Clinical Significance of Ultrasound Elastography and Fibrotic Focus and Their Association in Breast Cancer
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Clinicopathological Characteristics of the Patients
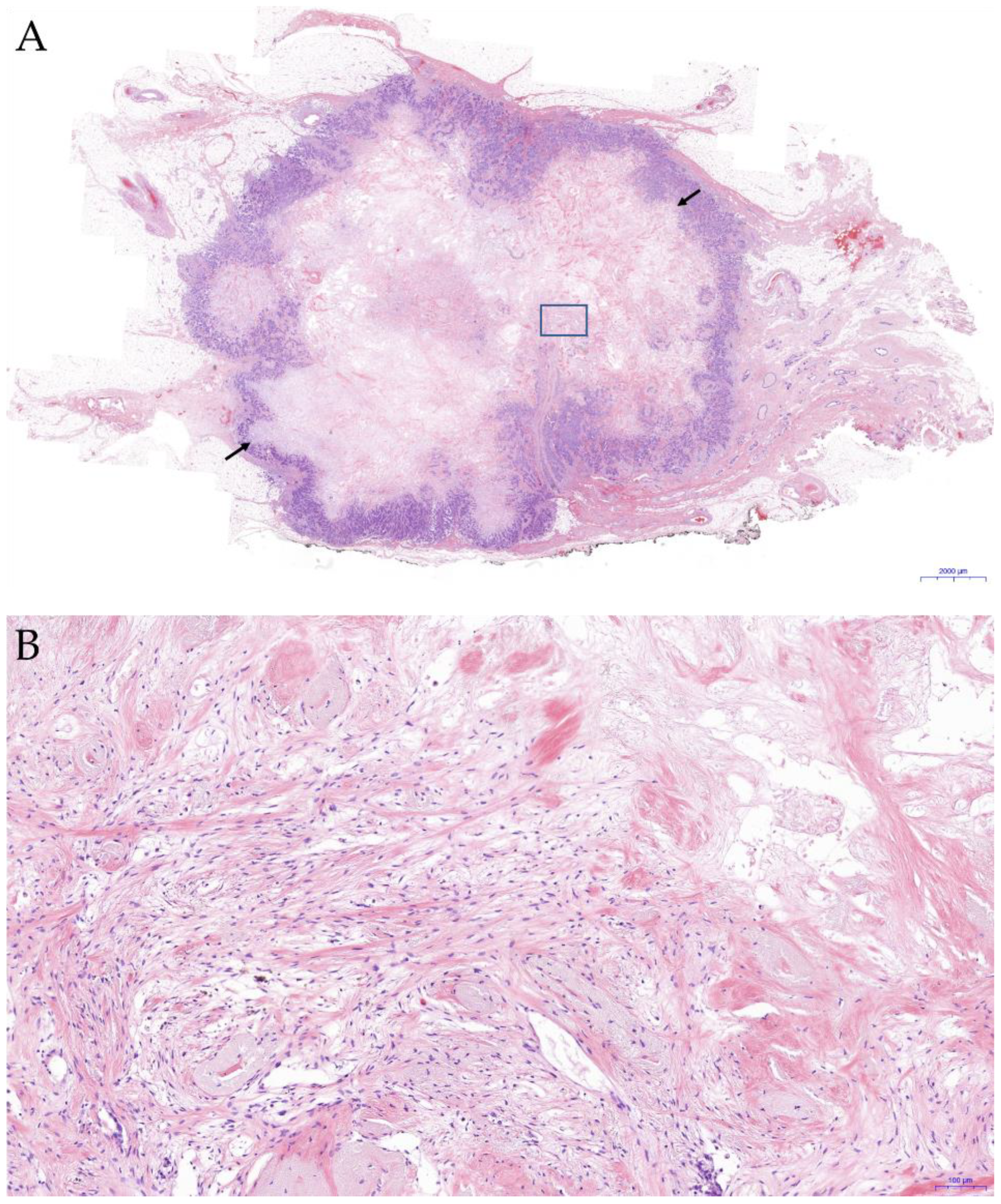
3.2. Association between US Elastography and FF
3.3. Association between US Elastography and Clinicopathological Features
3.4. Correlation between FF and Clinicopathological Features
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gennisson, J.L.; Deffieux, T.; Fink, M.; Tanter, M. Ultrasound elastography: Principles and techniques. Diagn. Interv. Imaging 2013, 94, 487–495. [Google Scholar] [CrossRef]
- Lee, S.H.; Chang, J.M.; Cho, N.; Koo, H.R.; Yi, A.; Kim, S.J.; Youk, J.H.; Son, E.J.; Choi, S.H.; Kook, S.H.; et al. Practice guideline for the performance of breast ultrasound elastography. Ultrasonography 2014, 33, 3–10. [Google Scholar] [CrossRef]
- Krouskop, T.A.; Wheeler, T.M.; Kallel, F.; Garra, B.S.; Hall, T. Elastic moduli of breast and prostate tissues under compression. Ultrason. Imaging 1998, 20, 260–274. [Google Scholar] [CrossRef]
- Meng, W.; Zhang, G.; Wu, C.; Wu, G.; Song, Y.; Lu, Z. Preliminary results of acoustic radiation force impulse (ARFI) ultrasound imaging of breast lesions. Ultrasound Med. Biol. 2011, 37, 1436–1443. [Google Scholar] [CrossRef]
- Fleury, E.F. The importance of breast elastography added to the BI-RADS (5th edition) lexicon classification. Rev. Assoc. Med. Bras. 2015, 61, 313–316. [Google Scholar] [CrossRef]
- Imtiaz, S. Breast elastography: A new paradigm in diagnostic breast imaging. Appl. Radiol. 2018, 47, 14–19. [Google Scholar] [CrossRef]
- Durhan, G.; Öztekin, P.S.; Ünverdi, H.; Değirmenci, T.; Durhan, A.; Karakaya, J.; Nercis Koşar, P.; Necip Köseoğlu, E.; Hücümenoğlu, S. Do Histopathological Features and Microcalcification Affect the Elasticity of Breast Cancer? J. Ultrasound Med. 2017, 36, 1101–1108. [Google Scholar] [CrossRef]
- Evans, A.; Whelehan, P.; Thomson, K.; McLean, D.; Brauer, K.; Purdie, C.; Baker, L.; Jordan, L.; Rauchhaus, P.; Thompson, A. Invasive breast cancer: Relationship between shear-wave elastographic findings and histologic prognostic factors. Radiology 2012, 263, 673–677. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Yamamoto, Y.; Sueta, A.; Tomiguchi, M.; Yamamoto-Ibusuki, M.; Kawasoe, T.; Hamada, A.; Iwase, H. Associations between Elastography Findings and Clinicopathological Factors in Breast Cancer. Medicine 2015, 94, e2290. [Google Scholar] [CrossRef] [PubMed]
- Cha, Y.J.; Youk, J.H.; Kim, B.G.; Jung, W.H.; Cho, N.H. Lymphangiogenesis in Breast Cancer Correlates with Matrix Stiffness on Shear-Wave Elastography. Yonsei Med. J. 2016, 57, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.; Guo, X.; Ma, B.; Zhu, L.; Liu, L. Relationship between ultrasound elastography and myofibroblast distribution in breast cancer and its clinical significance. Sci. Rep. 2016, 6, 19584. [Google Scholar] [CrossRef] [PubMed]
- Bonnans, C.; Chou, J.; Werb, Z. Remodelling the extracellular matrix in development and disease. Nat. Rev. Mol. Cell Biol. 2014, 15, 786–801. [Google Scholar] [CrossRef] [PubMed]
- Cox, T.R.; Erler, J.T. Remodeling and homeostasis of the extracellular matrix: Implications for fibrotic diseases and cancer. Dis. Model. Mech. 2011, 4, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Hasebe, T.; Sasaki, S.; Imoto, S.; Mukai, K.; Yokose, T.; Ochiai, A. Prognostic Significance of Fibrotic Focus in Invasive Ductal Carcinoma of the Breast: A Prospective Observational Study. Mod. Pathol. 2002, 15, 502–516. [Google Scholar] [CrossRef]
- Jeong, Y.J.; Park, S.H.; Mun, S.H.; Kwak, S.G.; Lee, S.J.; Oh, H.K. Association between lysyl oxidase and fibrotic focus in relation with inflammation in breast cancer. Oncol. Lett. 2018, 15, 2431–2440. [Google Scholar] [CrossRef]
- Van den Eynden, G.G.; Colpaert, C.G.; Couvelard, A.; Pezzella, F.; Dirix, L.Y.; Vermeulen, P.B.; Van Marck, E.A.; Hasbe, T. A fibrotic focus is a prognostic factor and a surrogate marker for hypoxia and (lymph)angiogenesis in breast cancer: Review of the literatureand proposal on the criteria of evaluation. Histopathology 2007, 51, 440–451. [Google Scholar] [CrossRef]
- Mujtaba, S.S.; Ni, Y.B.; Tsang, J.Y.; Chan, S.K.; Yamaguchi, R.; Tanaka, M.; Tan, P.H.; Tse, G.M. Fibrotic focus in breast carcinomas: Relationship with prognostic parameters and biomarkers. Ann. Surg. Oncol. 2013, 20, 2842–2849. [Google Scholar] [CrossRef]
- Itoh, A.; Ueno, E.; Tohno, E.; Kamma, H.; Takahashi, H.; Shiina, T.; Yamakawa, M.; Matsumura, T. Breast disease: Clinical application of US elastography for diagnosis. Radiology 2006, 239, 341–350. [Google Scholar] [CrossRef]
- Wu, B.; Sodji, Q.H.; Oyelere, A.K. Inflammation, Fibrosis and Cancer: Mechanisms, Therapeutic Options and Challenges. Cancers 2022, 14, 552. [Google Scholar] [CrossRef]
- Chandler, C.; Liu, T.; Buckanovich, R.; Coffman, L.G. The double edge sword of fibrosis in cancer. Transl. Res. 2019, 209, 55–67. [Google Scholar] [CrossRef]
- Danforth, D.N. The Role of Chronic Inflammation in the Development of Breast Cancer. Cancers 2021, 13, 3918. [Google Scholar] [CrossRef] [PubMed]
- Piersma, B.; Hayward, M.K.; Weaver, V.M. Fibrosis and cancer: A strained relationship. Biochim. Biophys. Acta Rev. Cancer 2020, 1873, 188356. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, A.; Grajo, J.R.; Dhyani, M.; Anthony, B.W.; Samir, A.E. Principles of ultrasound elastography. Abdom. Radiol. 2018, 43, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Babaniyi, O.A.; Hall, T.J.; Barbone, P.E.; Oberai, A.A. Noninvasive In-Vivo Quantification of Mechanical Heterogeneity of Invasive Breast Carcinomas. PLoS ONE 2015, 10, e0130258. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.M.; Won, J.K.; Lee, K.B.; Park, I.A.; Yi, A.; Moon, W.K. Comparison of shear-wave and strain ultrasound elastography in the differentiation of benign and malignant breast lesions. AJR Am. J. Roentgenol. 2013, 201, W347–W356. [Google Scholar] [CrossRef] [PubMed]
- Youk, J.H.; Gweon, H.M.; Son, E.J.; Kim, J.A.; Jeong, J. Shear-wave elastography of invasive breast cancer: Correlation between quantitative mean elasticity value and immunohistochemical profile. Breast Cancer Res. Treat. 2013, 138, 119–126. [Google Scholar] [CrossRef]
- Gu, J.; Polley, E.C.; Boughey, J.C.; Fazzio, R.T.; Fatemi, M.; Alizad, A. Prediction of Invasive Breast Cancer Using Mass Characteristic Frequency and Elasticity in Correlation with Prognostic Histologic Features and Immunohistochemical Biomarkers. Ultrasound Med. Biol. 2021, 47, 2193–2201. [Google Scholar] [CrossRef]
- Gregory, A.; Mehrmohammadi, M.; Denis, M.; Bayat, M.; Stan, D.L.; Fatemi, M.; Alizad, A. Effect of Calcifications on Breast Ultrasound Shear Wave Elastography: An Investigational Study. PLoS ONE 2015, 10, e0137898. [Google Scholar] [CrossRef]
- Choi, S.H.; Ko, E.Y.; Han, B.K.; Ko, E.S.; Choi, J.S.; Park, K.W. Effect of Calcifications on Shear-Wave Elastography in Evaluating Breast Lesions. Ultrasound Med. Biol. 2021, 47, 95–103. [Google Scholar] [CrossRef]
- Kayadibi, Y.; Ucar, N.; Kaya, M.F.; Yildirim, E.; Bektas, S. Characterization of Suspicious Microcalcifications on Mammography Using 2D Shear-Wave Elastography. Ultrasound Med. Biol. 2021, 47, 2532–2542. [Google Scholar] [CrossRef]

| Variables | Value (n = 151) |
|---|---|
| Age (years) | |
| Mean age ± SD, (range) | 57.6 ± 11.4 years (25–82) |
| Menopausal status, n (%) | |
| Premenopausal | 48 (31.8) |
| Postmenopausal | 103 (68.2) |
| Breast surgery method, n (%) | |
| Mastectomy | 45 (63.4) |
| Breast-conserving surgery | 26 (36.6) |
| Tumor size | |
| Mean size ± SD (range) (cm) | 1.6 ± 1.0 (0.1–6.3) |
| <2 cm, n (%) | 107 (70.9) |
| ≥2 cm, n (%) | 44 (29.1) |
| Histologic grade, n (%) | |
| I | 32 (21.2) |
| II | 53 (35.1) |
| III | 66 (43.7) |
| Lymphovascular invasion, n (%) | 32 (21.2) |
| LN metastasis, n (%) | 36 (24.2) |
| Extranodal extension, n (%) | 19 (12.8) |
| Microcalcification, n (%) | 70 (46.4) |
| Stage, n (%) | |
| I | 92 (60.9) |
| II | 44 (29.2) |
| III | 15 (9.9) |
| ER, n (%) | |
| Negative | 41 (27.2) |
| Positive | 110 (72.8) |
| PR, n (%) | |
| Negative | 47 (31.1) |
| Positive | 104 (68.9) |
| HER2 overexpression, n (%) | |
| Negative | 127 (84.1) |
| Positive | 24 (15.9) |
| Molecular subtype, n (%) | |
| Luminal A | 53 (35.1) |
| Luminal B | 61 (40.4) |
| HER2 | 17 (11.3) |
| Basal-like | 20 (13.2) |
| Bcl2, n (%) | |
| Negative | 35 (23.2) |
| Positive | 116 (76.8) |
| P53, n (%) | |
| Negative | 35 (23.2) |
| Positive | 116 (76.8) |
| Ki-67, n (%) | |
| <14% | 60 (39.7) |
| ≥14% | 91 (60.3) |
| EGFR, n (%) | |
| Negative | 119 (78.8) |
| Positive | 32 (21.2) |
| Positive fibrotic focus, n (%) | 68 (46.9) |
| Positive intratumoral inflammation, n (%) | 110 (75.3) |
| Positive peritumoral inflammation, n (%) | 117 (80.1) |
| Elastography, n (%) | |
| Equivocal | 30 (19.9) |
| Positive | 121 (80.1) |
| Adjuvant chemotherapy | 88 (58.7) |
| Adjuvant endocrine therapy | 115 (76.2) |
| Recurrence, n (%) | 15 (9.9) |
| Breast cancer-related death, n (%) | 10 (6.6) |
| Variables | Elastography | p-Value | |
|---|---|---|---|
| Equivocal | Positive | ||
| Fibrotic focus, n (%) | 0.633 | ||
| Negative | 16 (57.1) | 61 (52.1) | |
| Positive | 12 (42.9) | 56 (47.9) | |
| Fibrotic focus grade, n (%) | 0.439 | ||
| 0 | 16 (57.1) | 61 (53.5) | |
| 1 | 2 (7.1) | 8 (7.0) | |
| 2 | 9 (32.1) | 28 (24.6) | |
| 3 | 1 (3.6) | 17 (14.9) | |
| Fibrotic focus size (cm), mean ± SD | 0.2 ± 0.4 | 0.3 ± 0.5 | 0.363 |
| Intratumoral inflammation, n (%) | 0.963 | ||
| Negative | 7 (25.0) | 29 (24.6) | |
| Positive | 21 (75.0) | 89 (75.4) | |
| Peritumoral inflammation, n (%) | 0.767 | ||
| Negative | 5 (17.9) | 24 (20.3) | |
| Positive | 23 (82.1) | 94 (79.7) | |
| Age (years), mean ± SD | 53.8 ± 12.2 | 58.6 ± 11.1 | 0.040 * |
| Menopausal status, n (%) | 0.129 | ||
| Premenopausal | 13 (43.3) | 35 (28.9) | |
| Postmenopausal | 17 (56.7) | 86 (71.1) | |
| Tumor size (cm), mean ± SD | 1.2 ± 08 | 1.7 ± 1.0 | 0.004 * |
| <2 cm, n (%) | 26 (86.7) | 81 (66.9) | 0.033 * |
| ≥2 cm, n (%) | 4 (13.3) | 40 (33.1) | |
| Histologic grade, n (%) | 0.555 | ||
| I | 5 (16.7) | 27 (22.3) | |
| II | 11 36.7) | 42 (34.7) | |
| III | 14 (46.7) | 52 (43.0) | |
| Lymphovascular invasion, n (%) | 5 (16.7) | 27 (22.3) | 0.498 |
| LN metastasis, n (%) | 3 (10.0) | 33 (27.7) | 0.043 * |
| Microcalcification, n (%) | 18 (60.0) | 52 (43.0) | 0.094 |
| Stage, n (%) | 0.042 * | ||
| I | 24 (80.0) | 68 (56.2) | |
| II | 4 (13.3) | 40 (33.1) | |
| III | 2 (6.7) | 13 (10.7) | |
| Molecular subtype, n (%) | 0.513 | ||
| Luminal A | 12 (40.0) | 41 (33.9) | |
| Luminal B | 7 (23.3) | 54 (44.6) | |
| HER2 | 6 (20.0) | 11 (9.1) | |
| Basal-like | 5 (16.7) | 15 (12.4) | |
| MaxSUV on PET-CT, mean ± SD | 2.8 ± 3.2 | 2.8 ± 3.4 | 0.954 |
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Older age | 1.039 (1.001–1.079) | 0.044 * | 1.021 (0.964–1.082) | 0.477 |
| Postmenopause | 1.879 (0.826–4.275) | 0.133 | 1.327 (0.363–4.848) | 0.669 |
| Large tumor size | 2.353 (1.304–4.243) | 0.004 * | 2.493 (1.355–4.587) | 0.003 * |
| Positive lymph node metastasis | 3.453 (0.981–12.157) | 0.054 | 9.621 (0.885–104.604) | 0.063 |
| Stage II vs. Stage I, III | 3.529 (1.142–10.907) | 0.028 * | 0.429 (0.071–2.587) | 0.429 |
| Stage III vs. Stage I, II | 2.294 (0.482–10.914) | 0.297 | 0.075 (0.003–1.757) | 0.107 |
| Presence of microcalcifications | 0.502 (0.223–1.134) | 0.098 | 0.482 (0.206–1.124) | 0.091 |
| Variables | Fibrotic Focus | p-Value | |
|---|---|---|---|
| Positive | Negative | ||
| Age (years), mean ± SD | 60.6 ± 11.0 | 54.8 ± 11.2 | 0.002 * |
| Menopausal status, n (%) | 0.008 * | ||
| Premenopausal | 15 (22.1) | 33 (42.9) | |
| Postmenopausal | 53 (77.9) | 44 (57.1) | |
| Tumor size (cm), mean ± SD | 2.0 ± 1.0 | 1.3 ± 1.0 | <0.001 * |
| <2 cm, n (%) | 38 (55.9) | 65 (84.4) | <0.001 * |
| ≥2 cm, n (%) | 30 (44.1) | 12 (15.6) | |
| Histologic grade, n (%) | 0.332 | ||
| I | 11 (16.2) | 20 (26.0) | |
| II | 26 (38.2) | 24 (31.2) | |
| III | 31 (45.6) | 33 (42.9) | |
| Lymphovascular invasion, n (%) | 20(29.4) | 10 (13.0) | 0.015 * |
| LN metastasis, n (%) | 22 (32.8) | 13 (17.1) | 0.029 * |
| Extranodal extension, n (%) | 11 (16.4) | 7 (9.2) | 0.195 |
| Microcalcification, n (%) | 34 (50.0) | 36 (46.8) | 0.696 |
| Stage, n (%) | 0.004 * | ||
| I | 32 (47.1) | 57 (74.0) | |
| II | 27 (39.1) | 14 (18.2) | |
| III | 9 (13.2) | 6 (7.8) | |
| ER, n (%) | 0.628 | ||
| Negative | 17 (25.0) | 22 (28.6) | |
| Positive | 51 (75.0) | 55 (71.4) | |
| PR, n (%) | 0.554 | ||
| Negative | 19 (27.9) | 25 (32.5) | |
| Positive | 49 (72.1) | 52 (67.5) | |
| HER2 overexpression, n (%) | 0.909 | ||
| Negative | 57 (83.8) | 64 (83.1) | |
| Positive | 11 (16.2) | 13 (16.9) | |
| Molecular subtype, n (%) | 0.718 | ||
| Luminal A | 21 (30.9) | 28 (36.4) | |
| Luminal B | 32 (47.1) | 29 (37.7) | |
| HER2 | 7 (10.3) | 10 (13.0) | |
| Basal-like | 8 (11.8) | 10 (13.0) | |
| Bcl2, n (%) | 0.545 | ||
| Negative | 17 (25.0) | 16 (20.8) | |
| Positive | 51 (75.0) | 61 (79.2) | |
| P53, n (%) | 0.111 | ||
| Negative | 20 (29.4) | 14 (18.2) | |
| Positive | 48 (70.6) | 63 (81.8) | |
| Ki-67, n (%) | 0.338 | ||
| <14% | 23 (33.8) | 32 (41.6) | |
| ≥14% | 45 (66.2) | 45 (58.4) | |
| EGFR, n (%) | 0.827 | ||
| Negative | 54 (79.4) | 60 (77.9) | |
| Positive | 14 (20.6) | 17 (22.1) | |
| Positive intratumoral inflammation, n (%) | 60 (88.2) | 50 (64.9) | <0.001 * |
| Positive peritumoral inflammation, n (%) | 62 (91.2) | 55 (71.4) | 0.003 * |
| MaxSUV on PET-CT, mean ± SD | 2.6 ± 2.9 | 2.6 ± 3.0 | 0.983 |
| Adjuvant chemotherapy | 44 (64.7) | 41 (53.9) | 0.190 |
| Adjuvant endocrine therapy | 54 (79.4) | 57 (74.0) | 0.445 |
| Recurrence, n (%) | 0.419 | ||
| Yes | 8 (11.8) | 6 (7.8) | |
| No | 60 (88.2) | 71 9 (92.2) | |
| Breast cancer-related death, n (%) | 0.190 | ||
| Yes | 7 (10.4) | 3 (3.9) | |
| No | 60 (89.6) | 73 (96.1) | |
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Older age | 1.048 (1.016–1.081) | 0.003 * | 1.038 (1.003–1.074) | 0.034 * |
| Postmenopause | 2.650 (1.278–5.497) | 0.009 * | 1.588 (0.484–5.207) | 0.446 |
| Large tumor size | 2.512 (1.592–3.964) | <0.001 * | 2.272 (1.397–3.696) | 0.001 * |
| Positive lymphovascular invasion | 2.792 (1.199–6.497) | 0.017 * | 1.644 (0.542–4.987) | 0.380 |
| Positive lymph node metastasis | 2.369 (1.080–5.195) | 0.031 * | 1.920 (0.426–8.658) | 0.396 |
| Stage II vs. Stage I, III | 3.435 (1.579–7.473) | 0.002 * | 0.840 (0.193–3.647) | 0.816 |
| Stage III vs. Stage I, II | 2.672 (0.872–8.189) | 0.085 | 0.230 (0.021–2.526) | 0.229 |
| Positive intratumoral inflammation | 4.050 (1.691–9.703) | 0.002 * | 3.811 (1.435–10.123) | 0.007 * |
| Positive peritumoral inflammation | 4.133 (1.562–10.936) | 0.004 * | 1.764 (0.427–7.291) | 0.433 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, N.-R.; Oh, H.-K.; Jeong, Y.-J. Clinical Significance of Ultrasound Elastography and Fibrotic Focus and Their Association in Breast Cancer. J. Clin. Med. 2022, 11, 7435. https://doi.org/10.3390/jcm11247435
Lee N-R, Oh H-K, Jeong Y-J. Clinical Significance of Ultrasound Elastography and Fibrotic Focus and Their Association in Breast Cancer. Journal of Clinical Medicine. 2022; 11(24):7435. https://doi.org/10.3390/jcm11247435
Chicago/Turabian StyleLee, Na-Rang, Hoon-Kyu Oh, and Young-Ju Jeong. 2022. "Clinical Significance of Ultrasound Elastography and Fibrotic Focus and Their Association in Breast Cancer" Journal of Clinical Medicine 11, no. 24: 7435. https://doi.org/10.3390/jcm11247435
APA StyleLee, N.-R., Oh, H.-K., & Jeong, Y.-J. (2022). Clinical Significance of Ultrasound Elastography and Fibrotic Focus and Their Association in Breast Cancer. Journal of Clinical Medicine, 11(24), 7435. https://doi.org/10.3390/jcm11247435






