Digital Online Anaesthesia Patient Informed Consent before Elective Diagnostic Procedures or Surgery: Recent Practice in Children—An Exploratory ESAIC Survey (2021)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Protocol
2.2. Questionnaire
2.3. Statistical Analysis
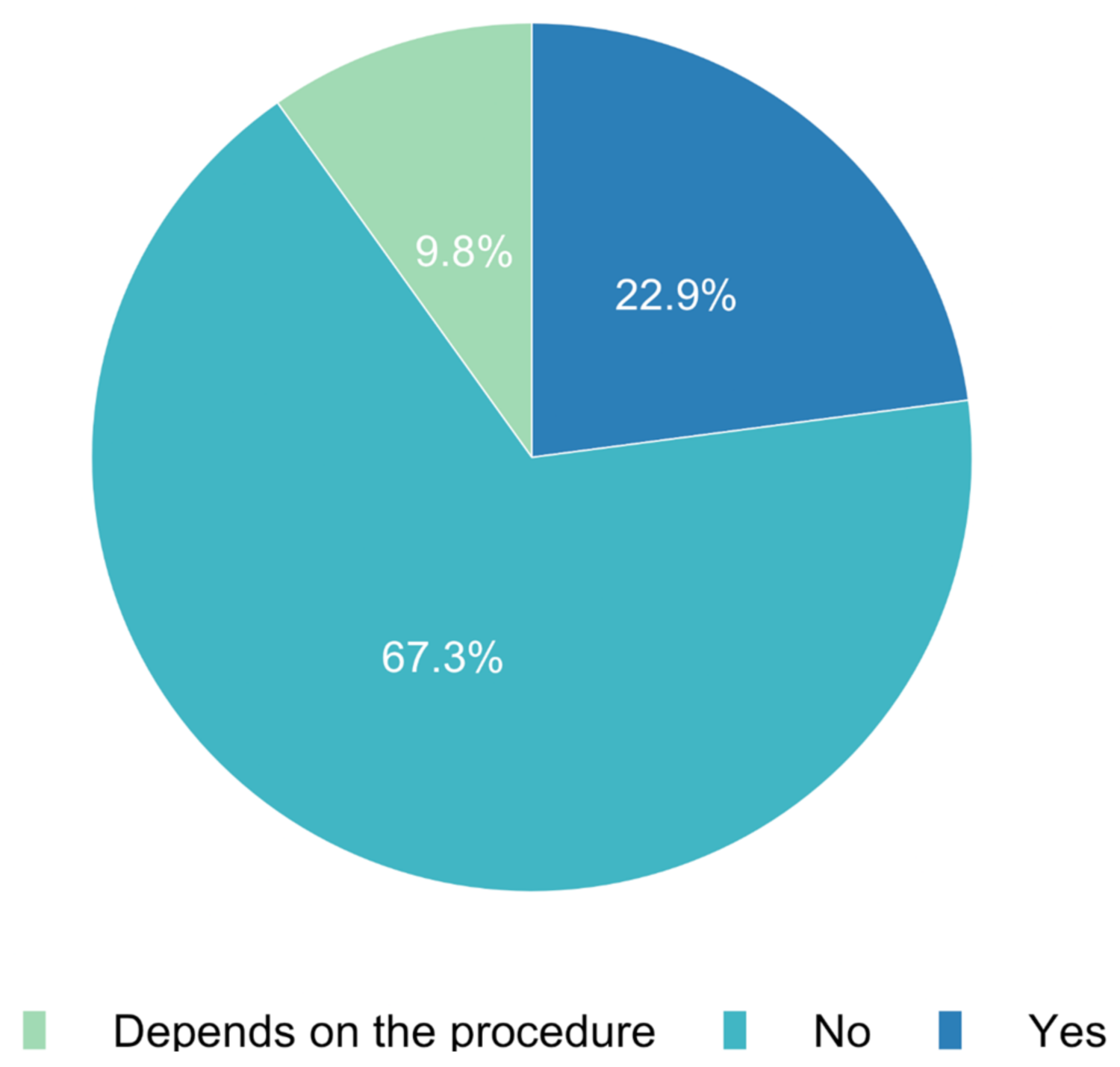
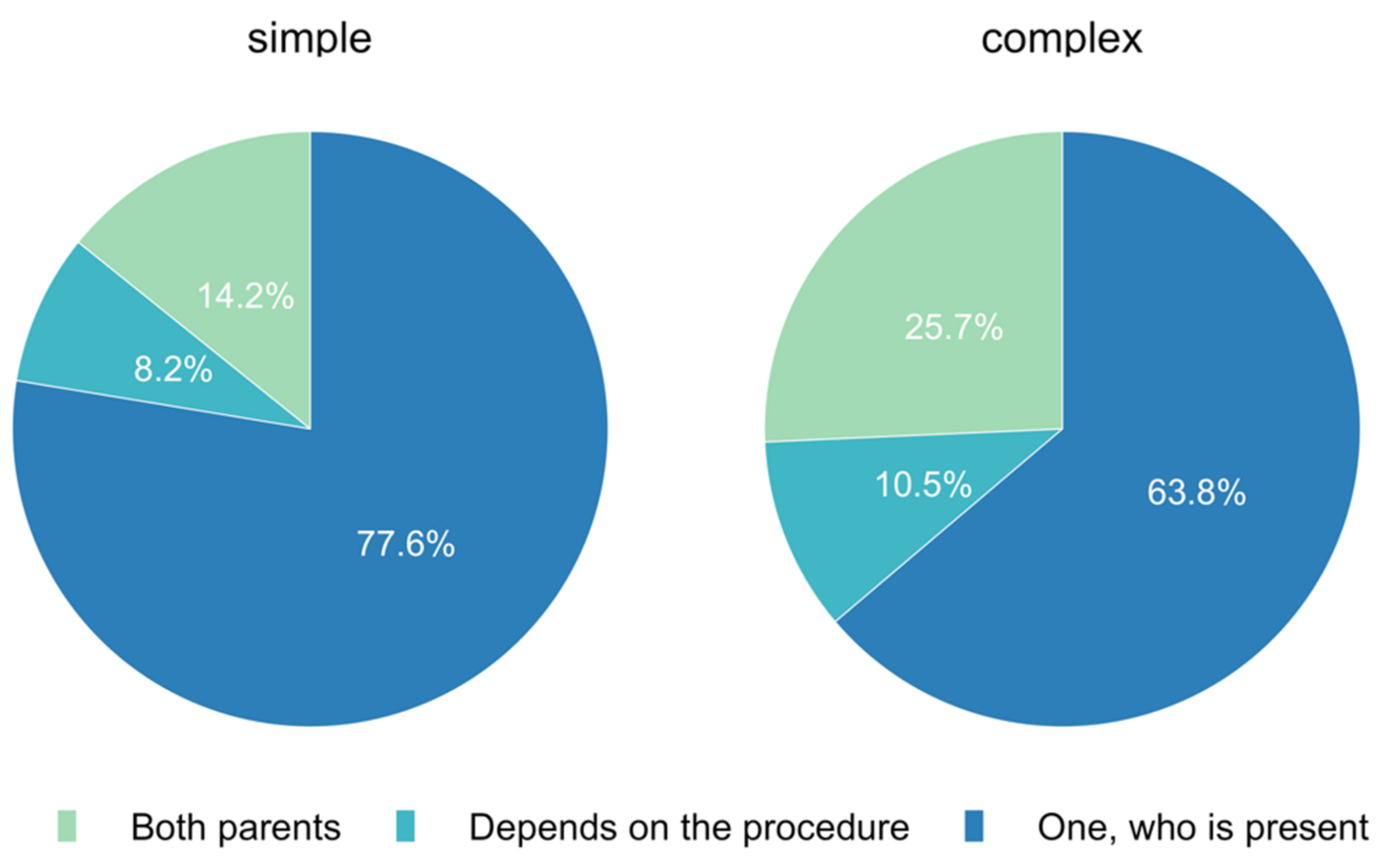
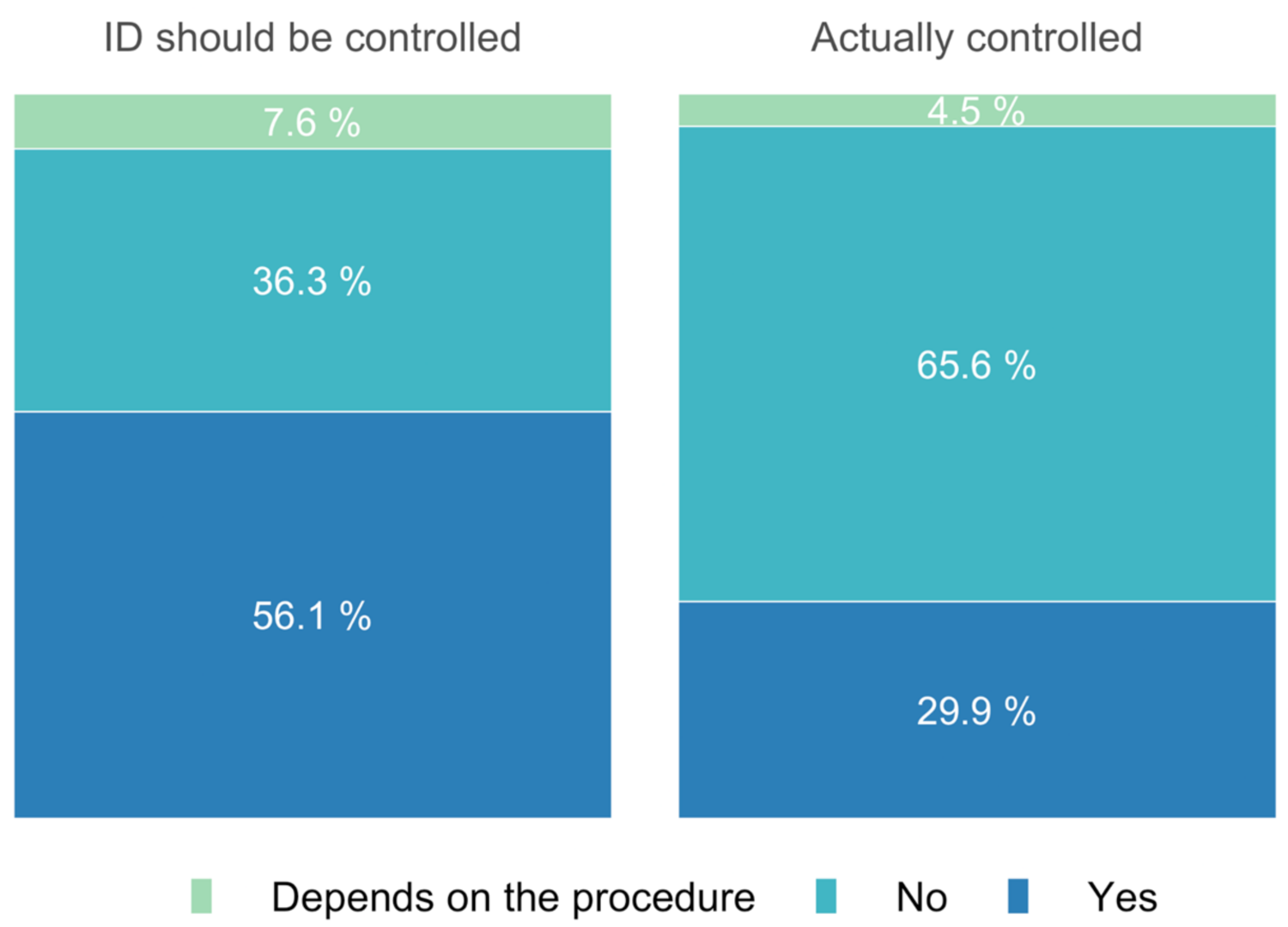
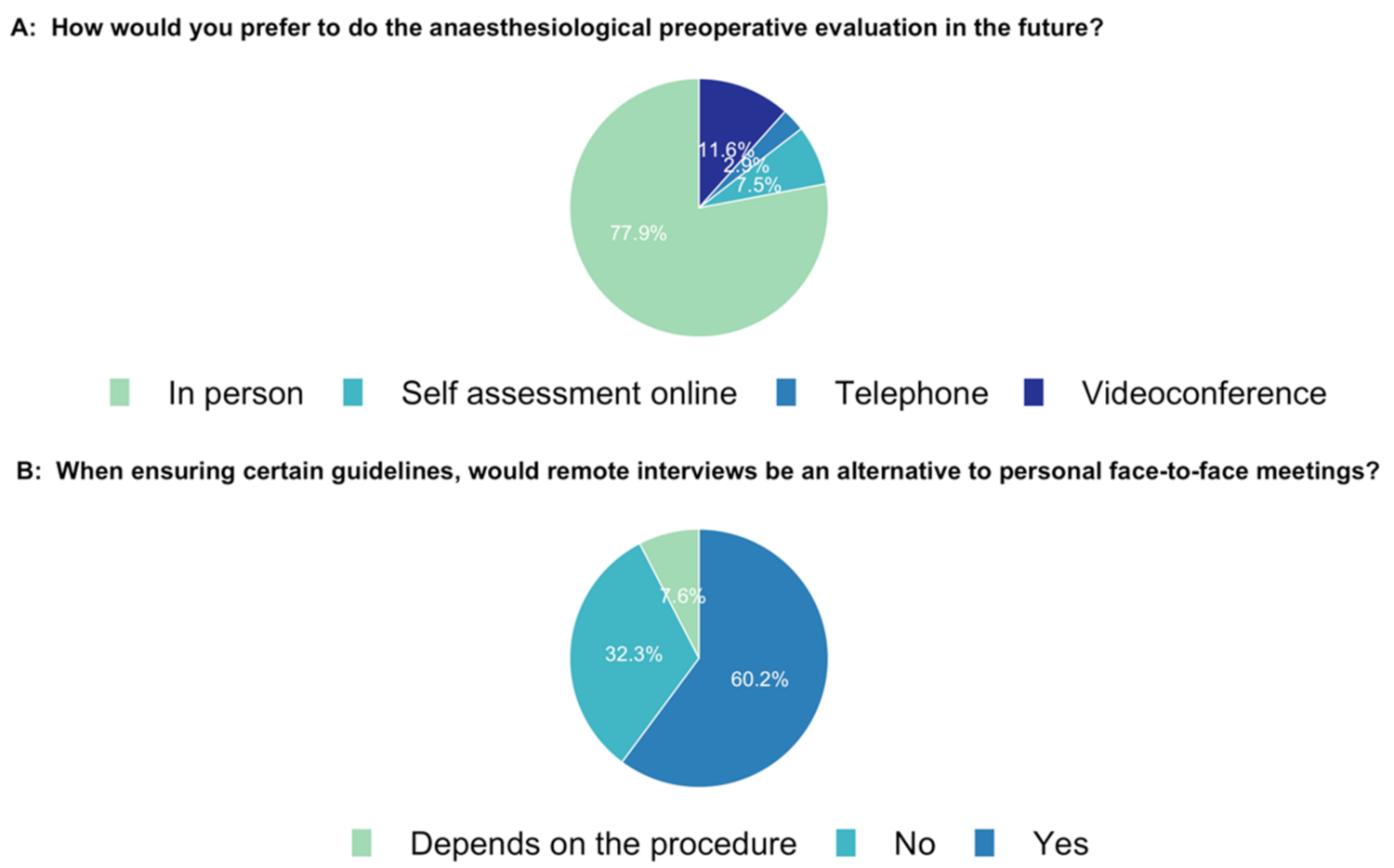
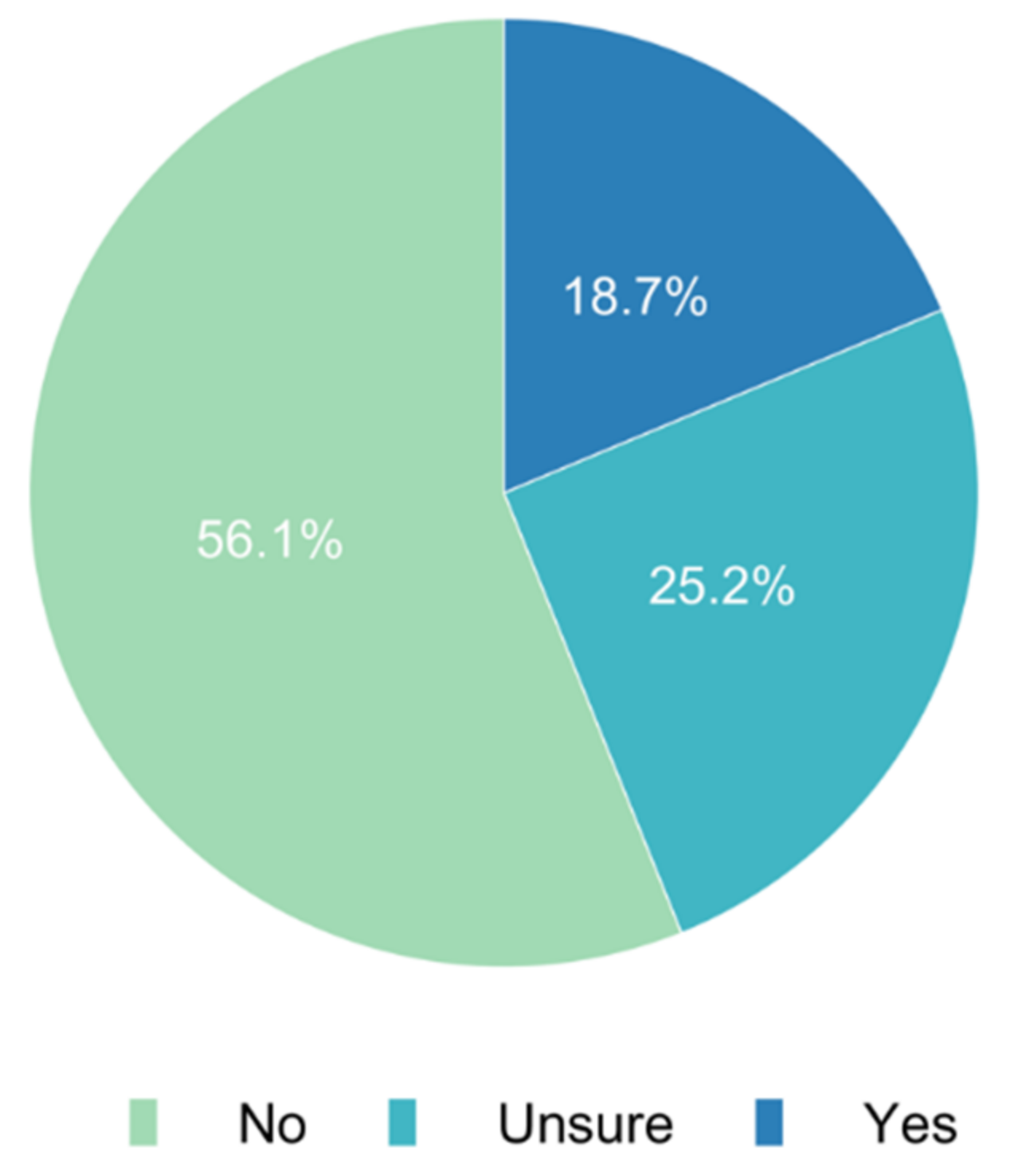
3. Results
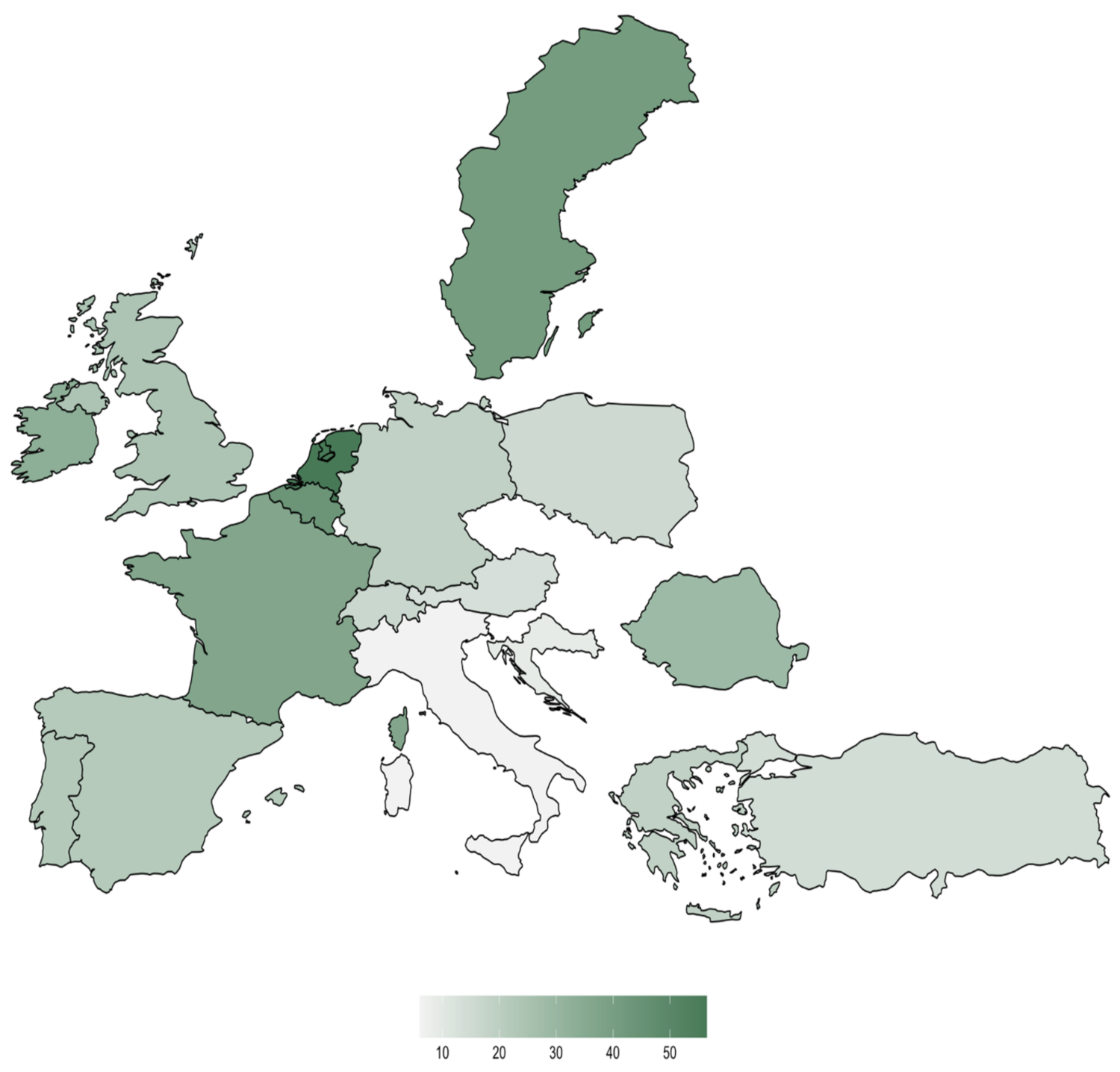
Population
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yu, X.; Chen, M.; Liu, X.; Chen, Y.; Hao, Z.; Zhang, H.; Wang, W. Risk factors of nosocomial infection after cardiac surgery in children with congenital heart disease. BMC Infect. Dis. 2020, 20, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ibrahim, L.F.; Hopper, S.M.; Orsini, F.; Daley, A.J.; Babl, F.E.; Bryant, P.A. Efficacy and safety of intravenous ceftriaxone at home versus intravenous flucloxacillin in hospital for children with cellulitis (CHOICE): A single-centre, open-label, randomised, controlled, non-inferiority trial. Lancet Infect. Dis. 2019, 19, 477–486. [Google Scholar] [CrossRef]
- Marx, G.; Dusch, M.; Czaplik, M.; Balzer, F.; Brokmann, J.C.; Deisz, R.; Rossaint, R. Telemedizin für die vier für Telemedizin (DG Telemed) Säulen der Anästhesiologie. Positionspapier der Deutschen Gesellschaft für Anästhesiologie und Intensivmedizin (DGAI) und der Deutschen Gesellschaft für Telemedizin (DG Telemed). Anästh. Intensivmed. 2019, 60, 191–207. [Google Scholar]
- Flodgren, G.; Rachas, A.; Farmer, A.J.; Inzitari, M.; Shepperd, S. Interactive telemedicine: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2015, 2015, CD002098. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.T.; Kamming, D.; Salenieks, M.E.; Go, K.; Kohm, C.; Chung, F. Preadmission anesthesia consultation using telemedicine technology: A pilot study. Anesthesiology 2004, 100, 1605–1607. [Google Scholar] [CrossRef] [PubMed]
- Wood, E.W.; Strauss, R.A.; Janus, C.; Carrico, C.K. Telemedicine consultations in oral and maxillofacial surgery: A follow-up study. J. Oral Maxillofac. Surg. 2016, 74, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Vogel, H.; Schaaf, W.; Jacob, M. Videoassistierte anästhesiologische Patientenaufklärung. Anaesthesist 2018, 67, 829–836. [Google Scholar] [CrossRef] [PubMed]
- Raposo, V.L. Telemedicine: The legal framework (or the lack of it) in Europe. GMS Health Technol. Assess. 2016, 12. [Google Scholar] [CrossRef]
- Gesualdo, F.; Daverio, M.; Palazzani, L.; Dimitriou, D.; Diez-Domingo, J.; Fons-Martinez, J.; Jackson, S.; Vignally, P.; Rizzo, C.; Tozzi, A.E. Digital tools in the informed consent process: A systematic review. BMC Med. Ethic. 2021, 22, 18. [Google Scholar] [CrossRef] [PubMed]
- Baehner, T.; Dewald, O.; Heinze, I.; Mueller, M.; Schindler, E.; Schirmer, U.; Baumgarten, G.; Hoeft, A.; Ellerkmann, R.K. The provision of pediatric cardiac anesthesia services in Germany: Current status of structural and personnel organization. Pediatr. Anesth. 2017, 27, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Baehner, T.; Kiefer, N.; Ghamari, S.; Graeff, I.; Huett, C.; Pflugradt, S.; Sendzik, B.; Heinze, I.; Mueller, M.; Schindler, E.; et al. A National Survey: Current Clinical Practice in Pediatric Anesthesia for Congenital Heart Surgery. World J. Pediatr. Congenit. Heart Surg. 2020, 11, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Beck, C.E.; Rudolph, D.; Becke-Jakob, K.; Schindler, E.; Etspüler, A.; Trapp, A.; Fink, G.; Müller-Lobeck, L.; Röher, K.; Genähr, A.; et al. Real fasting times and incidence of pulmonary aspiration in children: Results of a German prospective multicenter observational study. Paediatr. Anaesth. 2019, 29, 1040–1045. [Google Scholar] [CrossRef] [PubMed]
- Beck, C.E.; Rudolph, D.; Mahn, C.; Etspüler, A.; Korf, M.; Lüthke, M.; Schindler, E.; Päukert, S.; Trapp, A.; Megens, J.H.A.M.; et al. Impact of clear fluid fasting on pulmonary aspiration in children undergoing general anesthesia: Results of the German prospective multicenter observational (NiKs) study. Paediatr. Anaesth. 2020, 30, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Bashshur, R.L.; Shannon, G.W.; Krupinski, E.A.; Grigsby, J.; Kvedar, J.C.; Weinstein, R.S.; Sanders, J.H.; Rheuban, K.S.; Nesbitt, T.S.; Alverson, D.C.; et al. National Telemedicine Initiatives: Essential to Healthcare Reform. Telemed. Ee-Health 2009, 15, 600–610. [Google Scholar] [CrossRef] [PubMed]
- Schallner, N.; Bürkle, H. Patientenaufklärung in der Anästhesiologie. Anästh. Intensivmed. 2020, 61, 320–328. [Google Scholar]
- HASTA HAKLARI YÖNETMELİĞİ, ÜÇÜNCÜ BÖLÜM Sağlık Durumu İle İlgili Bilgi Alma Hakkı Madde 18- (Değişik:RG-8/5/2014-28994). Available online: https://www.mevzuat.gov.tr/File/GeneratePdf?mevzuatNo=4847&mevzuatTur=KurumVeKurulusYonetmeligi&mevzuatTertip=5 (accessed on 30 November 2021).
- De Hert, S.; Imberger, G.; Carlisle, J.; Diemunsch, P.; Fritsch, G.; Moppett, I.; Solca, M.; Staender, S.; Wappler, F.; Smith, A. Preoperative evaluation of the adult patient undergoing non-cardiac surgery. Eur. J. Anaesthesiol. 2011, 28, 684–722. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mihalj, M.; Carrel, T.; Gregoric, I.D.; Andereggen, L.; Zinn, P.O.; Doll, D.; Stueber, F.; Gabriel, R.A.; Urman, R.D.; Luedi, M.M. Telemedicine for preoperative assessment during a COVID-19 pandemic: Recommendations for clinical care. Best Pract. Res. Clin. Anaesthesiol. 2020, 34, 345–351. [Google Scholar] [CrossRef] [PubMed]
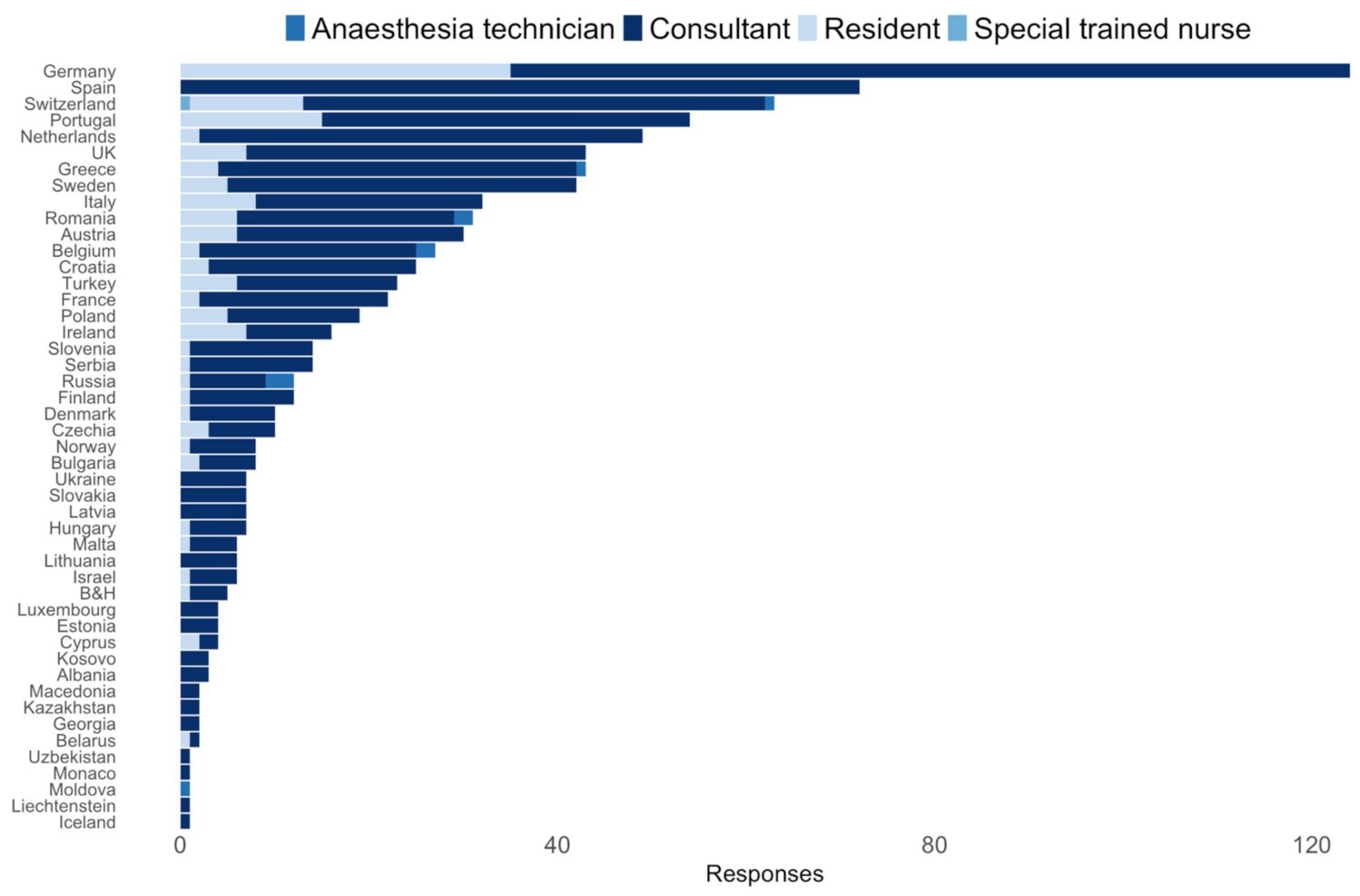


| Stratified by Gender | ||||
|---|---|---|---|---|
| Diverse | Female | Male | p | |
| n (%) | 3 (0.3) | 406 (43.6) | 521 (56) | |
| Profession (%) | <0.001 | |||
| Medical doctor | 2 (66.7) | 402 (99.0) | 516 (99.2) | |
| Nurse | 1 (33.3) | 0 (0.0) | 1 (0.2) | |
| Physician assistant | 0 (0.0) | 4 (1.0) | 2 (0.4) | |
| Other | 0 (0.0) | 0 (0.0) | 1 (0.2) | |
| Expertise (%) | 0.33 | |||
| Anaesthesia technician | 0 (0.0) | 4 (1.0) | 6 (1.2) | |
| Consultant | 2 (66.7) | 303 (74.8) | 426 (81.8) | |
| Resident | 1 (33.3) | 75 (18.5) | 67 (12.9) | |
| Special trained nurse | 0 (0.0) | 0 (0.0) | 1 (0.2) | |
| Other | 0 (0.0) | 23 (5.7) | 21 (4.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neumann, C.; Schleifer, G.; Strassberger-Nerschbach, N.; Kamp, J.; Massoth, G.; Görtzen-Patin, A.; Cudian, D.; Velten, M.; Coburn, M.; Schindler, E.; et al. Digital Online Anaesthesia Patient Informed Consent before Elective Diagnostic Procedures or Surgery: Recent Practice in Children—An Exploratory ESAIC Survey (2021). J. Clin. Med. 2022, 11, 502. https://doi.org/10.3390/jcm11030502
Neumann C, Schleifer G, Strassberger-Nerschbach N, Kamp J, Massoth G, Görtzen-Patin A, Cudian D, Velten M, Coburn M, Schindler E, et al. Digital Online Anaesthesia Patient Informed Consent before Elective Diagnostic Procedures or Surgery: Recent Practice in Children—An Exploratory ESAIC Survey (2021). Journal of Clinical Medicine. 2022; 11(3):502. https://doi.org/10.3390/jcm11030502
Chicago/Turabian StyleNeumann, Claudia, Grigorij Schleifer, Nadine Strassberger-Nerschbach, Johannes Kamp, Gregor Massoth, Alexandra Görtzen-Patin, Dishalen Cudian, Markus Velten, Mark Coburn, Ehrenfried Schindler, and et al. 2022. "Digital Online Anaesthesia Patient Informed Consent before Elective Diagnostic Procedures or Surgery: Recent Practice in Children—An Exploratory ESAIC Survey (2021)" Journal of Clinical Medicine 11, no. 3: 502. https://doi.org/10.3390/jcm11030502
APA StyleNeumann, C., Schleifer, G., Strassberger-Nerschbach, N., Kamp, J., Massoth, G., Görtzen-Patin, A., Cudian, D., Velten, M., Coburn, M., Schindler, E., & Wittmann, M. (2022). Digital Online Anaesthesia Patient Informed Consent before Elective Diagnostic Procedures or Surgery: Recent Practice in Children—An Exploratory ESAIC Survey (2021). Journal of Clinical Medicine, 11(3), 502. https://doi.org/10.3390/jcm11030502









