Local Resection in Choroidal Melanoma: A Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
4.1. TRANSSCLERAL RESECTION (AB EXTERNO)
4.1.1. Indications and Contraindications
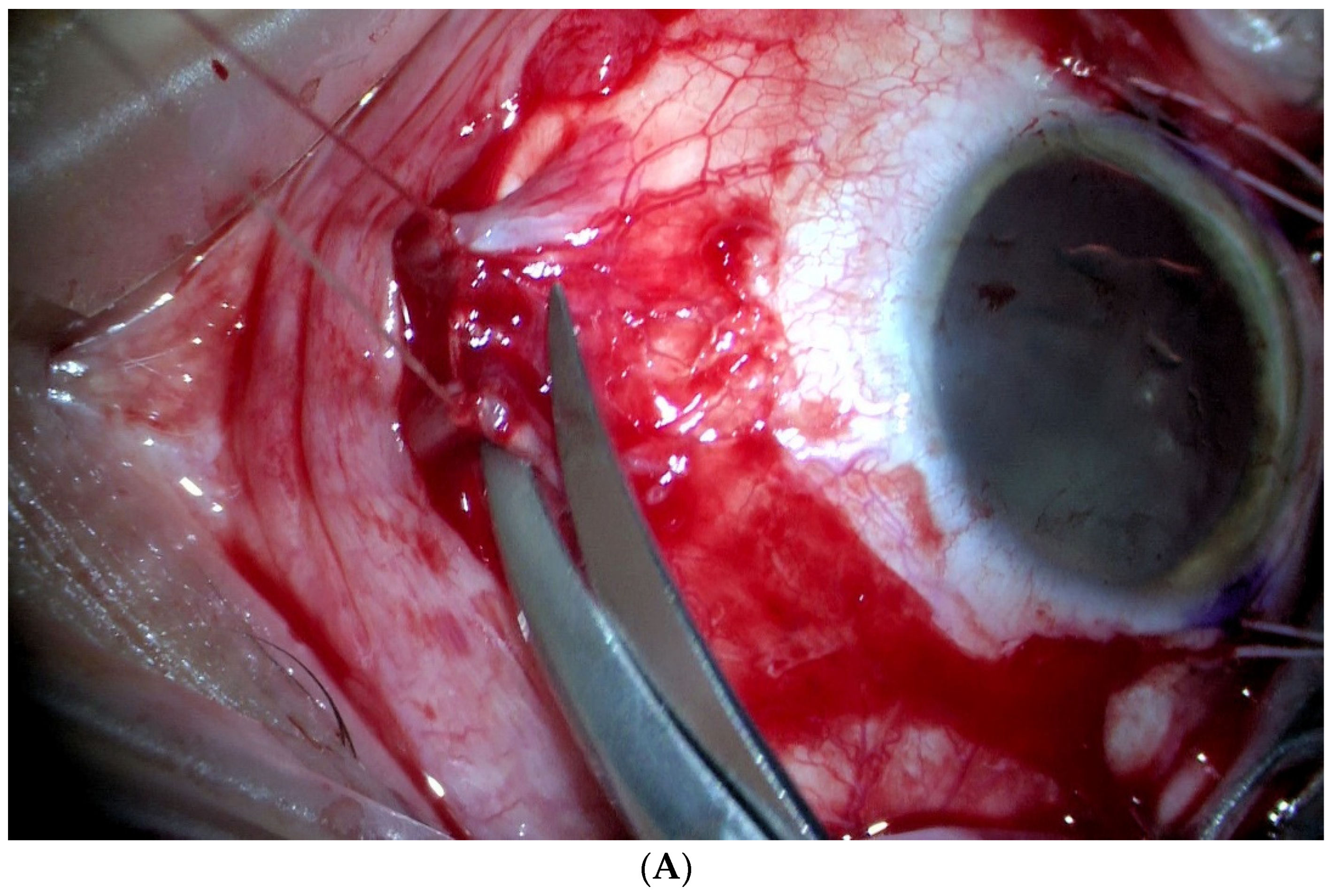
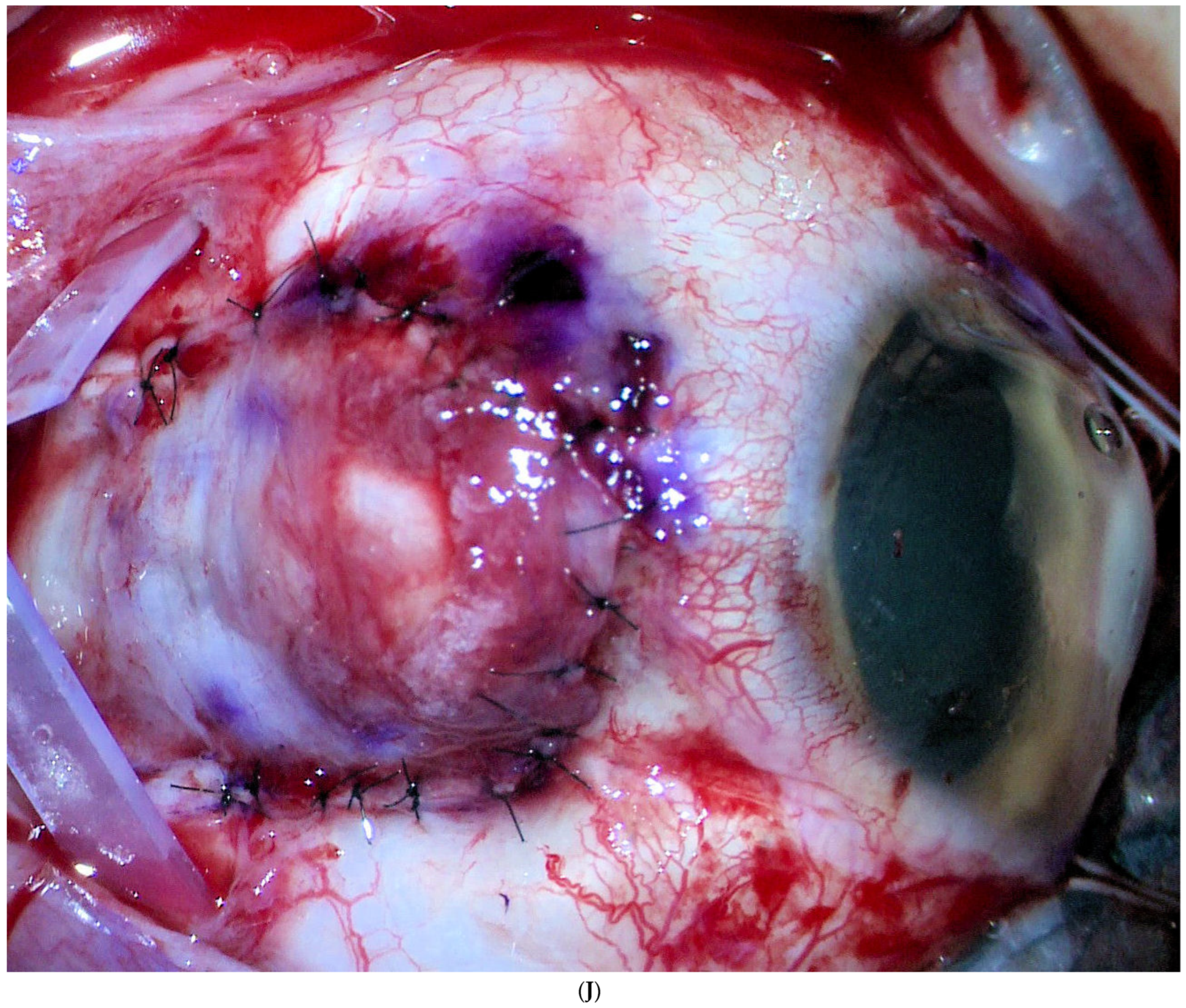
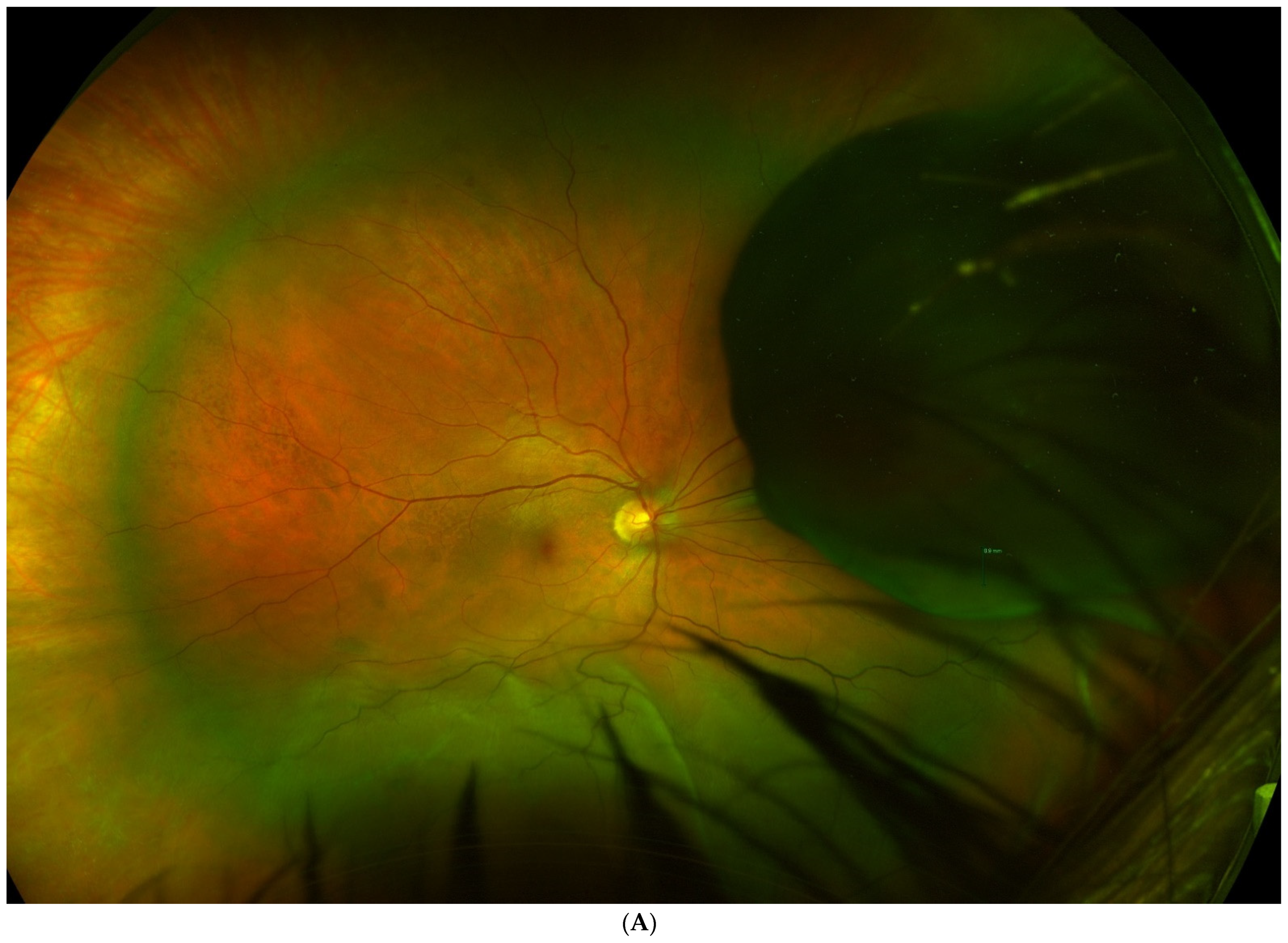
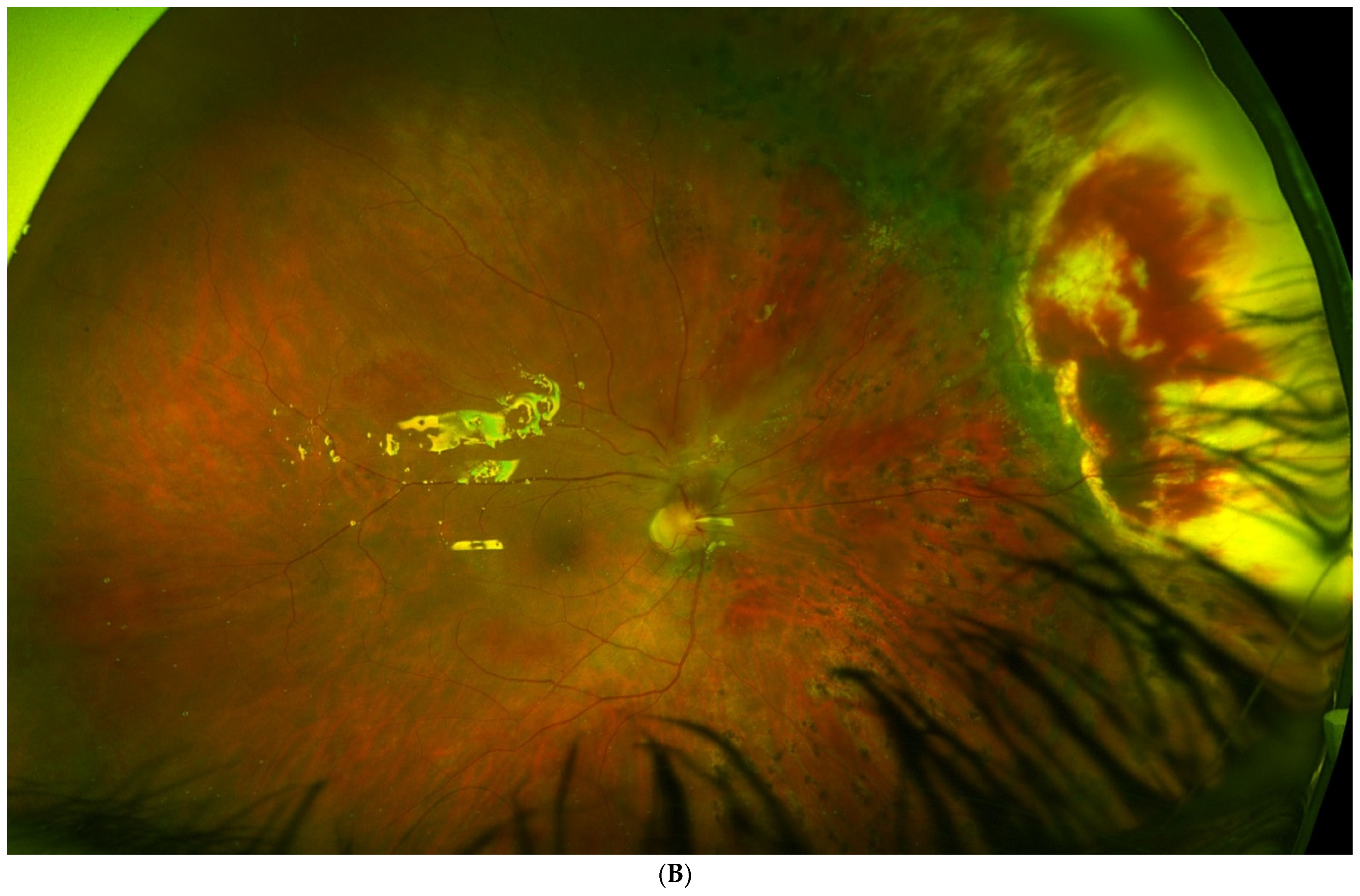
4.1.2. Surgical Techniques
4.1.3. Metastasis and Death
4.1.4. Local Tumour Control
4.1.5. Enucleation
4.1.6. Complications and Visual Outcomes
4.1.7. Comparison between Treatments: Enucleation and Brachytherapy (Table 3)
4.1.8. Conclusions
4.2. ENDORESECTION (OR RESECTION AB INTERNO)
4.2.1. Indications and Contraindications
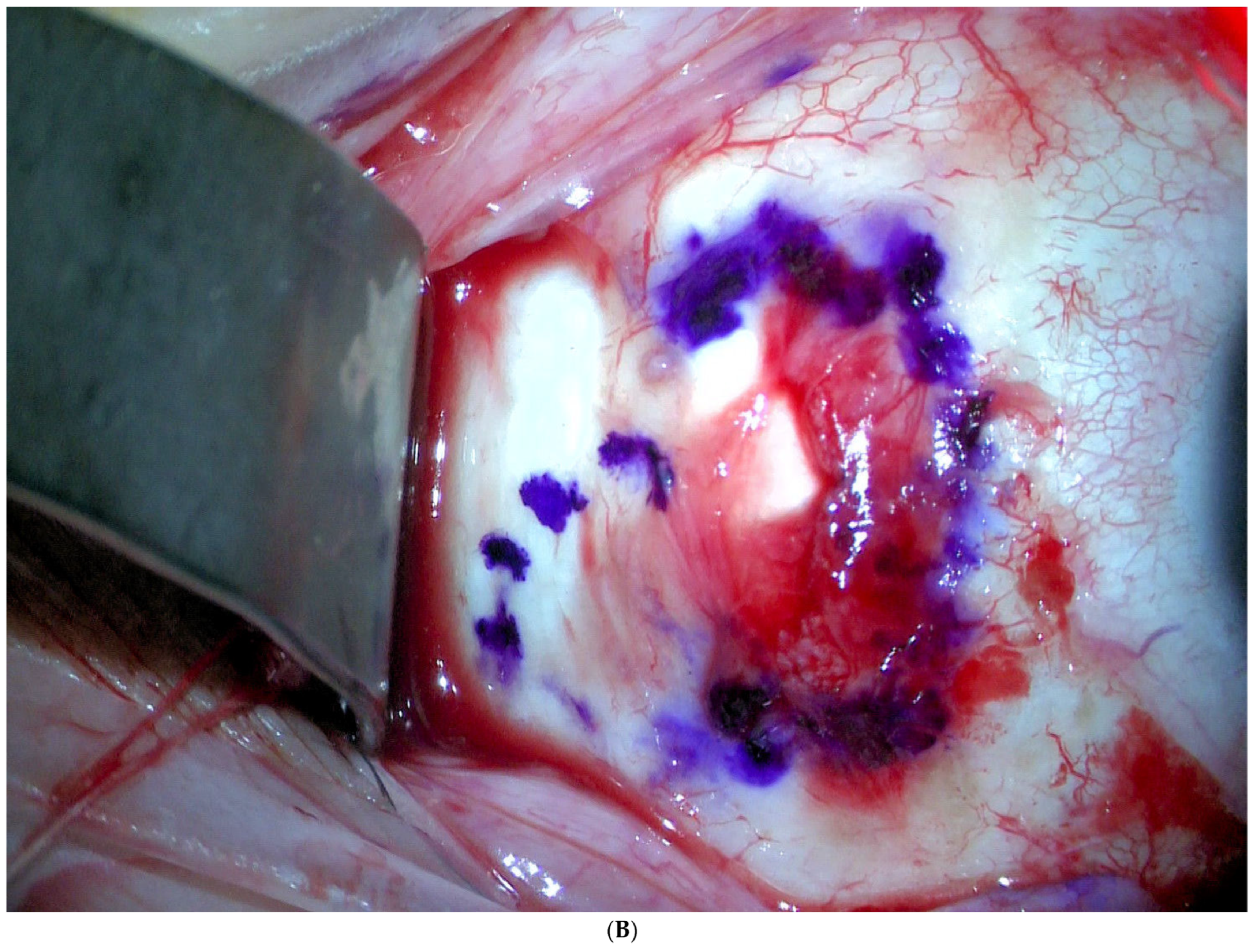
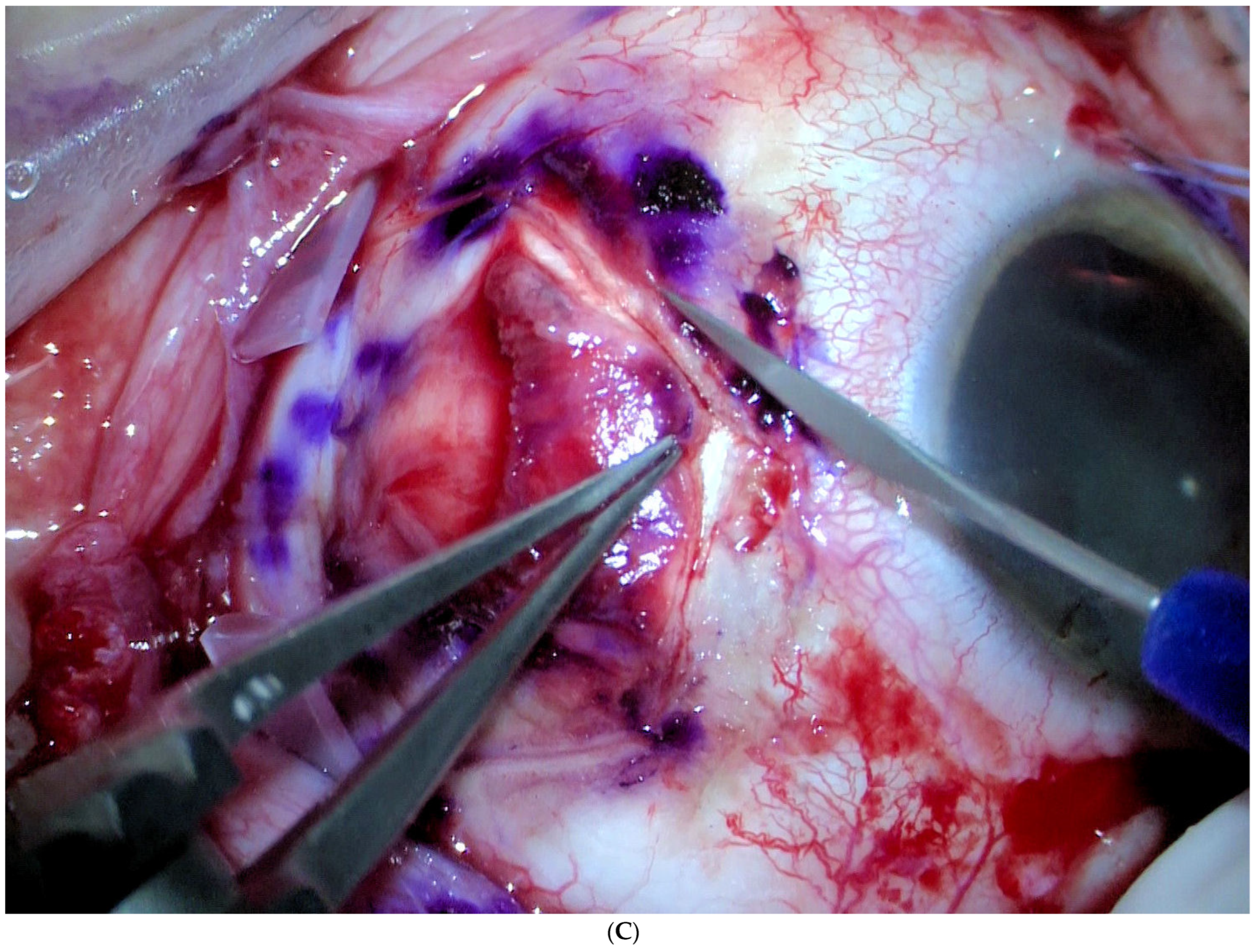
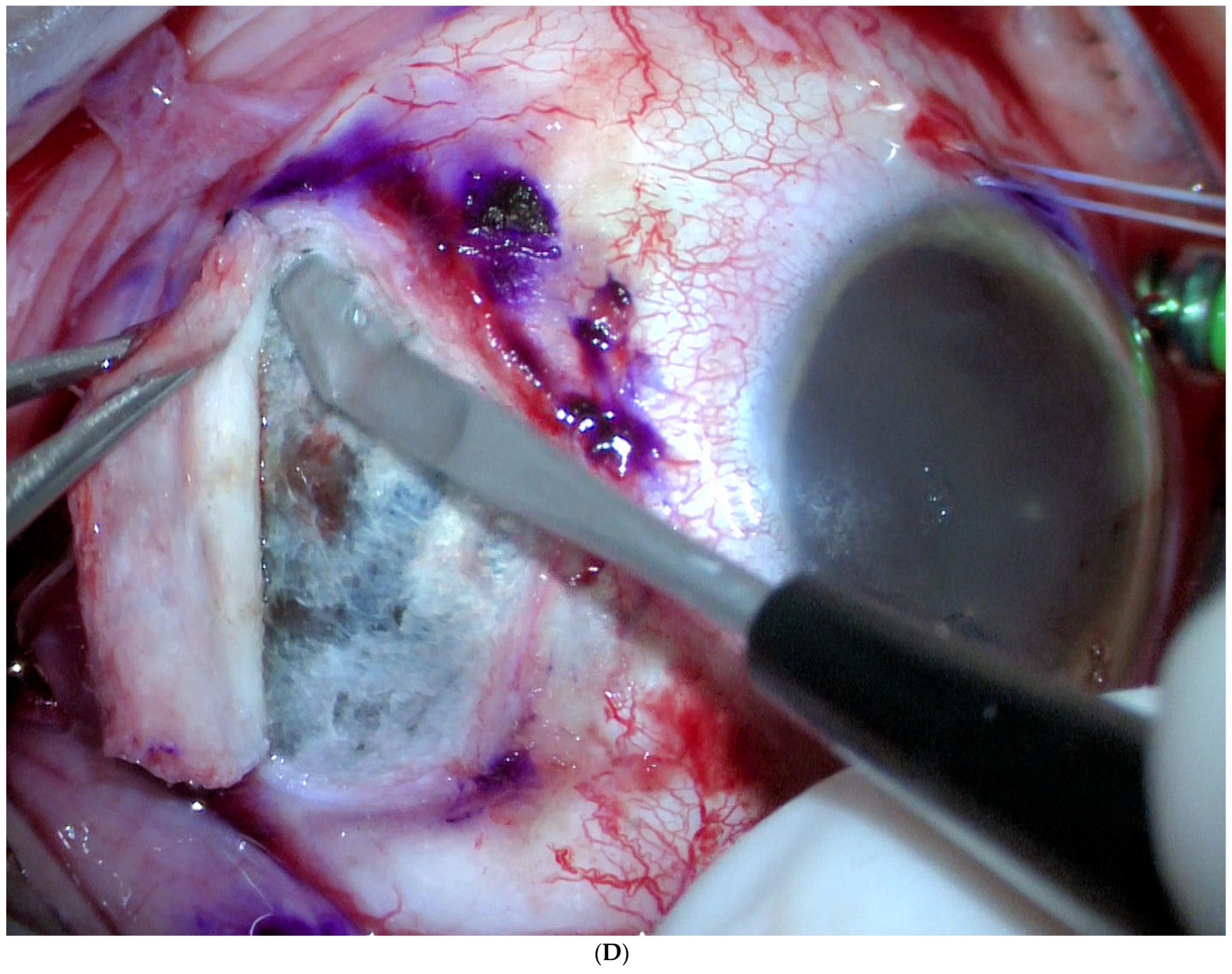
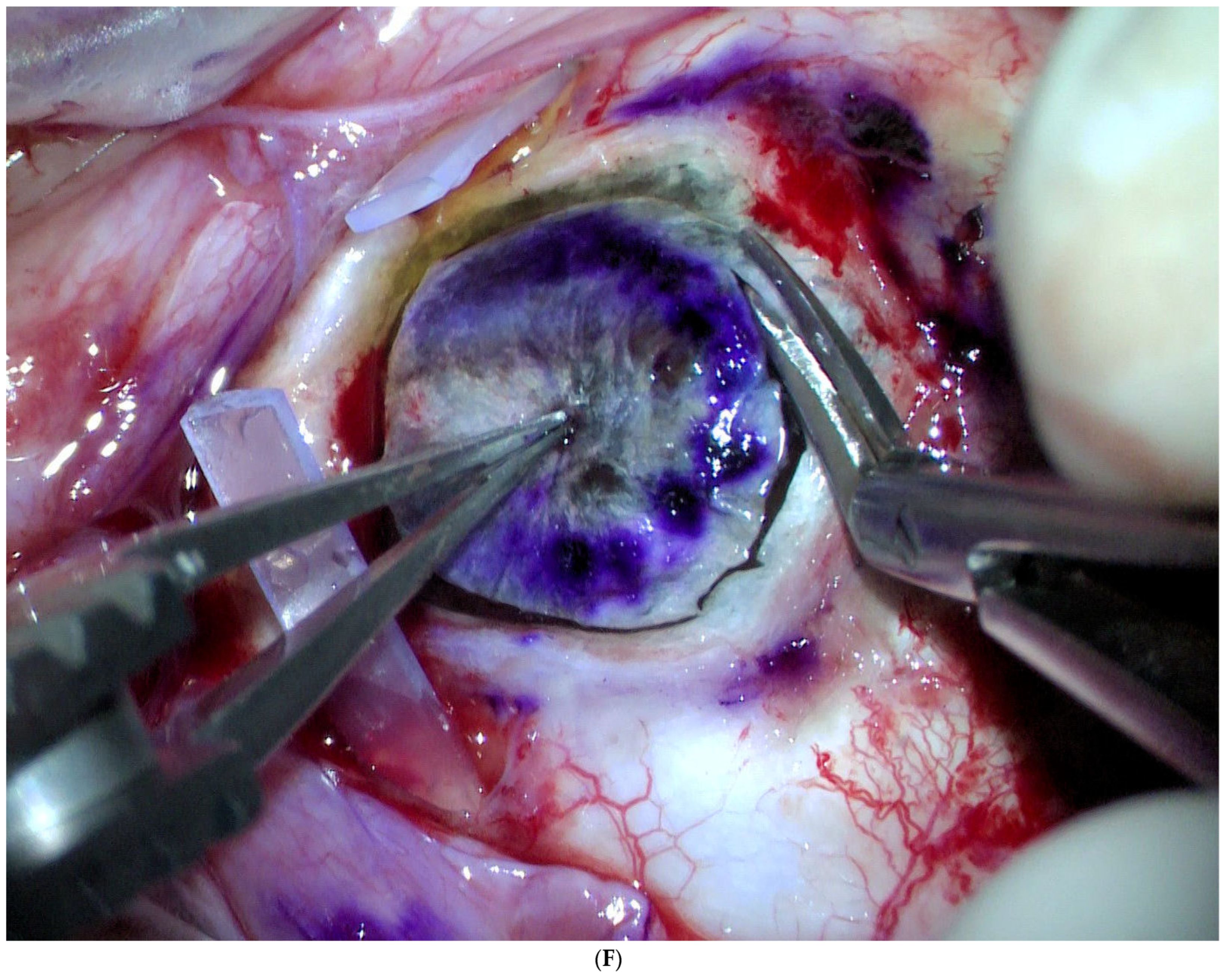
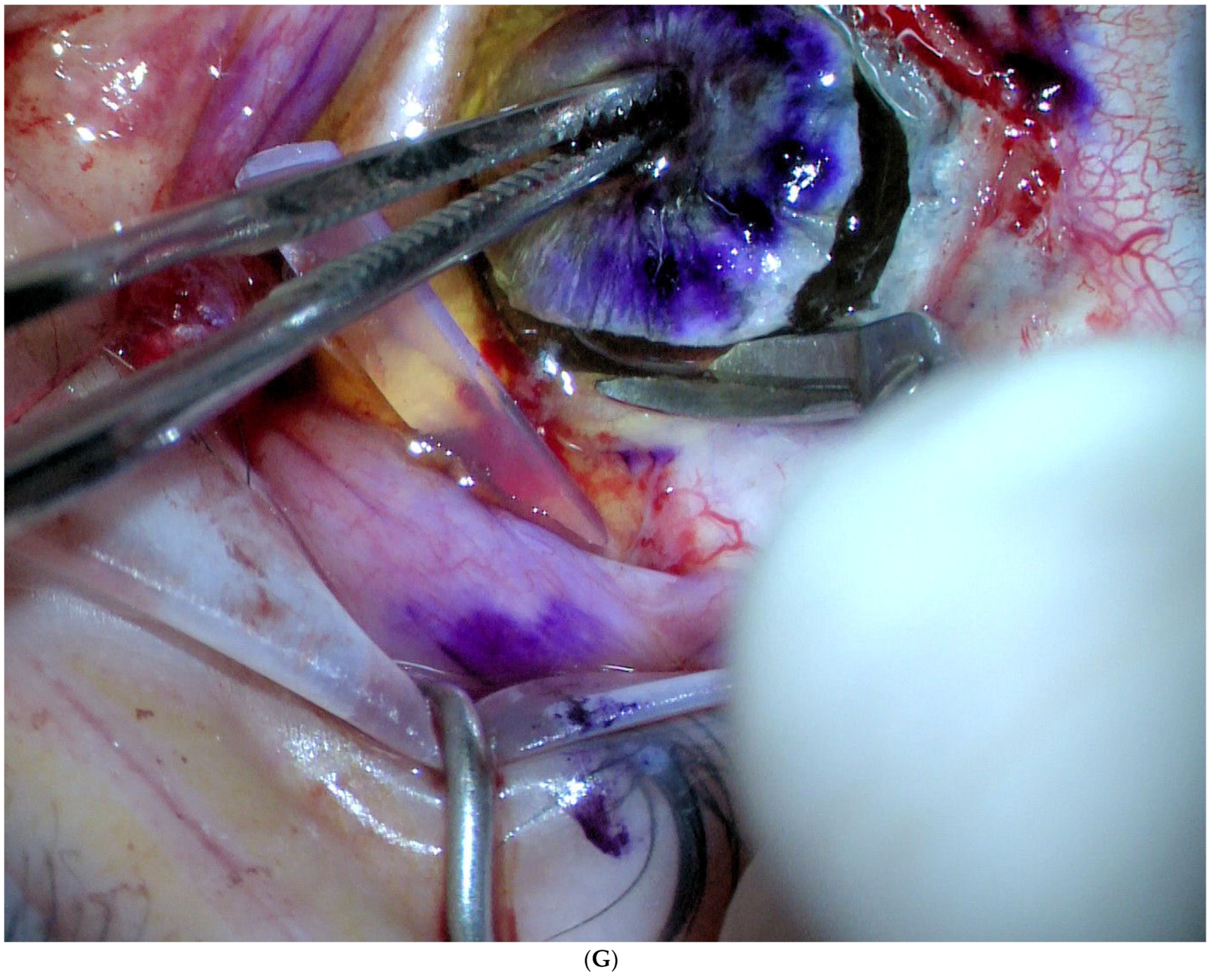
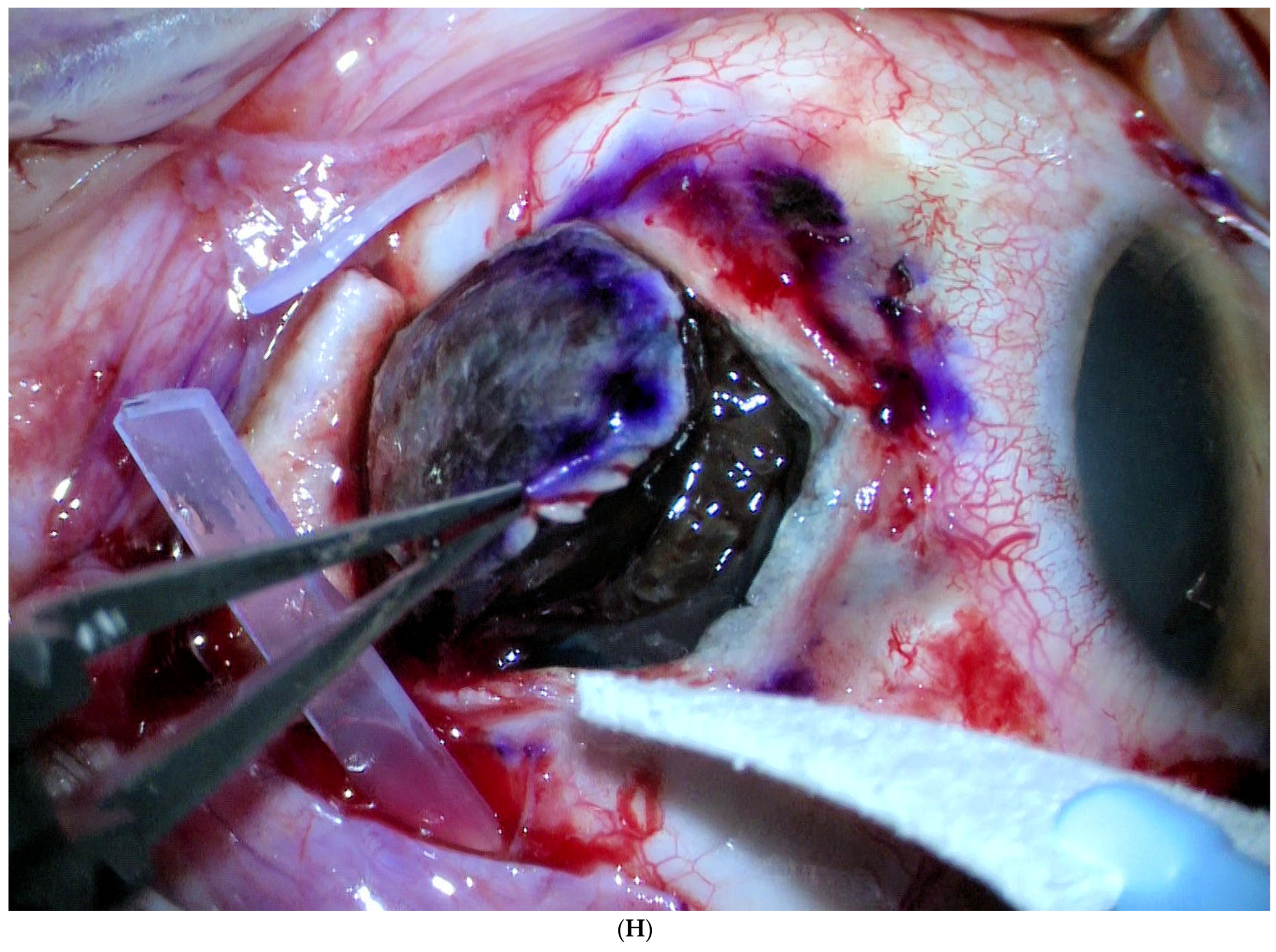
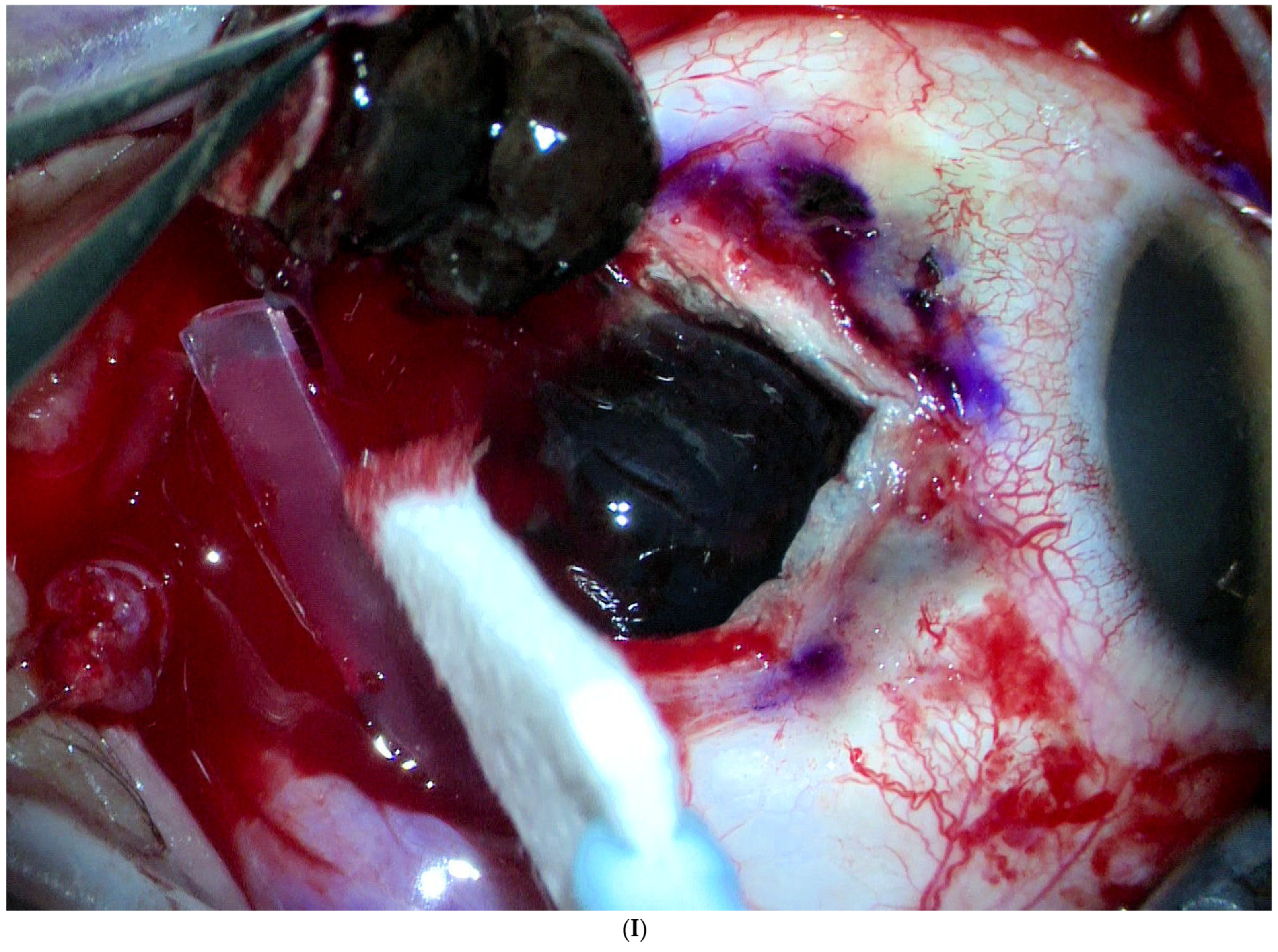
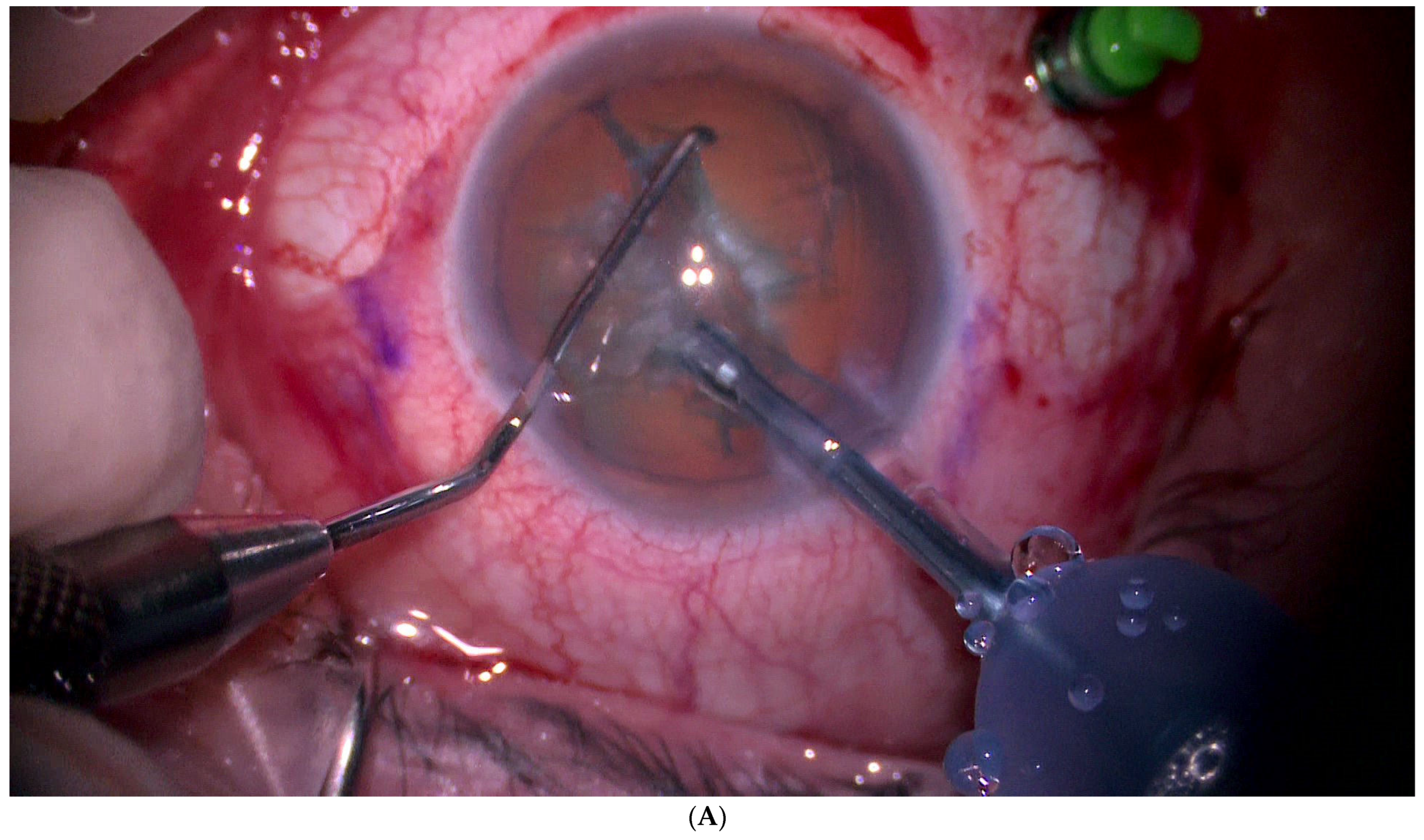
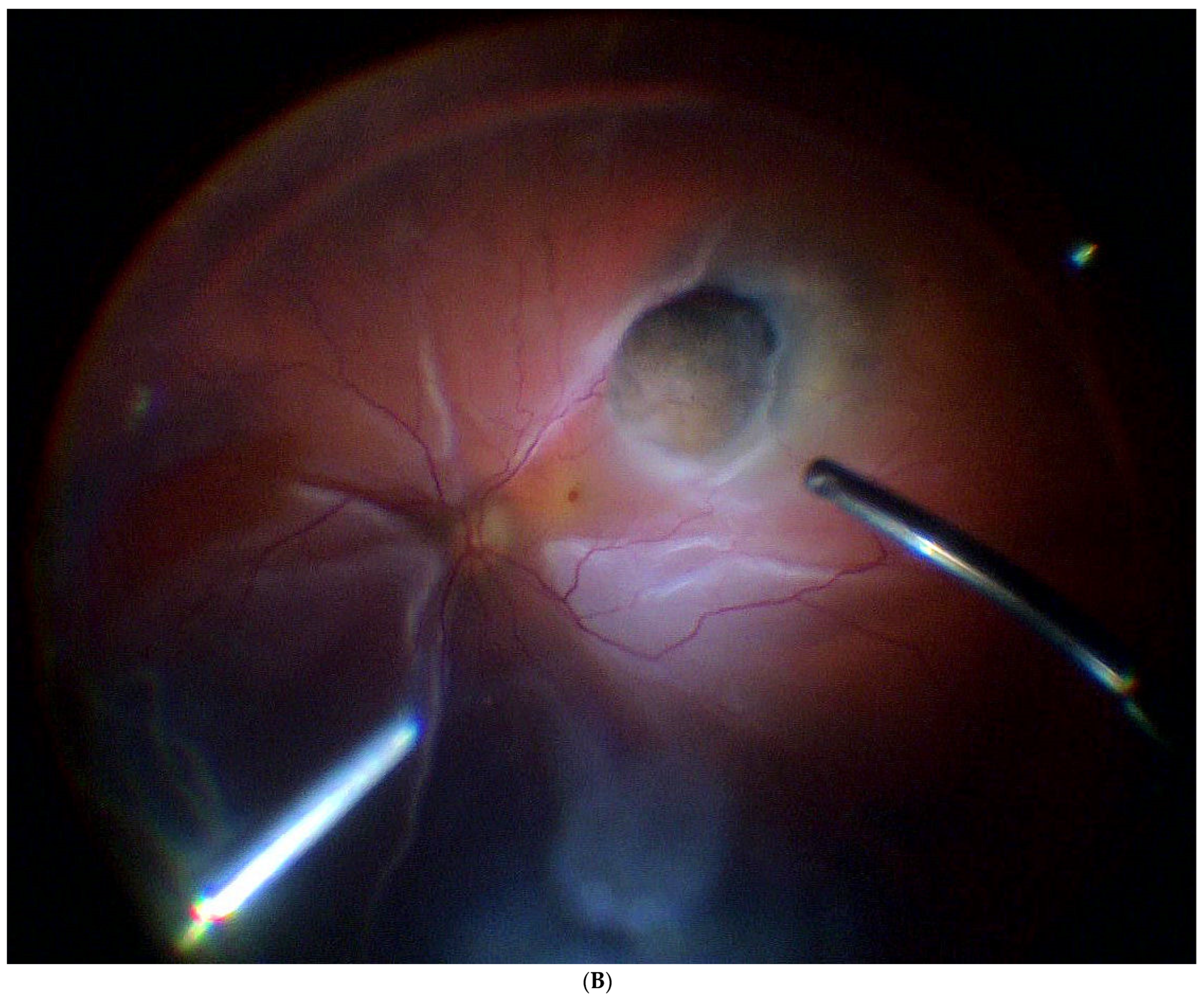
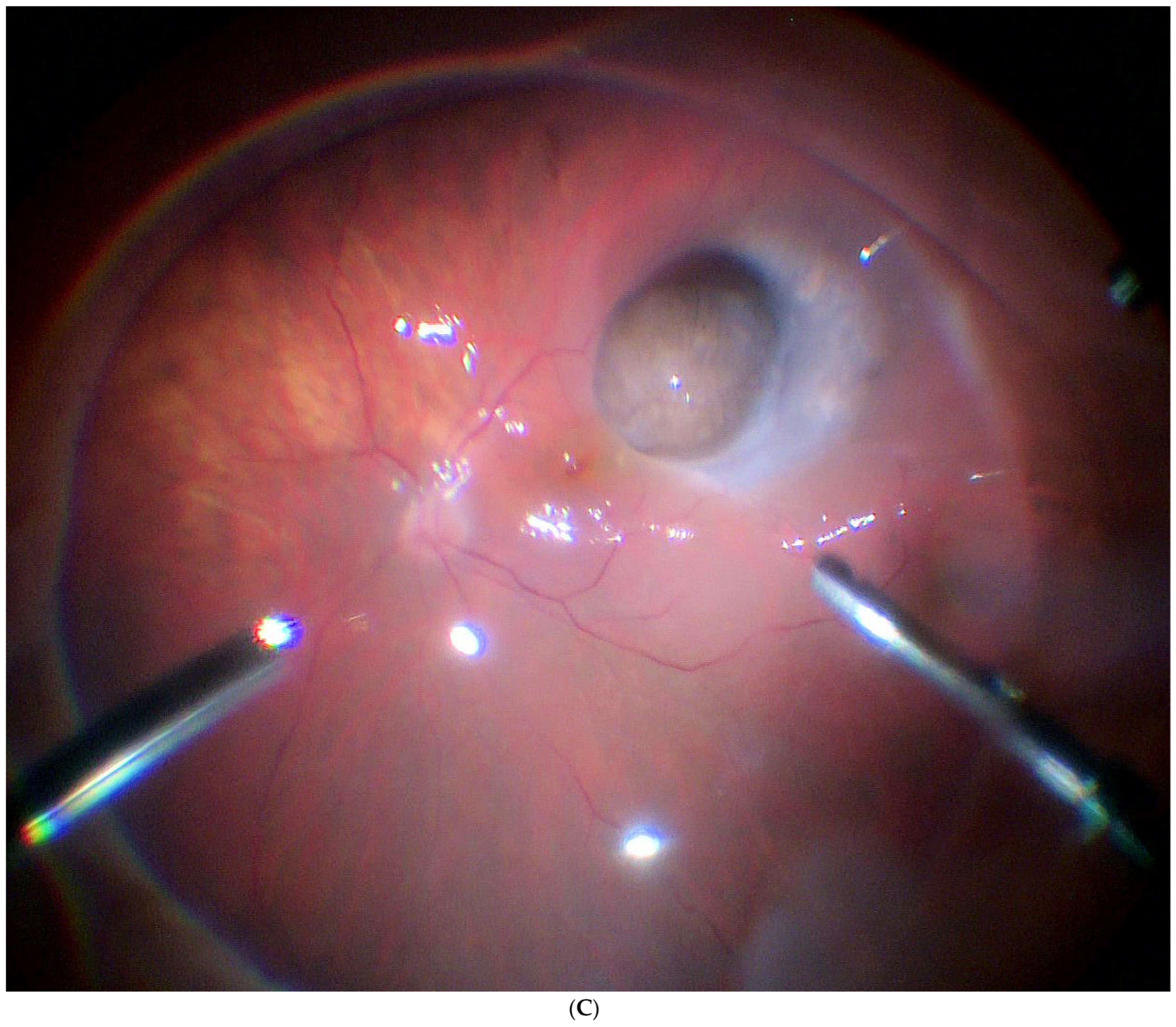
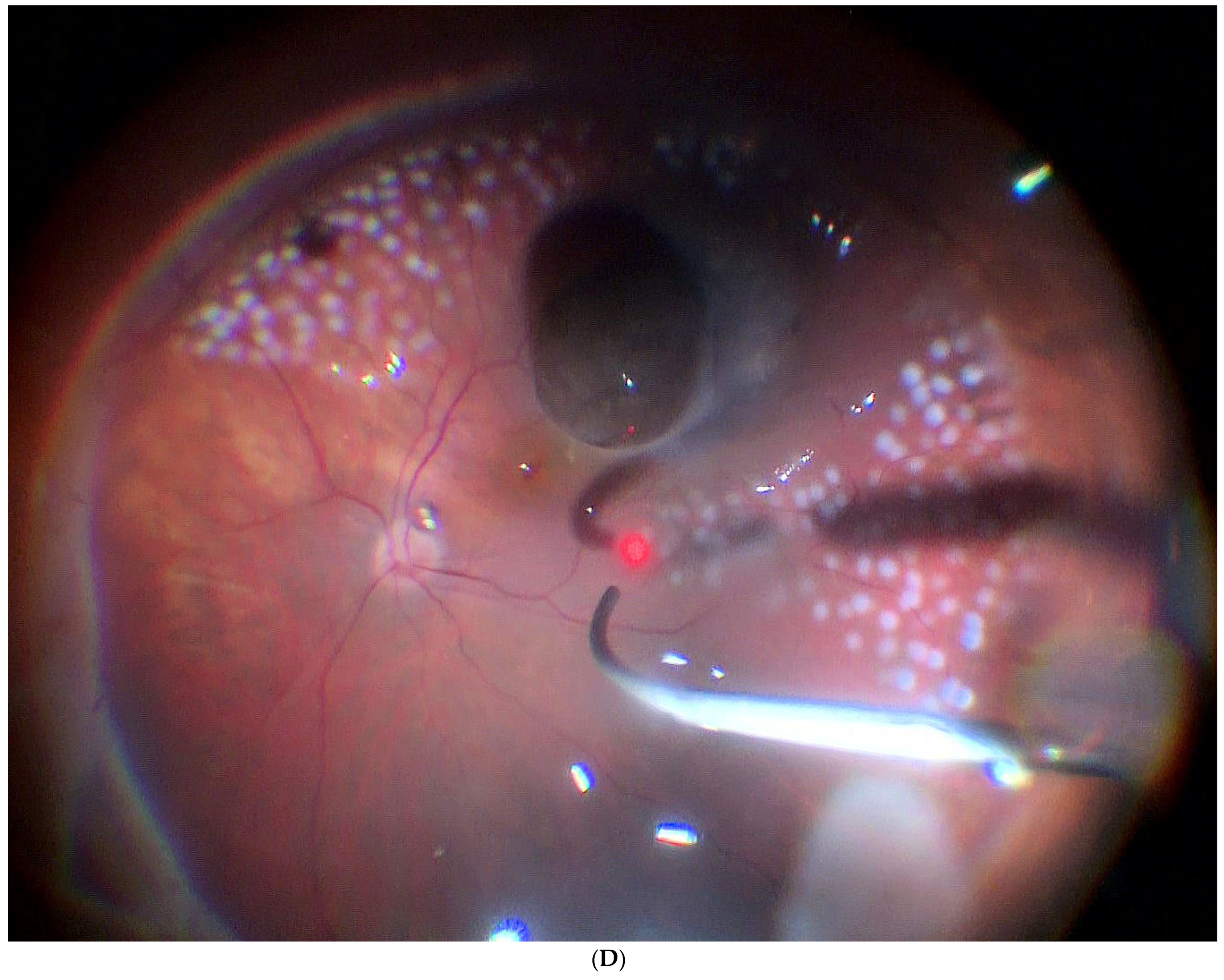
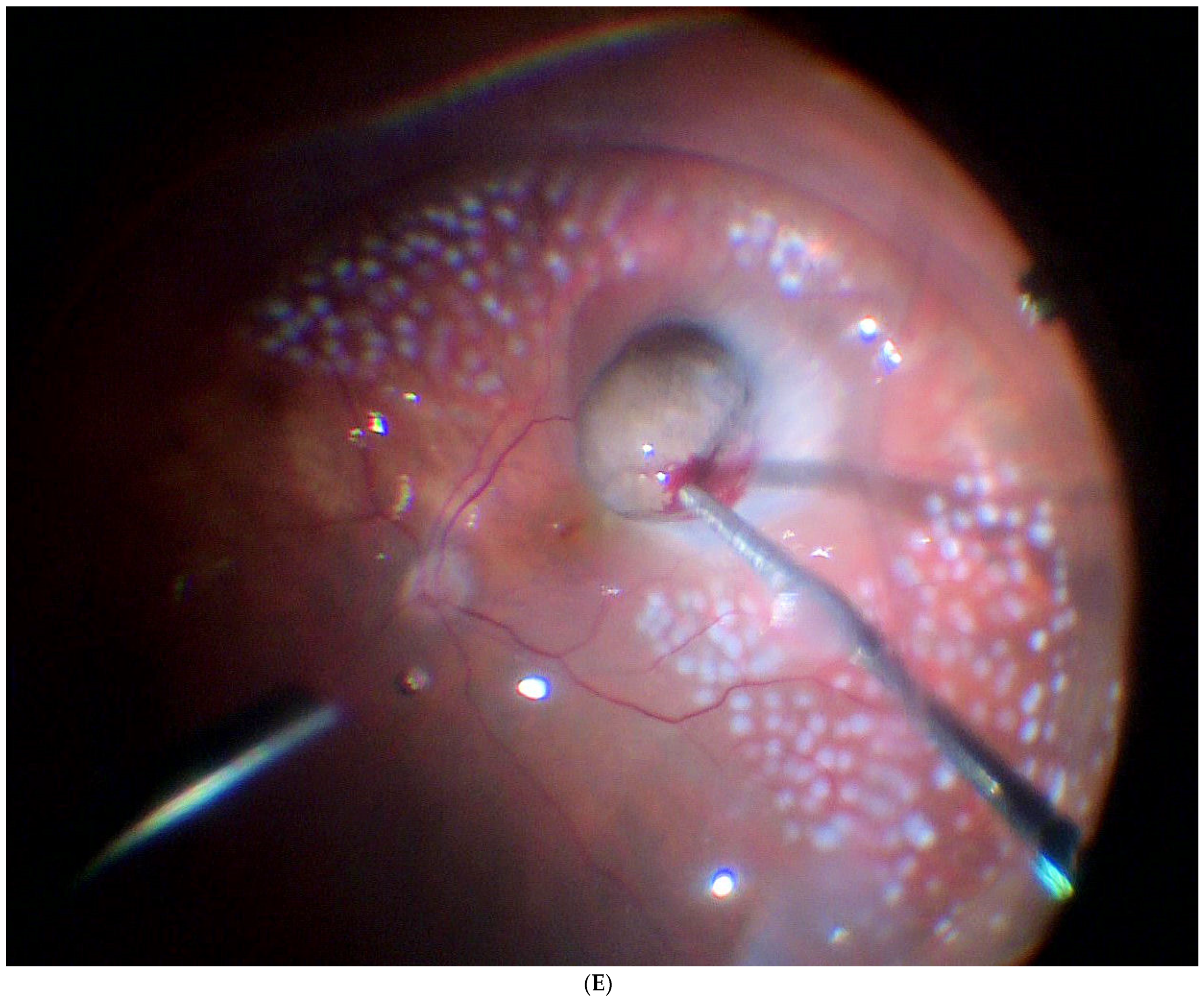
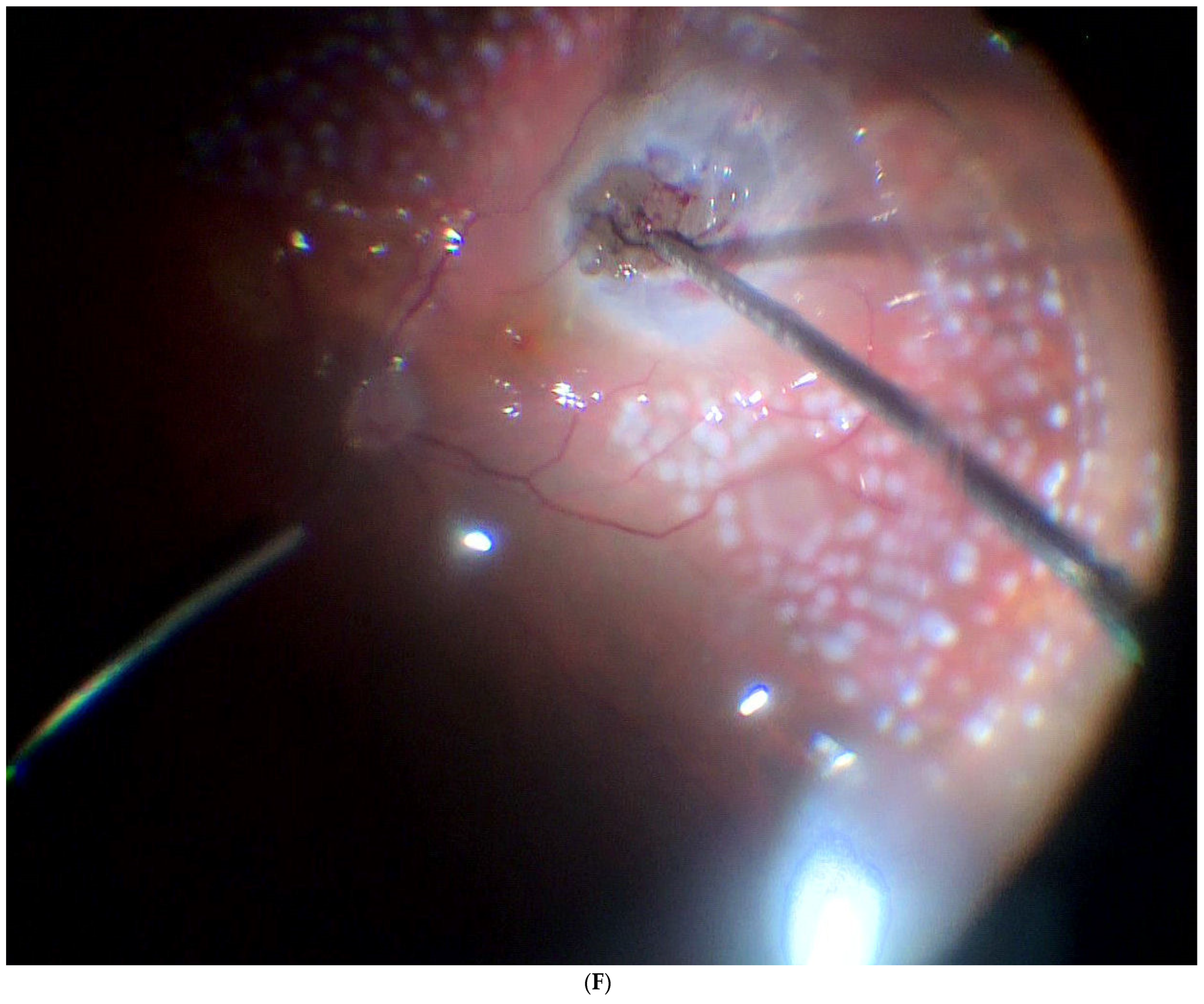
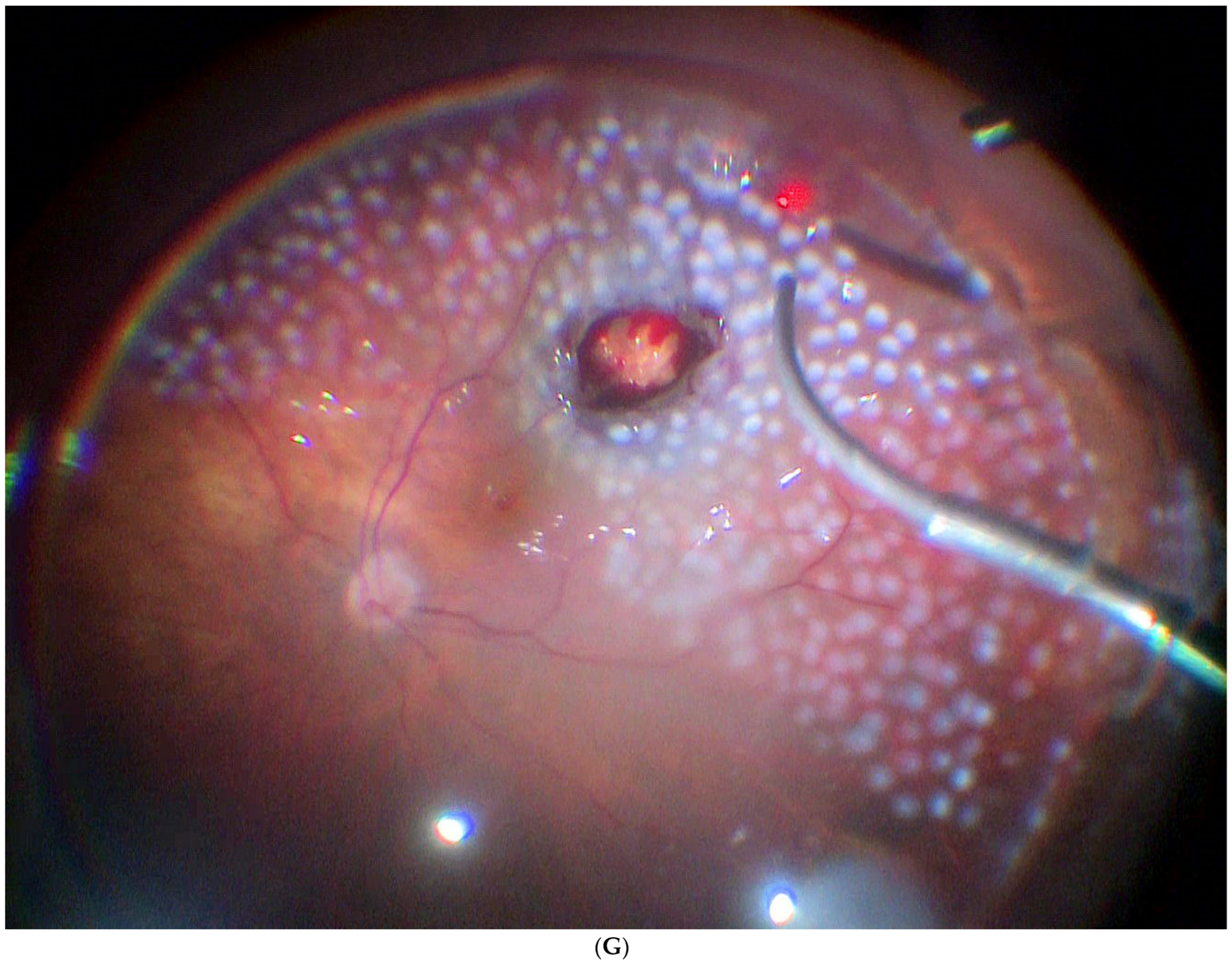
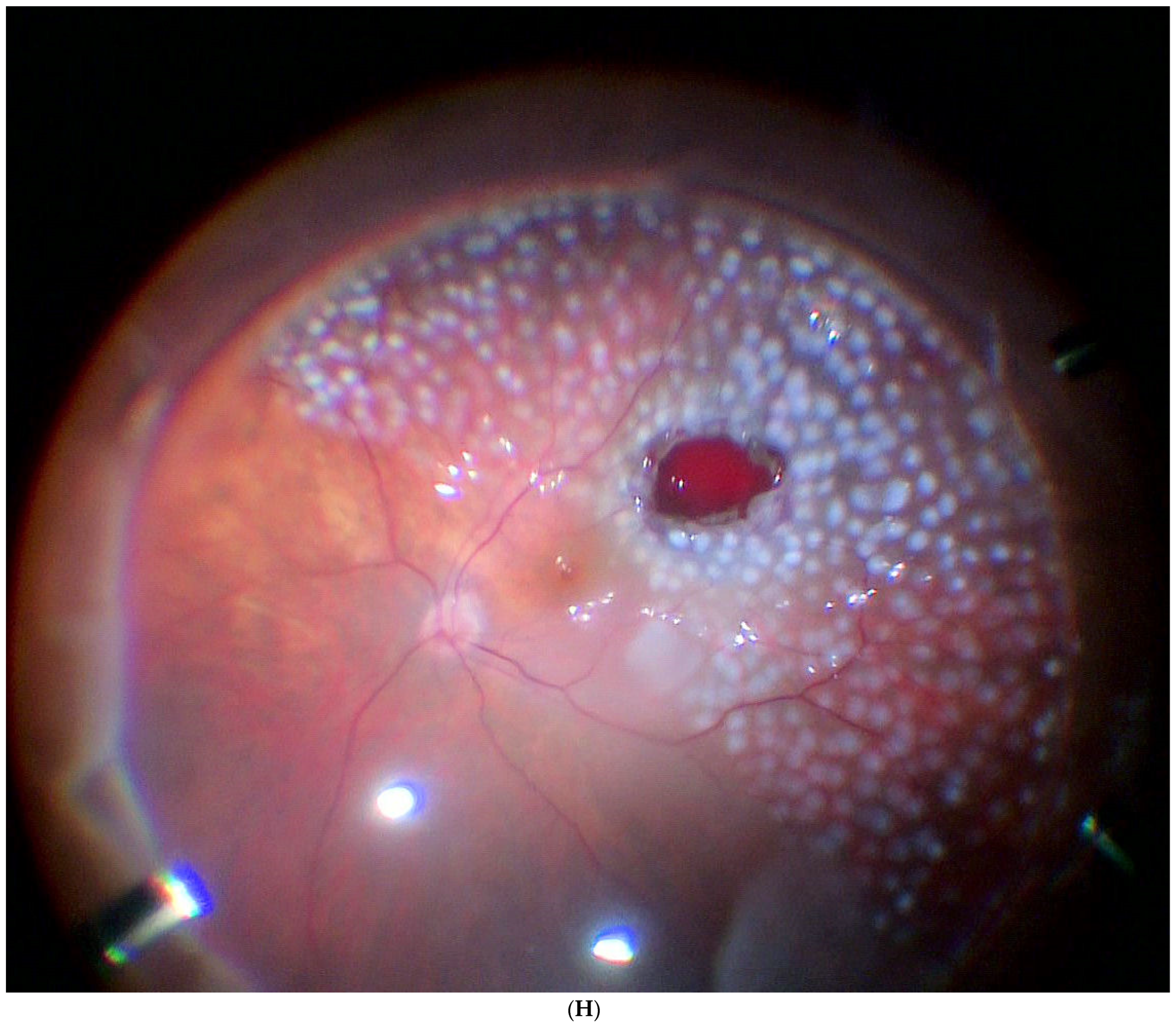
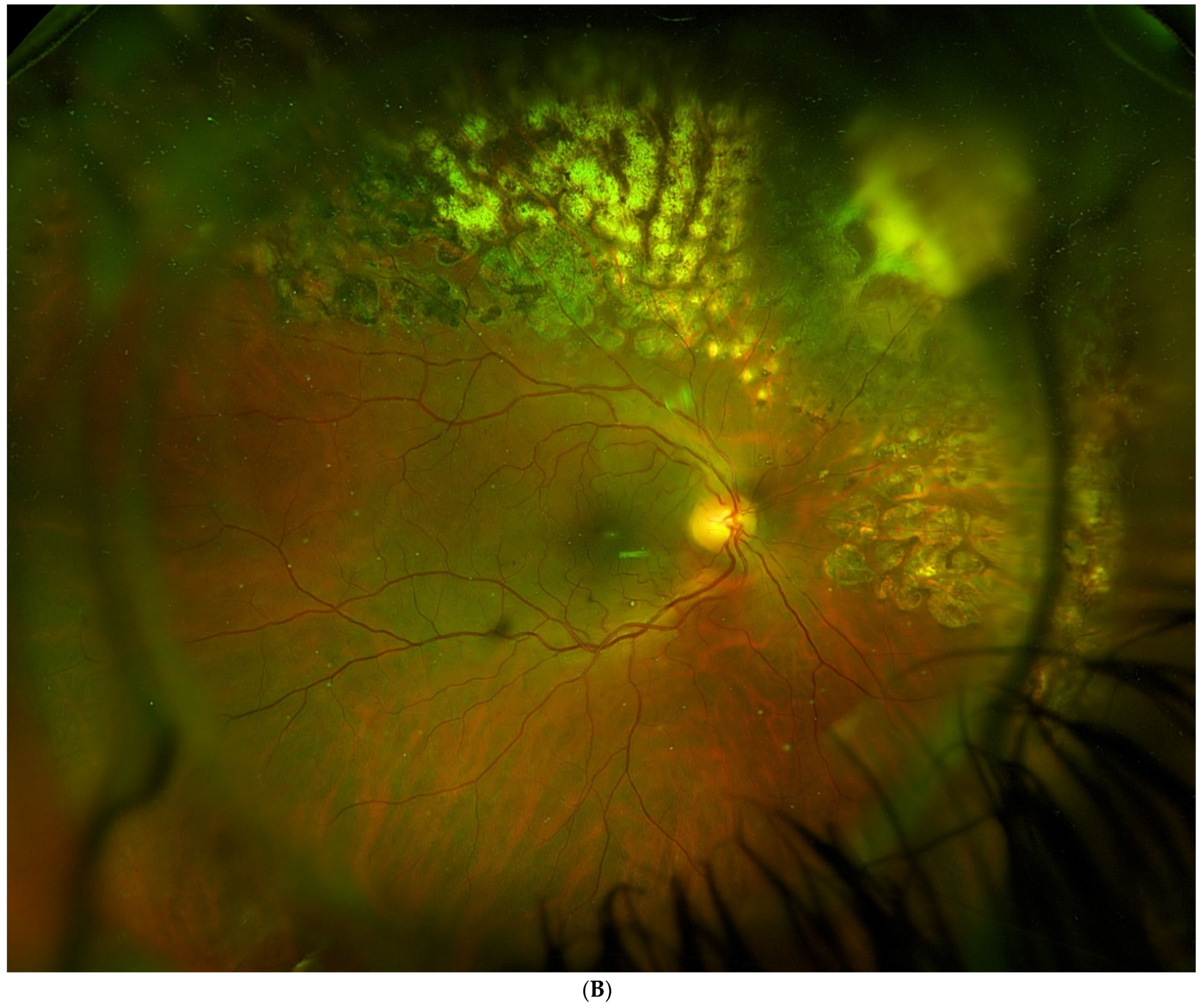
4.2.2. Surgical Technique
4.2.3. Metastasis and Death
4.2.4. Local Tumour Control
4.2.5. Complications and Functional Outcomes
4.2.6. Comparison between Treatments: Brachytherapy (Table 4)
4.2.7. Conclusions
5. Conclusions
- Choroidal tumour resection is an alternative to brachytherapy in selected cases. The available data suggest that this approach may offer better visual results and eye sparing without compromising local tumour control and survival.
- Resection techniques for choroidal tumours are based on modern vitreoretinal surgical techniques, which allow for the treatment of more challenging cases.
- The main limitations to surgical resection of these tumours are the risk of severe complications, which may include retinal detachment, proliferative vitreoretinopathy, severe intraoperative haemorrhage, air embolism, and local tumour recurrence at the resection edge.
- Surgical resection of uveal melanomas should be limited to centres with substantial experience in the management of intraocular tumours.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singh, M.; Durairaj, P.; Yeung, J. Uveal Melanoma: A Review of the Literature. Oncol. Ther. 2018, 6, 87–104. [Google Scholar] [CrossRef] [PubMed]
- Shields, J.A.; Shields, C.L. Management of Posterior Uveal Melanoma: Past, Present, and Future. Ophthalmology 2015, 122, 414–428. [Google Scholar] [CrossRef]
- Kapoor, A.; Beniwal, V.; Beniwal, S.; Mathur, H.; Kumar, H.S. Management of uveal tract melanoma: A comprehensive review. J. Egypt. Natl. Cancer Inst. 2016, 28, 65–72. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gunduz, K.; Bechrakis, N. Exoresection and endoresection for uveal melanoma. Middle East Afr. J. Ophthalmol. 2010, 17, 210. [Google Scholar] [CrossRef]
- Damato, B.; Groenewald, C. Uveal Malignant Melanoma: Management Options—Resection Techniques. In Clinical Ophthalmic Oncology; Elsevier Inc.: Amsterdam, The Netherlands, 2007; pp. 259–266. [Google Scholar] [CrossRef]
- Rospond-Kubiak, I.; Damato, B. The surgical approach to the management of anterior uveal melanomas. Eye 2014, 28, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Peyman, G.A.; Juarez, C.P.; Diamond, J.G.; Raichand, M. Ten years experience with eye wall resection for uveal malignant melanomas. Ophthalmology 1984, 91, 1720–1725. [Google Scholar] [CrossRef] [PubMed]
- Foulds, W.S.; Damato, B.E. Alternatives to Enucleation in the Management of Choroidal Melanoma. Aust. N. Z. J. Ophthalmol. 1986, 14, 19–27. [Google Scholar] [CrossRef]
- Shields, J.A.; Shields, C.L.; Shah, P.; Sivalingam, V. Partial lamellar sclerouvectomy for ciliary body and choroidal tumors. Ophthalmology 1991, 98, 971–983. [Google Scholar] [CrossRef]
- Damato, B.E.; Paul, J.; Foulds, W.S. Risk factors for metastatic uveal melanoma after trans-scleral local resection. Br. J. Ophthalmol. 1996, 80, 109–116. [Google Scholar] [CrossRef]
- Puusaari, I.; Damato, B.; Kivelä, T. Transscleral local resection versus iodine brachytherapy for uveal melanomas that are large because of tumour height. Graefe’s Arch. Clin. Exp. Ophthalmol. 2006, 245, 522–533. [Google Scholar] [CrossRef]
- Bechrakis, N.E.; Petousis, V.; Willerding, G.; Krause, L.; Wachtlin, J.; Stroux, A.; Foerster, M.H. Ten-year results of transscleral resection of large uveal melanomas: Local tumour control and metastatic rate. Br. J. Ophthalmol. 2010, 94, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Foulds, W.S.; Damato, B.E.; Burton, R.L. Local resection versus enucleation in the management of choroidal melanoma. Eye 1987, 1, 676–679. [Google Scholar] [CrossRef] [PubMed]
- Augsburger, J.J.; Lauritzen, K.; Gamel, J.W.; DeBrakeleer, D.J.; Lowry, J.C.; Eisenman, R. Matched group study of surgical resection versus cobalt-60 plaque radiotherapy for primary choroidal or ciliary body melanoma. Ophthalmic Surg. 1990, 21, 682–688. [Google Scholar] [CrossRef] [PubMed]
- Bechrakis, N.E.; Bornfeld, N.; Zöller, I.; Foerster, M.H. Iodine 125 plaque brachytherapy versus transscleral tumor resection in the treatment of large uveal melanomas. Ophthalmology 2002, 109, 1855–1861. [Google Scholar] [CrossRef] [PubMed]
- Kivelä, T.; Puusaari, I.; Damato, B. Transscleral resection versus iodine brachytherapy for choroidal malignant melanomas 6 millimeters or more in thickness: A matched case-control study. Ophthalmology 2003, 110, 2235–2244. [Google Scholar] [CrossRef]
- Caminal, J.M.; Padrón-Pérez, N.; Arias, L.; Masuet-Aumatell, C.; Gutiérrez, C.; Piulats, J.M.; Pera, J.; Català, J.; Rubio, M.J.; Arruga, J. Transscleral resection without hypotensive anaesthesia vs. iodine-125 plaque brachytherapy in the treatment of choroidal melanoma. Eye 2016, 30, 833–842. [Google Scholar] [CrossRef]
- Kertes, P.J.; Johnson, J.C.; Peyman, G.A. Internal resection of posterior uveal melanomas. Br. J. Ophthalmol. 1998, 82, 1147–1153. [Google Scholar] [CrossRef] [PubMed]
- Damato, B.; Groenewald, C.; McGalliard, J.; Wong, D. Endoresection of choroidal melanoma. Br. J. Ophthalmol. 1998, 82, 213–218. [Google Scholar] [CrossRef]
- García-Arumí, J.; Sararols, L.; Martinez, V.; Corcostegui, B. Vitreoretinal surgery and endoresection in high posterior choroidal melanomas. Retina 2001, 21, 445–452. [Google Scholar] [CrossRef]
- Bechrakis, N.E.; Foerster, M.H. Neoadjuvant proton beam radiotherapy combined with subsequent endoresection of choroidal melanomas. Int. Ophthalmol. Clin. 2006, 46, 95–107. [Google Scholar] [CrossRef]
- Karkhaneh, R.; Chams, H.; Amoli, F.A.; Riazi-Esfahani, M.; Ahmadabadi, M.N.; Mansouri, M.R.; Nouri, K.; Karkhaneh, A. Long-term surgical outcome of posterior choroidal melanoma treated by endoresection. Retina 2007, 27, 908–914. [Google Scholar] [CrossRef] [PubMed]
- García-Arumí, J.; Zapata, M.A.; Balaguer, O.; Fonollosa, A.; Boixadera, A.; Martinez-Castillo, V. Endoresection in high posterior choroidal melanomas: Long-term outcome. Br. J. Ophthalmol. 2008, 92, 1040–1045. [Google Scholar] [CrossRef] [PubMed]
- Konstantinidis, L.; Groenewald, C.; Coupland, S.E.; Damato, B. Long-term outcome of primary endoresection of choroidal melanoma. Br. J. Ophthalmol. 2014, 98, 82–85. [Google Scholar] [CrossRef] [PubMed]
- Garcia-arumi, J.; Leila, M.; Zapata, M.A.; Velázquez, D.; Dinares-fernandez, M.C.; Tresserra, F. Endoresection technique with /without brachytherapy for management of high posterior choroidal melanoma: Extended Follow-up Results. Retina 2015, 35, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Biewald, E.; Lautner, H.; Gök, M.; Horstmann, G.A.; Sauerwein, W.; Flühs, D.; Bornfeld, N. Endoresection of large uveal melanomas: Clinical results in a consecutive series of 200 cases. Br. J. Ophthalmol. 2017, 101, 204–208. [Google Scholar] [CrossRef]
- Vidoris, A.A.C.; Maia, A.; Lowen, M.; Morales, M.; Isenberg, J.; Fernandes, B.F.; Belfort, R.N. Outcomes of primary endoresection for choroidal melanoma. Int. J. Retin. Vitr. 2017, 3, 42. [Google Scholar] [CrossRef]
- Süsskind, D.; Dürr, C.; Paulsen, F.; Kaulich, T.; Bartz-Schmidt, K.U. Endoresection with adjuvant ruthenium brachytherapy for selected uveal melanoma patients—The Tuebingen experience. Acta Ophthalmol. 2017, 95, e727–e733. [Google Scholar] [CrossRef]
- Caminal, J.M.; Mejia, K.; Masuet-Aumatell, C.; Arias, L.; Piulats, J.M.; Gutierrez, C.; Pera, J.; Catala, J.; Rubio, M.; Arruga, J. Endoresection versus iodine-125 plaque brachytherapy for the treatment of choroidal melanoma. Am. J. Ophthalmol. 2013, 156, 334–342.e1. [Google Scholar] [CrossRef]
- Rice, J.C.; Stannard, C.; Cook, C.; Lecuona, K.; Myer, L.; Scholtz, R.P. Brachytherapy and endoresection for choroidal melanoma: A cohort study. Br. J. Ophthalmol. 2014, 98, 86–91. [Google Scholar] [CrossRef]
- Zirm, E. Über endobulbare operationen. Arch Augenheilkd 1911, 69, 233–251. [Google Scholar]
- Stallard, H.B. Partial choroidectomy. Br. J. Ophthalmol. 1966, 50, 660–662. [Google Scholar] [CrossRef] [PubMed]
- Foulds, W.S. The local excision of choroidal melanomata. Trans. Ophthalmol. Soc. U. K. 1973, 93, 343–346. [Google Scholar] [PubMed]
- Peyman, G.A.; Axelrod, A.J.; Graham, R.O. Full-Thickness Eye Wall Resection: An Experimental Approach for Treatment of Choroidal Melanoma: Evaluation of Cryotherapy, Diathermy, and Photocoagulation. Arch. Ophthalmol. 1974, 91, 219–222. [Google Scholar] [CrossRef] [PubMed]
- Shields, J.A.; Augsburger, J.J.; Stefanyszyn, M.A.; Connor, R.W. Sclerochorioretinal resection for choroidal melanoma. A clinicopathologic correlation of a postmortem eye. Ophthalmology 1984, 91, 1726–1730. [Google Scholar] [CrossRef] [PubMed]
- Shields, J.A.; Shields, C.L. Surgical approach to lamellar sclerouvectomy for posterior uveal melanomas: The 1986 Schoenberg lecture. Ophthalmic Surg. 1988, 19, 774–780. [Google Scholar]
- Damato, B. The role of eyewall resection in uveal melanoma management. Int. Ophthalmol. Clin. 2006, 46, 81–93. [Google Scholar] [CrossRef]
- Peyman, G.A.; Apple, D.J. Local Excision of Choroidal Malignant Melanoma: Full-Thickness Eye Wall Resection. Arch. Ophthalmol. 1974, 92, 216–218. [Google Scholar] [CrossRef]
- Meyer-Schwickerath, G. Excision of malignant melanoma of the choroid. Mod. Probl. Ophthalmol. 1974, 12, 562–566. [Google Scholar]
- Damato, B.; Foulds, W.S. Indications for trans-scleral local resection of uveal melanoma. Br. J. Ophthalmol. 1996, 80, 1029–1030. [Google Scholar] [CrossRef][Green Version]
- Char, D.H.; Miller, T.; Crawford, J.B. Uveal tumour resection. Br. J. Ophthalmol. 2001, 85, 1213–1219. [Google Scholar] [CrossRef]
- Kim, J.W.; Damato, B.E.; Hiscott, P. Noncontiguous tumor recurrence of posterior uveal melanoma after transscleral local resection. Arch. Ophthalmol. 2002, 120, 1659–1664. [Google Scholar] [CrossRef]
- Damato, B.E.; Paul, J.; Foulds, W.S. Risk factors for residual and recurrent uveal melanoma after trans-scleral local resection. Br. J. Ophthalmol. 1996, 80, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Damato, B. Adjunctive plaque radiotherapy after local resection of uveal melanoma. Front. Radiat. Ther. Oncol. 1997, 30, 123–132. [Google Scholar] [PubMed]
- Damato, B.; Groenewald, C.P.; McGalliard, J.N.; Wong, D. Rhegmatogenous retinal detachment after transscleral local resection of choroidal melanoma. Ophthalmology 2002, 109, 2137–2143. [Google Scholar] [CrossRef] [PubMed]
- Damato, B.E.; Paul, J.; Foulds, W.S. Predictive factors of visual outcome after local resection of choroidal melanoma. Br. J. Ophthalmol. 1993, 77, 616–623. [Google Scholar] [CrossRef]
- Peyman, G.A.; Barrada, A. Retinochoroidectomy ab interno. Ophthalmic Surg. 1984, 15, 749–751. [Google Scholar]
- Peyman, G.A.; Cohen, S.B. Ab interno resection of uveal melanoma. Int. Ophthalmol. 1986, 9, 29–36. [Google Scholar] [CrossRef]
- Robertson, D.M.M. Melanoma Endoresection: A Perspective. Retin. J. Retin. Vitr. Dis. 2001, 21, 403–407. [Google Scholar] [CrossRef]
- Garcia-arumi, J.; Distefano, L.N.; Quijano, C. Endoresection of a high equatorial choroidal melanoma. Retina 2015, 9, 30–32. [Google Scholar] [CrossRef]
- Ledowski, T.; Kiese, F.; Jeglin, S.; Scholz, J. Possible air embolism during eye surgery. Anesth. Analg. 2005, 100, 1651–1652. [Google Scholar] [CrossRef]
- Rice, J.C.; Liebenberg, L.; Scholtz, R.P.; Torr, G. Fatal air embolism during endoresection of choroidal melanoma. Retin. Cases Brief Rep. 2014, 8, 127–129. [Google Scholar] [CrossRef] [PubMed]
- Morris, R.E.; Sapp, M.R.; Oltmanns, M.H.; Kuhn, F. Presumed air by vitrectomy embolisation (PAVE) a potentially fatal syndrome. Br. J. Ophthalmol. 2014, 98, 765–768. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Wei, W.-B. Acute pulmonary embolism caused by local resection of choroidal melanoma. Chin. Med. J. 2016, 129, 743–745. [Google Scholar] [CrossRef] [PubMed]
- Gayer, S.; Palte, H.D.; Albini, T.A.; Flynn, H.W.; Martinez-Ruiz, R.; Salas, N.; McClellan, A.J.; Relhan, N.; Parel, J.-M. In-Vivo Porcine Model of Venous Air Embolism During Pars Plana Vitrectomy. Am. J. Ophthalmol. 2017, 177, 139–144. [Google Scholar] [CrossRef]
- Suesskind, D.; Ulmer, A.; Schiebel, U.; Fierlbeck, G.; Spitzer, B.; Spitzer, M.S.; Bartz-Schmidt, K.U.; Grisanti, S. Circulating melanoma cells in peripheral blood of patients with uveal melanoma before and after different therapies and association with prognostic parameters: A pilot study. Acta Ophthalmol. 2011, 89, 17–24. [Google Scholar] [CrossRef]
- Diener-West, M.; Earle, J.D.; Fine, S.L.; Hawkins, B.S.; Moy, C.S.; Reynolds, S.M.; Schachat, A.P.; Straatsma, B.R.; Collaborative Ocular Melanoma Study Group. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma, III: Initial mortality findings. COMS Report No. 18. Arch Ophthalmol. 2001, 119, 969–982. [Google Scholar]
- Damato, B.; Wong, D.; Green, F.D.; Mackenzie, J.M. Intrascleral recurrence of uveal melanoma after transretinal “endoresection”. Br. J. Ophthalmol. 2001, 85, 114–115. [Google Scholar] [CrossRef]
- Mittica, N.; Vemuganti, G.K.; Duffy, M.; Torczynski, E.; Edward, D.P. Late Orbital Recurrence of a Choroidal Melanoma Following Internal Resection. Surv. Ophthalmol. 2003, 48, 181–190. [Google Scholar] [CrossRef]
- Ruest, P.; Aroichane, M.; Cordahi, G.; Bureau, N. Possible venous air embolism during open eye surgery in a child. Can. J. Anaesth. 2007, 54, 840–844. [Google Scholar] [CrossRef][Green Version]
- Dermigny, F.; Daelman, F.; Guinot, P.-G.; Hubert, V.; Jezraoui, P.; Thomas, F.; Milazzo, S.; Dupont, H. Fatal air embolism during open eye surgery. Ann. Fr. Anesth. Reanim. 2008, 27, 840–842. [Google Scholar] [CrossRef]


| Local Resection of Uveal Melanoma * |
|---|
| Exoresection (ab externo technique) Iridectomy Cyclectomy Choroidectomy Any combination of the terms above Endoresection (ab interno technique) |
| Author | Patients, n | Diameter, mm | Thickness, mm | Follow-Up, mean | Mortality/Survival | Enucleation | Recurrence | VA, Pre-Treatment | VA, Post-Treatment | Complications/BT | Adjuvant Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Peyman et al., 1984 [7] | 34 | Mean, 5.3 years (range, 1 to 10 years) | 6% (2 pts died due to mets) | 11 (32.3%) | 14.7% (5 pts) incomplete resection | Postoperative VA ranged from 20/30 to light perception. Ten cases had VA > 20/200 (33%) | Most common operative complication: vitreous hemorrhage. Tractional RD occurred in 10 cases, 5 of which were inoperable, leading to phthisis bulbi and enucleation, cataract formation (9 pts), preretinal membranes, macular pucker, and chronic cystoid macular edema (4 pts). | No BT. | |||
| Foulds et al., 1986 [8] | 140 | Tumours up to 15 mm | 9% (12 pts) 5-year survival 84% | Overall: 18% Recurrence 8.5% | 14% 8.5% (12 pts) 1 orbital recurrence first cases | 60% retained useful vision and 25% good vision | Not reported | No BT. | |||
| Shields et al., 1991 [9] | 95 | Mean 8.4 (range, 3.0 to 16.0) | Range, 2.0 to 12.0 (mean, 6.5) | Mean, 5.0 years; Median, 2.5 years (Range, 0.5 to 15.0 years) | 5% mets (5 pts) | 15 pts (16%) | 15 pts (16%) | 23 cases (24%) VA was ≥preoperative VA | VH 83%, intraretinal o subretinal hemorrhage 35% (most resolved spontaneously) RD: 28% Cataract: 34% RD surgery: 17% | No BT | |
| Damato et al., 1996 [10] | 332 | 13.2 (SD: 4.1) | 7.4 (SD, 3.0) | Median: 36 m (Range, 42 days–20.9 years) | 5-year mortality rates for pts with largest basal tumour diameters of <11 mm, 11–15 mm, and >15 mm: 3%, 20%, and 44%, respectively. | Adjuvant BT in 50 pts (15%) | |||||
| Damato et al., 2006 [11] | 344 | Median 13 (range, 4 to 21.0) | Median 8 (range, 1.5 to 16.5) | Median: 13.0 years | 16-year metastatic mortality was 20.2% if no risk factors *, 32.5% with one risk factor, and 46.7% with 2 risk factors. | 8 y actuarial rates of eye preservation ranged from 57.1% (>1 ocular risk factor) to 81% for no risk factors *** | 8-year actuarial rates of local tumour control were 75.2% in the absence of any risk factors **, 71.2% with one risk factor, and 47.1% with ≥1 risk factor | 20/17–20/40 in 59.3%, 20/50–20/200 in 28.5%, counting fingers in 8.7%, and hand movements to light perception in 3.5% | 8-year actuarial rates of conservation of vision of counting fingers or better were 63.9% if no risk factors *** were present, 60.1% with one risk factor, and 43.5% with more than one risk factor | RD tended to occur in the early postoperative period. The 2-year actuarial rate of RD was 16.6% (if the tumour height was <6 mm, increasing to 34.0% if the tumour was >9 mm). | Adjuvant BT: 129 pts (37.5%) |
| Bechrakis et al., 2010 [12] | 150 included over 210 | Median 14.5 (SD: 3.1) (range, 6.0–22.5) | Median 9.4 (SD: 2.0); (range, 2.0–14.6 | Median 45.5 (SD 31.6) 3–142 months | 5- and 10-year metastatic rates were 28% and 44%, respectively. Significant risk factors were extraocular spread, tumour thickness, and local tumour recurrence | 9 pts (6%) | Residual tumour: 6%; Recurrence: 26 pts (17.3%); 5 and 10 year recurrence rates: 24% and 32%. Significant risk factors: older age, large basal diameter, lack of adjuvant ruthenium brachytherapy, and RD. | Not reported | No reported complications | Adjuvant BT in 136 pts (90.6%) |
| Author | Treatment | Patients, n. | Diameter, mm | Thickness, mm | Follow-Up, mean | Survival | Enucleation | Recurrence | VA Pre-Treatment | VA Post-Treatment | BT |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Foulds et al., 1987 (Matched for diameter) [13] | PLSU (Laser or BT adjuvant not all) | 157 | 13.3 ± 4 mm maximum diameter | Overall 5 years 79% (26/33) <15 mm diameter 5-year mortality 11.6% and >16 mm 57% | 22% | 17% residual or recurrent 2% orbital recurrent | 65% useful vision (between 6/6 and CF) | VH: 23% RD: 25% CT:15–61% | |||
| Enucleation | 241 | 13.3 ± 4 mm maximum diameter | 5 years: 47% (89/188) 5-year mortality by diameter <15 mm: 30% >16 mm: 65% | 100% | 0 | 0 | - | ||||
| Augsburger et al., 1990 [14] | PLSU (No BT adjuvant) | 30 | 9.8 | 5.7 | 3.0 y | 3/30 KM 5 years: 85.2% | 20/30 | 20/200 <20/200 at 5 years 66.8% | Significantly worse vision in PLSU | ||
| BT Co60 | 30 | 10.7 | 5.8 | 6.0 y | 7/30 KM 5 years: 81.8% | 20/25 | 20/40 <20/200 at 5 years 44.4% (p = 0.0008) | No difference in mortality | |||
| Bechrakis et al., 2002 [15] | PLSU (BT Ruth-106 adj., not all) | 85 (36 matched) | 14.4 (±3.0) | 9.5 (±2.1) | 24.0 m (±16) | 5.6% NO KM curves | 11.1% | Persistent tumour: 13.9% Recurrence: 8.3% | ≥20/200 retained in 61.1% | Cataract: 44.4% Additional VR surgery: 44.4% Peripheral cryo: 5.6% PRP:2.8% Neovascular glaucoma 5.6% Cyclocrio: 0% | |
| BT I-125 | 152 (80 matched) | 14.6 (±2.4) | 9.0 (±1.1) | 33.0 m (±19) | 11.1% NO KM curves | 5.6% | Persisting tumour 5.6% Recurrence 5.6% | 20/200 or better was retained in 5.6% | Cataract: 28% PRP: 66.6% Peripheral cryo: 11.1% Neovasc glaucoma 33.3% Cyclocryo: 5.6% | ||
| Kivela et al., 2003 [16] two centres only, one treatment in each centre (UK/ Finland retrospective study) | PLSU (BT Ruth106 adjuvant not all) | 49 | less than 12 mm for 13 pairs (26%), between 12 and 14 mm for 17 pairs (35%), and 14 mm or more for 19 pairs (39%). | Median 8.0 IQR (7.0–9.0) | 18.3% (9 pts mets) 8 year all-cause and melanoma-specific survivals did not differ | Not reported Almost 32.6% (16 recurrences) | 16 pts (32.6%) (14 pts, no adjuvant RT) 2 pts also developed an extrascleral recurrence | 20/40 or better for 17 (35%) matched pairs, between 20/50 and 20/200 for 25 pairs (51%), and worse than 20/200 for 7 pairs (14% | The risk of losing 20/60 vision did not differ statistically after TSR and IBT The risk of losing 20/200 vision was significantly higher after IBT than after TSR | Higher risk of cataract, vitreous hemorrhage, maculopathy after IBT Rubeosis, neovascular glaucoma, and optic neuropathy developed only after IBT | |
| BT I-125 | 49 | idem | Median 7.8 IQR (7.0–9.3) | 22.4% (11 pts mets) | 6.1% (3 pts) | 6.1% (3 pts) | Significantly Higher risk of local recurrence after TSR The risk of retinal detachment did not differ between TSR and IBT | ||||
| Puusaari et al., 2007 [11] two centres only, one treatment in each centre (UK/ Finland retrospective study) | PLSU (BT Ruth106 adjuvant not all) | 33 | Median 12.5 mm (range 9.8–16) | Median 11.0 mm (range, 8.0–14) | 2.3 years | Not reported | 24.2% (8 pts) 5-year incidence 28% (95% CI, 7–40) | 27% (9 pts) 5-year incidence of local recurrence 41% (95% CI, 17–63) after TSR. 37% vs. 46% adjuvant irradiation vs. none. | 33% (11 pts) in the TSR arm and 33% (18 pts) in the IBT arm had visual acuity better than 20/70 | The mean visual acuity after TSR was 20/320 to 20/640 throughout the first 5 years and approximately one line better than the mean visual acuity after IBT, which varied between 20/640 and 20/1250 Cumulative incidence of loss of visual acuity 20/400 was 53% at one and 60% at 2 and 3 years | Adj. ruth BT. At 5 years, cataract in 91% after TSR and 78% after IBT. At 5 years, maculopathy in 63% after TSR and 43% after IBT. RD 5-year cumulative incidence 43%. decreased rapidly to <20% after TSR. Vitreous bleeding in 69% within 6 months of surgery but no new bleeding after this period. Glaucoma and optic neuropathy were rare after TSR |
| BT I-125 | 54 | 14.0 mm (range, 7.3–16) | median, 10.6 mm; range, 8.2–13.3 | 5.3 years | Not reported | 5 pts 5-year incidence 10% (95% CI 4–20) | 3 pts 5-year incidence of local recurrence: 7% (95% CI, 2–17) after IBT | Cumulative incidence of loss of visual acuity 20/400 were 60% (95% CI, 44–73), 75% (95% CI, 59–86) and 91% (95% CI, 76–97) | Iris NV and glaucoma only in IBT optic neuropathy 5 years was 7% TSR and 58% in IBT RD exudative 5-year cumulative incidence 27% vitreous haemorrhage 5-year cumulative incidence of was 39% after IBT Cataract, maculopathy, RD, and vitreous haemorrhage were common after either treatment. | ||
| Caminal et al., 2016 [17] Resection without hypotensive anaesthesia | PLSU (adjvant BT in some but not all) | 19 | Median 14.7 (11.0–20.0) | Median 11 (4.0–12.0) | 50.9 months (9.6–102.5 | 15.8% (3 mets) 10.5% (2 deaths) K-M at 5 years 79.1% without mets K-M DSS: 84% at 5 y | 21.1% (5 pts) KM at 5 ears 70.9% maintain the eye | 10.5% (3 pts) K-M at 5 years 82.5% free Recurrences in pts no adjuvant BT | 20/200 (20/20.000–20/20) | 20/34 (20/20.000–20/20) ≥20/200 or better: 53.3% | Better preservation of VA. Most common complications: rhegmatogenous RD (21.1%) and ocular hypertension (21.1%). |
| I-125 BT | 53 | Median 15.5 (8.0–20.0) | Median 9 (6.0–11.0) | 55.9 months (9.6–107.8) | 26.4% (14 mets) 9.4% (5 deaths) K-M at 5 years: 74.2% without mets K-M at 5 years DSS: 93.2% | 9.4% (4 pts) KM at 5 y 89.8% | 5.7% (2 pts) K-M at 5 years 94.1% free | 20/40 (20/20.000–20/20) | 20/20.000 (20/200.000–20/25) ≥20/200: 31.2% | Most common complications: radiation-induced retinopathy (45.3%), neovascular glaucoma (28.3%) and macular oedema. (24.5%) |
| Authors | Patients, n | Diameter, mm | Thickness, mm | Follow-Up, mean | Survival | Enucleation | Recurrence | VA Pretreatment | VA Posttreatment | Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| Kertes et al., 1998 [18] Case series retrospective No adjuvant BT | 32 | 8.0 (range 3–18) | 5.3 (flat to 12.0) | 40 | 9.4% (3 pts) died | 9.4% (3 pts) | 3.1% (1 pts) | 31.2% had VA ≥ 6/60; 56.3% between 6/120 and light perception, 12.5% NLP | VH (37.5%); cataract (25%); RD (9.3%); glaucoma (9.3%). | |
| Damato et al., 1998 [19] Retrospective case series Adjuvant BT selected pts | 52 | 8.2 (range 4.0–14.0) | 3.9 (1.5–10.1) | 20 | 0 | 10% | 0 | 90% eye retention | RD (16), cataract (25), ocular hypertension (14), phthisis (one), epiretinal membrane (one), VH (two), possible local tumour recurrence (eight), and endophthalmitis (one) | |
| Garcia-Arumi et al., 2001 [20] Retrospective case series Adjuvant BT selected pts | 25 | 12.1 (range, 8.9–14.8) | 10.6 (range, 9.1–12.8) | 31 (12–72) | 0 | 0 | 0 | Mean, 20/60 (range, 20/400 to 20/20) | Hand motions to 20/30 (mean, 20/100) | Hemorrhage at the scleral bed (100%), cataract (40%), ocular hypertension (32%), RD (16%), macular traction (16%), epiretinal macular proliferation (8%), branch vein occlusion (4%), and submacular hemorrhage (4%). |
| Bechrakis et al., 2006 [21] Retrospective case series Adjunctive Proton radiotherapy | 58 | 15.6 (11.1–21.6) | Median: 8.8 (range, 7.0–14.5) | Median 18 m (3.0–48) | 4% (2 mets) | KM at 2 years was 8.4% | 2% (1 recurrence at 40 m) | 20/40 (range, 20/400–20/20) | Median: 20/200 | KM at 2 years: Cataract: 46.6%; RD 32.1%; Macular hole 4.0%; Secondary glaucoma 2.6%; Phthisis 2.1%; Macular pucker 1.8%; Radiation retinopathy: 27.5%; radiation optic neuropathy: 29.4% |
| Karkhaneh et al., 2007 [22] Retrospective case series No adjuvant BT | 20 | 11.67 (range, 8.0–15.7) | 8.51 (range, 5.5–11) | 89.55 months (24–132) | 5% (1 pt) | 15% (3 pts) | 10% (2 pts) | Mean, 20/100 (hand motions to 20/30) | No light perception to 20/30 | Cataract: 25%: RD: 15%; Bullous keratopathy: 10% |
| Garcia-Arumi et al., 2008 [23] Retrospective case series BT all pts | 38 | 9.9 (5–15) | 10.1(7.7–13.5) | Mean 70.63 (23 to 129) | 13% (3/23) 90.9% at 5 years (K-M) | 7.9% (3 pts) | 5.8% (2 pts) | 20/60 (‘‘hand-movements’’ to 20/20) | Mean 20/300 (‘‘no light perception’’ to 20/30) | Hemorrhage at the scleral bed: 100%; ocular hypertension: 31.5%; RD: 26%; epiretinal macular proliferation: 11%; post-radiation retinopathy: 5.2%; and subretinal neovascularisation: 5.2% at 2 years |
| Konstantinidis et al., 2014 [24] NO adjuvant BT | 71 | 9.5 (4.8–14.5) | 4.4 (0.9–11.1) | 49.2 m (range, 24 to 195.6 m) | 7% (5/71) 9% at 5 years and 10 years | 4% | 3% (2 pts) 3.7% at 10 years KM | Better than 6/12 in 9 (13%) and better than 6/30 in 21 (31%) | Cataract (94%), transient ocular hypertension (10%), epiretinal membrane (13%) and moderate haemorrhage (3%); RD (22%). | |
| Garcia-Arumi J. et al., 2015 [25] 20 pat endoresection alone 21 pts BT | 41 | 9.9 (range, 5–15) | 9.8 (range, 7.7–13.5) | 102.5 (20–180) | 7.3% (3 pts) KM at 10 years 97.6% | 12..2% | 5 pts (12.2%) in the group endo alone | 20/100 (range, hand movement–20/20) | No light perception to 20/20, with mean 20/1625 | RD 28.9%; Phthisis bulbi 12.2%; PRP 9.8%; ERM 12.2%; CNVM 4.9%; Subretinal fibrosis 2.4%; Ocular hypertension 34.1%; VH 2.4%; CME 2.4%; corneal decompensation 2.4% |
| Biewald E et al., 2017 [26] Prior treatment with gamma and postop BT | 200 | 12 (range, 6.3–20) | 9.4 (range 6–14.8) | 32.3 months | 15.5% (31 /200) | 11% (22/200) | 5% (10 pts) | 13.4% the VA of 20/50 or better and 20/400 to 20/50 in 33.6% | Cataract surgery in 70%; pars plana vitrectomy revision surgery in 1.5%; use of an adjuvant ruthenium-106 plaque did not lower recurrence | |
| Vidoris et al., 2017 [27] No adjuvant BT | 14 | 15.98 ± 4.76 (range: 4.3–23) | 6.05 ± 1.94 (range: 3.3–9.7) | Mean 54.5 (range: 12–60 m) | 7.1% (1 pt) | 0 | 0 | Between 20/60 and 20/200 (78.5%) | Macular bleeding (7.1%); elevated IOP (7.1%); RD (14.2%) | |
| Susskind et al., 2017 Adjuvant BT [28] | 35 | Mean 13.0 (8..4–17.6) | Mean: 7.33 (range, 4.06–12.2) | Mean: 65.7 (12 and 154) | 20% (7 pts) 92.0% 5 years and 57.9% 10 years KM | 22.9% (8 pts) 77.3% 5 years and 70.8% 10 years KM | 22.9% (8 pts) (22.7% at 5 years and 29.2% at 10 years (KM) | Median 0.2 (2.3–0) LogMar | Median 2.0 (4.0–0.4) LogMar | Radiation retinopathy: 11.4%; CNV: 8.6%); pale optic disc (opticopathy): 31.4%; corneal decompensation: 8.6%; epiretinal membrane: 5.7%; RD PVR: 11.4%; macular hole: 2.8%; persistent corneal erosion: 2.8%; corneal band keratopathy: 5.7%; persistent hypotony: 5.7%. |
| Author | Treatment | Pts, n | Diameter, mm | Thickness | Follow-Up, mean | Survival | Enucleation | Recurrence | VA, Pre-Treatment | VA, Post-Treatment | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Caminal et al., 2013 [29] | Endoresection (no BT adjuvant) | 27 | 11 (IQR 2.9) | 7.69 (IQR 2.27) | 59.37 (12–138) | 3.7% (1/27) metastasis 3.7% specific death 100% at 5 years (K-M) cause-specific survival | 11.1% (3 pts) 87.8% at 5 years (K-M) | 7.4% (2 pts) 92.4% at 5 years (K-M) | 0.2 | 22.2% 20/200 or better KM probability of maintaining a VA equal or superior to 20/200 at 5 years was 59.9% | |
| BT | 54 | 12.5 (IQR 2.0) | 6.95 (IQR1.8) | 70.52 (12–148) | 20.4% (11 pts) 18.5% specific death 84.2% at 5 years (K-M) cause-specific survival | 13% (7 pts) 85.7% at 5 years (K-M) | 1.8% (1 pts) 96.6% at 5 years (K-M) | 35.2% 20/200 or better KM probability of maintaining a VA equal or superior to 20/200 at 5 years was 66.4% group and 59.9% in the endoresection group | |||
| Rice et al., 2014 [30] | Endoresection (BT adjuvant) | 22 | 11.2(3.4–16.0) | 7.3 mm (3.0–10.0) | 62.4 (7.9–121.8) | 18.2% metastasis 20.4% died | 4.6% (1 pts) | 18.2% (4 pts) | Snellen ±6/24 | ±6/50 6/18 or better in 41% of endoresection group and 35% of the BT group retained vision of 6/18 or better at the end of follow-up. Eight out of 22 (36%) endoresection and 68/142 (48%) BT had 2/60 or worse at the last visit | |
| BT | 148 | 10.3 mm (range 4.5–16.0) | 4.9 mm (range 2.5–10.0 | 55.4 (6.6–175.8) | 14.2% | 10.8% | Local recurrence rate higher in endoresection group (18.2% vs. 14.9%, p = 0.75) but not significant. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caminal, J.M.; Lorenzo, D.; Gutierrez, C.; Slocker, A.; Piulats, J.M.; Cobos, E.; Garcia-Bru, P.; Morwani, R.; Santamaria, J.F.; Arias, L. Local Resection in Choroidal Melanoma: A Review. J. Clin. Med. 2022, 11, 7156. https://doi.org/10.3390/jcm11237156
Caminal JM, Lorenzo D, Gutierrez C, Slocker A, Piulats JM, Cobos E, Garcia-Bru P, Morwani R, Santamaria JF, Arias L. Local Resection in Choroidal Melanoma: A Review. Journal of Clinical Medicine. 2022; 11(23):7156. https://doi.org/10.3390/jcm11237156
Chicago/Turabian StyleCaminal, Josep Maria, Daniel Lorenzo, Cristina Gutierrez, Andrea Slocker, Josep Maria Piulats, Estefania Cobos, Pere Garcia-Bru, Rahul Morwani, Juan Francisco Santamaria, and Luis Arias. 2022. "Local Resection in Choroidal Melanoma: A Review" Journal of Clinical Medicine 11, no. 23: 7156. https://doi.org/10.3390/jcm11237156
APA StyleCaminal, J. M., Lorenzo, D., Gutierrez, C., Slocker, A., Piulats, J. M., Cobos, E., Garcia-Bru, P., Morwani, R., Santamaria, J. F., & Arias, L. (2022). Local Resection in Choroidal Melanoma: A Review. Journal of Clinical Medicine, 11(23), 7156. https://doi.org/10.3390/jcm11237156






