Could Short Stems THA Be a Good Bone-Saving Option Even in Obese Patients?
Abstract
1. Introduction
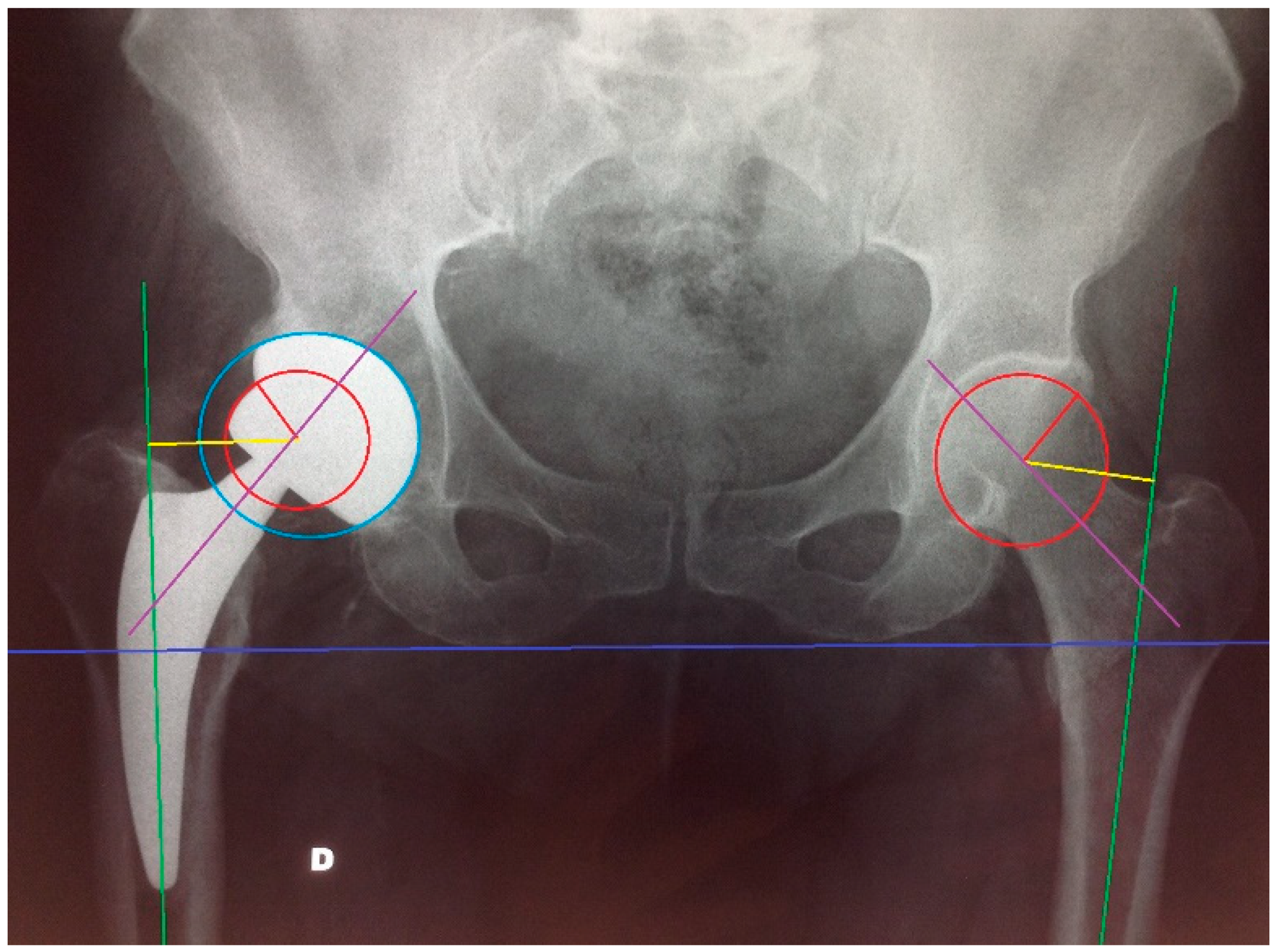
2. Materials and Methods
Statistical Analysis
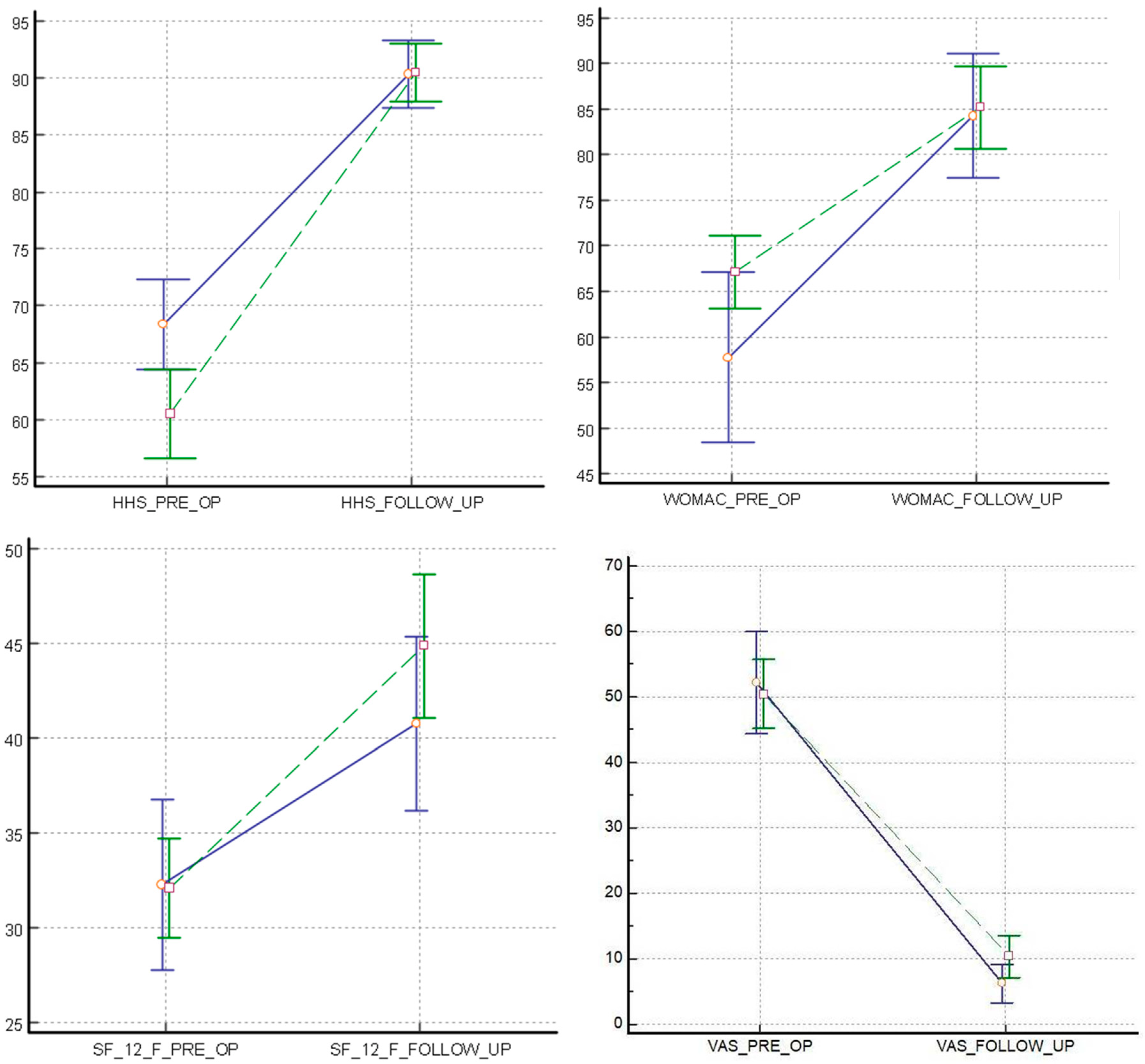
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- D’Errico, M.; Pavlova, M.; Spandonaro, F. The economic burden of obesity in Italy: A cost-of-illness study. Eur. J. Health Econ. 2022, 23, 177–192. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; He, C. Pro-inflammatory cytokines: The link between obesity and osteoarthritis. Cytokine Growth Factor Rev. 2018, 44, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Stihsen, C.; Radl, R.; Keshmiri, A.; Rehak, P.; Windhager, R. Subsidence of a cementless femoral component influenced by body 339 weight and body mass index. Int. Orthop. 2012, 36, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Anderl, C.; Steinmair, M.; Hochreiter, J. Bone Preservation in Total Hip Arthroplasty. J. Arthroplast. 2022, 37, 1118–1123. [Google Scholar] [CrossRef]
- Logroscino, G.; Ciriello, V.; D’Antonio, E.; De, T.V.; Piciocco, P.; Magliocchetti, L.G.; Santori, F.S.; Albanese, C.V. Bone integration of new stemless hip implants (proxima vs. nanos). A DXA study: Preliminary results. Int. J. Immunopathol. Pharmacol. 2011, 24, 113–116. [Google Scholar] [CrossRef]
- Rometsch, E.; Bos, P.K.; Koes, B.W. Survival of short hip stems with a “modern”, trochanter-sparing design—A systematic literature review. Hip Int. 2012, 22, 344–354. [Google Scholar] [CrossRef]
- Banerjee, S.; Pivec, R.; Issa, K.; Harwin, S.F.; Mont, M.A.; Khanuja, H.S. Outcomes of short stems in total hip arthroplasty. Orthopedics 2013, 36, 700–707. [Google Scholar] [CrossRef]
- Chammaï, Y.; Brax, M. Medium-term comparison of results in obese patients and non-obese hip prostheses 345 with Metha® short stem. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 503–508. [Google Scholar] [CrossRef]
- Hungerford, M.W.; Schuh, R.; O’Reilly, M.P.; Jones, L.C. Outcome of minimally invasive hip replacement in obese, 347 overweight, and nonobese patients. J. Surg. Orthop. Adv. 2014, 23, 68–74. [Google Scholar] [CrossRef]
- Feyen, H.; Shimmin, A.J. Is the length of the femoral component important in primary total hip replacement? Bone Jt. J. 2014, 96, 442–448. [Google Scholar] [CrossRef]
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Jt. Surg. Am. 1969, 51, 737–755. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar] [PubMed]
- Busija, L.; Pausenberger, E.; Haines, T.P.; Haymes, S.; Buchbinder, R.; Osborne, R.H. Adult measures of general health and health-related quality of life: Medical Outcomes Study Short Form 36-Item (SF-36) and Short Form 12-Item (SF-12) Health Surveys, Nottingham Health Profile (NHP), Sickness Impact Profile (SIP), Medical Outcomes Study Short Form 6D (SF-6D), Health Utilities Index Mark 3 (HUI3), Quality of Well-Being Scale (QWB), and Assessment of Quality of Life (AQoL). Arthritis Care Res. 2011, 63 (Suppl. 11), S383–S412. [Google Scholar] [CrossRef]
- Engh, C.A.; Massin, P.; Suthers, K.E. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin. Orthop. Relat. Res. 1990, 257, 107–128. [Google Scholar] [CrossRef]
- Gruen, T.; McNeice, G.; Amstutz, H.C. “Model of failure” of cemented stem-type femoral components. A radiographic analysis of loosening. Clin. Orthop. Relat. Res. 1979, 141, 17–27. [Google Scholar]
- Albanese, C.V.; Santori, F.S.; Pavan, L.; Learmonth, I.D.; Passariello, R. Periprosthetic DXA after total hip arthroplasty with short vs. ultra-short custom-made femoral stems: 37 patients followed for 3 years. Acta Orthop. 2009, 80, 291–297. [Google Scholar] [CrossRef]
- Logroscino, G.; Donati, F.; Campana, V.; Saracco, M. Stemless hip arthroplasty versus traditional implants: A comparative observational study at 30 months follow-up. Hip Int. 2018, 28 (Suppl. 2), 21–27. [Google Scholar] [CrossRef]
- Hodgkinson, J.P.; Shelley, P.; Wroblewski, B.M. The correlation between the roentgenographic appearance and operative findings at the bone-cement junction of the socket in Chanley lower friction arthroplasties. Clin. Orthop. Relat. Res. 1988, 228, 105–109. [Google Scholar] [CrossRef]
- DeLee, J.G.; Charnley, J. Radiological demarcation of cemented sockets in total hip replacement. Clin. Orthop. Relat. Res. 1976, 121, 20–32. [Google Scholar] [CrossRef]
- Brooker, A.F.; Bowerman, J.W. Ectopic ossification following total hip replacement. J. Bone Jt. Surg. Am. 1973, 55, 1629–1632. [Google Scholar] [CrossRef]
- Lementowski, P.W.; Zelicof, S.B. Obesity and osteoarthritis. Am. J. Orthop. 2008, 37, 148–151. [Google Scholar] [PubMed]
- Wendelboe, A.M.; Hegmann, K.T.; Biggs, J.J.; Cox, C.M.; Portmann, A.J.; Gildea, J.H.; Gren, L.H.; Lyon, J.L. Relationships between body mass indices and surgical replacements of knee and hip joints. Am. J. Prev. Med. 2003, 25, 290–295. [Google Scholar] [PubMed]
- Muehleman, C.; Margulis, A.; Bae, W.C.; Masuda, K. Relationship between knee and ankle degeneration in a population of organ donors. BMC Med. 2010, 8, 48. [Google Scholar] [CrossRef] [PubMed]
- Horan, F. Obesity and joint replacement. J. Bone Jt. Surg. 2006, 88, 1269–1271. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, J.R.; Lee, K.R. The outcome of total hip replacement in obese and nonobese patients at 10- to 18-years. J. Bone Jt. Surg. 2006, 88, 1286–1292. [Google Scholar] [CrossRef]
- Jiganti, J.J.; Goldstein, W.M.; Williams, C.S. A comparison of the perioperative morbidity in total joint arthroplasty in the obese and nonobese patient. Clin. Orthop. 1993, 289, 175–179. [Google Scholar] [CrossRef]
- Jackson, M.P.; Sexton, S.A.; Yeung, E.; Walter, W.L.; Walter, W.K.; Zicat, B.A. The effect of obesity on the mid-term survival and clinical outcome of cementless total hip replacement. J. Bone Jt. Surg. Br. 2009, 91, 1296–1300. [Google Scholar] [CrossRef]
- Michalka, P.K.; Khan, R.J.; Scaddan, M.C.; Haebich, S.; Chirodian, N.; Wimhurst, J.A. The influence of obesity on early outcomes in primary hip arthroplasty. J. Arthroplast. 2012, 27, 391–396. [Google Scholar]
- Kim, Y.; Morshed, S.; Joseph, T.; Bozic, K.; Ries, M.D. Clinical impact of obesity on stability following revision total hip arthroplasty. Clin. Orthop. 2006, 453, 142–146. [Google Scholar] [CrossRef]
- Pipino, F.; Keller, A. Tissue-sparing surgery: 25 years experience with femoral neck preserving hip arthroplasty. J. Orthop. Traumatol. 2006, 7, 36–41. [Google Scholar] [CrossRef]
- Lübbeke, A.; Stern, R.; Garavaglia, G.; Zurcher, L.; Hoffmeyer, P. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Rheum 2007, 57, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, T.; Hobson, S.; Beiri, A.; Esler, C.N. No influence of body mass index on early outcome following total hip arthroplasty. Int. Orthop. 2005, 29, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Pirard, E.; De Lint, J.A. Anteversion of the acetabular component in obese patients. Hip Int. 2007, 17, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Todkar, M. Obesity does not necessarily affect the accuracy of acetabular cup implantation in total hip replacement. Acta Orthop. Belg. 2008, 74, 206–209. [Google Scholar] [PubMed]
- Bosker, B.H.; Verheyen, C.C.P.M.; Horstmann, W.G.; Tulp, N.J.A. Poor accuracy of freehand cup positioning during total hip arthroplasty. Arch. Orthop. Trauma Surg. 2007, 127, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Callanan, M.C.; Jarrett, B.; Bragdon, C.R.; Zurakowski, D.; Rubash, H.E.; Freiberg, A.A.; Malchau, H. The John Charnley Award: Risk factors for cup malpositioning: Quality improvement through a joint registry at a tertiary hospital. Clin. Orthop. Relat. Res. 2011, 469, 319–329. [Google Scholar] [CrossRef]
- Elson, L.C.; Barr, C.J.; Chandran, S.E.; Hansen, V.J.; Malchau, H.; Kwon, Y.M. Are morbidly obese patients undergoing total hip arthroplasty at an increased risk for component malpositioning? J. Arthroplast. 2013, 28, 41–44. [Google Scholar] [CrossRef]
- Tai, S.M.; Imbuldeniya, A.M.; Munir, S.; Walter, W.L.; Walter, W.K.; Zicat, B.A. The effect of obesity on the clinical, functional and radiological outcome of cementless total hip replacement: A case-matched study with a minimum 10-year follow-up. J. Arthroplast. 2014, 29, 1758–1762. [Google Scholar] [CrossRef]
- Brodt, S.; Jacob, B.; Windisch, C.; Seeger, J.; Matziolis, G. Morbidly Obese Patients Undergoing Reduced Cup Anteversion Through a Direct LateralApproach. J. Bone Jt. Surg. Am. 2016, 98, 729–734. [Google Scholar] [CrossRef][Green Version]
- Culliford, D.; Maskell, J.; Judge, A.; Arden, N.K.; COAST Study Group. A population-based survival analysis describing the association of body mass Index on time to revision for total hip and knee replacements: Results from the UK general practice research database. BMJ Open 2013, 3, e003614. [Google Scholar] [CrossRef]
- Braud, P.; Freeman, M.A. The effect of retention of the femoral neck and of cement upon the stability of proximal femoral prosthesis. J. Arthroplast. 1990, 5, S5–S10. [Google Scholar] [CrossRef] [PubMed]
- Freitag, T.; Kappe, T.; Fuchs, M.; Jung, S.; Reichel, H.; Bieger, R. Migration pattern of a femoral short-stem prosthesis: A 2-year ERBA-FCA-study. Arch. Orthop. Trauma Surg. 2014, 134, 1003–1008. [Google Scholar] [CrossRef] [PubMed]
- Andrew, J.G.; Palan, J.; Kurup, H.V.; Gibson, P.; Murray, D.W.; Beard, D.J. Obesity in total hip replacement. J. Bone Jt. Surg. Br. 2008, 90, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Wattanakit, K.; Lutsey, P.L.; Bell, E.J.; Gornik, H.; Cushman, M.; Heckbert, S.R.; Heckbert, S.R.; Folsom, A.R. Association between cardiovascular disease risk factors and occurrence of venous thromboembolism. A time-dependent analysis. Thromb. Haemost. 2012, 108, 508–515. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Friedman, R.J.; Hess, S.; Berkowitz, S.D.; Homering, M. Complication rates after hip or knee arthroplasty in morbidly obese patients. Clin. Orthop. Relat. Res. 2013, 471, 3358–3366. [Google Scholar] [CrossRef] [PubMed]
- Fidanza, A.; Schettini, I.; Palozzi, G.; Mitrousias, V.; Logroscino, G.; Romanini, E.; Calvisi, V. What Is the Inpatient Cost of Hip Replacement? A Time-Driven Activity Based Costing Pilot Study in an Italian Public Hospital. J. Clin. Med. 2022, 11, 6928. [Google Scholar] [CrossRef]
- Nadzadi, M.E.; Pedersen, D.R.; Yack, H.J.; Callaghan, J.J.; Brown, T.D. Kinematics, kinetics, and finite element analysis of commonplace maneuvers at risk for total hip dislocation. J. Biomech. 2003, 36, 577–591. [Google Scholar] [CrossRef]
- Liu, W.; Wahafu, T.; Cheng, M.; Cheng, T.; Zhang, Y.; Zhang, X. The influence of obesity on primary total hip arthroplasty outcomes: A meta-analysis of prospective cohort studies. Orthop. Traumatol. Surg. Res. 2015, 101, 289–296. [Google Scholar] [CrossRef]
- Elkins, J.M.; Stroud, N.J.; Rudert, M.J.; Tochigi, Y.; Pedersen, D.R.; Ellis, B.J.; Callaghan, J.J.; Weiss, J.A.; Brown, T.D. The capsule’s contribution to total hip construct stability: A finite element analysis. J. Orthop. Res. 2011, 29, 1642–1648. [Google Scholar] [CrossRef]
- Pulido, L.; Ghanem, E.; Joshi, A.; Purtill, J.J.; Parvizi, J. Periprosthetic joint infection: The incidence, timing, and predisposing factors. Clin. Orthop. Relat. Res. 2008, 466, 1710–1715. [Google Scholar] [CrossRef]
- Iannotti, F.; Prati, P.; Fidanza, A.; Iorio, R.; Ferretti, A.; Pèrez Prieto, D.; Kort, N.; Violante, B.; Pipino, G.; Schiavone Panni, A.; et al. Prevention of Periprosthetic Joint Infection (PJI): A Clinical Practice Protocol in High-Risk Patients. Trop. Med. Infect. Dis. 2020, 5, 186. [Google Scholar] [CrossRef] [PubMed]
- Moran, M.; Walmsley, P.; Gray, A.; Brenkel, I.J. Does body mass index affect the early outcome of primary total hip arthroplasty? J. Arthroplast. 2005, 20, 866–869. [Google Scholar] [CrossRef] [PubMed]
- Dowsey, M.M.; Choong, P.F. Obesity is a major risk factor for prosthetic infection after primary hip arthroplasty. Clin. Orthop. Relat Res. 2008, 466, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Zmistowski, B.; Tetreault, M.W.; Alijanipour, P.; Chen, A.F.; Della Valle, C.J.; Parvizi, J. Recurrent periprosthetic joint infection: Persistent or new infection? J. Arthroplast. 2013, 28, 1486–1489. [Google Scholar] [CrossRef]
- Patel, V.P.; Walsh, M.; Sehgal, B.; Preston, C.; DeWal, H.; Di Cesare, P.E. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J. Bone Jt. Surg. 2007, 89, 33–38. [Google Scholar] [CrossRef]
- Cordero-Ampuero, J.; De Dios, M. What are the risk factors for infection in hemiarthroplasties and total hip arthroplasties? Clin. Orthop. Relat. Res. 2010, 468, 3268–3277. [Google Scholar] [CrossRef]
- Baek, S.H. Identification and preoperative optimization of risk factors to prevent periprosthetic joint infection. World J. Orthop. 2014, 5, 362–367. [Google Scholar] [CrossRef]
- Belmont, P.J., Jr.; Goodman, G.P.; Hamilton, W.; Waterman, B.R.; Bader, J.O.; Schoenfeld, A.J. Morbidity and mortality in the thirty-day period following total hip arthroplasty: Risk factors and incidence. J. Arthroplast. 2014, 29, 2025–2030. [Google Scholar] [CrossRef]
- Watts, C.D.; Houdek, M.T.; Wagner, E.R.; Sculco, P.K.; Chalmers, B.P.; Taunton, M.J. High Risk of Wound Complications Following Direct Anterior Total Hip Arthroplasty in Obese Patients. J. Arthroplast. 2015, 30, 2296–2298. [Google Scholar] [CrossRef]
| Short Stems (SS) | Traditional Stems (TS) | |
|---|---|---|
| AGE, years | 63 (43–84) ± 10.05 | 67 (50–88) ± 10.03 |
| BMI, Kg/m2 | 33.5 (30.1–41.3) ± 3.07 | 34.7 (29.8–44.5) ± 4.68 |
| WEIGHT, Kg | 92.3 (75–113) ± 10.39 | 95.9 (67–130) ± 17.89 |
| FOLLOW-UP, months | 38 (3–120) ± 25.98 | 47.3 (12–168) ± 43.15 |
| PARVA, Adler | 20 (40%) | - |
| PROXIMA, DePuy-J&J | 7 (16%) | - |
| MINIMA, Lima | 7 (16%) | - |
| FITMORE, Zimmer Biomet | 4 (10%) | - |
| PULCHRA, Adler | 3 (6%) | - |
| SMF, S&N | 3 (6%) | - |
| GTS, Zimmer Biomet | 2 (3%) | - |
| NANOS, S&N | 2 (3%) | - |
| ABG, Stryker | - | 9 (59%) |
| SYNERGY, S&N | - | 6 (17%) |
| MERCURIUS, Adler | - | 5 (12%) |
| HYDRA, Adler | - | 4 (6%) |
| CORAIL, DePuy-J&J | - | 4 (6%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saracco, M.; Fidanza, A.; Necozione, S.; Maccauro, G.; Logroscino, G. Could Short Stems THA Be a Good Bone-Saving Option Even in Obese Patients? J. Clin. Med. 2022, 11, 7114. https://doi.org/10.3390/jcm11237114
Saracco M, Fidanza A, Necozione S, Maccauro G, Logroscino G. Could Short Stems THA Be a Good Bone-Saving Option Even in Obese Patients? Journal of Clinical Medicine. 2022; 11(23):7114. https://doi.org/10.3390/jcm11237114
Chicago/Turabian StyleSaracco, Michela, Andrea Fidanza, Stefano Necozione, Giulio Maccauro, and Giandomenico Logroscino. 2022. "Could Short Stems THA Be a Good Bone-Saving Option Even in Obese Patients?" Journal of Clinical Medicine 11, no. 23: 7114. https://doi.org/10.3390/jcm11237114
APA StyleSaracco, M., Fidanza, A., Necozione, S., Maccauro, G., & Logroscino, G. (2022). Could Short Stems THA Be a Good Bone-Saving Option Even in Obese Patients? Journal of Clinical Medicine, 11(23), 7114. https://doi.org/10.3390/jcm11237114







