Impact of Frailty Risk on Adverse Outcomes after Traumatic Brain Injury: A Historical Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Data Source
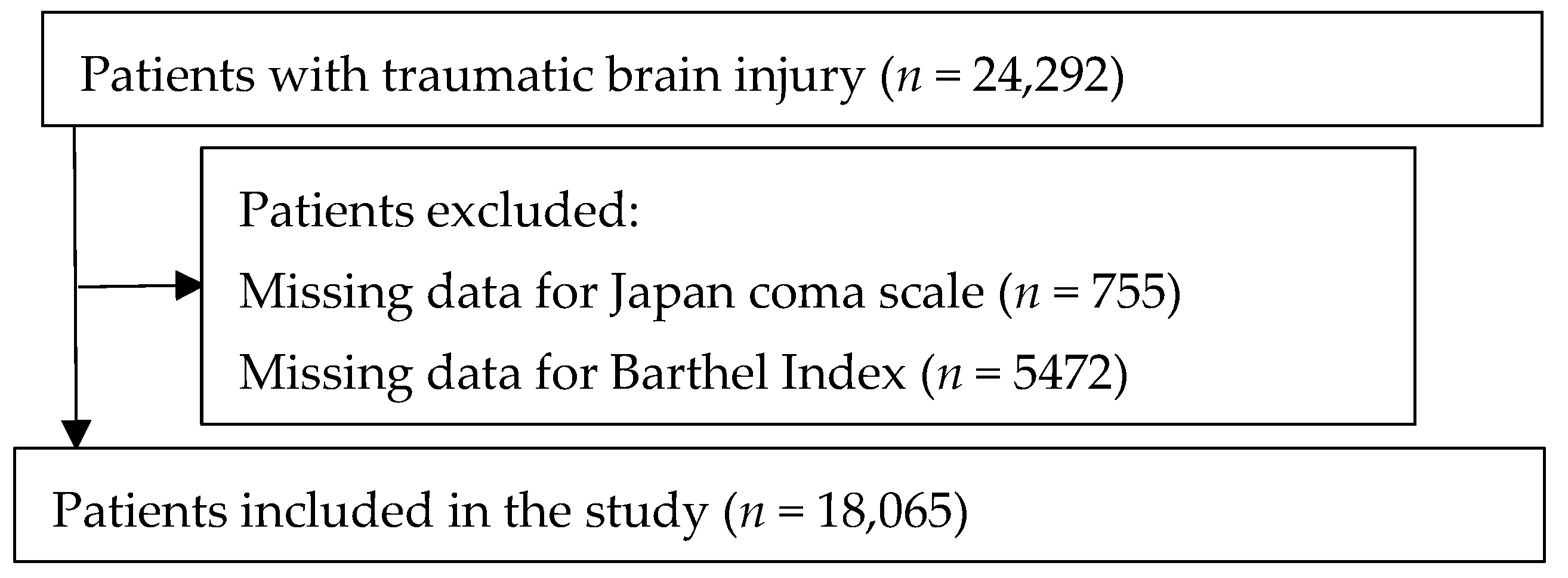
2.3. Study Population
2.4. Calculation of HFRS
2.5. Variables and Outcomes
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rodriguez, S.R.; Mallonee, S.; Archer, P.; Gofton, J. Evaluation of death certificate-based surveillance for traumatic brain injury–Oklahoma 2002. Public Health Rep. 2006, 121, 282–289. [Google Scholar] [CrossRef]
- Faul, M.; Wald, M.M.; Rutland-Brown, W.; Sullivent, E.E.; Sattin, R.W. Using a cost-benefit analysis to estimate outcomes of a clinical treatment guideline: Testing the Brain Trauma Foundation guidelines for the treatment of severe traumatic brain injury. J. Trauma 2007, 63, 1271–1278. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. National Center for Health Statistics: Mortality Data on CDC WONDER. Available online: https://wonder.cdc.gov (accessed on 21 May 2022).
- Surveillance Report of Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths; Centers for Disease Control and Prevention, U.S. Department of Health and Human Services: Atlanta, Georgia, 2014. Available online: https://www.cdc.gov/traumaticbraininjury/pdf/TBI-Surveillance-Report-FINAL_508.pdf (accessed on 21 May 2022).
- Vaishya, R.; Vaish, A. Falls in older adults are serious. Indian J. Orthop. 2020, 54, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Langlois, J.A.; Rutland-Brown, W.; Thomas, K.E. Traumatic Brain Injury in the United States Emergency Department Visits, Hospitalizations, and Deaths; Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: Atlanta, GA, USA, 2006. Available online: https://www.cdc.gov/traumaticbraininjury/tbi_ed.html (accessed on 21 May 2022).
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Guilherme, G.P.G.; Rodrigo, C.; Edson, L.Z.J.; Luca, G.; Mateus, M.; Stephanie, N.D.S.; Marcelo, V.S. Traumatic brain injury in the elderly: Clinical features, prognostic factors, and outcomes of 133 consecutive surgical patients. Cureus 2021, 27, e13587. [Google Scholar]
- Gilbert, T.; Neuburger, J.; Kraindler, J.; Keeble, E.; Smith, P.; Ariti, C.; Arora, S.; Street, A.; Parker, S.; Roberts, H.C.; et al. Development and validation of a hospital frailty risk score focusing on older people in acute care settings using electronic hospital records: An observational study. Lancet 2018, 391, 1775–1782. [Google Scholar] [CrossRef] [PubMed]
- McAlister, F.; Walraven, C.V. External validation of the hospital frailty risk score and comparison to the hospital-patient one-year mortality risk score to predict outcomes in elderly hospitalized patients: A retrospective cohort study. BMJ Qual. Saf. 2019, 28, 284–288. [Google Scholar] [CrossRef]
- Galimberti, S.; Graziano, F.; Maas, A.I.R.; Isernia, G.; Lecky, F.; Jain, S.; Sun, X.; Gardner, R.C.; Taylor, S.R.; Markowitz, A.J. CENTER-TBI and TRACK-TBI participants and investigators. Effect of frailty on 6-month outcome after traumatic brain injury: A multicentre cohort study with external validation. Lancet Neuro. 2022, 21, 153–162. [Google Scholar] [CrossRef]
- Tang, O.Y.; Shao, B.; Kimata, A.R.; Sastry, R.A.; Wu, J.; Asaad, W.F. The impact of frailty on traumatic brain injury outcomes: An analysis of 691,821 nationwide cases. Neurosurgery 2022, 91, 808–820. [Google Scholar] [CrossRef]
- Abdulle, A.E.; de Koning, M.E.; van der Horn, H.J.; Scheenen, M.E.; Roks, G.; Hageman, G.; Spikman, J.M.; van der Naalt, J. Early predictors for long-term functional outcome after mild traumatic brain injury in frail elderly patients. J. Head Trauma Rehabil. 2018, 33, E59–E67. [Google Scholar] [CrossRef]
- Tracy, B.M.; Carlin, M.N.; Tyson, J.W.; Schenker, M.L.; Gelbard, R.B. The 11-item modified frailty index as a tool to predict unplanned events in traumatic brain injury. Am. Surg. 2020, 86, 1596–1601. [Google Scholar] [CrossRef] [PubMed]
- Lascano, D.; Pak, J.S.; Kates, M.; Finkelstein, J.B.; Silva, M.; Hagen, E.; RoyChoudhury, A.; Bivalacque, T.J. Validation of a frailty index in patients undergoing curative surgery for urologic malignancy and comparison to other risk stratification tools. Urol. Oncol. 2015, 33, 426.e1–426.e12. [Google Scholar] [CrossRef] [PubMed]
- Kimura, S.; Sato, T.; Ikeda, S.; Noda, M.; Nakayama, T. Development of a database of health insurance claims: Standardization of disease classifications and anonymous record linkage. J. Epidemiol. 2010, 20, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Nagai, K.; Tanaka, T.; Kodaira, N.; Kimura, S.; Takahashi, Y.; Nakayama, T. Data resource profile: JMDC claims databases sourced from medical institutions. J. Gen. Fam. Med. 2020, 21, 211–218. [Google Scholar] [CrossRef]
- JMDC Claims Database. Japan Medical Data Center. Available online: https://www.jmdc.co.jp/en/jmdc-claims-database (accessed on 21 May 2022).
- Yasunaga, H.; Ide, H.; Imamura, T.; Ohe, K. Impact of the Japanese diagnosis procedure combination-based payment system on cardiovascular medicine-related costs. Int. Heart J. 2005, 46, 855–866. [Google Scholar] [CrossRef]
- Yamana, H.; Moriwaki, M.; Horiguchi, H.; Kodan, M.; Fushimi, K.; Yasunaga, H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J. Epidemiol. 2017, 27, 476–482. [Google Scholar] [CrossRef]
- Yumoto, T.; Naito, H.; Yorifuji, T.; Aokage, T.; Fujisaki, N.; Nakao, A. Association of Japan coma scale score on hospital arrival with in-hospital mortality among trauma patients. BMC Emerg. Med. 2019, 19, 65. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Gilbert, T.; Cordier, Q.; Polazzi, S.; Bonnefoy, M.; Keeble, E.; Street, A.; Conroy, S.; Duclos, A. External validation of the hospital frailty risk score in France. Age Ageing 2022, 51, afab126. [Google Scholar] [CrossRef]
- Kilkenny, M.F.; Phan, H.T.; Lindley, R.I.; Kim, J.; Lopez, D.; Dalli, L.L.; Grimley, R.; Sundararajan, V.; Thrift, A.G.; Andrew, N.E.; et al. Stroke123 Investigators and the AuSCR Consortium Utility of the hospital frailty risk score derived from administrative data and the association with stroke outcomes. Stroke 2021, 52, 2874–2881. [Google Scholar] [CrossRef]
- Shimizu, A.; Maeda, K.; Fujishima, I.; Kayashita, J.; Mori, N.; Okada, K.; Uno, C.; Shimizu, M.; Momosaki, R. Hospital frailty risk score predicts adverse events in older patients with hip fractures after surgery: Analysis of a nationwide inpatient database in Japan. Arch. Gerontol. Geriatr. 2022, 98, 104552. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.; Parik, L.; Leiß, F.; Renkawitz, T.; Grifka, J.; Weber, M. Hospital frailty risk score predicts adverse events in primary total hip and knee arthroplasty. J. Arthroplast. 2020, 35, 3498–3504.e3. [Google Scholar] [CrossRef] [PubMed]
- Hannah, T.C.; Neifert, S.N.; Caridi, J.M.; Martini, M.L.; Lamb, C.; Rothrock, R.J.; Yuk, F.J.; Gilligan, J.; Genadry, L.; Gal, J.S. Utility of the hospital frailty risk score for predicting adverse outcomes in degenerative spine surgery cohorts. Neurosurgery 2020, 87, 1223–1230. [Google Scholar] [CrossRef] [PubMed]
- Ushida, K.; Shimizu, A.; Hori, S.; Yamamoto, Y.; Momosaki, R. Hospital frailty risk score predicts outcomes in chronic obstructive pulmonary disease exacerbations. Arch. Gerontol. Geriatr. 2022, 100, 104658. [Google Scholar] [CrossRef]
- McAlister, F.A.; Savu, A.; Ezekowitz, J.A.; Armstrong, P.W.; Kaul, P. The hospital fraily risk score in patients with heart failure is strongly associated with outcomes but less so with pharmacotherapy. J. Intern. Med. 2022, 287, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Tuty Kuswardhani, R.A.; Henrina, J.; Pranata, R.; Anthonius Lim, M.; Lawrensia, S.; Suastika, K. Charlson comorbidity index and a composite of poor outcomes in COVID-19 patients: A systematic review and meta-analysis. Diabetes Metab. Syndr. 2020, 14, 2103–2109. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; Mackenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Baggiani, M.; Guglielmi, A.; Citerio, G. Acute traumatic brain injury in frail patients: The next pandemic. Curr. Opin. Crit. Care 2022, 28, 166–175. [Google Scholar] [CrossRef]
- Rehabilitation of persons with traumatic brain injury. NIH Consens. Statement 1998, 26–28, 1–41.
- Andriessen, T.M.; Horn, J.; Franschman, G.; van der Naalt, J.V.D.; Haitsma, I.; Jacobs, B.; Steyerberg, E.W.; Vos, P.E. Epidemiology, severity classification, and outcome of moderate and severe traumatic brain injury: A prospective multicenter study. J. Neurotrauma 2011, 28, 2019–2031. [Google Scholar] [CrossRef]
- Vitaz, T.W.; Jenks, J.; Raque, G.H.; Shields, C.B. Outcome following moderate traumatic brain injury. Surg. Neurol. 2003, 60, 285–291, discussion 291. [Google Scholar] [CrossRef] [PubMed]
- Persico, I.; Cesari, M.; Morandi, A.; Haas, J.; Mazzola, P.; Zambon, A.; Annoni, G.; Bellelli, G. Frailty and delirium in older adults: A systematic review and meta-analysis of the literature. J. Am. Geriatr. Soc. 2018, 66, 2022–2030. [Google Scholar] [CrossRef] [PubMed]
- Layton, A.M.; Armstrong, H.F.; Baldwin, M.R.; Podolanczuk, A.J.; Pieszchata, N.M.; Singer, J.P.; Arcasoy, S.M.; Meza, K.S.; D’Ovidio, F.; Lederer, D.J. Frailty and maximal exercise capacity in adult lung transplant candidates. Respir. Med. 2017, 131, 70–76. [Google Scholar] [CrossRef]
- Rabinstein, A.A. Administrative medical databases for clinical research: The good, the bad, and the ugly. Neurocrit. Care 2018, 29, 323–325. [Google Scholar] [CrossRef]
- Hashimoto, R.E.; Brodt, E.D.; Skelly, A.C.; Dettori, J.R. Administrative database studies: Goldmine or goose chase? Evid.-Based Spine Care J. 2014, 5, 74–76. [Google Scholar] [PubMed]
| Low-Frailty Risk Group (Hospital Frailty Risk Score < 5) | Intermediate-Frailty Risk Group (Hospital Frailty Risk Score 5–15) | High-Frailty Risk Group (Hospital Frailty Risk Score > 15) | p-Value | |
|---|---|---|---|---|
| Number of patients, n (%) | 10,139 (56.1) | 7388 (40.9) | 538 (3.0) | |
| Female sex, n (%) | 3607 (35.6) | 2944 (39.8) | 292 (54.3) | <0.001 |
| Age, years, n (%) | <0.001 | |||
| -<65 | 2444 (24.1) | 1384 (18.7) | 8 (1.5) | |
| -65–74 | 2214 (21.8) | 1397 (18.9) | 34 (6.3) | |
| -75–89 | 4418 (43.6) | 3608 (48.8) | 375 (69.7) | |
| -≥90 | 1063 (10.5) | 999 (13.5) | 121 (22.5) | |
| Body mass index, n (%) | <0.001 | |||
| -<18.5 | 1742 (17.2) | 1498 (20.3) | 158 (29.4) | |
| -18.5–25.0 | 5517 (54.4) | 3861 (52.3) | 241 (44.8) | |
| -≥25.0 | 1680 (16.6) | 1082 (14.6) | 55 (10.2) | |
| -Missing | 1200 (11.8) | 947 (12.8) | 84 (15.6) | |
| Injury type, n (%) | <0.001 | |||
| -Diffuse traumatic brain injury | 907 (8.9) | 712 (9.6) | 42 (7.8) | |
| -Focal traumatic brain injury | 301 (3.0) | 208 (2.8) | 12 (2.2) | |
| -Epidural hemorrhage | 363 (3.6) | 261 (3.5) | 13 (2.4) | |
| -Traumatic subdural hemorrhage | 5549 (54.7) | 3671 (49.7) | 340 (63.2) | |
| -Traumatic subarachnoid hemorrhage | 1923 (19.0) | 1597 (21.6) | 98 (18.2) | |
| -Other injury type | 1096 (10.8) | 939 (12.7) | 33 (6.1) | |
| Neurosurgical procedure on admission, n (%) | 3248 (32.0) | 1706 (23.1) | 169 (31.4) | <0.001 |
| Ventilator on admission, n (%) | 340 (3.4) | 495 (6.7) | 30 (5.6) | <0.001 |
| Intensive care unit management on admission, n (%) | 929 (9.2) | 925 (12.5) | 67 (12.5) | <0.001 |
| Japan coma scale at admission, n (%) | <0.001 | |||
| -0 | 4960 (48.9) | 2545 (34.4) | 118 (21.9) | |
| -1–3 | 3934 (38.8) | 3438 (46.5) | 304 (56.5) | |
| -10–30 | 659 (6.5) | 765 (10.4) | 75 (13.9) | |
| -100–300 | 586 (5.8) | 640 (8.7) | 41 (7.6) | |
| Barthel index at admission, mean (SD) | 47.7 ± 40.8 | 33.9 ± 38.1 | 19.3 ± 29.7 | <0.001 |
| Received inpatient rehabilitation services, n (%) | 5150 (50.8) | 4489 (60.8) | 423 (78.6) | <0.001 |
| Number of drugs during hospitalization, mean (SD) | 4.4 (4.5) | 5.9 (5.2) | 7.5 (5.3) | 0.004 |
| Number of complications occurring during hospitalization, mean (SD) | 0.5 (1.0) | 1.5 (1.8) | 2.4 (2.3) | <0.001 |
| Number of beds, n (%) | <0.001 | |||
| -20–99 | 186 (1.8) | 98 (1.3) | 8 (1.5) | |
| -100–199 | 2436 (24.0) | 1334 (18.1) | 131 (24.3) | |
| -200–299 | 1650 (16.3) | 1196 (16.2) | 120 (22.3) | |
| -300–499 | 2987 (29.5) | 2664 (36.1) | 165 (30.7) | |
| -≥500 | 2880 (28.4) | 2096 (28.4) | 114 (21.2) | |
| Year of admission, n (%) | <0.001 | |||
| -2014 | 858 (8.5) | 534 (7.2) | 24 (4.5) | |
| -2015 | 1308 (12.9) | 810 (11.0) | 36 (6.7) | |
| -2016 | 1498 (14.8) | 1148 (15.5) | 77 (14.3) | |
| -2017 | 1650 (16.3) | 1292 (17.5) | 108 (20.1) | |
| -2018 | 2004 (19.8) | 1412 (19.1) | 119 (22.1) | |
| -2019 | 1908 (18.8) | 1441 (19.5) | 120 (22.3) | |
| -2020 | 913 (9.0) | 751 (10.2) | 54 (10.0) |
| Low-Frailty Risk Group (Hospital Frailty Risk Score < 5) | Intermediate-Frailty Risk Group (Hospital Frailty Risk Score 5–15) | High-Frailty Risk Group (Hospital Frailty Risk Score > 15) | p-Value | |
|---|---|---|---|---|
| Length of hospital stay, Mean ± SD | 16.6 ± 27.9 | 25.0 ± 35.9 | 36.1 ± 42.9 | <0.001 |
| Barthel Index score ≥ 95 on discharge, n (%) | 6034 (59.5) | 2950 (39.9) | 59 (11.0) | <0.001 |
| Barthel index gain, Mean ± SD | 26.9 ± 37.4 | 25.1 ±38.2 | 14.0 ± 30.5 | <0.001 |
| Death in hospital, n (%) | 655 (6.5) | 640 (8.7) | 40 (7.4) | <0.001 |
| Variables | Coefficient | 95% Confidence Interval | p-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Length of hospital stay | ||||
| Low-frailty risk group (reference) | - | - | - | |
| Intermediate-frailty risk group | 1.952 | 1.117 | 2.786 | <0.001 |
| High-frailty risk group | 5.770 | 3.160 | 8.379 | <0.001 |
| Barthel index gain | ||||
| Low-frailty risk group (reference) | - | - | - | |
| Intermediate-frailty risk group | −4.868 | −5.599 | −3.773 | <0.001 |
| High-frailty risk group | −19.596 | −22.242 | −16.714 | <0.001 |
| Variables | Odds Ratio | 95% Confidence Interval | p-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Barthel Index score ≥ 95 on discharge | ||||
| Low-frailty risk group (reference) | - | - | - | |
| Intermediate-frailty risk group | 0.645 | 0.595 | 0.699 | <0.001 |
| High-frailty risk group | 0.221 | 0.157 | 0.311 | <0.001 |
| Death in hospital | ||||
| Low-frailty risk group (reference) | - | - | - | |
| Intermediate-frailty risk group | 0.901 | 0.766 | 1.061 | 0.690 |
| High-frailty risk group | 0.707 | 0.459 | 1.091 | 0.245 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, Y.; Hori, S.; Ushida, K.; Shirai, Y.; Shimizu, M.; Kato, Y.; Shimizu, A.; Momosaki, R. Impact of Frailty Risk on Adverse Outcomes after Traumatic Brain Injury: A Historical Cohort Study. J. Clin. Med. 2022, 11, 7064. https://doi.org/10.3390/jcm11237064
Yamamoto Y, Hori S, Ushida K, Shirai Y, Shimizu M, Kato Y, Shimizu A, Momosaki R. Impact of Frailty Risk on Adverse Outcomes after Traumatic Brain Injury: A Historical Cohort Study. Journal of Clinical Medicine. 2022; 11(23):7064. https://doi.org/10.3390/jcm11237064
Chicago/Turabian StyleYamamoto, Yoshinori, Shinsuke Hori, Kenta Ushida, Yuka Shirai, Miho Shimizu, Yuki Kato, Akio Shimizu, and Ryo Momosaki. 2022. "Impact of Frailty Risk on Adverse Outcomes after Traumatic Brain Injury: A Historical Cohort Study" Journal of Clinical Medicine 11, no. 23: 7064. https://doi.org/10.3390/jcm11237064
APA StyleYamamoto, Y., Hori, S., Ushida, K., Shirai, Y., Shimizu, M., Kato, Y., Shimizu, A., & Momosaki, R. (2022). Impact of Frailty Risk on Adverse Outcomes after Traumatic Brain Injury: A Historical Cohort Study. Journal of Clinical Medicine, 11(23), 7064. https://doi.org/10.3390/jcm11237064







