Treatment of Femoral Shaft Pseudarthrosis, Case Series and Medico-Legal Implications
Abstract
1. Introduction
2. Materials and Methods
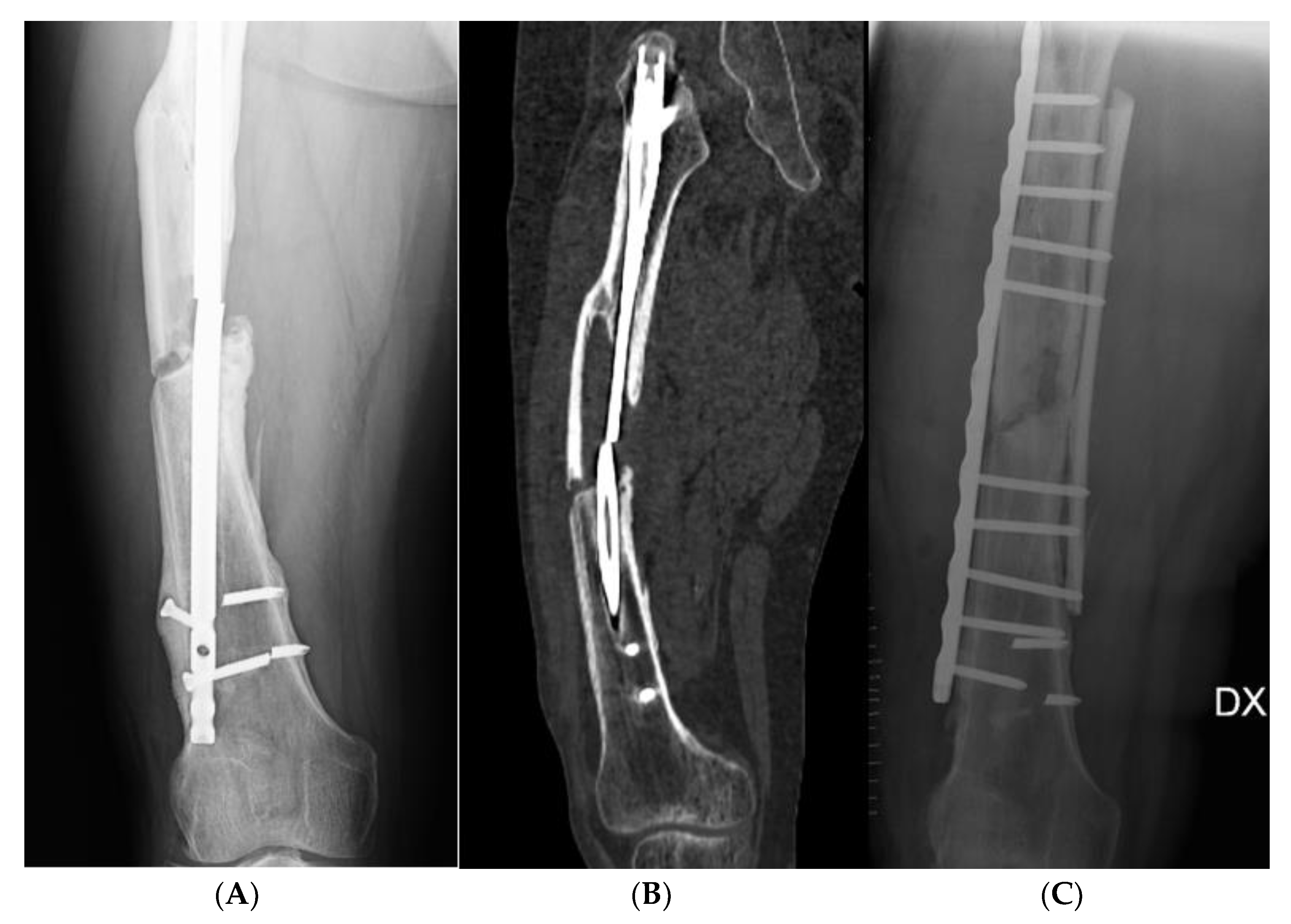
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Basile, G.; Avato, F.M.; Passeri, A.; Accetta, R.; Amadei, F.; Giorgetti, A.; Castoldi, D.; Fozzato, S. Atrophic Pseudarthrosis of Humeral Diaphyseal Fractures: Medico-Legal Implications and Methodological Analysis of the Evaluation. Acta Biomed. 2022, 93, e2022176. [Google Scholar] [CrossRef] [PubMed]
- Lambiris, E.; Panagopoulos, A.; Zouboulis, P.; Sourgiadaki, E. Current Concepts: Aseptic Nonunion of Femoral Shaft Diaphysis. Eur. J. Trauma Emerg. Surg. 2007, 33, 120–134. [Google Scholar] [CrossRef] [PubMed]
- Perisano, C.; Greco, T.; Polichetti, C.; Inverso, M.; Maccauro, G. Antibiotic-Coated Nail in Open Tibial Fracture: A Retrospective Case Series. J. Funct. Morphol. Kinesiol. 2021, 6, 97. [Google Scholar] [CrossRef] [PubMed]
- Mundi, R.; Axelrod, D.; Heels-Ansdell, D.; Chaudhry, H.; Ayeni, O.R.; Petrisor, B.; Busse, J.W.; Thabane, L.; Bhandari, M. Nonunion in Patients with Tibial Shaft Fractures: Is Early Physical Status Associated with Fracture Healing? Cureus 2020, 12, e7649. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-C. Aseptic Femoral Nonunion Treated with Exchange Locked Nailing with Intramedullary Augmentation Cancellous Bone Graft. J. Orthop. Surg. Res. 2022, 17, 339. [Google Scholar] [CrossRef]
- Galal, S. Minimally Invasive Plate Osteosynthesis Has Equal Safety to Reamed Intramedullary Nails in Treating Gustilo-Anderson Type I, II and III-A Open Tibial Shaft Fractures. Injury 2018, 49, 866–870. [Google Scholar] [CrossRef]
- Yang, J.; Zhang, X.; Liang, W.; Chen, G.; Ma, Y.; Zhou, Y.; Fen, R.; Jiang, K. Efficacy of Adjuvant Treatment for Fracture Nonunion/Delayed Union: A Network Meta-Analysis of Randomized Controlled Trials. BMC Musculoskelet. Disord. 2022, 23, 481. [Google Scholar] [CrossRef]
- Auersperg, V.; Trieb, K. Extracorporeal Shock Wave Therapy: An Update. EFORT Open Rev. 2020, 5, 584–592. [Google Scholar] [CrossRef]
- Sansone, V.; Ravier, D.; Pascale, V.; Applefield, R.; Del Fabbro, M.; Martinelli, N. Extracorporeal Shockwave Therapy in the Treatment of Nonunion in Long Bones: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 1977. [Google Scholar] [CrossRef]
- Rupp, M.; Biehl, C.; Budak, M.; Thormann, U.; Heiss, C.; Alt, V. Diaphyseal Long Bone Nonunions—Types, Aetiology, Economics, and Treatment Recommendations. Int. Orthop. 2018, 42, 247–258. [Google Scholar] [CrossRef]
- Wu, S.; Quan, K.; Mei, J.; Dai, M.; Song, S. Cortical Allograft Strut Augmented with Platelet-Rich Plasma for the Treatment of Long Bone Non-Union in Lower Limb—A Pilot Study. BMC Musculoskelet. Disord. 2022, 23, 512. [Google Scholar] [CrossRef] [PubMed]
- Attum, B.; Douleh, D.; Whiting, P.S.; White-Dzuro, G.A.; Dodd, A.C.; Shen, M.S.; Mir, H.R.; Obremskey, W.T.; Sethi, M.K. Outcomes of Distal Femur Nonunions Treated with a Combined Nail/Plate Construct and Autogenous Bone Grafting. J. Orthop. Trauma 2017, 31, e301–e304. [Google Scholar] [CrossRef] [PubMed]
- Perisano, C.; Cianni, L.; Polichetti, C.; Cannella, A.; Mosca, M.; Caravelli, S.; Maccauro, G.; Greco, T. Plate Augmentation in Aseptic Femoral Shaft Nonunion after Intramedullary Nailing: A Literature Review. Bioengineering 2022, 9, 560. [Google Scholar] [CrossRef] [PubMed]
- Ciatti, C.; Maniscalco, P.; Quattrini, F.; Gattoni, S.; Magro, A.; Capelli, P.; Banchini, F.; Fiazza, C.; Pavone, V.; Puma Pagliarello, C.; et al. The Epidemiology of Proximal Femur Fractures during COVID-19 Emergency in Italy: A Multicentric Study. Acta Biomed. 2021, 92, e2021398. [Google Scholar] [CrossRef]
- Gui, L. Arto inferiore. In Fratture e lussazioni; A. Gaggi Publisher: Bologna, Italy, 1973; pp. 312–428. [Google Scholar]
- Mastroroberto, L.; Pizzorno, E. La semeiotica medico-legale per l’accertamento dell’invalidità permanente” (la metodologia indicata dalla guida dell’American Medical Association ed il suo utilizzo nel sistema italiano); Giuffrè Editore: Milan, Italy, 2016. [Google Scholar]
- Browner, B.D.; Jupiter, J.B.; Krettek, C.; Anderson, P.A. Skeletal Trauma: Basic Science, Management, and Reconstruction, 2-Volume Set: Basic Science, Management, and Reconstruction. 2 Vol Set, 6th ed.; Elsevier: Amsterdam, The Netherlands, 2019; ISBN 9780323611152. [Google Scholar]
- Marongiu, G.; Dolci, A.; Verona, M.; Capone, A. The Biology and Treatment of Acute Long-Bones Diaphyseal Fractures: Overview of the Current Options for Bone Healing Enhancement. Bone Rep. 2020, 12, 100249. [Google Scholar] [CrossRef]
- Andrzejowski, P.; Giannoudis, P.V. The ‘Diamond Concept’ for Long Bone Non-Union Management. J. Orthop. Traumatol. 2019, 20, 21. [Google Scholar] [CrossRef]
- Senos, R.; Roberto-Rodrigues, M.; Fernandes, R.M.P.; Santos, T.M.P.; Viana, L.P.; Lima, I.; Guzman-Silva, M.A.; Gomes, M.S.; Rici, R.E.G.; Kfoury Júnior, J.R. Nandrolone Decanoate in Induced Fracture Nonunion with Vascular Deficit in Rat Model: Morphological Aspects. Musculoskelet. Surg. 2020, 104, 303–311. [Google Scholar] [CrossRef]
- Busardò, F.P.; Frati, P.; Sanzo, M.D.; Napoletano, S.; Pinchi, E.; Zaami, S.; Fineschi, V. The Impact of Nandrolone Decanoate on the Central Nervous System. Curr. Neuropharmacol. 2015, 13, 122–131. [Google Scholar] [CrossRef]
- Kouzelis, A.T.; Kourea, H.; Megas, P.; Panagiotopoulos, E.; Marangos, M.; Lambiris, E. Does Graded Reaming Affect the Composition of Reaming Products in Intramedullary Nailing of Long Bones? Orthopedics 2004, 27, 852–856. [Google Scholar] [CrossRef]
- Ding, P.; Chen, Q.; Zhang, C.; Yao, C. Revision with Locking Compression Plate by Compression Technique for Diaphyseal Nonunions of the Femur and the Tibia: A Retrospective Study of 54 Cases. Biomed Res. Int. 2021, 2021, 9905067. [Google Scholar] [CrossRef]
- Lodde, M.F.; Raschke, M.J.; Stolberg-Stolberg, J.; Everding, J.; Rosslenbroich, S.; Katthagen, J.C. Union Rates and Functional Outcome of Double Plating of the Femur: Systematic Review of the Literature. Arch. Orthop. Trauma Surg. 2022, 142, 1009–1030. [Google Scholar] [CrossRef] [PubMed]
- Chapman, M.W.; Finkemeier, C.G. Treatment of Supracondylar Nonunions of the Femur with Plate Fixation and Bone Graft. J. Bone Joint Surg. Am. 1999, 81, 1217–1228. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-W.; Weng, L.-H. Treatment of Distal Femoral Nonunion with Internal Fixation, Cortical Allograft Struts, and Autogenous Bone-Grafting. J. Bone Joint Surg. Am. 2003, 85, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Maimaitiyiming, A.; Amat, A.; Rehei, A.; Tusongjiang, M.; Li, C. Treatment of the Femoral Shaft Nonunion with Double Plate Fixation and Bone Grafting: A Case Series of 14 Patients. Injury 2015, 46, 1102–1107. [Google Scholar] [CrossRef]
- Vaishya, R.; Hasija, R. Mega Prosthetic Knee Replacement for Treatment of Resistant Distal Femoral Non-Union. Apollo Med. 2009, 6, 68–70. [Google Scholar] [CrossRef]
- Santolini, E.; West, R.; Giannoudis, P.V. Risk Factors for Long Bone Fracture Non-Union: A Stratification Approach Based on the Level of the Existing Scientific Evidence. Injury 2015, 46, S8–S19. [Google Scholar] [CrossRef] [PubMed]
- Hollensteiner, M.; Sandriesser, S.; Bliven, E.; von Rüden, C.; Augat, P. Biomechanics of Osteoporotic Fracture Fixation. Curr. Osteoporos. Rep. 2019, 17, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Nikolaou, V.S.; Efstathopoulos, N.; Kontakis, G.; Kanakaris, N.K.; Giannoudis, P.V. The Influence of Osteoporosis in Femoral Fracture Healing Time. Injury 2009, 40, 663–668. [Google Scholar] [CrossRef]
- Canton, G.; Giraldi, G.; Dussi, M.; Ratti, C.; Murena, L. Osteoporotic Distal Femur Fractures in the Elderly: Peculiarities and Treatment Strategies. Acta Biomed. 2019, 90, 25–32. [Google Scholar] [CrossRef]
- Meesters, D.; Wijnands, K.; Brink, P.; Poeze, M. Malnutrition and Fracture Healing: Are Specific Deficiencies in Amino Acids Important in Nonunion Development? Nutrients 2018, 10, 1597. [Google Scholar] [CrossRef]
- Manigrasso, M.B.; O’Connor, J.P. Comparison of Fracture Healing Among Different Inbred Mouse Strains. Calcif. Tissue Int. 2008, 82, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, A.; Ritz, U.; Hessmann, M.H.; Schmid, C.; Tresch, A.; Rompe, J.D.; Meurer, A.; Rommens, P.M. Cell viability, osteoblast differentiation, and gene expression are altered in human osteoblasts from hypertrophic fracture non-unions. Bone 2008, 42, 894–906. [Google Scholar] [CrossRef]
- Bartnikowski, M.; Bartnikowski, N.; Woloszyk, A.; Matthys, R.; Glatt, V. Genetic Variation in Mice Affects Closed Femoral Fracture Pattern Outcomes. Injury 2019, 50, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Smetana, J.; Brož, P. National Genome Initiatives in Europe and the United Kingdom in the Era of Whole-Genome Sequencing: A Comprehensive Review. Genes 2022, 13, 556. [Google Scholar] [CrossRef] [PubMed]
- Bertoldo, F.; Cianferotti, L.; Di Monaco, M.; Falchetti, A.; Fassio, A.; Gatti, D.; Gennari, L.; Giannini, S.; Girasole, G.; Gonnelli, S.; et al. Definition, Assessment, and Management of Vitamin D Inadequacy: Suggestions, Recommendations, and Warnings from the Italian Society for Osteoporosis, Mineral Metabolism and Bone Diseases (SIOMMMS). Nutrients 2022, 14, 4148. [Google Scholar] [CrossRef] [PubMed]
- Chinipardaz, Z.; Liu, M.; Graves, D.; Yang, S. Diabetes Impairs Fracture Healing through Disruption of Cilia Formation in Osteoblasts. Bone 2021, 153, 116176. [Google Scholar] [CrossRef]
- Tanios, M.; Brickman, B.; Cage, E.; Abbas, K.; Smith, C.; Atallah, M.; Baroi, S.; Lecka-Czernik, B. Diabetes and Impaired Fracture Healing: A Narrative Review of Recent Literature. Curr. Osteoporos. Rep. 2022, 20, 229–239. [Google Scholar] [CrossRef]
- Massari, L.; Benazzo, F.; Falez, F.; Cadossi, R.; Perugia, D.; Pietrogrande, L.; Aloj, D.C.; Capone, A.; D’Arienzo, M.; Cadossi, M.; et al. Can Clinical and Surgical Parameters Be Combined to Predict How Long It Will Take a Tibia Fracture to Heal? A Prospective Multicentre Observational Study: The FRACTING Study. BioMed Res. Int. 2018, 2018, 1809091. [Google Scholar] [CrossRef]
- Basile, G.; Accetta, R.; Marinelli, S.; D’Ambrosi, R.; Petrucci, Q.A.; Giorgetti, A.; Nuara, A.; Zaami, S.; Fozzato, S. Traumatology: Adoption of the Sm@rtEven Application for the Remote Evaluation of Patients and Possible Medico-Legal Implications. JCM 2022, 11, 3644. [Google Scholar] [CrossRef]

| Patients with Femoral PSA (n = 16) | |||
|---|---|---|---|
| Mean Age (years) | 50 (12; 82) | Side | |
| Sex | Left | 9 | |
| Right | 7 | ||
| Male | 10 | Open fractures (n) | 1 |
| Female | 6 | Fracture localization (n) | |
| High-energy trauma (n) | 16 | Proximal third | 8 |
| First implant rupture (n) | 7 | Middle third | 4 |
| Initial treatment (n) | Distal third | 4 | |
| Intramedullary nail | 8 | PSA treatment (n) | |
| Plate and screw | 8 | Plate + homologous bone graft | 7 |
| Smokers (n) | 3 | Plate + cortico-cancellous bone graft | 3 |
| Plate + screw | 8 | Intramedullary nail | 2 |
| Follow-up (months) | 15.4 (range 6–38) | Prosthetic implantation | 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basile, G.; Fozzato, S.; Petrucci, Q.A.; Gallina, M.; Bianco Prevot, L.; Accetta, R.; Zaami, S. Treatment of Femoral Shaft Pseudarthrosis, Case Series and Medico-Legal Implications. J. Clin. Med. 2022, 11, 7407. https://doi.org/10.3390/jcm11247407
Basile G, Fozzato S, Petrucci QA, Gallina M, Bianco Prevot L, Accetta R, Zaami S. Treatment of Femoral Shaft Pseudarthrosis, Case Series and Medico-Legal Implications. Journal of Clinical Medicine. 2022; 11(24):7407. https://doi.org/10.3390/jcm11247407
Chicago/Turabian StyleBasile, Giuseppe, Stefania Fozzato, Quirino Alessandro Petrucci, Mario Gallina, Luca Bianco Prevot, Riccardo Accetta, and Simona Zaami. 2022. "Treatment of Femoral Shaft Pseudarthrosis, Case Series and Medico-Legal Implications" Journal of Clinical Medicine 11, no. 24: 7407. https://doi.org/10.3390/jcm11247407
APA StyleBasile, G., Fozzato, S., Petrucci, Q. A., Gallina, M., Bianco Prevot, L., Accetta, R., & Zaami, S. (2022). Treatment of Femoral Shaft Pseudarthrosis, Case Series and Medico-Legal Implications. Journal of Clinical Medicine, 11(24), 7407. https://doi.org/10.3390/jcm11247407








