Clinical Outcome, Cognition, and Cerebrovascular Reactivity after Surgical Treatment for Moyamoya Vasculopathy: A Dutch Prospective, Single-Center Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Treatment
2.3. Clinical Follow-Up
2.4. Imaging
2.5. Cognitive Evaluation
2.6. Data-Analysis and Statistics
3. Results
3.1. Patient Characteristics and Treatment
3.2. Surgical Complications
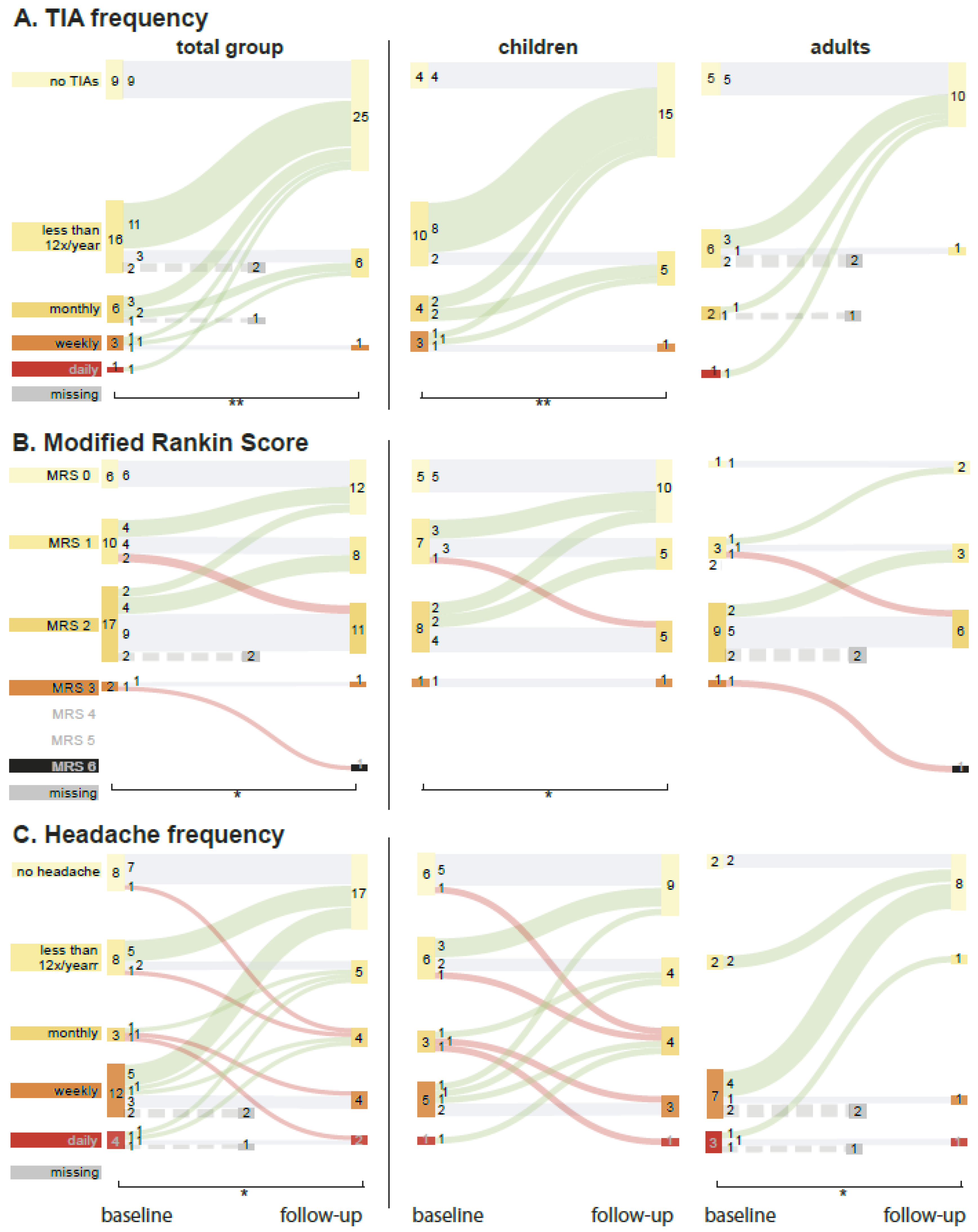
3.3. Clinical Follow-Up
3.4. Headache
3.5. Other Clinical Outcomes
3.6. mRS, (ped)NIHSS, PSOM
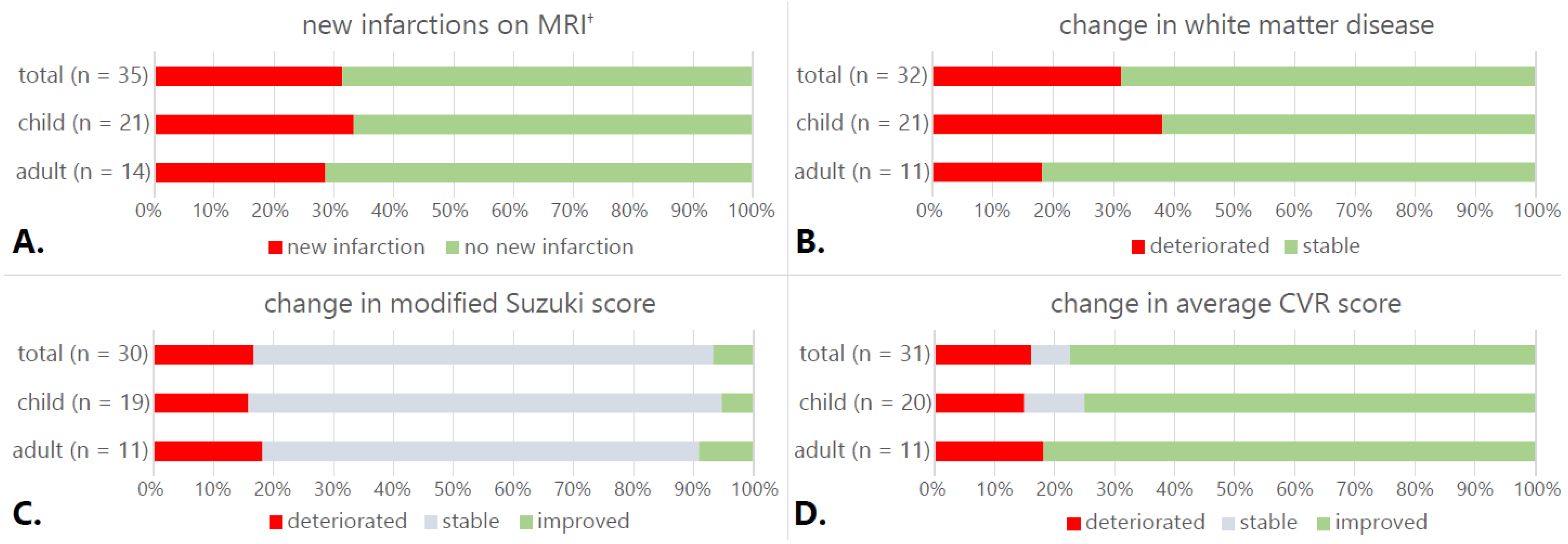
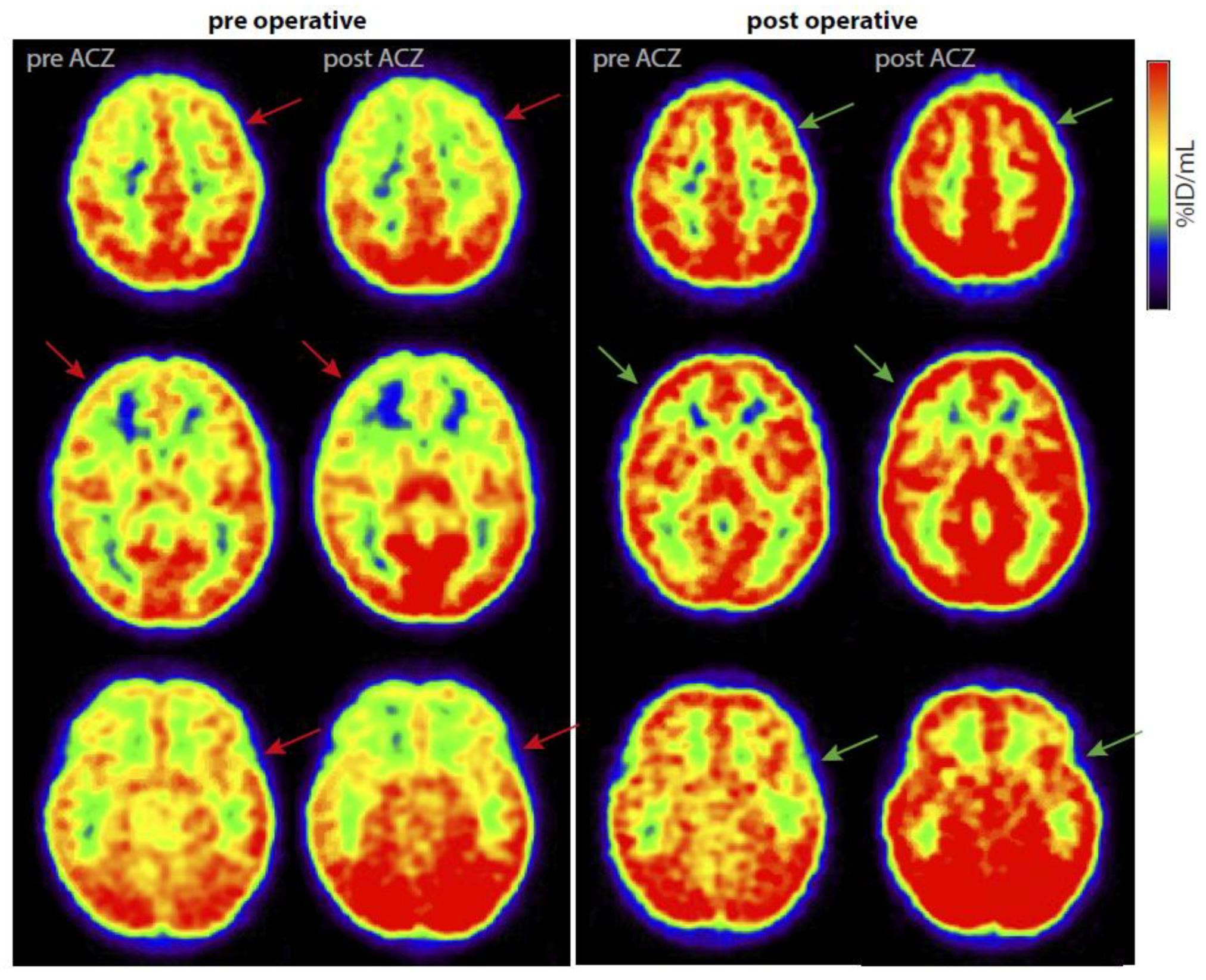
3.7. Imaging
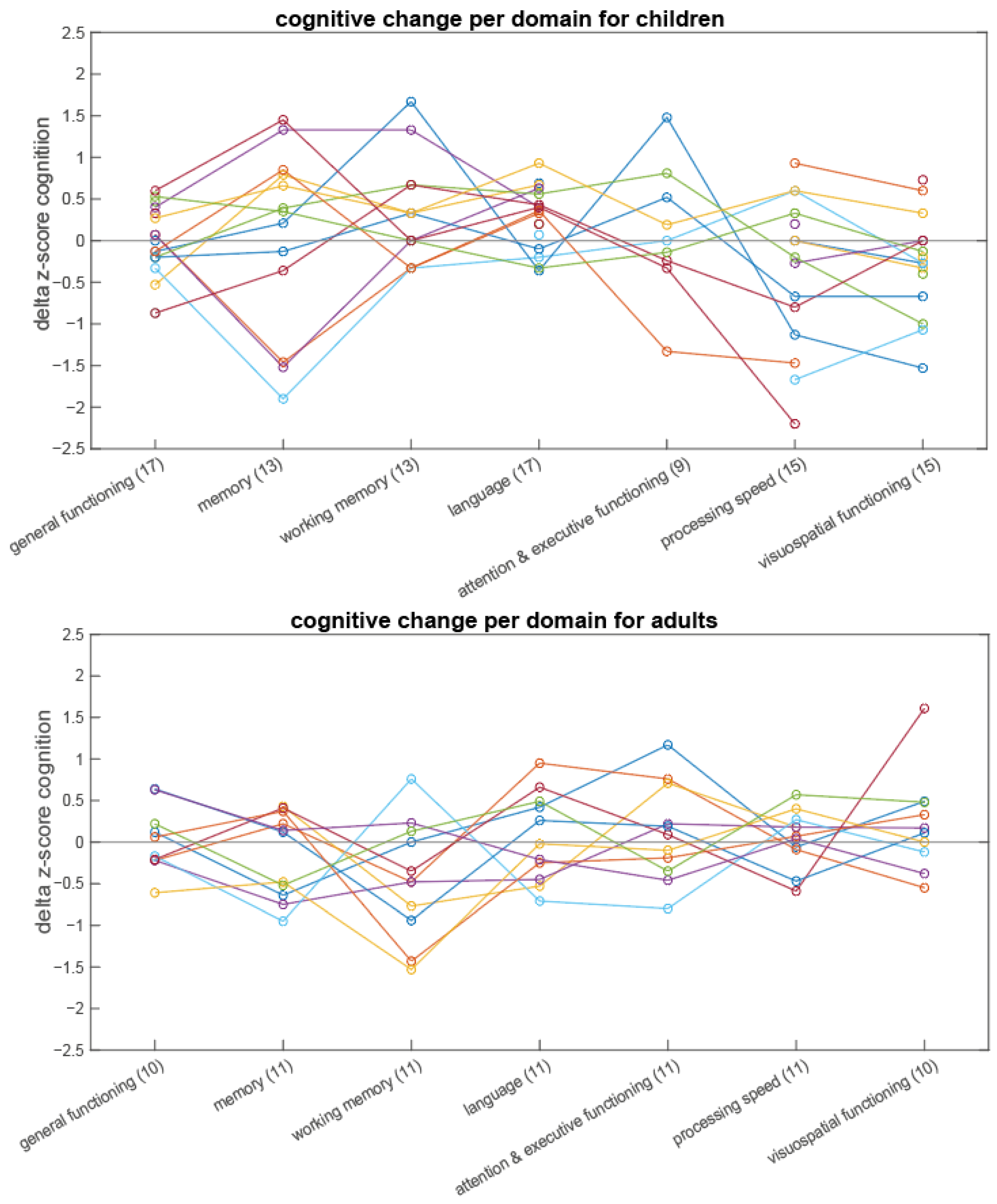
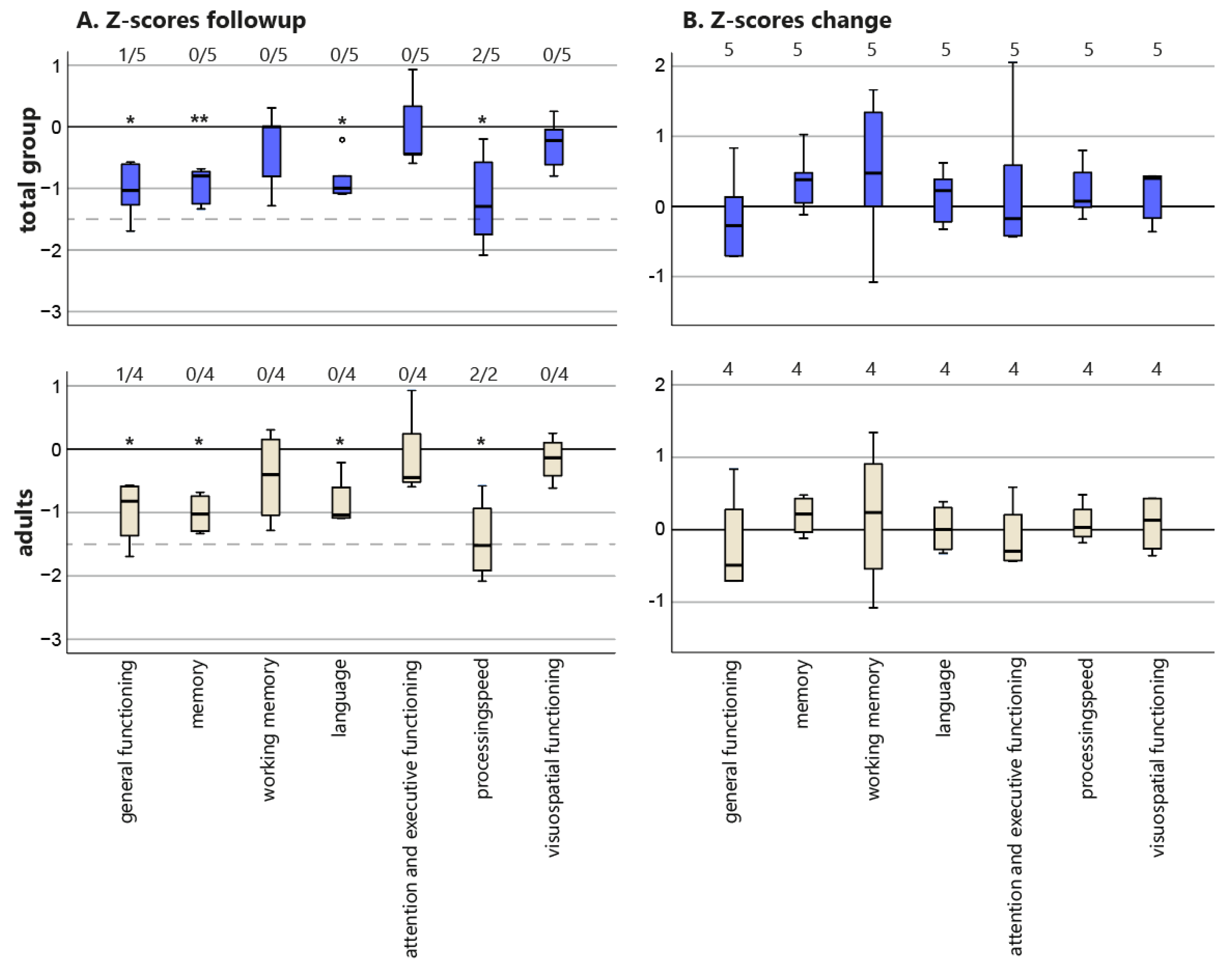
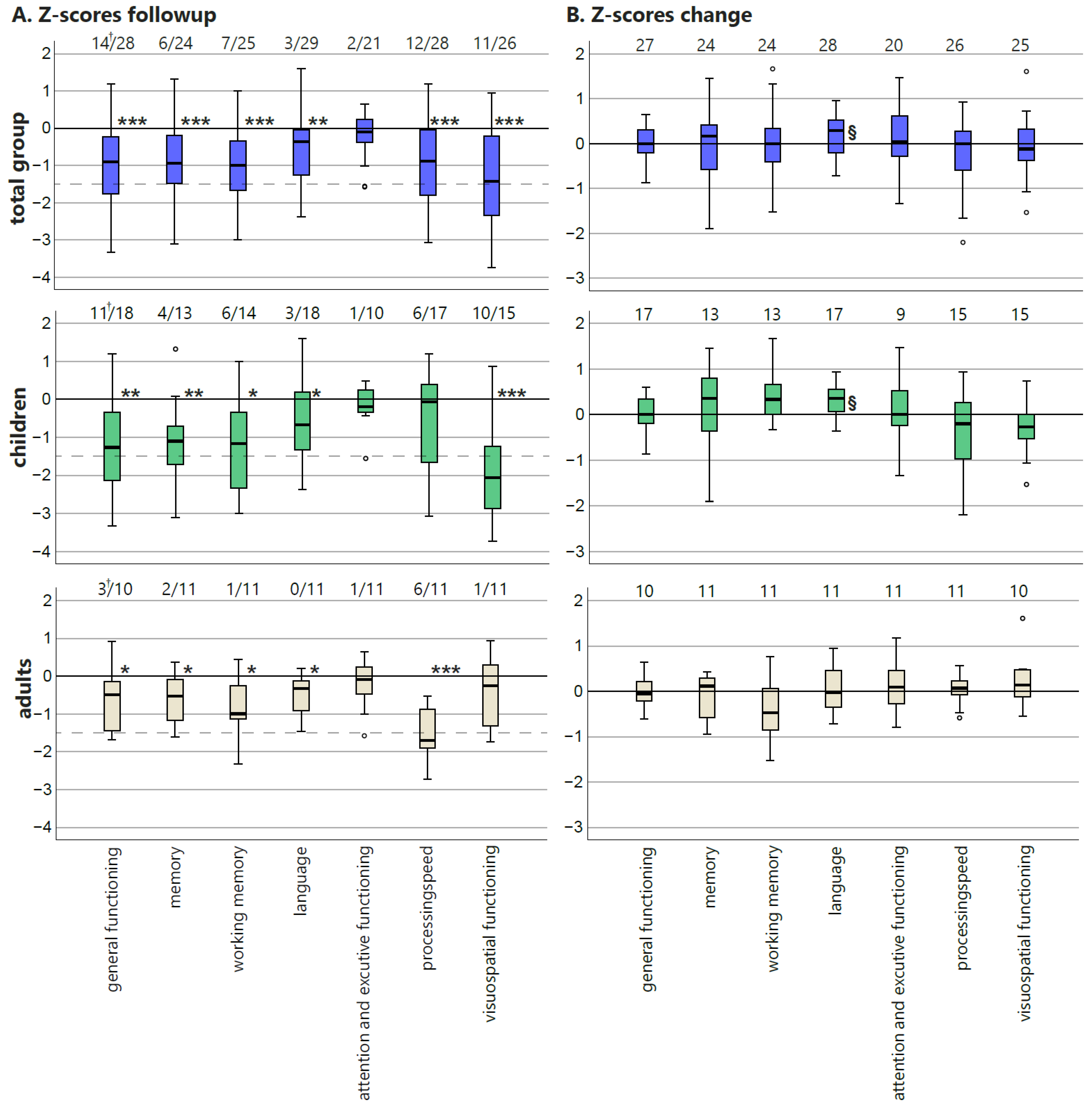
3.8. Neuropsychological Evaluation
3.9. Quality of Life
3.10. Correlation of Imaging Changes to Neurocognitive Changes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Surgical Treatment
Appendix B. Collected Characteristics
Appendix C. Additional Imaging Methods
Appendix C.1. MRI
Appendix C.2. Digital Subtraction Angiography (DSA)
Appendix C.3. [15O]H2O-PET
Appendix D
| Domains | Adults | Children |
|---|---|---|
| General Intelligence | National Adult Reading Test | Developmental age |
| Raven’s Advanced Progressive Matrices | Verbal IQ | |
| Similarities (WAIS-III) | Performance IQ | |
| Full-Scale IQ | ||
| Verbal Comprehension Index (VCI) | ||
| Perceptual Organization Index (POI) | ||
| Memory | Rey Auditory Verbal Learning Task (RAVLT) | RAVLT |
| Rey Complex Figure Test (RCFT) delayed recall | RCFT | |
| Rivermead Behavioral Memory Test (RBMT) A/B | Word list recall | |
| Paragraph recall | ||
| Working memory | Digit span (WAIS-III) | Number sequences |
| Language | Verbal Fluency | Passive Word comprehension (PPVT-III) |
| Vocabulary (WAIS-III) | Confrontation Naming (CELF-4) Active Vocabulary | |
| Boston Naming Test | CELF-4 Word Associations | |
| Attention and executive functioning | Zoo and rule-shifting task Behavioral Assessment of the Dysexecutive Syndrome (BADS) | Test of Everyday Attention for Children (TEA-Ch) |
| Stroop Color Word Test Part I and II | Zoo and rule-shifting task Behavioral Assessment of the Dysexecutive Syndrome (BADS-C) | |
| Brixton Spatial Anticipation Test | Questionnaire for Executive Functioning (BRIEF) for caregivers | |
| Processing speed | Symbol Digit Modalities Test | Processing Speed index (VSI) |
| Stroop Color Word Test Part I and II | ||
| Visuospatial functioning | Facial Recognition Test | Beery Visual Motor Integration (VMI) |
| Judgement Of Line Orientation (JLO) | ||
| RCFT copy |
Appendix E. Clinical Follow-Up of Patients with Complications of Operative Treatment
Appendix F
| Total Group (n = 35) | Baseline | Follow-Up | |||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (Range) | Valid n | Mean (SD) | Median (Range) | Valid n | ||
| NIHSS | 1 (1.48) | 0.5 (0–7) | 32 | 0.46 (0.72) | 0 (0–2) | 24 | |
| n (percentage) | n (percentage) | ||||||
| mRS baseline | 0 | 6 (17.1%) | 13 (37.1%) | ||||
| 1 | 11 (31.4%) | 8 (22.9%) | |||||
| 2 | 16 (45.7%) | 11 (31.4%) | |||||
| 3 | 2 (5.7%) | 0 (0%) | |||||
| Children(n = 21) | Baseline | Follow-Up | |||||
| Mean (SD) | Median (Range) | Validn | Mean (SD) | Median (Range) | Validn | ||
| Ped. Quality of Life | 72.6 (19.1) | 71.7 (43.5–97.8) | 15 | 74.2 (18.5) | 79.4 (39.1–96.3) | 16 | |
| Ped. Quality of Life parents | 68.6 (18.8) | 76.1 (33.7–97.8) | 21 | 69.4 (24.6) | 78.3 (17–98.8) | 19 | |
| Ped. NIHSS | 0.7 (1.1) | 0 (0–3) | 18 | 0.3 (0.6) | 0 (0–2) | 15 | |
| PSOM | 1.5 (1.7) | 1 (0–6) | 20 | 0.9 (1.2) | 0.3 (0–4) | 16 | |
| n (percentage) | n (percentage) | ||||||
| mRS baseline | 0 | 5 (23.8%) | 11 (52.3%) | ||||
| 1 | 7 (33.3%) | 5 (23.8%) | |||||
| 2 | 8 (38.1%) | 5 (23.8%) | |||||
| 3 | 1 (4.7%) | 0 (0%) | |||||
| Adults(n = 14) | Baseline | Follow-Up | |||||
| Mean (SD) | Median (Range) | Validn | Mean (SD) | Median (Range) | Validn | ||
| SF-36 Physical Component scale | 44.49 (9.31) | 43.68 (30.46–57.73) | 15 | 50.14 (7.73) | 51.6 (35.9–59.2) | 16 | |
| SF-36 Mental Component scale | 39.85 (14.05) | 42.5 (16.79–61.3) | 21 | 50.33 (11.88) | 53.6 (22.5–59.1) | 19 | |
| EQ5D VAS | 69.29 (16.71) | 65.5 (40–98) | 18 | 82 (12.26) | 82.5 (60–99) | 15 | |
| EQ5D index | 0.77 (0.27) | 0.8 (0–1) | 20 | 0.86 (0.17) | 0.93 (0.5–1) | 16 | |
| NIHSS | 1.36 (1.86) | 1 (0–7) | 21 | 0.78 (0.83) | 1 (0–2) | 17 | |
| n (percentage) | n (percentage) | ||||||
| mRS baseline | 0 | 1 (7.1%) | 2 (14.3%) | ||||
| 1 | 4 (28.6%) | 3 (21.4%) | |||||
| 2 | 8 (57.1%) | 6 (42.9%) | |||||
| 3 | 1 (7.1%) | 0 (0%) | |||||
Appendix G
Appendix H
| General Functioning | B (95%CI) | p | BF |
| Frontal baseline CVR | 8.898 × 10−4 (−0.168–0.17) | 0.991 | 0.358 |
| Middle baseline CVR | −0.085 (−0.280–0.109) | 0.375 | 0.484 |
| Posterior baseline CVR | −0.123 (−0.304–0.057) | 0.172 | 0.738 |
| Memory | B (95%CI) | p | BF |
| Frontal baseline CVR | −0.065 (−0.441–0.311) | 0.723 | 0.391 |
| Middle baseline CVR | −0.117 (−0.550–0.317) | 0.582 | 0.418 |
| Posterior baseline CVR | −0.043 (−0.430–0.344) | 0.819 | 0.38 |
| Working Memory | B (95%CI) | p | BF |
| Frontal baseline CVR | 0.055 (−0.275–0.386) | 0.731 | 0.39 |
| Middle baseline CVR | 0.301 (−0.059–0.661) | 0.097 | 1.073 |
| Posterior baseline CVR | −0.026 (−0.367–0.314) | 0.873 | 0.376 |
| Language | B (95%CI) | p | BF |
| Frontal baseline CVR | 0.072 (−0.261–0.404) | 0.662 | 0.357 |
| Middle baseline CVR | 0.013 (−0.189–0.215) | 0.899 | 0.355 |
| Posterior baseline CVR | 0.008 (−0.184–0.2) | 0.932 | 0.354 |
| Attention and Executive Functioning | B (95%CI) | p | BF |
| Frontal baseline CVR | 0.116 (−0.177–0.408) | 0.419 | 0.715 |
| Middle baseline CVR | −0.068 (−0.457–0.321) | 0.716 | 0.417 |
| Posterior baseline CVR | −0.053 (−0.390–0.283) | 0.742 | 0.413 |
| Processing Speed | B (95%CI) | p | BF |
| Frontal baseline CVR | −0.225 (−0.533–0.083) | 0.145 | 0.825 |
| Middle baseline CVR | −0.293 (−0.640–0.054) | 0.095 | 1.074 |
| Posterior baseline CVR | −0.124 (−0.443–0.194) | 0.428 | 0.461 |
| Visuo-spatial functioning | B (95%CI) | p | BF |
| Frontal baseline CVR | −0.228 (−0.474–0.018) | 0.068 | 1.341 |
| Middle baseline CVR | −0.378 (−0.634–−0.122) | 0.006 | 7.985 |
| Posterior baseline CVR | −0.314 (−0.569–−0.059) | 0.018 | 3.355 |
Appendix I. Outcome of Conservatively Treated Patients
Appendix I.1. TIAs
Appendix I.2. Headache
Appendix I.3. Clinical Scores and Functional Deficits
Appendix I.4. Other Clinical Outcome
Appendix I.5. Radiological Findings at Follow-Up
Appendix I.6. Cognitive Follow-Up
Appendix I.7. QOL
Appendix J
References
- Scott, R.M.; Smith, E.R. Moyamoya Disease and Moyamoya Syndrome. N. Engl. J. Med. 2009, 360, 1226–1237. [Google Scholar] [CrossRef] [PubMed]
- Kronenburg, A.; Braun, K.P.J.; Van Der Zwan, A.; Klijn, C.J.M. Recent Advances in Moyamoya Disease: Pathophysiology and Treatment. Curr. Neurol. Neurosci. Rep. 2014, 14, 423. [Google Scholar] [CrossRef] [PubMed]
- Kronenburg, A.; van den Berg, E.; van Schooneveld, M.M.; Braun, K.P.J.; Calviere, L.; van der Zwan, A.; Klijn, C.J.M. Cognitive Functions in Children and Adults with Moyamoya Vasculopathy: A Systematic Review and Meta-Analysis. J. Stroke 2018, 20, 332–341. [Google Scholar] [CrossRef] [PubMed]
- Fukui, M. Guidelines for the Diagnosis and Treatment of Spontaneous Occlusion of the Circle of Willis (“Moyamoya” Disease). Clin. Neurol. Neurosurg. 1997, 99, S238–S240. [Google Scholar] [CrossRef]
- Ferriero, D.M.; Fullerton, H.J.; Bernard, T.J.; Billinghurst, L.; Daniels, S.R.; Debaun, M.R.; Deveber, G.; Ichord, R.N.; Jordan, L.C.; Massicotte, P.; et al. Management of Stroke in Neonates and Children: A Scientific Statement from the American Heart Association/American Stroke Association. Stroke 2019, 50, e51–e96. [Google Scholar] [CrossRef]
- Kronenburg, A.; Deckers, P.T.; van den Berg, E.; van Schooneveld, M.M.; Vonken, E.-J.; van der Zwan, A.; van Berckel, B.N.M.; Yaqub, M.; Otte, W.; Klijn, C.J.M.; et al. The Profile of Cognitive Impairment and Hemodynamic Compromise in Moyamoya: A Single-Center Prospective Cohort Study. J. Neurosurg. 2022, 1, 1–12. [Google Scholar] [CrossRef]
- Ball, A.J.; Steinberg, G.K.; Elbers, J. Pediatric Quality of Life in Children with Moyamoya Disease and Stroke. Ann. Neurol. 2015, 78, S214–S215. [Google Scholar] [CrossRef]
- Kronenburg, A.; Esposito, G.; Fierstra, J.; Braun, K.P.; Regli, L. Combined Bypass Technique for Contemporary Revascularization of Unilateral MCA and Bilateral Frontal Territories in Moyamoya Vasculopathy. Trends Neurovascular Interv. 2014, 119, 65–70. [Google Scholar] [CrossRef]
- Ichord, R.N.; Bastian, R.; Abraham, L.; Askalan, R.; Benedict, S.; Bernard, T.J.; Beslow, L.; Dowling, M.; Friedman, N.; Jordan, L.; et al. Inter-Rater Reliability of the Pediatric NIH Stroke Scale (PedNIHSS) in a Multicenter Study. Stroke 2011, 42, 613–617. [Google Scholar] [CrossRef]
- Brott, T.; Adams, H.P.; Olinger, C.P.; Marle, J.R.; Barsan, W.G.; Biller, J.; Spilker, J.; Holleran, R.; Eberle, R.; Hertzberg, V.; et al. Measurements of Acute Cerebral Infarction: A Clinical Examination Scale. Stroke 1989, 20, 864–870. [Google Scholar] [CrossRef]
- van Swieten, J.C.; Koudstaal, P.J.; Visser, M.C.; Schouten, H.J.; van Gijn, J. Interobserver Agreement for the Assessment of Handicap in Stroke Patients. Stroke 1988, 19, 604–607. [Google Scholar] [CrossRef] [PubMed]
- DeVeber, G.A.; MacGregor, D.; Curtis, R.; Mayank, S. Neurologic Outcome in Survivors of Childhood Arterial Ischemic Stroke and Sinovenous Thrombosis. J. Child Neurol. 2000, 15, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Planning, U. Pediatric Quality of Life InventoryTM PedsQL. Available online: http://www.pedsql.org/ (accessed on 1 December 2022).
- Brazier, J.; Roberts, J.; Deverill, M. The Estimation of a Preference-Based Measure of Health from the SF-36. J. Health Econ. 2002, 21, 271–292. [Google Scholar] [CrossRef] [PubMed]
- Langsdale, T. Eq-5D. Pharmacoecon. Outcomes News 1997, 109, 3–4. [Google Scholar] [CrossRef]
- Deckers, P.T.; van Hoek, W.; Kronenburg, A.; Yaqub, M.; Siero, J.C.W.; Bhogal, A.A.; van Berckel, B.N.M.; van der Zwan, A.; Braun, K.P.J. Contralateral Improvement of Cerebrovascular Reactivity and TIA Frequency after Unilateral Revascularization Surgery in Moyamoya Vasculopathy. NeuroImage Clin. 2021, 30, 102684. [Google Scholar] [CrossRef] [PubMed]
- Fazekas, F.; Kleinert, R.; Offenbacher, H.; Schmidt, R.; Kleinert, G.; Payer, F.; Radner, H.; Lechner, H. Pathologic Correlates of Incidental MRI White Matter Signal Hyperintensities. Neurology 1993, 43, 1683. [Google Scholar] [CrossRef]
- Kang, K.H.; Kim, H.S.; Kim, S.Y. Quantitative Cerebrovascular Reserve Measured by Acetazolamide-Challenged Dynamic CT Perfusion in Ischemic Adult Moyamoya Disease: Initial Experience with Angiographic Correlation. Am. J. Neuroradiol. 2008, 29, 1487–1493. [Google Scholar] [CrossRef]
- Lezak, M.D.; Howieson, D.B.; Loring, D.W.; Fischer, J.S. Neuropsychological Assessment; Oxford University Press: Cary, NC, USA, 2004; ISBN 0195111214. [Google Scholar]
- Kass, R.E.; Raftery, A.E. Bayes Factors. J. Am. Stat. Assoc. 1995, 90, 773–795. [Google Scholar] [CrossRef]
- Yu, J.; Shi, L.; Guo, Y.; Xu, B.; Xu, K. Progress on Complications of Direct Bypass for Moyamoya Disease. Int. J. Med. Sci. 2016, 13, 578–587. [Google Scholar] [CrossRef]
- Guzman, R.; Lee, M.; Achrol, A.; Bell-Stephens, T.; Kelly, M.; Do, H.M.; Marks, M.P.; Steinberg, G.K. Clinical Outcome after 450 Revascularization Procedures for Moyamoya Disease: Clinical Article. J. Neurosurg. 2009, 111, 927–935. [Google Scholar] [CrossRef]
- Khan, N.; Achrol, A.S.; Guzman, R.; Burns, T.C.; Dodd, R.; Bell-Stephens, T.; Steinberg, G.K. Sex Differences in Clinical Presentation and Treatment Outcomes in Moyamoya Disease. Neurosurgery 2012, 71, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Calviere, L.; Loubiere, P.; Planton, M.; Cazzola, V.; Catalaa, I.; Mirabel, H.; Sol, J.C.; Bonneville, F. Decreased Frontal White-Matter Diffusion and Improved Cognitive Flexibility after Burr-Hole Surgery in Moyamoya Angiopathy. BMC Neurol. 2020, 20, 30. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, S.; Yoshimoto, T.; Hashimoto, N.; Okada, Y.; Tsuji, I.; Tominaga, T.; Nakagawara, J.; Takahashi, J.C.; Yamada, K.; Tomata, Y.; et al. Effects of Extracranial-Intracranial Bypass for Patients with Hemorrhagic Moyamoya Disease: Results of the Japan Adult Moyamoya Trial. Stroke 2014, 45, 1415–1421. [Google Scholar] [CrossRef] [PubMed]
- Funaki, T.; Takahashi, J.C.; Takagi, Y.; Kikuchi, T.; Yoshida, K.; Mitsuhara, T.; Kataoka, H.; Okada, T.; Fushimi, Y.; Miyamoto, S. Unstable Moyamoya Disease: Clinical Features and Impact on Perioperative Ischemic Complications. J. Neurosurg. 2015, 122, 400–407. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, H.; Yoo, M.; Jin, S.; Lee, S.; Choi, B.S.; Kim, H.Y.; Jin, S.C. Angiographic and Clinical Outcomes of Non-Patent Anastomosis after Bypass Surgery in Adult Moyamoya Disease. Acta Neurochir. 2019, 161, 379–384. [Google Scholar] [CrossRef]
- Suzuki, Y.; Negoro, M.; Shibuya, M.; Yoshida, J.; Negoro, T.; Watanabe, K. Surgical Treatment for Pediatric Moyamoya Disease: Use of the Superficial Temporal Artery for Both Areas Supplied by the Anterior and Middle Cerebral Arteries. Neurosurgery 1997, 40, 324–330. [Google Scholar] [CrossRef]
- Blauwblomme, T.; Mathon, B.; Naggara, O.; Kossorottof, M.; Bourgeois, M.; Puget, S.; Meyer, P.; Brousse, V.; De Montalembert, M.; Brunelle, F.; et al. Long-Term Outcome after Multiple Burr Hole Surgery in Children with Moyamoya Angiopathy: A Single-Center Experience in 108 Hemispheres. Neurosurgery 2017, 80, 950–956. [Google Scholar] [CrossRef]
- Gao, B.; Kang, K.; Zhang, J.; Zhang, D.; Zhao, X. Clinical Characteristics and Long-Term Outcome of Headaches Associated with Moyamoya Disease in the Chinese Population—A Cohort Study. Front. Neurol. 2020, 11, 605636. [Google Scholar] [CrossRef]
- Han, J.S.; Abou-Hamden, A.; Mandell, D.M.; Poublanc, J.; Crawley, A.P.; Fisher, J.A.; Mikulis, D.J.; Tymianski, M. Impact of Extracranial-Intracranial Bypass on Cerebrovascular Reactivity and Clinical Outcome in Patients with Symptomatic Moyamoya Vasculopathy. Stroke 2011, 42, 3047–3054. [Google Scholar] [CrossRef]
- Roder, C.; Haas, P.; Fudali, M.; Milian, M.; Ernemann, U.; Meyer, P.T.; Tatagiba, M.; Khan, N. Neuropsychological Impairment in Adults with Moyamoya Angiopathy: Preoperative Assessment and Correlation to MRI and H215O PET. Neurosurg. Rev. 2020, 43, 1615–1622. [Google Scholar] [CrossRef]
- Silvestrini, M.; Pasqualetti, P.; Baruffaldi, R.; Bartolini, M.; Handouk, Y.; Matteis, M.; Moffa, F.; Provinciali, L.; Vernieri, F. Cerebrovascular Reactivity and Cognitive Decline in Patients with Alzheimer Disease. Stroke 2006, 37, 1010–1015. [Google Scholar] [CrossRef] [PubMed]
- Hever, P.; Alamri, A.; Tolias, C. Moyamoya Angiopathy—Is There a Western Phenotype? Br. J. Neurosurg. 2015, 29, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Zeifert, P.D.; Karzmark, P.; Bell-Stephens, T.E.; Steinberg, G.K.; Dorfman, L.J. Neurocognitive Performance after Cerebral Revascularization in Adult Moyamoya Disease. Stroke 2017, 48, 1514–1517. [Google Scholar] [CrossRef] [PubMed]
- Hogan, A.M.; Kirkham, F.J.; Isaacs, E.B.; Wade, A.M.; Vargha-Khadem, F. Intellectual Decline in Children with Moyamoya and Sickle Cell Anaemia. Dev. Med. Child Neurol. 2005, 47, 824–829. [Google Scholar] [CrossRef]
- Kazumata, K.; Tha, K.K.; Tokairin, K.; Ito, M.; Uchino, H.; Kawabori, M.; Sugiyama, T. Brain Structure, Connectivity, and Cognitive Changes Following Revascularization Surgery in Adult Moyamoya Disease. Clin. Neurosurg. 2019, 85, E943–E952. [Google Scholar] [CrossRef]
- Hara, S.; Kudo, T.; Hayashi, S.; Inaji, M.; Tanaka, Y.; Maehara, T.; Ishii, K.; Nariai, T. Improvement in Cognitive Decline after Indirect Bypass Surgery in Adult Moyamoya Disease: Implication of 15O-Gas Positron Emission Tomography. Ann. Nucl. Med. 2020, 34, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, K.; Chida, K.; Kobayashi, M.; Kubo, Y.; Yoshida, K.; Terasaki, K.; Ogasawara, K. Two-Year Clinical, Cerebral Hemodynamic, and Cognitive Outcomes of Adult Patients Undergoing Medication Alone for Symptomatically Ischemic Moyamoya Disease without Cerebral Misery Perfusion: A Prospective Cohort Study. Neurosurgery 2019, 84, 1233–1241. [Google Scholar] [CrossRef]
- Hsu, Y.H.; Chen, Y.F.; Yang, S.H.; Yang, C.C.; Kuo, M.F. Postoperative Change of Neuropsychological Function after Indirect Revascularization in Childhood Moyamoya Disease: A Correlation with Cerebral Perfusion Study. Child’s Nerv. Syst. 2020, 36, 1245–1253. [Google Scholar] [CrossRef]
- Lee, J.Y.; Phi, J.H.; Wang, K.C.; Cho, B.K.; Shin, M.S.; Kim, S.K. Neurocognitive Profiles of Children with Moyamoya Disease before and after Surgical Intervention. Cerebrovasc. Dis. 2011, 31, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.; Lee, E.-Y.; Park, S.-E.; Park, E.-K.; Kim, J.-S.; Kim, D.-S.; Shim, K.-W. Neuropsychological Impacts of Indirect Revascularization for Pediatric Moyamoya Disease. Child’s Nerv. Syst. 2018, 34, 1199–1206. [Google Scholar] [CrossRef]
- Engelen, V.; Haentjens, M.M.; Detmar, S.B.; Koopman, H.M.; Grootenhuis, M.A. Health Related Quality of Life of Dutch Children: Psychometric Properties of the PedsQL in the Netherlands. BMC Pediatr. 2009, 9, 68. [Google Scholar] [CrossRef] [PubMed]
- Kalra, N.; Bautista, M.; McCullagh, H.; Tyagi, A. PedsQL Score Post Encephalo-Duro-Arterio-Myo-Synangiosis Procedure for Moyamoya Disease: A Single Center Experience. World Neurosurg. 2020, 144, e674–e678. [Google Scholar] [CrossRef] [PubMed]
- König, H.-H.; Bernert, S.; Angermeyer, M.C.; Matschinger, H.; Martinez, M.; Vilagut, G.; Haro, J.M.; de Girolamo, G.; de Graaf, R.; Kovess, V.; et al. Comparison of Population Health Status in Six European Countries. Med. Care 2009, 47, 255–261. [Google Scholar] [CrossRef] [PubMed]
| Total Group (n = 35) | Children (n = 21) | Adults (n = 14) | |||||
|---|---|---|---|---|---|---|---|
| Sex | Female | 27 | 77.10% | 15 | 71.40% | 12 | 85.70% |
| Moyamoya diagnosis | MMD unilateral | 1 | 2.90% | 0 | 0.00% | 1 | 7.10% |
| MMD bilateral | 22 | 62.90% | 11 | 52.40% | 11 | 78.60% | |
| MMS unilateral | 3 | 8.60% | 3 | 14.30% | 0 | 0.00% | |
| MMS bilateral | 9 | 25.70% | 7 | 33.30% | 2 | 14.30% | |
| Age at follow-up in years (mean (SD)) | 20.6 (15.5) | 11.0 (4.1) | 38.8 (12.4) | ||||
| Time between baseline and follow-up in months (median (min-max)) | 21 (14–72) | 21 (14–72) | 20 (14–24) | ||||
| Time between last OR and follow-up in months (median (min–max)) | 15 (10–27) | 16 (10–27) | 12 (10–24) | ||||
| Treatment type | Bilateral treatment | 21 | 60.00% | 16 | 76.20% | 5 | 35.70% |
| Unilateral treatment | 14 | 40.00% | 5 | 23.80% | 9 | 64.30% | |
| Total patients with direct bypass | 29 | 82.90% | 15 | 71.40% | 14 | 100.00% | |
| Total patients with frontal procedure | 13 | 37.10% | 13 | 61.90% | 0 | 0.00% | |
| General Functioning | B (95%CI) | p | BF |
| Adult vs. child | 0.14 (−0.345–0.624) | 0.552 | 0.325 |
| Infarct score change | −0.103 (−0.996–0.791) | 0.811 | 0.316 |
| MSS change | −0.045 (−0.504–0.414) | 0.837 | 0.295 |
| WMD score change | 0.942 (−0.641–2.525) | 0.226 | 0.469 |
| CVR score change | −0.053 (−0.267–0.161) | 0.610 | 0.314 |
| Other reason for cognitive defect | 0.307 (−0.399–1.013) | 0.371 | 0.361 |
| Memory | B (95%CI) | p | BF |
| Adult vs. child | −0.606 (−1.469–0.258) | 0.155 | 0.813 |
| Infarct score change | 1.326 (−0.583–3.236) | 0.158 | 0.854 |
| mSS change | −0.963 (−1.741–−0.185) | 0.019 | 2.474 |
| WMD score change | −0.972 (−4.942–2.997) | 0.608 | 0.608 |
| CVR score change | −0.020 (−0.368–0.329) | 0.905 | 0.571 |
| Other reason for cognitive defect | 0.144 (−1.821–2.11) | 0.877 | 0.630 |
| Working Memory | B (95%CI) | p | BF |
| Adult vs. child | −1.057 (−1.974–−0.140) | 0.027 | 1.965 |
| Infarct score change | 0.294 (−1.733–2.322) | 0.760 | 0.51 |
| mSS change | 0.465 (−0.360–1.291) | 0.247 | 0.599 |
| WMD score change | −0.609 (−4.823–3.605) | 0.761 | 0.505 |
| CVR score change | −0.191 (−0.561–0.179) | 0.286 | 0.585 |
| Other reason for cognitive defect | −0.652 (−2.739–1.435) | 0.514 | 0.483 |
| Language | B (95%CI) | p | BF |
| Adult vs. child | −0.330 (−0.788–0.129) | 0.148 | 0.682 |
| Infarct score change | 0.11 (−0.753–0.974) | 0.791 | 0.360 |
| mSS change | −0.347 (−0.791–0.096) | 0.117 | 0.686 |
| WMD score change | −0.110 (−1.640–1.421) | 0.882 | 0.356 |
| CVR score change | 0.035 (−0.172–0.242) | 0.727 | 0.375 |
| Other reason for cognitive defect | −0.095 (−0.778–0.587) | 0.772 | 0.366 |
| Attention and Executive Functioning | B (95%CI) | p | BF |
| Adult vs. child | 0.172 (−0.710–1.055) | 0.676 | 0.528 |
| Infarct score change | −1.706 (−3.722–0.31) | 0.090 | 1.214 |
| mSS change | −0.186 (−1.044–0.671) | 0.642 | 0.526 |
| WMD score change | 0.678 (−3.322–4.678) | 0.716 | 0.655 |
| CVR score change | −0.144 (−0.496–0.208) | 0.387 | 0.658 |
| Other reason for cognitive defect | 1.338 (−0.519–3.196) | 0.141 | 0.716 |
| Processing Speed | B (95%CI) | p | BF |
| Adult vs. child | 0.308 (−0.416–1.031) | 0.381 | 0.445 |
| Infarct score change | −0.781 (−2.154–0.592) | 0.245 | 0.424 |
| mSS change | 0.234 (−0.513–0.98) | 0.517 | 0.366 |
| WMD score change | 1.931 (−0.496–4.359) | 0.111 | 0.610 |
| CVR score change | −0.036 (−0.371–0.298) | 0.821 | 0.365 |
| Other reason for cognitive defect | −0.474 (−2.260–1.312) | 0.582 | 0.400 |
| Visuo-spatial functioning | B (95%CI) | p | BF |
| Adult vs. child | 0.321 (−0.298–0.94) | 0.288 | 1.326 |
| Infarct score change | 0.317 (−0.820–1.454) | 0.563 | 0.854 |
| mSS change | −0.020 (−0.595–0.554) | 0.941 | 0.668 |
| WMD score change | 2.11 (0.119–4.101) | 0.039 | 2.205 |
| CVR score change | −0.256 (−0.530–0.017) | 0.064 | 1.632 |
| Other reason for cognitive defect | −0.097 (−0.992–0.799) | 0.822 | 0.677 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deckers, P.T.; Kronenburg, A.; van den Berg, E.; van Schooneveld, M.M.; Vonken, E.-J.P.A.; Otte, W.M.; van Berckel, B.N.M.; Yaqub, M.; Klijn, C.J.M.; van der Zwan, A.; et al. Clinical Outcome, Cognition, and Cerebrovascular Reactivity after Surgical Treatment for Moyamoya Vasculopathy: A Dutch Prospective, Single-Center Cohort Study. J. Clin. Med. 2022, 11, 7427. https://doi.org/10.3390/jcm11247427
Deckers PT, Kronenburg A, van den Berg E, van Schooneveld MM, Vonken E-JPA, Otte WM, van Berckel BNM, Yaqub M, Klijn CJM, van der Zwan A, et al. Clinical Outcome, Cognition, and Cerebrovascular Reactivity after Surgical Treatment for Moyamoya Vasculopathy: A Dutch Prospective, Single-Center Cohort Study. Journal of Clinical Medicine. 2022; 11(24):7427. https://doi.org/10.3390/jcm11247427
Chicago/Turabian StyleDeckers, Pieter Thomas, Annick Kronenburg, Esther van den Berg, Monique M. van Schooneveld, Evert-Jan P. A. Vonken, Willem M. Otte, Bart N. M. van Berckel, Maqsood Yaqub, Catharina J. M. Klijn, Albert van der Zwan, and et al. 2022. "Clinical Outcome, Cognition, and Cerebrovascular Reactivity after Surgical Treatment for Moyamoya Vasculopathy: A Dutch Prospective, Single-Center Cohort Study" Journal of Clinical Medicine 11, no. 24: 7427. https://doi.org/10.3390/jcm11247427
APA StyleDeckers, P. T., Kronenburg, A., van den Berg, E., van Schooneveld, M. M., Vonken, E.-J. P. A., Otte, W. M., van Berckel, B. N. M., Yaqub, M., Klijn, C. J. M., van der Zwan, A., & Braun, K. P. J. (2022). Clinical Outcome, Cognition, and Cerebrovascular Reactivity after Surgical Treatment for Moyamoya Vasculopathy: A Dutch Prospective, Single-Center Cohort Study. Journal of Clinical Medicine, 11(24), 7427. https://doi.org/10.3390/jcm11247427





