gender and TSH. Gender was expressed as a percentage. Since the distribution of TSH was skewed, values were expressed as medians (interquartile range). Differences among various variables by sex-specific TPO-Ab tertile in the normal range (negative) were evaluated. Significant differences were evaluated using Student’s t-test for continuous variables and the χ2 test for categorical variables.
Logistic regression was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) to determine associations between baseline atherosclerosis and active arterial wall thickening, TPO-Ab titers in the normal range (negative) and baseline atherosclerosis, and TPO-Ab titers in the normal range (negative) and active arterial wall thickening.
In the analysis of the association between baseline atherosclerosis and active arterial wall thickening and the association between TPO-Ab titers in the normal range (negative) and baseline atherosclerosis, two models were used. Model 1 only adjusted for age and sex. Model 2 included variables in Model 1 plus potential confounding factors directly associated with thyroid function, namely, levels of TSH (μIU/mL) and free T3 (pg/mL).
In the analysis of the association between TPO-Ab titers in the normal range (negative) and active arterial wall thickening, three models were used. Model 1 only adjusted for age and sex. Model 2 included variables in Model 1 and levels of TSH (μIU/mL) and free T3 (pg/mL). Model 3 included variables in Model 2 plus baseline CIMT (mm). We performed a sex-specific analysis as a sensitivity analysis.
The goodness of fit of all logistic regression models in the present study was assessed using the Hosmer–Lemeshow test. All statistical analyses were performed with SAS for Windows (version 9.4: SAS Inc., Cary, NC, USA). Values of p < 0.05 were regarded as statistically significant.
3. Results
Among the present study population (n = 1069), 107 (10.0%) participants were diagnosed as having atherosclerosis at baseline, and 433 (40.5%) were found to have active arterial wall thickening during follow-up.
3.1. Characteristics of the Study Population
Characteristics of the study population by TPO-Ab tertile in the normal range (negative) are shown in
Table 1. Having a normal TPO-Ab titer tertile was significantly positively associated with baseline CIMT but not with thyroid function (free T3, free T4, and TSH).
3.2. Association between Baseline Atherosclerosis and Active Arterial Wall Thickening
Table 2 shows the ORs and 95% CIs of baseline atherosclerosis for active arterial wall thickening. Baseline atherosclerosis is significantly inversely associated with active arterial wall thickening. This association was unchanged even after adjusting for thyroid function.
3.3. Association between TPO-Ab Titers in the Normal Range (Negative) and the Outcomes of Baseline Atherosclerosis and Active Arterial Wall Thickening
Table 3 shows the associations between TPO-Ab titers in the normal range (negative) and baseline atherosclerosis and between TPO-Ab titers in the normal range (negative) and active arterial wall thickening. Having a TPO-Ab titer in the normal range was significantly positively associated with baseline atherosclerosis. Having a TPO-Ab titer in the normal range was significantly inversely associated with active arterial wall thickening.
Table 4 shows the association between TPO-Ab titers in the normal range (negative) and baseline atherosclerosis and between TPO-Ab titers in the normal range (negative) and active arterial wall thickening in participants with TSH values within the normal range. We found essentially the same associations. Independent of known confounding factors, having a TPO-Ab titer in the normal range was significantly positively associated with baseline atherosclerosis and inversely associated with active arterial wall thickening.
3.4. Sensitivity Analysis
For a sensitivity analysis, we performed a sex-specific analysis for the association between TPO-Ab titers in the normal range (negative) and baseline atherosclerosis and for the association between TPO-Ab titers in the normal range (negative) and active arterial wall thickening. We found essentially the same associations. Among participants with TSH values within the normal range, the age-adjusted ORs (95% CIs) of logarithmic values of TPO-Ab titers for baseline atherosclerosis and active arterial wall thickening were 3.64 (1.30, 10.18) and 0.57 (0.32, 1.00) for males (n = 373) and 1.82 (0.63, 5.21) and 0.40 (0.19, 0.82) for females (n = 626), respectively.
4. Discussion
The main findings of the present study are that having a TPO-Ab titer in the normal range (negative) is positively associated with baseline atherosclerosis but inversely associated with active arterial wall thickening among euthyroid individuals. These findings are consistent with those of our previous cross-sectional study, which found an independent positive association between TPO-Ab titers in the normal range (negative) and atherosclerosis among euthyroid individuals [
3].
Subclinical hypothyroidism is reported to be positively associated with carotid atherosclerosis [
2]. Thus, a reduction in thyroid function could not explain the present results because similar associations were observed when we limited the analysis to participants with TSH levels within the normal range.
Inflammation is a known cause of endothelial dysfunction, which is related to atherosclerosis [
14]. A previous case–control study of 1402 non-obese euthyroid individuals with autoimmune thyroiditis and 4206 non-obese euthyroid healthy controls found that thyroid function is not associated with inflammatory markers while TPO-Ab titers are positively associated with levels of high-sensitivity C-reactive protein [
15]. Therefore, low-grade inflammation might be underlying the positive association between having a TPO-Ab titer in the normal range and baseline atherosclerosis in our present study.
However, in the present study, we also found a significant inverse association between TPO-Ab titers in the normal range (negative) and active arterial wall thickening among the euthyroid population.
Our previous prospective study of 363 Japanese males aged 60–69 years followed for two years revealed an inverse association between baseline atherosclerosis (CIMT ≥ 1.1 mm) and active arterial wall thickening (CIMT ≥ 0.01 mm/year), possibly due to lower levels of CD34-positive cells [
8]. Active arterial wall thickening is a process of aggressive endothelial repair. During aggressive endothelial repair, many CD34-positive cells differentiate into mature (CD34-negative) cells such as macrophages and foam cells [
9]. Progression of atherosclerotic lesions might reduce the number of circulating CD34-positive cells due to consumption. Therefore, participants with baseline atherosclerosis might have fewer CD34-positive cells and less active arterial wall thickening. In the present study, we found a significant inverse association between baseline atherosclerosis and active arterial wall thickening, as found in our previous study [
8]. Participants with low levels of circulating CD34-positive cells might have a higher risk of cardiovascular disease than those with high levels of circulating CD34-positive cells [
16,
17] because low levels of CD34-positive cells indicate a deficiency in endothelial repair. Among patients with a history of atherothrombotic cerebral ischemic events, a strong inverse association between circulating CD34-positive cells and the number of cerebral infarcts was reported. However, this study did not find any correlation between the degrees of atherosclerosis and circulating CD34-positive cells [
16].
The findings of the present study have many clinical implications. First, among euthyroid individuals, participants with high–normal TPO-Ab titers have a risk of developing atherosclerosis, as evaluated by CIMT. High–normal TPO-Ab titers could be associated with endothelial repair deficiency, which inhibits yearly increases in CIMT. This study also indicates that not having yearly CIMT progression does not always indicate a healthy endothelium.
Potential limitations of the present study warrant consideration. Although endothelial repair deficiency might be underlying the inverse association between having a TPO-Ab titer in the normal range and active arterial wall thickening, we could not evaluate the degree of endothelial deficiency directly. Since fewer circulating CD34-positive cells could indicate endothelial deficiency directly [
8,
18], further studies with data on circulating CD34-positive cell counts are necessary. Low-grade inflammation also might be underlying the present associations, but we could not evaluate inflammation directly.
5. Conclusions
In conclusion, among euthyroid individuals, having a TPO-Ab titer within the normal range (negative) is positively associated with baseline atherosclerosis but inversely associated with active arterial wall thickening. These findings can help clarify the mechanisms of endothelial maintenance.
Author Contributions
Conceptualization, Y.S. and T.M.; methodology, Y.S., S.-Y.K., S.N., Y.N. (Yasuhiro Nagata), N.H. and T.M.; software Y.S., Y.N. (Yuko Noguchi) and T.M.; validation Y.S., Y.N. (Yuko Noguchi), N.H. and T.M.; formal analysis, Y.S. and Y.N. (Yuko Noguchi); investigation, Y.S.; resources, all authors; data curation, all authors; writing original draft preparation, Y.S.; writing—review and editing, all authors; visualization, Y.S., Y.N. (Yuko Noguchi), N.H. and T.M.; supervision, N.H. and T.M.; project administration, Y.S.; funding acquisition, T.M. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the Japan Society for the Promotion of Science (No. 21H02575). This funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Institutional Review Board Statement
This study was approved by the Ethics Committee of Nagasaki University Graduate School of Biomedical Sciences (project registration number 14051404). This manuscript was written based on the STROBE statement to assess the reporting of cohort and cross-sectional studies. All procedures involving human participants in this study were performed in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki Declaration and its later amendments for comparable ethical standards.
Informed Consent Statement
Written consent forms were used to ensure that participants understood the objectives of the study when obtaining informed consent.
Data Availability Statement
We cannot publicly provide individual data due to participant privacy according to the ethical guidelines in Japan. Additionally, the informed consent obtained does not include a provision for publicly sharing data. Qualifying researchers may apply to access a minimal dataset by contacting Prof Naomi Hayashida, Principal Investigator, Division of Promotion of Collaborative Research on Radiation and Environment Health Effects, Atomic Bomb Disease Institute, Nagasaki University, Nagasaki, Japan at
naomin@nagasaki-u.ac.jp. Or, please contact the office of data management at
ritouken@vc.fctv-net.jp. Information for where data can be requested is also available at
https://www.genken.nagasaki-u.ac.jp/dscr/message/ and
http://www.med.nagasaki-u.ac.jp/cm/ (accesed on 20 December 2021).
Acknowledgments
We are grateful to the staff from the Saza Town Office for their outstanding support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Raterman, H.G.; Voskuyl, A.E.; Simsek, S.; Schreurs, M.W.; van Hoogstraten, I.M.; Peters, M.J.; van Halm, V.P.; Dijkmans, B.A.; Lips, P.; Lems, W.F.; et al. Increased progression of carotid intima media thickness in thyroid peroxidase antibodies-positive rheumatoid arthritis patients. Eur. J. Endocrinol. 2013, 169, 751–757. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Valentina, V.N.; Marijan, B.; Chedo, D.; Branka, K. Subclinical hypothyroidism and risk to carotid atherosclerosis. Arq. Bras. Endocrinol. Metabol. 2011, 55, 475–480. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, Y.; Kawashiri, S.Y.; Noguchi, Y.; Nagata, Y.; Maeda, T.; Hayashida, N. Normal range of anti–thyroid peroxidase antibody (TPO-Ab) and atherosclerosis among eu-thyroid population: A cross-sectional study. Medicine 2020, 99, e22214. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Wang, W.; Wilsdon, A.; Butler, K.R.; Adabag, S.; Griswold, M.E.; Nambi, V.; Rosamond, W.; Sotoodehnia, N.; Mosley, T.H. Carotid intima-media thickness and the risk of sudden cardiac death: The ARIC Study and the CHS. J. Am. Heart Assoc. 2020, 9, e016981. [Google Scholar] [CrossRef] [PubMed]
- Tu, S.T.; Wang, I.W.; Lin, H.F.; Liao, Y.C.; Lin, R.T.; Liu, C.S.; Juo, S.H. Carotid intima-media thickness and stiffness are independent risk factors for atherosclerotic diseases. J. Investig. Med. 2010, 58, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Polak, J.F.; Pencina, M.J.; O’Leary, D.H.; D’Agostino, R.B. Common carotid artery intima-media thickness progression as a predictor of stroke in multi-ethnic study of atherosclerosis. Stroke 2011, 42, 3017–3021. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, M.W.; Polak, J.F.; Kavousi, M.; Mathiesen, E.B.; Völzke, H.; Tuomainen, T.P.; Sander, D.; Plichart, M.; Catapano, A.L.; Robertson, C.M.; et al. Carotid intima-media thickness progression to predict cardiovascular events in the general population (the PROG-IMT collaborative project): A meta-analysis of individual participant data. Lancet 2012, 379, 2053–2062. [Google Scholar] [CrossRef]
- Shimizu, Y.; Kawashiri, S.Y.; Kiyoura, K.; Koyamatsu, J.; Fukui, S.; Tamai, M.; Nobusue, K.; Yamanashi, H.; Nagata, Y.; Maeda, T. Circulating CD34+ cells and active arterial wall thickening among elderly men: A prospective study. Sci. Rep. 2020, 10, 4656. [Google Scholar] [CrossRef] [PubMed]
- Stellos, K.; Seizer, P.; Bigalke, B.; Daub, K.; Geisler, T.; Gawaz, M. Platelet aggregates-induced human CD34+progenitor cell proliferation and differentiation to macrophages and foam cells is mediated by stromal cell derived factor 1 in vitro. Semin. Thromb. Hemost. 2010, 36, 139–145. [Google Scholar] [CrossRef] [PubMed]
- LSI Medience Corporation Information. Rinsyokensa Jugyo. 2017. Available online: http://www.medience.co.jp/information/02.html (accessed on 23 November 2021).
- Hara, T.; Takamura, N.; Akashi, S.; Nakazato, M.; Maeda, T.; Wada, M.; Nakashima, K.; Abe, Y.; Kusano, Y.; Aoyagi, K. Evaluation of clinical markers of atherosclerosis in young and elderly Japanese adults. Clin. Chem. Lab. Med. 2006, 44, 824–829. [Google Scholar] [CrossRef] [PubMed]
- Yanase, T.; Nasu, S.; Mukuta, Y.; Shimizu, Y.; Nishihara, T.; Okabe, T.; Nomura, M.; Inoguchi, T.; Nawata, H. Evaluation of a new carotid intima-media thickness measurement by B-mode ultrasonography using an innovative measurement software, intimascope. Am. J. Hypertens. 2006, 19, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Kawamori, R.; Yamasaki, Y.; Matsushima, H.; Nishizawa, H.; Nao, K.; Hougaku, H.; Maeda, H.; Handa, N.; Matsumoto, M.; Kamada, T. Prevalence of carotid atherosclerosis in diabetic patients ultrasound high-resolution B-mode imaging on carotid arteries. Diabetes Care 1992, 15, 1290–1294. [Google Scholar] [CrossRef]
- Gisterå, A.; Hansson, G.K. The immunology of atherosclerosis. Nat. Rev. Nephrol. 2017, 13, 368–380. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Duan, Y.; Fu, J.; Wang, G. Association between thyroid hormones, thyroid antibodies, and cardiometabolic factors in non-obese individuals with normal thyroid function. Front. Endocrinol. 2018, 9, 130. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, A.; Matsuyama, T.; Moriwaki, H.; Hayashi, T.; Hayashida, K.; Nagatsuka, K.; Todo, K.; Mori, K.; Stern, D.M.; Soma, T.; et al. Circulating CD34-positive cells provide an index of cerebrovascular function. Circulation 2004, 109, 2972–2975. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.S.; Li, Q.; Ghasemzadeh, N.; Eapen, D.J.; Moss, L.D.; Janjua, A.U.; Manocha, P.; Kassem, H.A.; Veledar, E.; Samady, H.; et al. Circulating CD34+ progenitor cells and risk of mortality in a population with coronary artery disease. Circ. Res. 2015, 116, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, Y.; Yamanashi, H.; Noguchi, Y.; Koyamatsu, J.; Nagayoshi, M.; Kiyoura, K.; Fukui, S.; Tamai, M.; Kawashiri, S.Y.; Kondo, H.; et al. Cardio-ankle vascular index and circulating CD34-positive cell levels as indicators of endothelial repair activity in older Japanese men. Geriatr. Gerontol. Int. 2019, 19, 557–562. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).