Cord Blood Cardiovascular Biomarkers in Left-Sided Congenital Heart Disease
Abstract
1. Introduction
2. Materials and Methods
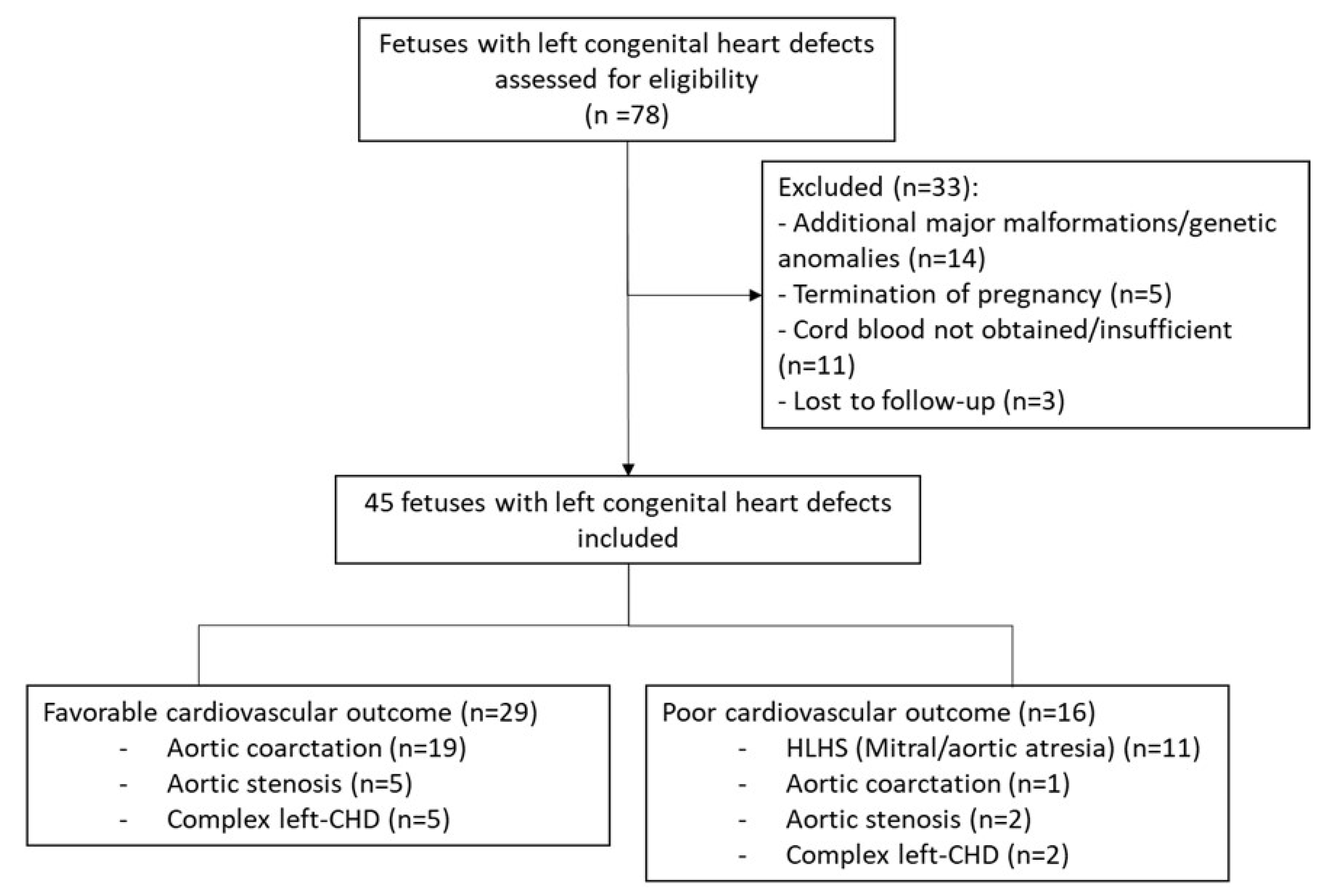
2.1. Study Population
2.2. Fetal Standard Ultrasound and Echocardiography
2.3. Cord Blood Biomarkers
2.4. Statistical Analysis
3. Results
3.1. Study Populations
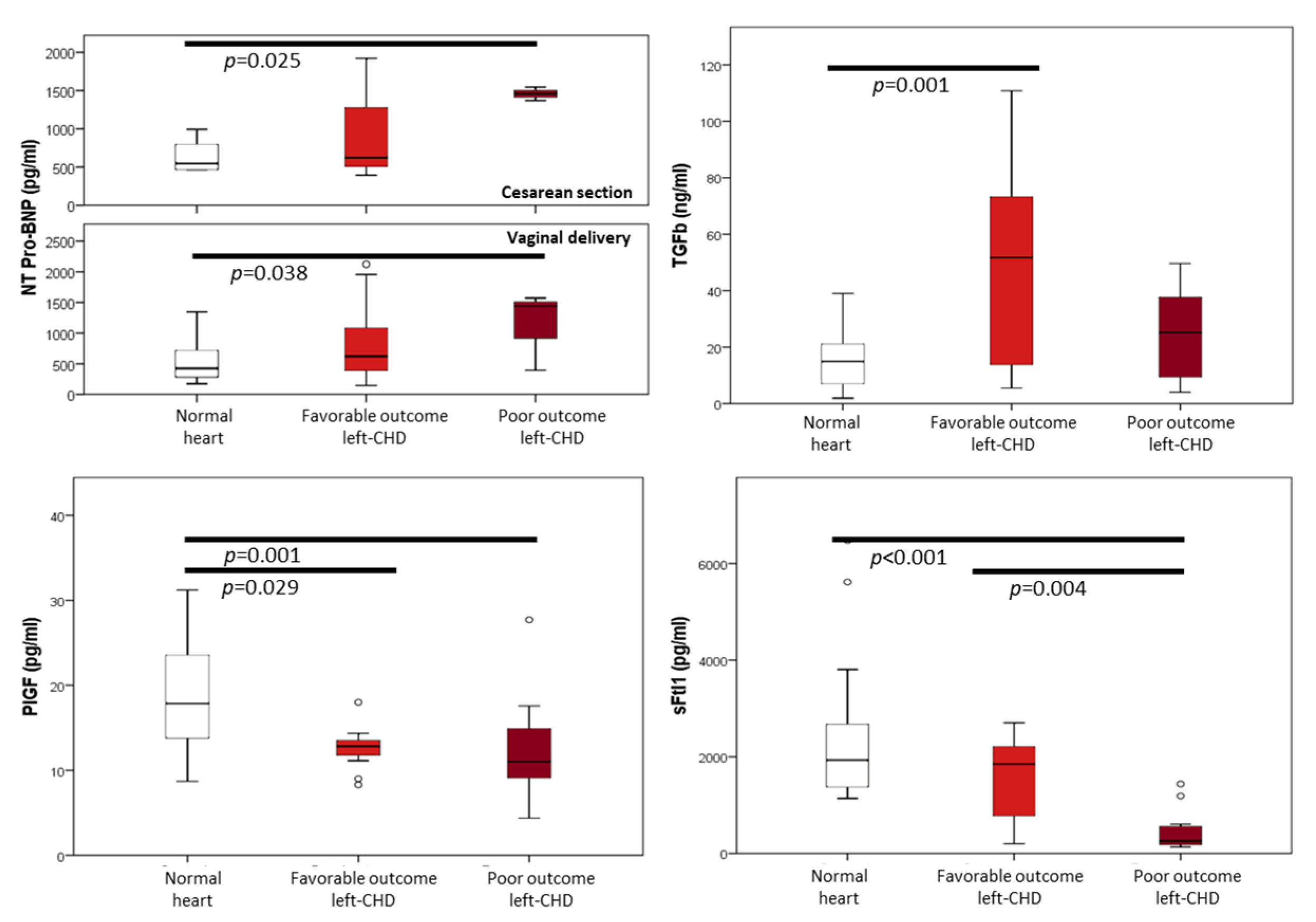
3.2. Cord Blood Biomarkers Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Wren, C.; Reinhardt, Z.; Khawaja, K. Twenty-Year Trends in Diagnosis of Life-Threatening Neonatal Cardiovascular Malformations. Arch. Dis. Child. Fetal Neonatal Ed. 2008, 93, F33–F35. [Google Scholar] [CrossRef]
- Khoo, N.S.; Van Essen, P.; Richardson, M.; Robertson, T. Effectiveness of Prenatal Diagnosis of Congenital Heart Defects in South Australia: A Population Analysis 1999–2003. Aust. N. Z. J. Obstet. Gynaecol. 2008, 48, 559–563. [Google Scholar] [CrossRef]
- Davlouros, P.A.; Karatza, A.A.; Xanthopoulou, I.; Dimitriou, G.; Georgiopoulou, A.; Mantagos, S.; Alexopoulos, D. Diagnostic Role of Plasma BNP Levels in Neonates with Signs of Congenital Heart Disease. Int. J. Cardiol. 2011, 147, 42–46. [Google Scholar] [CrossRef]
- Cantinotti, M.; Giordano, R.; Scalese, M.; Molinaro, S.; Della Pina, F.; Storti, S.; Arcieri, L.; Murzi, B.; Marotta, M.; Pak, V.; et al. Prognostic Role of BNP in Children Undergoing Surgery for Congenital Heart Disease: Analysis of Prediction Models Incorporating Standard Risk Factors. Clin. Chem. Lab. Med. 2015, 53, 1839–1846. [Google Scholar] [CrossRef]
- Agewall, S.; Giannitsis, E.; Jernberg, T.; Katus, H. Troponin Elevation in Coronary vs. Non-Coronary Disease. Eur. Heart J. 2011, 32, 404–411. [Google Scholar] [CrossRef]
- Lee, S.M.; Kwon, J.E.; Song, S.H.; Kim, G.B.; Park, J.Y.; Kim, B.J.; Lee, J.H.; Park, C.W.; Park, J.S.; Jun, J.K. Prenatal Prediction of Neonatal Death in Single Ventricle Congenital Heart Disease. Prenat. Diagn. 2016, 36, 346–352. [Google Scholar] [CrossRef]
- Dabek, J.; Kułach, A.; Monastyrska-Cup, B.; Gasior, Z. Transforming Growth Factor β and Cardiovascular Diseases: The Other Facet of the “Protective Cytokine”. Pharmacol. Rep. 2006, 58, 799–805. [Google Scholar]
- Clark, D.A.; Coker, R. Transforming Growth Factor-Beta (TGF-β). Int. J. Biochem. Cell Biol. 1998, 30, 293–298. [Google Scholar] [CrossRef]
- Guerri-Guttenberg, R.A.; Castilla, R.; Francos, G.C.; Müller, A.; Ambrosio, G.; Milei, J. Transforming Growth Factor Β1 and Coronary Intimal Hyperplasia in Pediatric Patients With Congenital Heart Disease. Can. J. Cardiol. 2013, 29, 849–857. [Google Scholar] [CrossRef]
- Doetschman, T.; Barnett, J.V.; Runyan, R.B.; Camenisch, T.D.; Heimark, R.L.; Granzier, H.L.; Conway, S.J.; Azhar, M. Transforming Growth Factor Beta Signaling in Adult Cardiovascular Diseases and Repair. Cell Tissue Res. 2012, 347, 203–223. [Google Scholar]
- Dobaczewski, M.; Chen, W.; Frangogiannis, N.G. Transforming Growth Factor (TGF)-β Signaling in Cardiac Remodeling. J. Mol. Cell. Cardiol. 2011, 51, 600–606. [Google Scholar] [CrossRef]
- Iwama, H.; Uemura, S.; Naya, N.; Imagawa, K.I.; Takemoto, Y.; Asai, O.; Onoue, K.; Okayama, S.; Somekawa, S.; Kida, Y.; et al. Cardiac Expression of Placental Growth Factor Predicts the Improvement of Chronic Phase Left Ventricular Function in Patients With Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2006, 47, 1559–1567. [Google Scholar] [CrossRef]
- Nakamura, T.; Funayama, H.; Kubo, N.; Yasu, T.; Kawakami, M.; Momomura, S.I.; Ishikawa, S.E. Elevation of Plasma Placental Growth Factor in the Patients with Ischemic Cardiomyopathy. Int. J. Cardiol. 2009, 131, 186–191. [Google Scholar] [CrossRef]
- Accornero, F.; Molkentin, J.D. Placental Growth Factor as a Protective Paracrine Effector in the Heart. Trends Cardiovasc. Med. 2011, 21, 220–224. [Google Scholar] [CrossRef]
- Chau, K.; Hennessy, A.; Makris, A. Placental Growth Factor and Pre-Eclampsia. J. Hum. Hypertens. 2017, 31, 782–786. [Google Scholar] [CrossRef]
- Llurba, E.; Sanchez, O.; Ferrer, Q.; Nicolaides, K.H.; Ruiz, A.; Dominguez, C.; Sanchez-de-Toledo, J.; Garcia-Garcia, B.; Soro, G.; Arevalo, S.; et al. Maternal and Foetal Angiogenic Imbalance in Congenital Heart Defects. Eur. Heart J. 2014, 35, 701–707. [Google Scholar] [CrossRef]
- Robinson, H.P.; Sweet, E.M.; Adam, A.H. The Accuracy of Radiological Estimates of Gestational Age Using Early Fetal Crown-Rump Length Measurements by Ultrasound as a Basis for Comparison. Br. J. Obstet. Gynaecol. 1979, 86, 525–528. [Google Scholar] [CrossRef]
- Familiari, A.; Morlando, M.; Khalil, A.; Sonesson, S.-E.; Scala, C.; Rizzo, G.; Del Sordo, G.; Vassallo, C.; Elena Flacco, M.; Manzoli, L.; et al. Risk Factors for Coarctation of the Aorta on Prenatal UltrasoundClinical Perspective. Circulation 2017, 135, 772–785. [Google Scholar] [CrossRef]
- Schneider, C.; McCrindle, B.W.; Carvalho, J.S.; Hornberger, L.K.; McCarthy, K.P.; Daubeney, P.E.F. Development of Z-Scores for Fetal Cardiac Dimensions from Echocardiography. Ultrasound Obstet. Gynecol. 2005, 26, 599–605. [Google Scholar] [CrossRef]
- Shone, J.D.; Sellers, R.D.; Anderson, R.C.; Adams, P.; Lillehei, C.W.; Edwards, J.E. The Developmental Complex of “Parachute Mitral Valve,” Supravalvular Ring of Left Atrium, Subaortic Stenosis, and Coarctation of Aorta. Am. J. Cardiol. 1963, 11, 714–725. [Google Scholar] [CrossRef]
- Rodríguez-López, M.; Cruz-Lemini, M.; Valenzuela-Alcaraz, B.; Garcia-Otero, L.; Sitges, M.; Bijnens, B.; Gratacos, E.; Crispi, F. Descriptive Analysis of the Different Phenotypes of Cardiac Remodeling in Fetal Growth Restriction. Ultrasound Obstet. Gynecol. 2017, 50, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Crispi, F.; Bijnens, B.; Figueras, F.; Bartrons, J.; Eixarch, E.; Le Noble, F.; Ahmed, A.; Gratacos, E. Fetal Growth Restriction Results in Remodeled and Less Efficient Hearts in Children. Circulation 2010, 121, 2427–2436. [Google Scholar] [CrossRef] [PubMed]
- Barker, D.J.P. Adult Consequences of Fetal Growth Restriction. Clin. Obstet. Gynecol. 2006, 49, 270–283. [Google Scholar] [CrossRef]
- Kocylowski, R.D.; Dubiel, M.; Gudmundsson, S.; Sieg, I.; Fritzer, E.; Alkasi, Ö.; Breborowicz, G.H.; von Kaisenberg, C.S. Biochemical Tissue-Specific Injury Markers of the Heart and Brain in Postpartum Cord Blood. Am. J. Obstet. Gynecol. 2009, 200, 273.e1–273.e25. [Google Scholar] [CrossRef]
- Patey, O.; Carvalho, J.S.; Thilaganathan, B. Perinatal Changes in Fetal Cardiac Geometry and Function in Diabetic Pregnancy at Term. Ultrasound Obstet. Gynecol. 2019, 54, 634–642. [Google Scholar] [CrossRef]
- Mert, M.K.; Satar, M.; Özbarlas, N.; Yaman, A.; Özgünen, F.T.; Asker, H.S.; Çekinmez, E.K.; Tetiker, T. Troponin T and NT ProBNP Levels in Gestational, Type 1 and Type 2 Diabetic Mothers and Macrosomic Infants. Pediatr. Cardiol. 2016, 37, 76–83. [Google Scholar] [CrossRef]
- García-Otero, L.; López, M.; Gómez, O.; Goncé, A.; Bennasar, M.; Martínez, J.M.; Valenzuela-Alcaraz, B.; Rodriguez-López, M.; Sitges, M.; Loncà, M.; et al. Zidovudine Treatment in HIV-Infected Pregnant Women Is Associated with Fetal Cardiac Remodelling. AIDS 2016, 30, 1393–1401. [Google Scholar] [CrossRef]
- Hadlock, F.P.; Harrist, R.B.; Shah, Y.P.; King, D.E.; Park, S.K.; Sharman, R.S. Estimating Fetal Age Using Multiple Parameters: A Prospective Evaluation in a Racially Mixed Population. Am. J. Obstet. Gynecol. 1987, 156, 955–957. [Google Scholar] [CrossRef]
- Figueras, F.; Meler, E.; Iraola, A.; Eixarch, E.; Coll, O.; Figueras, J.; Francis, A.; Gratacos, E.; Gardosi, J. Customized Birthweight Standards for a Spanish Population. Eur. J. Obstet. Gynecol. Reprod. Biol. 2008, 136, 20–24. [Google Scholar] [CrossRef]
- Carvalho, J.; Allan, L.; Chaoui, R.; Copel, J.; DeVore, G.; Hecher, K.; Lee, W.; Munoz, H.; Paladini, D.; Tutschek, B.; et al. ISUOG Practice Guidelines (Updated): Sonographic Screening Examination of the Fetal Heart. Ultrasound Obstet. Gynecol. 2013, 41, 348–359. [Google Scholar] [CrossRef]
- Bhide, A.; Acharya, G.; Bilardo, C.M.; Brezinka, C.; Cafici, D.; Hernandez-Andrade, E.; Kalache, K.; Kingdom, J.; Kiserud, T.; Lee, W.; et al. ISUOG Practice Guidelines: Use of Doppler Ultrasonography in Obstetrics. Ultrasound Obstet. Gynecol. 2013, 41, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Baschat, A.A.; Gembruch, U. The Cerebroplacental Doppler Ratio Revisited. Ultrasound Obstet. Gynecol. 2003, 21, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Figueras, F.; Gratacós, E. Update on the Diagnosis and Classification of Fetal Growth Restriction and Proposal of a Stage-Based Management Protocol. Fetal Diagn. Ther. 2014, 36, 86–98. [Google Scholar] [CrossRef]
- Paladini, D.; Chita, S.K.; Allan, L.D. Prenatal Measurement of Cardiothoracic Ratio in Evaluation of Heart Disease. Arch. Dis. Child. 1990, 65, 20–23. [Google Scholar] [CrossRef]
- García-Otero, L.; Soveral, I.; Sepúlveda-Martínez, Á.; Rodriguez-lópez, M.; Torres, X.; Guirado, L.; Nogué, L.; Valenzuela-Alcaraz, B.; Martínez, J.M.; Gratacós, E.; et al. Reference Ranges for Fetal Cardiac, Ventricular and Atrial Relative Size, Sphericity, Ventricular Dominance, Wall Asymmetry and Relative Wall Thickness from 18 to 41 Weeks of Gestation. Ultrasound Obstet. Gynecol. 2020, 58, 388–397. [Google Scholar] [CrossRef]
- Sepúlveda-Martínez, A.; García-Otero, L.; Soveral, I.; Guirado, L.; Valenzuela-Alcaraz, B.; Torres, X.; Rodriguez-Lopez, M.; Gratacos, E.; Gómez, O.; Crispi, F. Comparison of 2D versus M-Mode Echocardiography for Assessing Fetal Myocardial Wall Thickness. J. Matern. Neonatal Med. 2018, 32, 2319–2327. [Google Scholar] [CrossRef]
- García-Otero, L.; Gómez, O.; Rodriguez-López, M.; Torres, X.; Soveral, I.; Sepúlveda-Martínez, Á.; Guirado, L.; Valenzuela-Alcaraz, B.; López, M.; Martínez, J.M.; et al. Nomograms of Fetal Cardiac Dimensions at 18–41 Weeks of Gestation. Fetal Diagn. Ther. 2020, 47, 387–398. [Google Scholar] [CrossRef]
- Guirado, L.; Crispi, F.; Soveral, I.; Valenzuela-Alcaraz, B.; Rodriguez-López, M.; García-Otero, L.; Torres, X.; Sepúlveda-Martínez, Á.; Escobar-Diaz, M.C.; Martínez, J.M.; et al. Nomograms of Fetal Right Ventricular Fractional Area Change by 2D Echocardiography. Fetal Diagn. Ther. 2020, 47, 399–410. [Google Scholar] [CrossRef]
- DeVore, G.R.; Siassi, B.; Platt, L.D. Fetal Echocardiography. Am. J. Obstet. Gynecol. 1984, 150, 981–988. [Google Scholar] [CrossRef]
- Soveral, I.; Crispi, F.; Guirado, L.; García-Otero, L.; Torres, X.; Bennasar, M.; Sepúlveda-Martínez, Á.; Nogué, L.; Gratacós, E.; Martínez, J.M.; et al. Cardiac Filling and Ejection Time Fractions by Pulsed Doppler: Fetal Nomograms and Potential Clinical Application. Ultrasound Obstet. Gynecol. 2020, 58, 83–91. [Google Scholar] [CrossRef]
- Trevisanuto, D.; Pitton, M.; Altinier, S.; Zaninotto, M.; Plebani, M.; Zanardo, V. Cardiac Troponin I, Cardiac Troponin T and Creatine Kinase MB Concentrations in Umbilical Cord Blood of Healthy Term Neonates. Acta Paediatr. Int. J. Paediatr. 2003, 92, 1463–1467. [Google Scholar] [CrossRef]
- Eindhoven, J.A.; Van Den Bosch, A.E.; Jansen, P.R.; Boersma, E.; Roos-Hesselink, J.W. The Usefulness of Brain Natriuretic Peptide in Complex Congenital Heart Disease: A Systematic Review. J. Am. Coll. Cardiol. 2012, 60, 2140–2149. [Google Scholar] [CrossRef] [PubMed]
- Holmgren, D.; Westerlind, A.; Berggren, H.; Lundberg, P.A.; Wåhlander, H. Increased Natriuretic Peptide Type B Level after the Second Palliative Step in Children with Univentricular Hearts with Right Ventricular Morphology but Not Left Ventricular Morphology. Pediatr. Cardiol. 2008, 29, 786–792. [Google Scholar] [CrossRef] [PubMed]
- Wåhlander, H.; Westerlind, A.; Lindstedt, G.; Lundberg, P.A.; Holmgren, D. Increased Levels of Brain and Atrial Natriuretic Peptides after the First Palliative Operation, but Not after a Bidirectional Glenn Anastomosis, in Children with Functionally Univentricular Hearts. Cardiol. Young 2003, 13, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Eerola, A.; Jokinen, E.O.; Savukoski, T.I.; Pettersson, K.S.I.; Poutanen, T.; Pihkala, J.I. Cardiac Troponin I in Congenital Heart Defects with Pressure or Volume Overload. Scand. Cardiovasc. J. 2013, 47, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, M.; Ota, K.; Kajihama, A.; Nakau, K.; Manabe, H.; Kajino, H. Volume Overload and Pressure Overload Due to Left-to-Right Shunt-Induced Myocardial Injury: Evaluation Using a Highly Sensitive Cardiac Troponin-I Assay in Children with Congenital Heart Disease. Circ. J. 2011, 75, 2213–2219. [Google Scholar] [CrossRef]
- Goodwill, A.G.; Dick, G.M.; Kiel, A.M.; Tune, J.D. Regulation of Coronary Blood Flow. Compr. Physiol. 2017, 7, 321–382. [Google Scholar] [CrossRef]
- Briana, D.D.; Liosi, S.; Gourgiotis, D.; Boutsikou, M.; Marmarinos, A.; Baka, S.; Hassiakos, D.; Malamitsi-Puchner, A. Fetal Concentrations of the Growth Factors TGF-α and TGF-Β1 in Relation to Normal and Restricted Fetal Growth at Term. Cytokine 2012, 60, 157–161. [Google Scholar] [CrossRef]
- Walshe, T.E.; Dela Paz, N.G.; D’Amore, P.A. The Role of Shear-Induced Transforming Growth Factor-β Signaling in the Endothelium. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 2608–2617. [Google Scholar] [CrossRef]
- Swartz, M.F.; Morrow, D.; Atallah-Yunes, N.; Cholette, J.M.; Gensini, F.; Kavey, R.E.; Alfieris, G.M. Hypertensive Changes within the Aortic Arch of Infants and Children with Isolated Coarctation. Ann. Thorac. Surg. 2013, 96, 190–195. [Google Scholar] [CrossRef]
- Ikeda, T.; Sun, L.; Tsuruoka, N.; Ishigaki, Y.; Yoshitomi, Y.; Yoshitake, Y.; Yonekura, H. Hypoxia Down-Regulates SFlt-1 (SVEGFR-1) Expression in Human Microvascular Endothelial Cells by a Mechanism Involving MRNA Alternative Processing. Biochem. J. 2011, 436, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Salhiyyah, K.; Sarathchandra, P.; Latif, N.; Yacoub, M.H.; Chester, A.H. Hypoxia-Mediated Regulation of the Secretory Properties of Mitral Valve Interstitial Cells. Am. J. Physiol. Circ. Physiol. 2017, 313, H14–H23. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, J.W.; Ko, J.; Ju, C.; Eltzschig, H.K. Hypoxia Signaling in Human Diseases and Therapeutic Targets. Exp. Mol. Med. 2019, 51, 1–13. [Google Scholar] [CrossRef] [PubMed]

| Normal Heart | Favorable Outcome Left-CHD (n = 29) | Poor Outcome Left-CHD (n = 16) | p | |
|---|---|---|---|---|
| (n = 35) | ||||
| Maternal baseline characteristics | ||||
| Maternal age (years) | 33.2 ± 5.2 | 31.9 ± 6.7 | 33.7 ± 5.6 | 0.567 |
| Maternal body mass index | 23.2 ± 3.2 | 25.6 ± 3.7 | 25.6 ± 5.4 | 0.095 |
| Nulliparity | 17 (48.6%) | 15 (51.7%) | 7 (43.8%) | 0.877 |
| Smoking | 4 (11.4%) | 4 (13.8%) | 1 (6.3%) | 0.745 |
| Pregestational diabetes | 0 (0%) | 0 (0%) | 0 (0%) | 1.000 |
| Standard Obstetrical Ultrasound | ||||
| Gestational age at scan (weeks) | 33.1 (29.6–35.1) | 33.1 (32.3–34.3) | 33.1 (32.3–34.3) | 0.646 |
| Female fetus | 14 (40%) | 15 (51.7%) | 6 (37.6%) | 0.548 |
| Estimated fetal weight (g) | 2011 ± 681 | 2037 ± 560 | 1918 ± 680 | 0.933 |
| Estimated fetal weight centile | 58.0 (27.0–76.0) | 32.5 (18.3–73.0) | 84.0 (43.0–86.5) | 0.132 |
| Intrauterine growth restriction | 0 (0%) | 2 (6.9%) | 0 (0%) | 0.165 |
| Umbilical artery PI | 1.0 (0.9–1.1) | 1.0 (0.8–1.3) | 1.0 (0.8–1.3) | 0.723 |
| Umbilical artery PI >95th centile | 0 (0%) | 1 (3.4%) | 0 (0%) | 0.410 |
| Median cerebral artery PI | 2.0 ± 0.4 | 1.8 ± 0.3 | 1.7 ± 0.1 | 0.087 |
| Median cerebral artery <5th centile | 1 (2.9%) | 1 (3.4%) | 0 (0%) | 0.765 |
| Cerebro-placental ratio | 2.0 ± 0.5 | 1.8 ± 0.4 | 1.8 ± 0.5 | 0.111 |
| Cerebro-placental ratio <5th centile | 2 (5.7%) | 2 (6.7%) | 0 (0%) | 0.577 |
| Mean Uterine Artery PI | 0.7 (0.5–0.8) | 0.9 (0.7–1.1) | 0.7 (0.7–0.9) | 0.074 |
| Mean Uterine Artery PI >95th centile | 1 (2.9%) | 5 (17.2%) | 0 (0%) | 0.042 |
| Perinatal Results | ||||
| Gestational age delivery (weeks) | 39.8 (38.6–40.5) | 39.7 (38.4–40.3) | 40.0 (39.5–40.0) | 0.723 |
| Cesarean section | 8 (22.8%) | 6 (21.4%) | 7 (63.6%) * | 0.019 |
| Spontaneous preterm birth < 37 weeks | 1 (2.9%) | 1 (3.4%) | 0 (0%) | 0.765 |
| Gestational diabetes | 3 (8.6%) | 3 (10.3%) | 2 (12.5%) | 0.907 |
| Preeclampsia | 0 (0%) | 1 (3.4%) | 1 (6.3%) | 0.381 |
| Birth weight (g) | 3256 ± 416 | 3173 ± 525 | 3275 ± 415 | 0.660 |
| Birth weight < 3rd centile | 0 (0%) | 2 (6.9%) | 0 (0%) | 0.165 |
| Birth weight > 4000 g | 0 (0%) | 1 (3.4%) | 0 (0%) | 0.410 |
| 5-min Apgar score < 7 | 0 (0%) | 1 (3.4%) | 0 (0%) | 0.410 |
| Umbilical artery pH | 7.22 (7.17–7.27) | 7.25 (7.18–7.27) | 7.26 (7.20–7.30) | 0.416 |
| Cardiovascular outcome | ||||
| Follow-up (years) | ------- | 3.1 (1.4–3.9) | ------- | |
| Univentricular circulation | ------- | ------- | 11 (68.8%) | ------- |
| Cardiac transplant | ------- | ------- | 1 (6.3%) | ------- |
| Death | ------- | ------- | 5 (31.3%) | ------- |
| Parameter | Normal Heart | Favorable Outcome | Poor Outcome | p |
|---|---|---|---|---|
| Left-CHD | Left-CHD | |||
| (n = 35) | (n = 29) | (n = 16) | ||
| Cardiac morphometric parameters | ||||
| Gestational age at scan (weeks) | 33.1 (29.6–35.1) | 33.1 (32.3–34.3) | 33.1 (32.3–34.3) | 0.646 |
| Cardio-thoracic ratio | 0.28 ± 0.04 | 0.30 ± 0.05 * | 0.32 ± 0.05 * | 0.002 |
| Cardiac sphericity index | 1.2 (1.1–1.3) | 1.2 (1.1–1.3) | 1.1 (1.0–1.3) | 0.087 |
| Left atrial-to-heart ratio | 0.15 ± 0.04 | 0.13 ± 0.03 * | 0.10 ± 0.03 * | <0.001 |
| Left ventricular-to-heart ratio † | 0.23 (0.19–0.28) | 0.15 (0.14–0.20) * | 0.11 (0.03–0.14) * | <0.001 |
| Right atria-to-heart ratio | 0.17 ± 0.05 | 0.20 ± 0.03 | 0.23 ± 0.08 * | 0.001 |
| Right ventricle-to-heart ratio | 0.23 (0.20–0.27) | 0.24 (0.21–0.26) | 0.29 (0.25–0.36) * | 0.016 |
| Right-to-left ventricular ratio (basal) | 1.0 (0.9–1.1) | 1.4 (1.3–1.7) * | 2.1 (1.9–3.7) * | <0.001 |
| Septal wall thickness (mm) | 3.1 (2.6–3.7) | 3.5 (3.0–4.1) | 3.6 (3.4–3.9) | 0.040 |
| Cardiac function parameters | ||||
| Heart rate | 141 (134–144) | 137 (131–145) | 140 (131–141) | 0.693 |
| Left ventricular Shortening Fraction ‡ | 36.7 ± 8.8 | 44.3 ± 12.9 * | 21.0 ± 11.2 * | <0.001 |
| Left filling time fraction ‡ | 43.2 ± 4.9 | 42.0 ± 3.6 | 41.2 ± 14.6 | 0.633 |
| Left ejection time fraction ‡ | 41.0 (338.9–43.4) | 42.1 (37.9–44.8) | 45.1 (38.4–64.6) | 0.282 |
| Right ventricular Fractional Area Change | 30.4 ± 8.4 | 30.7 ± 11.2 | 35.6 ± 10.6 | 0.371 |
| Right filling time fraction | 40.4 (37.6–43.9) | 42.3 (38.4–44.2) | 38.9 (35.4–43.4) | 0.480 |
| Right ejection time fraction | 42.6 ± 3.3 | 41.8 ± 3.8 | 43.0 ± 4.1 | 0.577 |
| Cord Blood Cardiovascular Biomarkers | Normal Heart | Favorable Outcome | Poor Outcome | p |
|---|---|---|---|---|
| Left-CHD | Left-CHD | |||
| (n = 35) | (n = 29) | (n = 16) | ||
| NT Pro-BNP (pg/mL) | 508.0 (287.5–776.3) | 617.0 (389.8–1087.8) | 1450.0 (919.0–1645.0) * | 0.001 |
| TroponinI (% positive) | 7/31 (22.6%) | 9/19 (47.4%) | 2/9 (22.2%) | 0.153 |
| TGFβ (ng/mL) | 15.0 (6.8–21.4) | 51.7 (13.8–73.9) * | 25.1 (6.9–39.0) | 0.001 |
| PlGF (pg/mL) | 17.9 (13.8–23.9) | 12.8 (11.7–13.6) * | 11.0 (8.8–15.4) * | <0.001 |
| sFlt1 (pg/mL) | 1929.7 (1364.3–2715.8) | 1848.3 (646.9–2313.6) | 259.0 (182.0–606.0) * | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soveral, I.; Guirado, L.; Escobar-Diaz, M.C.; Alcaide, M.J.; Martínez, J.M.; Rodríguez-Sureda, V.; Bijnens, B.; Antolin, E.; Llurba, E.; Bartha, J.L.; et al. Cord Blood Cardiovascular Biomarkers in Left-Sided Congenital Heart Disease. J. Clin. Med. 2022, 11, 7119. https://doi.org/10.3390/jcm11237119
Soveral I, Guirado L, Escobar-Diaz MC, Alcaide MJ, Martínez JM, Rodríguez-Sureda V, Bijnens B, Antolin E, Llurba E, Bartha JL, et al. Cord Blood Cardiovascular Biomarkers in Left-Sided Congenital Heart Disease. Journal of Clinical Medicine. 2022; 11(23):7119. https://doi.org/10.3390/jcm11237119
Chicago/Turabian StyleSoveral, Iris, Laura Guirado, Maria C. Escobar-Diaz, María José Alcaide, Josep Maria Martínez, Víctor Rodríguez-Sureda, Bart Bijnens, Eugenia Antolin, Elisa Llurba, Jose L. Bartha, and et al. 2022. "Cord Blood Cardiovascular Biomarkers in Left-Sided Congenital Heart Disease" Journal of Clinical Medicine 11, no. 23: 7119. https://doi.org/10.3390/jcm11237119
APA StyleSoveral, I., Guirado, L., Escobar-Diaz, M. C., Alcaide, M. J., Martínez, J. M., Rodríguez-Sureda, V., Bijnens, B., Antolin, E., Llurba, E., Bartha, J. L., Gómez, O., & Crispi, F. (2022). Cord Blood Cardiovascular Biomarkers in Left-Sided Congenital Heart Disease. Journal of Clinical Medicine, 11(23), 7119. https://doi.org/10.3390/jcm11237119







