“Orphaned” Stomach—An Infrequent Complication of Gastric Bypass Revision
Abstract
1. Introduction
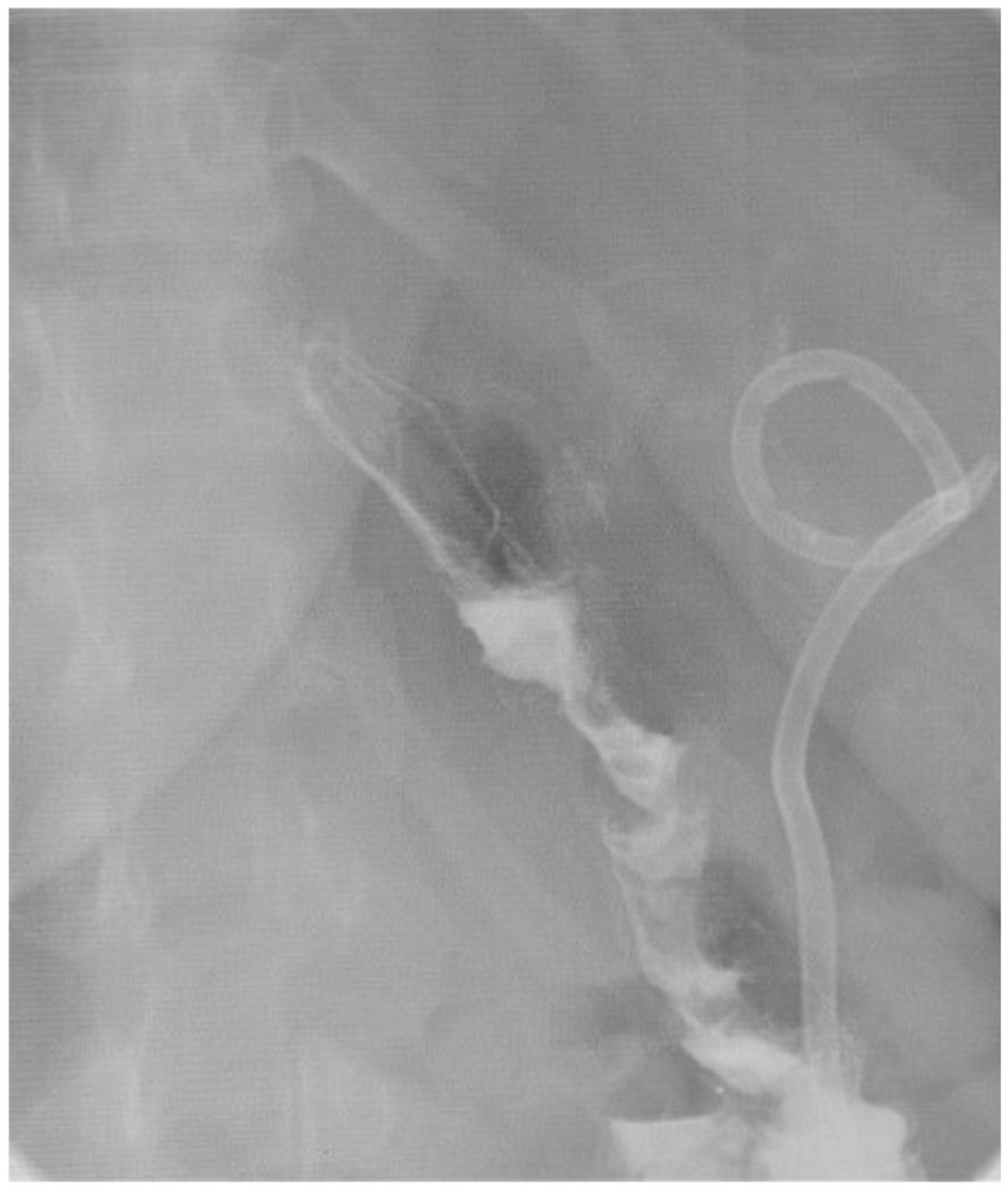
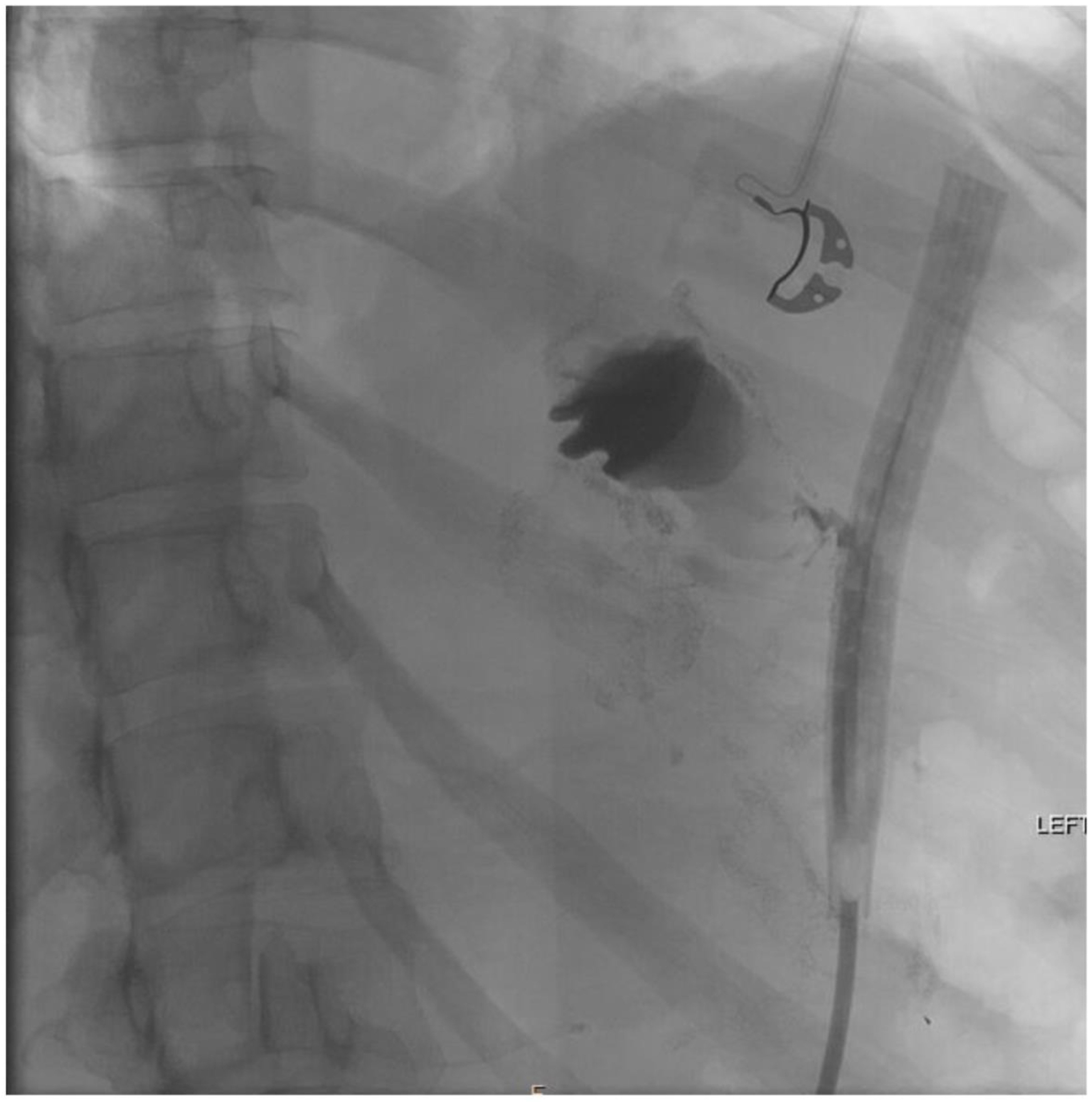
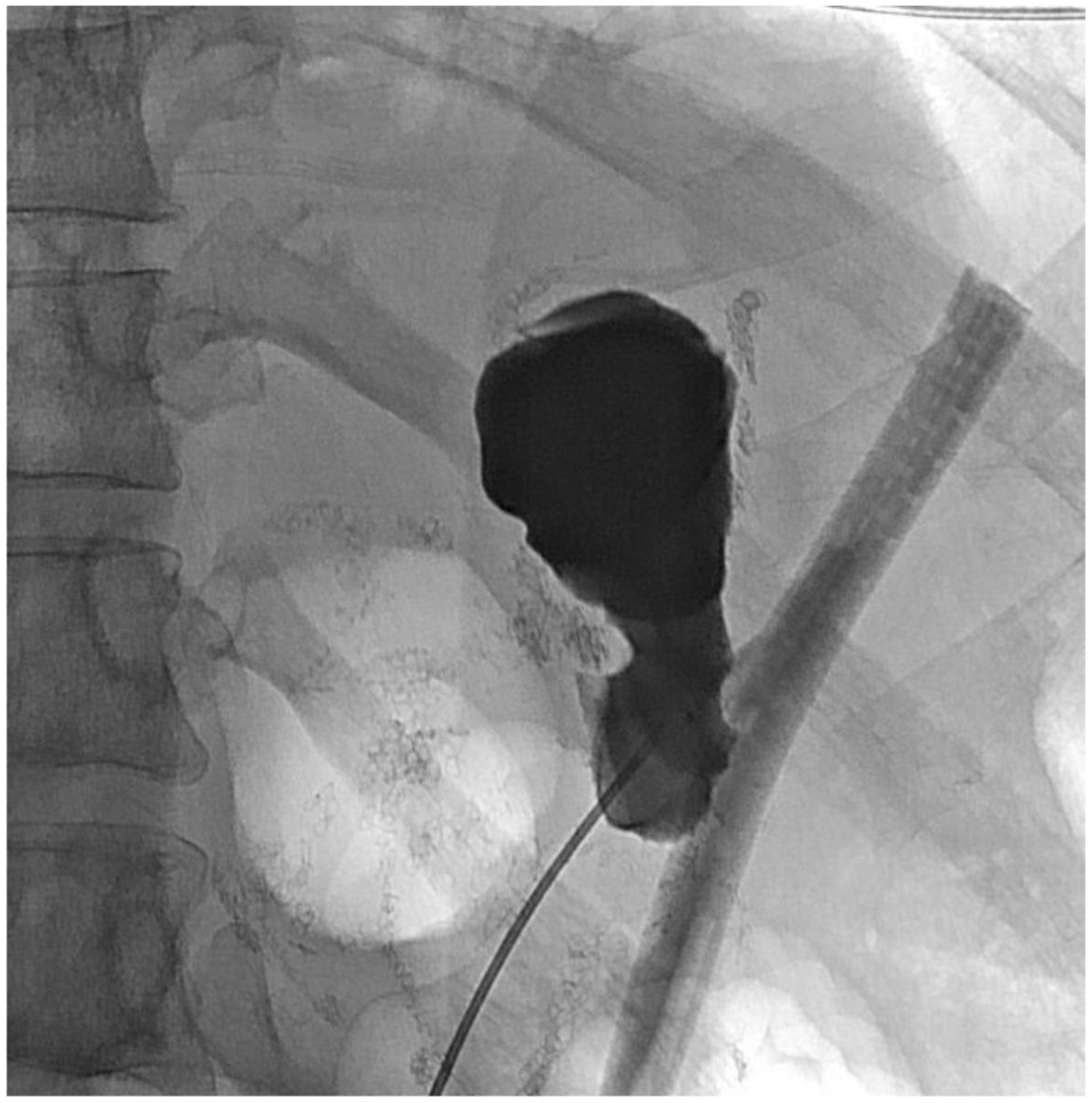
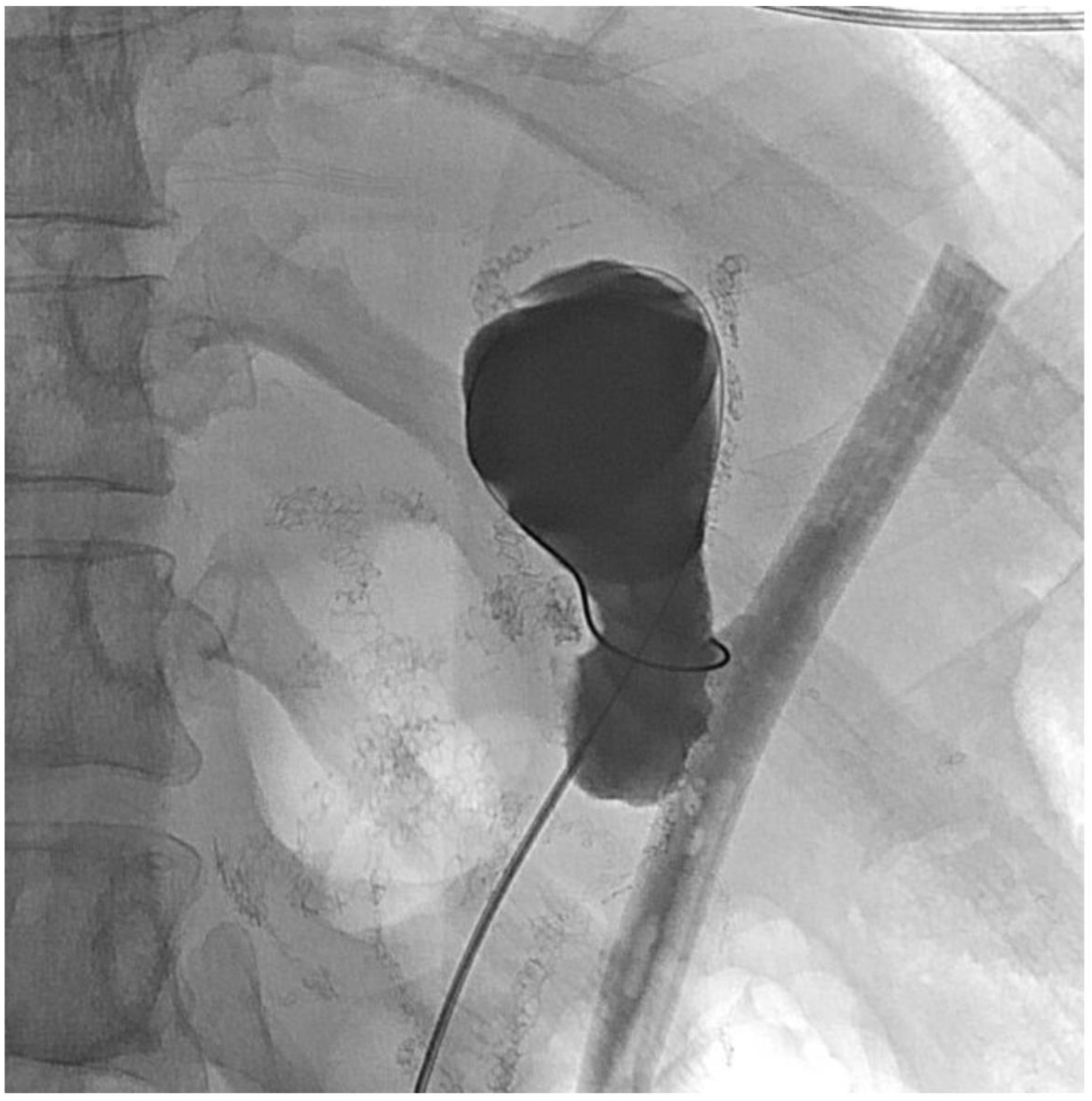
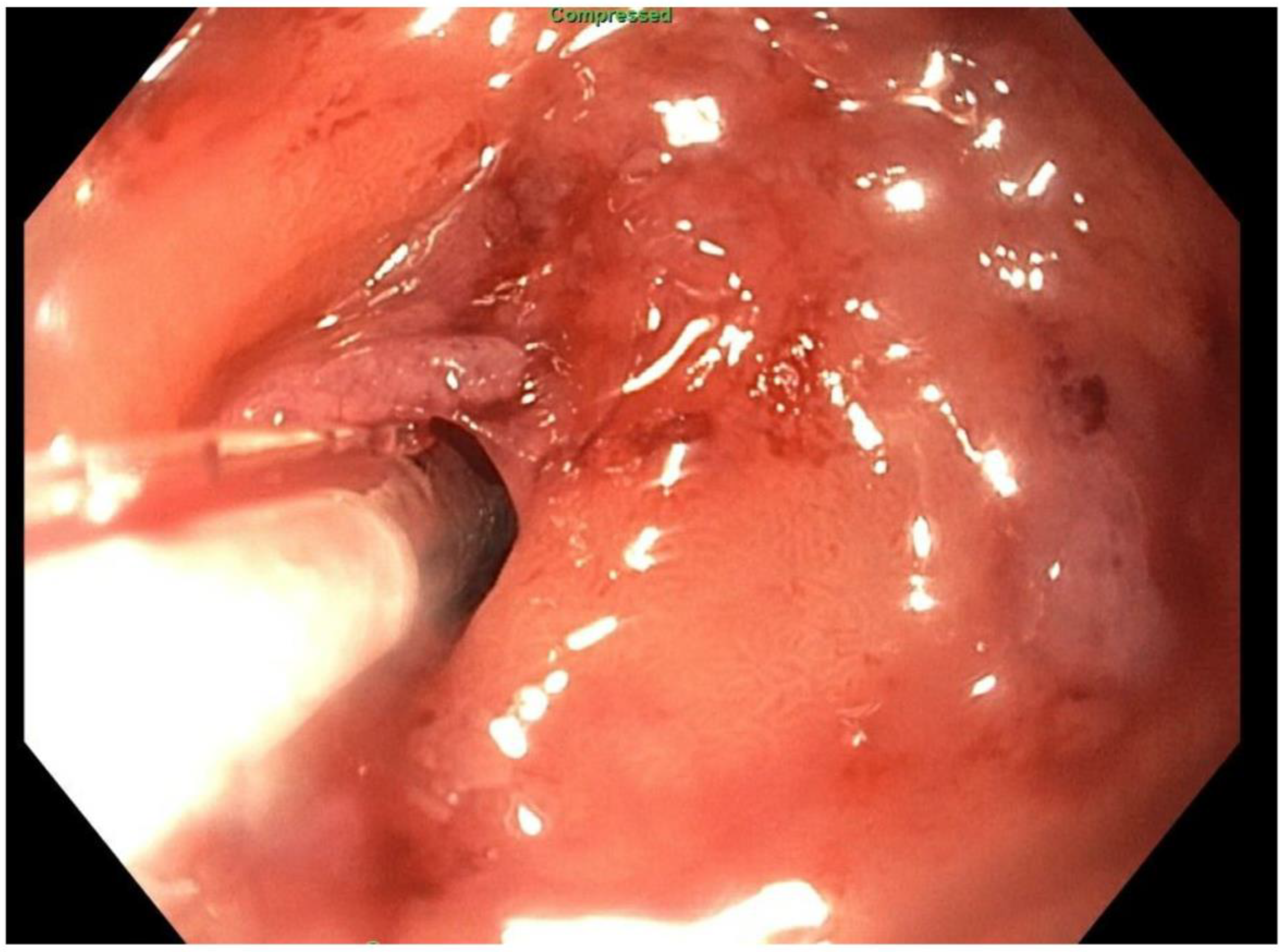
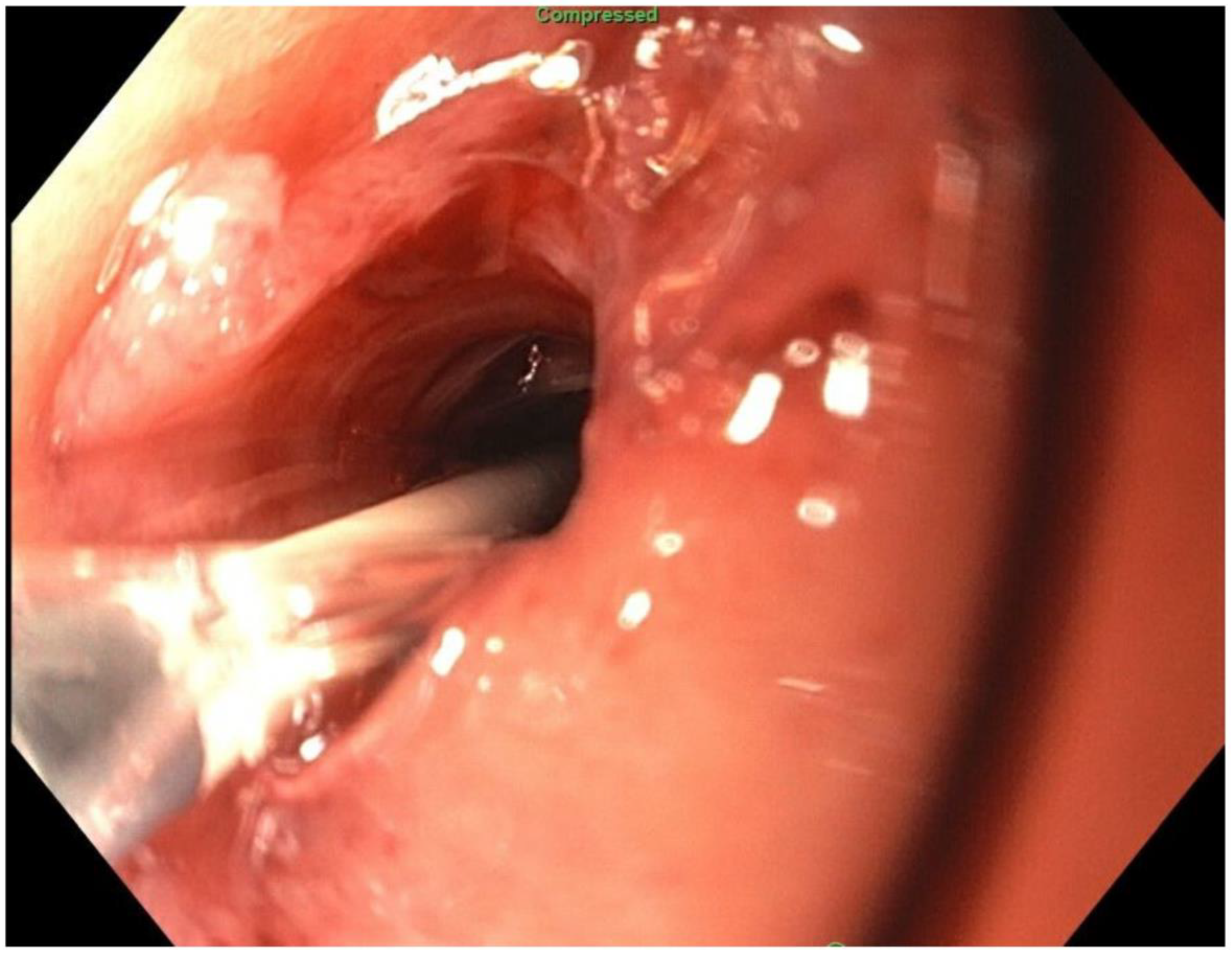
2. Detailed Case Description
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Obesity and Overweight. Available online: http://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 12 January 2022).
- Angrisani, L.; Santonicola, A.; Iovino, P.; Vitiello, A.; Higa, K.; Himpens, J.; Buchwald, H.; Scopinaro, N. IFSO Worldwide Survey 2016: Primary, Endoluminal, and Revisional Procedures. Obes. Surg. 2018, 28, 3783–3794. [Google Scholar] [CrossRef] [PubMed]
- Chung, A.Y.; Strassle, P.D.; Schlottmann, F.; Patti, M.G.; Duke, M.C.; Farrell, T.M. Trends in Utilization and Relative Complication Rates of Bariatric Procedures. J. Gastrointest. Surg. 2019, 23, 1362–1372. [Google Scholar] [CrossRef] [PubMed]
- Golzarand, M.; Toolabi, K.; Farid, R. The bariatric surgery and weight losing: A meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults. Surg. Endosc. 2017, 31, 4331–4345. [Google Scholar] [CrossRef]
- Dogan, K.; Gadiot, R.P.M.; Aarts, E.O.; Betzel, B.; van Laarhoven, C.J.H.M.; Biter, L.U.; Mannaerts, G.H.H.; Aufenacker, T.J.; Janssen, I.M.C.; Berends, F.J. Effectiveness and Safety of Sleeve Gastrectomy, Gastric Bypass, and Adjustable Gastric Banding in Morbidly Obese Patients: A Multicenter, Retrospective, Matched Cohort Study. Obes. Surg. 2015, 25, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Perrone, F.; Bianciardi, E.; Ippoliti, S.; Nardella, J.; Fabi, F.; Gentileschi, P. Long-term effects of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass for the treatment of morbid obesity: A monocentric prospective study with minimum follow-up of 5 years. Updat. Surg. 2017, 69, 101–107. [Google Scholar] [CrossRef]
- Sharples, A.J.; Mahawar, K. Systematic Review and Meta-Analysis of Randomised Controlled Trials Comparing Long-Term Outcomes of Roux-En-Y Gastric Bypass and Sleeve Gastrectomy. Obes. Surg. 2020, 30, 664–672. [Google Scholar] [CrossRef]
- Magro, D.O.; Geloneze, B.; Delfini, R.; Pareja, B.C.; Callejas, F.; Pareja, J.C. Long-term Weight Regain after Gastric Bypass: A 5-year Prospective Study. Obes. Surg. 2008, 18, 648–651. [Google Scholar] [CrossRef]
- Christou, N.V.; Look, D.; MacLean, L.D. Weight Gain after Short- and Long-Limb Gastric Bypass in Patients Followed for Longer than 10 Years. Ann. Surg. 2006, 244, 734–740. [Google Scholar] [CrossRef]
- Peterli, R.; Wölnerhanssen, B.; Peters, T.; Vetter, D.; Kröll, D.; Borbély, Y.; Schultes, B.; Beglinger, C.; Drewe, J.; Schiesser, M.; et al. Effect of Laparoscopic Sleeve Gastrectomy vs. Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss in Patients with Morbid Obesity. JAMA 2018, 319, 255–265. [Google Scholar] [CrossRef]
- Azagury, D.E.; Abu Dayyeh, B.K.; Greenwalt, I.T.; Thompson, C.C. Marginal ulceration after Roux-en-Y gastric bypass surgery: Characteristics, risk factors, treatment, and outcomes. Endoscopy 2011, 43, 950–954. [Google Scholar] [CrossRef]
- Csendes, A.; Burgos, A.M.; Altuve, J.; Bonacic, S. Incidence of Marginal Ulcer 1 Month and 1 to 2 Years after Gastric Bypass: A Prospective Consecutive Endoscopic Evaluation of 442 Patients with Morbid Obesity. Obes. Surg. 2009, 19, 135–138. [Google Scholar] [CrossRef] [PubMed]
- El-Hayek, K.; Timratana, P.; Shimizu, H.; Chand, B. Marginal ulcer after Roux-en-Y gastric bypass: What have we really learned? Surg. Endosc. 2012, 26, 2789–2796. [Google Scholar] [CrossRef] [PubMed]
- Capella, J.F.; Capella, R.F. Gastro-Gastric Fistulas and Marginal Ulcers in Gastric Bypass Procedures for Weight Reduction. Obes. Surg. 1999, 9, 22–27, discussion 28. [Google Scholar] [CrossRef] [PubMed]
- Carrodeguas, L.; Szomstein, S.; Soto, F.; Whipple, O.; Simpfendorfer, C.; Gonzalvo, J.P.; Villares, A.; Zundel, N.; Rosenthal, R. Management of gastrogastric fistulas after divided Roux-en-Y gastric bypass surgery for morbid obesity: Analysis of 1292 consecutive patients and review of literature. Surg. Obes. Relat. Dis. 2005, 1, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Chahine, E.; Kassir, R.; Dirani, M.; Joumaa, S.; Debs, T.; Chouillard, E. Surgical Management of Gastrogastric Fistula After Roux-en-Y Gastric Bypass: 10-Year Experience. Obes. Surg. 2018, 28, 939–944. [Google Scholar] [CrossRef]
- Yimcharoen, P.; Heneghan, H.; Chand, B.; Talarico, J.A.; Tariq, N.; Kroh, M.; Brethauer, S.A. Successful management of gastrojejunal strictures after gastric bypass: Is timing important? Surg. Obes. Relat. Dis. 2012, 8, 151–157. [Google Scholar] [CrossRef]
- Mathew, A.; Veliuona, M.A.; DePalma, F.J.; Cooney, R.N. Gastrojejunal Stricture after Gastric Bypass and Efficacy of Endoscopic Intervention. Dig. Dis. Sci. 2009, 54, 1971–1978. [Google Scholar] [CrossRef]
- Bruenderman, E.H.; Vitale, G.C.; Kehdy, F.J. Endoscopic Management of an Excluded Gastric Segment after Reversal of Roux-en-Y Gastric Bypass. Am. Surg. 2020, 86, e98–e100. [Google Scholar] [CrossRef]
- Siddiqui, A.A.; DeWitt, J.M.; Strongin, A.; Singh, H.; Jordan, S.; Loren, D.E.; Kowalski, T.; Eloubeidi, M.A. Outcomes of EUS-guided drainage of debris-containing pancreatic pseudocysts by using combined endoprosthesis and a nasocystic drain. Gastrointest. Endosc. 2013, 78, 589–595. [Google Scholar] [CrossRef]
- Pereira, F.; Caldeira, A.; Leite, S.; Marques, S.; Moreira, T.; Moutinho-Ribeiro, P.; Nunes, N.; Bispo, M. GRUPUGE Perspective: Endoscopic Ultrasound-Guided Drainage of Peripancreatic Collections. GE-Port. J. Gastroenterol. 2020, 28, 39–51. [Google Scholar] [CrossRef]
- Ng, P.; Rasmussen, D.; Vilmann, P.; Hassan, H.; Gheorman, V.; Burtea, D.; Surlin, V.; Saftoiu, A. Endoscopic ultrasound-guided drainage of pancreatic pseudocysts: Medium-term assessment of outcomes and complications. Endosc. Ultrasound 2013, 2, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Sãftoiu, A.; Vilmann, A.; Vilmann, P. Endoscopic ultrasound-guided drainage of pancreatic pseudocysts. Endosc. Ultrasound 2015, 4, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Vedantam, S.; Roberts, J. Endoscopic Stents in the Management of Bariatric Complications: Our Algorithm and Outcomes. Obes. Surg. 2020, 30, 1150–1158. [Google Scholar] [CrossRef]
- Kanters, A.E.; Shubeck, S.P.; Varban, O.A.; Dimick, J.B.; Telem, D.A. Incidence and Efficacy of Stent Placement in Leak Management after Bariatric Surgery: An MBSAQIP Analysis. Ann. Surg. 2020, 271, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Phillips, M.S.; Gosain, S.; Bonatti, H.; Friel, C.M.; Ellen, K.; Northup, P.G.; Kahaleh, M. Enteral Stents for Malignancy: A Report of 46 Consecutive Cases over 10 years, with Critical Review of Complications. J. Gastrointest. Surg. 2008, 12, 2045–2050. [Google Scholar] [CrossRef]
- Khashab, M.; Alawad, A.S.; Shin, E.J.; Kim, K.; Bourdel, N.; Singh, V.K.; Lennon, A.M.; Hutfless, S.; Sharaiha, R.Z.; Amateau, S.; et al. Enteral stenting versus gastrojejunostomy for palliation of malignant gastric outlet obstruction. Surg. Endosc. 2013, 27, 2068–2075. [Google Scholar] [CrossRef]
- Binmoeller, K.F.; Shah, J.N. Endoscopic ultrasound-guided gastroenterostomy using novel tools designed for transluminal therapy: A porcine study. Endoscopy 2012, 44, 499–503. [Google Scholar] [CrossRef]
- de Lima, M.F.; Nunes, N.; Sousa, L.; Duarte, M.A. Opening New Ways through the Esophagus with Combined Anterograde-Retrograde Recanalization. GE-Port. J. Gastroenterol. 2021, 28, 364–366. [Google Scholar] [CrossRef]
- Tang, S.-J.; Wu, R.; Chatha, A.M. Combined Antegrade and Retrograde Endoscopy (CARE) with Pharyngo-esophageal Puncture (PEP) for Complete Esophageal Introital Obstruction. Video J. Encycl. GI Endosc. 2014, 2, 65–69. [Google Scholar] [CrossRef]
- Nishiwaki, S.; Hatakeyama, H.; Iwashita, M.; Araki, H. Transgastrostomal Observation and Management Using an Ultrathin Endoscope after Percutaneous Endoscopic Gastrostomy. In Therapeutic Gastrointestinal Endoscopy; IntechOpen: London, UK, 2011. [Google Scholar] [CrossRef][Green Version]
- Amjad, W.; Hussain, Q.; Ullah, W.; Hurairah, A. A tough scope to swallow: Endoscopic retrograde cholangiopancreatography through percutaneous endoscopic gastrostomy. Turk. J. Gastroenterol. 2018, 29, 121–123. [Google Scholar] [CrossRef]
- Lohsiriwat, V. Percutaneous endoscopic gastrostomy tube replacement: A simple procedure? World J. Gastrointest. Endosc. 2013, 5, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, C.I.; Hilden, K.; Glasgow, R.E.; Ollerenshaw, J.; Carlisle, J.G.; Fang, J.C. Evaluation of Gastropexy and Stoma Tract Maturation Using a Novel Introducer Kit for Percutaneous Gastrostomy in a Porcine Model. J. Parenter. Enter. Nutr. 2011, 35, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.T.; Milanchi, S. Malposition of percutaneous endoscopic-guided gastrostomy: Guideline and management. J. Minimal Access Surg. 2008, 4, 1. [Google Scholar] [CrossRef] [PubMed]
















Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Varvoglis, D.N.; Sanchez-Casalongue, M.; Baron, T.H.; Farrell, T.M. “Orphaned” Stomach—An Infrequent Complication of Gastric Bypass Revision. J. Clin. Med. 2022, 11, 7487. https://doi.org/10.3390/jcm11247487
Varvoglis DN, Sanchez-Casalongue M, Baron TH, Farrell TM. “Orphaned” Stomach—An Infrequent Complication of Gastric Bypass Revision. Journal of Clinical Medicine. 2022; 11(24):7487. https://doi.org/10.3390/jcm11247487
Chicago/Turabian StyleVarvoglis, Dimitrios N., Manuel Sanchez-Casalongue, Todd H. Baron, and Timothy M. Farrell. 2022. "“Orphaned” Stomach—An Infrequent Complication of Gastric Bypass Revision" Journal of Clinical Medicine 11, no. 24: 7487. https://doi.org/10.3390/jcm11247487
APA StyleVarvoglis, D. N., Sanchez-Casalongue, M., Baron, T. H., & Farrell, T. M. (2022). “Orphaned” Stomach—An Infrequent Complication of Gastric Bypass Revision. Journal of Clinical Medicine, 11(24), 7487. https://doi.org/10.3390/jcm11247487





