Relationship between Periodontal Condition of the Pregnant Woman with Preterm Birth and Low Birth Weight
Abstract
1. Introduction
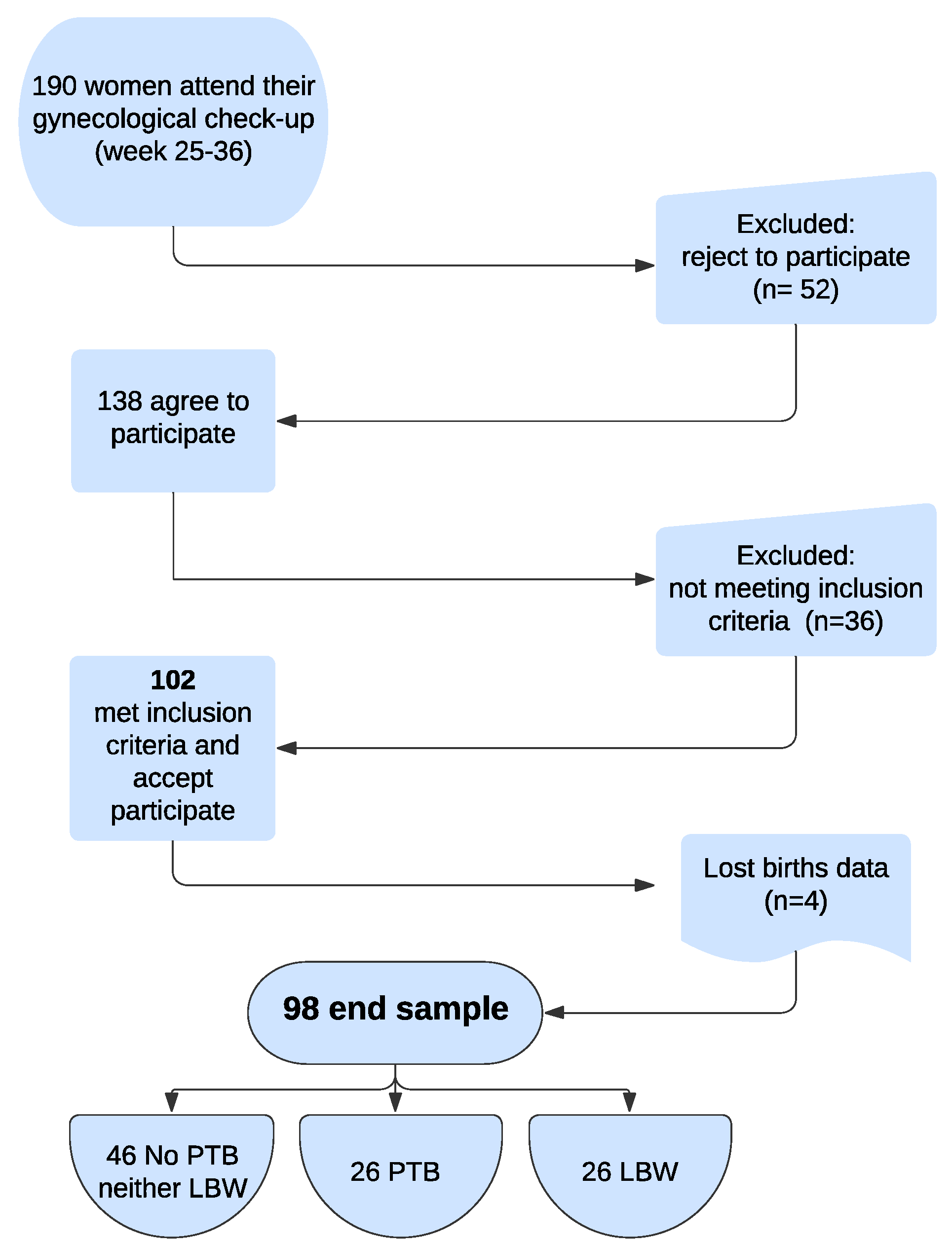
2. Materials and Methods
3. Results
3.1. Sample Description
3.2. Variables Related with the Childbirth
3.3. Oral Health Mother Status Variables
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- López, N.J.; Uribe, S.; Martinez, B. Effect of periodontal treatment on preterm birth rate: A systematic review of meta-analyses. Periodontol. 2000 2015, 67, 87–130. [Google Scholar] [CrossRef] [PubMed]
- WHO. Newborns: Improving Survival and Well-Being 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality (accessed on 6 April 2022).
- Liu, L.; Oza, S.; Hogan, D.; Chu, Y.; Perin, J.; Zhu, J.; Lawn, J.E.; Cousens, S.; Mathers, C.; Black, R.E. Global, regional, and national causes of under-5 mortality in 2000-15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016, 388, 3027–3035. [Google Scholar] [CrossRef]
- OMS. Born Too Soon. In The Global Action Report on Preterm Birth; World Health Organization: Geneva, Switzerland, 2012; Available online: https://apps.who.int/iris/rest/bitstreams/53412/retrieve (accessed on 6 April 2022).
- Tedesco, R.P.; Galvão, R.B.; Guida, J.P.; Passini-Júnior, R.; Lajos, G.J.; Nomura, M.L.; Rehder, P.M.; Dias, T.Z.; Souza, R.T.; Cecatti, J.G. Group Brazilian Multicentre Study on Preterm Birth Study. The role of maternal infection in preterm birth: Evidence from the Brazilian Multicentre Study on Preterm Birth (EMIP). Clinics 2020, 75, e1508. [Google Scholar] [CrossRef] [PubMed]
- Manrique-Corredor, E.J.; Orozco-Beltran, D.; Lopez-Pineda, A.; Quesada, J.A.; Gil-Guillen, V.F.; Carratala-Munuera, C. Maternal periodontitis and preterm birth: Systematic review and meta-analysis. Community Dent. Oral Epidemiol. 2019, 47, 243–251. [Google Scholar] [CrossRef]
- Figuero, E.; Han, Y.W.; Furuichi, Y. Periodontal diseases and adverse pregnancy outcomes: Mechanisms. Periodontol. 2000 2020, 83, 175–188. [Google Scholar] [CrossRef]
- Puertas, A.; Magan-Fernandez, A.; Blanc, V.; Revelles, L.; O’Valle, F.; Pozo, E.; León, R.; Mesa, F. Association of periodontitis with preterm birth and low birth weight: A comprehensive review. J. Matern.-Fetal Neonatal Med. 2018, 31, 597–602. [Google Scholar] [CrossRef]
- Sanz, M.; Kornman, K. Working group 3 of joint EFP/AAP workshop. Periodontitis and adverse pregnancy outcomes: Consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J. Clin. Periodontol. 2013, 40 (Suppl. S14), S164–S169. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Periodontol. 2018, 89 (Suppl. S1), S159–S172. [Google Scholar] [CrossRef]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89 (Suppl. S1), S173–S182. [Google Scholar] [CrossRef]
- Río, I.; Castelló, A.; Jané, M.; Prats, R.; Barona, C.; Más, R.; Rebagliato, M.; Zurriaga, O.; Bolúmar, F. Reproductive and perinatal health indicators in immigrant and Spanish-born women in Catalonia and Valencia (2005–2006). Gac. Sanit. 2010, 24, 123–127. [Google Scholar] [CrossRef]
- World Health Organization. Oral Health Surveys—Basic Method, 5th ed.; World Health Organization: Geneva, Switzerland, 2013; pp. 1–137. [Google Scholar]
- Jarjoura, K.; Devine, P.C.; Perez-Delboy, A.; Herrera-Abreu, M.; D’Alton, M.; Papapanou, P.N. Markers of periodontal infection and preterm birth. Am. J. Obstet. Gynecol. 2005, 192, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Dörtbudak, O.; Eberhardt, R.; Ulm, M.; Persson, G.R. Periodontitis, a marker of risk in pregnancy for preterm birth. J. Clin. Periodontol. 2005, 32, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Turton, M.; Africa, C.W.J. Further evidence for periodontal disease as a risk indicator for adverse pregnancy outcomes. Int. Dent. J. 2017, 67, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Jeffcoat, M.K.; Geurs, N.C.; Reddy, M.S.; Cliver, S.P.; Goldenberg, R.L.; Hauth, J.C. Periodontal infection and preterm birth. J. Am. Dent. Assoc. 2001, 132, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Romero, B.C.; Chiquito, C.S.; Elejalde, L.E.; Bernardoni, C.B. Relationship between Periodontal Disease in Pregnant Women and the Nutritional Condition of Their Newborns. J. Periodontol. 2002, 73, 1177–1183. [Google Scholar] [CrossRef] [PubMed]
- Goepfert, A.R.; Jeffcoat, M.K.; Andrews, W.W.; Faye-Petersen, O.; Cliver, S.P.; Goldenberg, R.L.; Hauth, J.C. Periodontal disease and upper genital tract inflammation in early spontaneous preterm birth. Obstet. Gynecol. 2004, 104, 777–783. [Google Scholar] [CrossRef]
- Manau, C.; Echeverria, A.; Agueda, A.; Guerrero, A.; Echeverria, J.J. Periodontal disease definition may determine the association between periodontitis and pregnancy outcomes. J. Clin. Periodontol. 2008, 35, 385–397. [Google Scholar] [CrossRef]
- Offenbacher, S.; Katz, V.; Fertik, G.; Collins, J.; Boyd, D.; Maynor, G. Periodontal infection as a possible risk factor for preterm low birth weight. J. Periodontol. 1996, 67 (Suppl. S10), 1103–1113. [Google Scholar] [CrossRef]
- de Oliveira, L.J.C.; Cademartori, M.G.; Schuch, H.S.; Barros, F.C.; Silveira, M.F.; Correa, M.B.; Demarco, F.F. Periodontal disease and preterm birth: Findings from the 2015 Pelotas birth cohort study. Oral Dis. 2021, 27, 1519–1527. [Google Scholar] [CrossRef]
- Offenbacher, S.; Lieff, S.; Boggess, K.A.; Murtha, A.P.; Madianos, P.N.; Champagne, C.M.; McKaig, R.G.; Jared, H.L.; Mauriello, S.M.; Auten, R.L., Jr.; et al. Maternal periodontitis and prematurity. Part I: Obstetric outcome of prematurity and growth restriction. Ann. Periodontol. 2001, 6, 164–174. [Google Scholar] [CrossRef]
- López, N.J.; Smith, P.C.; Gutierrez, J. Higher Risk of Preterm Birth and Low Birth Weight in Women with Periodontal Disease. J. Dent. Res. 2002, 81, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Boggess, K.A.; Lieff, S.; Murtha, A.P.; Moss, K.; Beck, J.; Offenbacher, S. Maternal periodontal disease is associated with an increased risk for preeclampsia. Obstet. Gynecol. 2003, 101, 227–231. [Google Scholar] [PubMed]
- Marin, C.; Segura-Egea, J.J.; Martínez-Sahuquillo, Á.; Bullón, P. Correlation between infant birth weight and mother’s periodontal status. J. Clin. Periodontol. 2005, 32, 299–304. [Google Scholar] [CrossRef]
- Moreu, G.; Téllez, L.; González-Jaranay, M. Relationship between maternal periodontal disease and low-birth-weight pre-term infants. J. Clin. Periodontol. 2005, 32, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Bobetsis, Y.A.; Graziani, F.; Gürsoy, M.; Madianos, P.N. Periodontal disease and adverse pregnancy outcomes. Periodontol. 2000 2020, 83, 154–174. [Google Scholar] [CrossRef] [PubMed]
- Caneiro, L.; Lopez-Carral, J.M.; Martin-Lancharro, P.; Linares, A.; Batalla, P.; Blanco-Carrion, J. Periodontitis as a Preterm Birth Risk Factor in Caucasian Women: A Cohort Study. Oral Health Prev. Dent. 2020, 18, 77–83. [Google Scholar]
- Offenbacher, S.; Jared, H.L.; O’Reilly, P.G.; Wells, S.R.; Salvi, G.E.; Lawrence, H.P.; Beck, J.D. Potential pathogenic mechanisms of periodontitis associated pregnancy complications. Ann. Periodontol. 1998, 3, 233–250. [Google Scholar] [CrossRef]
- Cruz, S.S.; Costa, M.D.C.N.; Gomes-Filho, I.S.; Rezende, E.J.C.; Barreto, M.L.; Dos Santos, C.A.S.T.; Vianna, M.I.P.; Passos, J.S.; Cerqueira, E.M.M. Contribution of periodontal disease in pregnant women as a risk factor for low birth weight. Community Dent. Oral Epidemiol. 2009, 37, 527–533. [Google Scholar] [CrossRef]
- Martins Moliterno, L.F.; Monteiro, B.; da Silva Figueredo, C.M.; Fischer, R.G. Association between periodontitis and low birth weight: A case-control study. J. Clin. Periodontol. 2005, 32, 886–890. [Google Scholar] [CrossRef]
- Vettore, M.V.; Leal, M.D.C.; Leão, A.T.; Monteiro Da Silva, A.M.; Lamarca, G.A.; Sheiham, A. The relationship between periodontitis and preterm low birthweight. J. Dent. Res. 2008, 87, 73–78. [Google Scholar] [CrossRef]
- Bulut, G.; Olukman, O.; Calkavur, S. Is there a relationship between maternal periodontitis and pre-term birth? A prospective hospital-based case-control study. Acta Odontol. Scand. 2014, 72, 866–873. [Google Scholar] [CrossRef] [PubMed]
- Ide, M.; Papapanou, P.N. Epidemiology of association between maternal periodontal disease and adverse pregnancy outcomes —Systematic review. J. Periodontol. 2013, 84, S181–S194. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Martínez, R.E.; Moreno-Castillo, D.F.; Loyola-Rodríguez, J.P.; Sánchez-Medrano, A.G.; Miguel-Hernández, J.H.S.; Olvera-Delgado, J.H.; Domínguez-Pérez, R.A. Association between periodontitis, periodontopathogens and preterm birth: Is it real? Arch. Gynecol. Obstet. 2016, 294, 47–54. [Google Scholar] [CrossRef]
- Fogacci, M.F.; Cardoso, E.D.O.; Barbirato, D.D.S.; de Carvalho, D.P.; Sansone, C. No association between periodontitis and preterm low birth weight: A case–control study. Arch. Gynecol. Obstet. 2018, 297, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Marquez-Corona, M.D.L.; Tellez-Giron-Valdez, A.; Pontigo-Loyola, A.P.; Islas-Zarazúa, R.; Robles-Bermeo, N.L.; Gonzalez-López, B.S.; Medina-Solís, C.E. Preterm birth associated with periodontal and dental indica-tors: A pilot case-control study in a developing country. J. Matern. Fetal Neonatal Med. 2021, 34, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.; Ide, M.; Coward, P.Y.; Randhawa, M.; Borkowska, E.; Baylis, R.; Wilson, R.F. A prospective study to investigate the relationship between periodontal disease and adverse pregnancy outcome. Br. Dent. J. 2004, 197, 251–258. [Google Scholar] [CrossRef]
- Srinivas, S.K.; Sammel, M.D.; Stamilio, D.M.; Clothier, B.; Jeffcoat, M.K.; Parry, S.; Macones, G.A.; Elovitz, M.A.; Metlay, J. Periodontal disease and adverse pregnancy outcomes: Is there an association? Am. J. Obstet. Gynecol. 2009, 200, 497.e1–497.e8. [Google Scholar] [CrossRef]
- Corbella, S.; Taschieri, S.; Del Fabbro, M.; Francetti, L.; Weinstein, R.; Ferrazzi, E. Adverse pregnancy outcomes and periodontitis: A systematic review and meta- analysis exploring potential association. Quintessence Int. 2016, 47, 193–204. [Google Scholar]
- Ye, C.; Kapila, Y. Oral microbiome shifts during pregnancy and adverse pregnancy outcomes: Hormonal and Immunologic changes at play. Periodontol. 2000 2021, 87, 276–281. [Google Scholar] [CrossRef]
- Al Habashneh, R.; Guthmiller, J.M.; Levy, S.; Johnson, G.K.; Squier, C.; Dawson, D.V.; Fang, Q. Factors related to utilization of dental services during pregnancy. J. Clin. Periodontol. 2005, 32, 815–821. [Google Scholar] [CrossRef]
- Usin, M.M.; Menso, J.; Rodríguez, V.I.; González, A.; Tabares, S.; Parodi, R.; Sembaj, A. Association between maternal periodontitis and preterm and/or low birth weight infants in normal pregnancies. J. Matern. Fetal Neonatal Med. 2016, 29, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Kruse, A.B.; Kuerschner, A.C.; Kunze, M.; Woelber, J.P.; Al-Ahmad, A.; Wittmer, A.; Vach, K.; Ratka-Krueger, P. Association between high risk for preterm birth and changes in gingiva parameters during pregnancy—A prospective cohort study. Clin. Oral Investig. 2017, 22, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Karimi, M.R.; Hamissi, J.H.; Naeini, S.R.; Karimi, M. The Relationship Between Maternal Periodontal Status of and Preterm and Low Birth Weight Infants in Iran: A Case Control Study. Glob. J. Health Sci. 2015, 8, 184–188. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hughes, M.M.; Black, R.E.; Katz, J. 2500-g Low Birth Weight Cutoff: History and Implications for Future Research and Policy. Matern. Child Health J. 2016, 21, 283–289. [Google Scholar] [CrossRef]
- Andonova, I.; Iliev, V.; Živković, N.; Sušič, E.; Bego, I.; Kotevska, V. Can oral anaerobic bacteria cause adverse pregnancy outcomes? Prilozi 2015, 36, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Marakoglu, I.; Gursoy, U.K.; Marakoglu, K.; Cakmak, H.; Ataoglu, T. Periodontitis as a Risk Factor for Preterm Low Birth Weight. Yonsei Med. J. 2008, 49, 200–203. [Google Scholar] [CrossRef] [PubMed]
- Resende, M.; Pinto, E.; Pinto, M.; Montenegro, N. Periodontal disease, tobacco and preterm delivery. Acta Med. Port. 2011, 24 (Suppl. S2), 419–430. [Google Scholar]
- Baig, S.A.; Khan, N.; Baqai, T.; Fatima, A.; Karim, S.A.; Aziz, S. Preterm birth and its associated risk factors. A study at tertiary care hospitals of Karachi, Pakistan. J. Pak. Med. Assoc. 2013, 63, 414–418. [Google Scholar]
- Lee, H.J.; Ha, J.E.; Bae, K.H. Synergistic effect of maternal obesity and periodontitis on preterm birth in women with pre-eclampsia: A prospective study. J. Clin. Periodontol. 2016, 43, 646–651. [Google Scholar] [CrossRef]
- Moliner-Sánchez, C.A.; Iranzo-Cortés, J.E.; Almerich-Silla, J.M.; Bellot-Arcís, C.; Ortolá-Siscar, J.C.; Montiel-Company, J.M.; Almerich-Torres, T. Effect of per Capita Income on the Relationship between Periodontal Disease during Pregnancy and the Risk of Preterm Birth and Low Birth Weight Newborn. Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health. 2020, 17, 8015. [Google Scholar] [CrossRef]
| Variable | Mean or % (CI at 95%) |
|---|---|
| Mother’s age | 32.43 (31.32–33.53) |
| Initial Maternal BMI | 23.11 (22.42–23.81) |
| Pregnancy history | 1.11 (0.84–1.38) |
| Vaginal births | 0.51 (0.33–0.69) |
| C-sections | 0.13 (0.06–0.21) |
| Abortions | 0.46 (0.33–0.59) |
| Level of education | |
| Low level | 18.6% (12.3–27.3) |
| Middle level | 36.3% (27.6–45.9) |
| High level | 45.1% (35.8–54.8) |
| Periodontal condition | |
| Periodontal disease 1 | 24.5% (17.2–33.7) |
| % of bleeding | 16.43% (13.52–19.35) |
| Pockets > 3 mm | 8.83 (6.66–11.01) |
| Pockets > 5 mm | 0.53 (0.23–0.83) |
| CAL > 0 mm | 1.14 (0.58–1.69) |
| Caries status | |
| Component D (DMFT) | 0.62 (0.34–0.90) |
| Component M (DMFT) | 0.64 (0.37–0.91) |
| Component filled (BMFT) | 2.37 (1.85–2.89) |
| DMFT | 3.63 (2.97–4.28) |
| % caries-free (DMFT = 0) | 15.7% (9.9% a 23.9%) |
| Prevalence of caries | 84.3% (76.0–90.1%) |
| Variable | Preterm Birth (PTB) | p Value Test | |
|---|---|---|---|
| YES (n = 26) | NO (n = 72) | ||
| New-born’s weight (gr) | 2450.8 (2278.9–2622.7) | 3244.9 (3134.8–3355.2) | p < 0.001 * |
| New-born’s height (cm) | 48.7 (48.4–49.1) | 49.6 (48.4–50.7) | p = 0.396 |
| Length of time after rupturing of membranes | 4.31 (2.68–5.94) | 6.86 (5.57–8.15) | p = 0.033 * |
| Apgar score at 5 min of life | 8.96 (8.35–8.57) | 9.51 (9.31–9.71) | p = 0.026 * |
| Arterial pH | 7.17 (7.13–7.21) | 7.19 (7.17–7.21) | p = 0.323 |
| Epidural anaesthesia | 80.8% (62.1–91.5) | 94.4% (86.6–97.9) | p = 0.115 |
| Local anaesthesia | 3.8% (0.7–18.9) | 1.4% (0.3–7.5) | |
| No anaesthesia | 15.4% (6.2–33.5) | 4.2% (1.4–11.5) | |
| Use of oxytocin | 61.5% (42.5–77.6) | 90.3% (81.2–95.2) | p = 0.001 |
| Clear amniotic fluid | 84.6% (66.5–93.4) | 87.5% (77.8–93.3) | p = 0.710 |
| Meconial amniotic fluid | 15.4% (6.2–33.5) | 12.5% (6.7–22.1) | |
| Spontaneous birth | 57.7% (39.0–74.5) | 66.7% (55.2–76.5) | p = 0.589 |
| Instrumental vaginal birth | 30.8% (16.5–50.0) | 20.8% (13.1–31.6) | |
| C-section | 11.5% (4.0–29.0) | 12.5% (6.7–22.1) | |
| Variable | Preterm Birth (PTB) | p Value Test | |
|---|---|---|---|
| YES (n = 26) | NO (n = 72) | ||
| % of Bleeding | 17.0% (11.2–22.7) | 16.4% (12.8–20.0) | p = 0.871 |
| Pockets > 3 mm | 10.81 (5.76–15.86) | 8.51 (5.99–11.0) | p = 0.374 |
| Prevalence of pockets > 3 mm | 92.3% (75.9–97.9) | 79.2% (68.4–87.0) | p = 0.129 OR = 3.2 (0.7–14.9) |
| Pockets > 5 mm | 0.85 (0–1.69) | 0.41 (0.11–0.73) | p = 0.233 |
| Prevalence Pockets > 5 mm | 23.1% (11.0–42.1) | 16.7% (9.8–27.0) | p = 0.469 OR = 1.5 (0.49–4.5) |
| Points with CAL > 0 mm | 1.88 (0.50–3.27) | 0.90 (0.28–1.52) | p = 0.138 |
| Prevalence of CAL | 46.2% (28.8–64.5) | 30.6% (21.1–42.0) | p = 0.152 OR = 1.94 (0.8–4.9) |
| Periodontal disease | 30.8% (16.5–50.0) | 23.6% (15.3–34.6) | p = 0.473 OR = 1.43 (0.53–3.88) |
| Component D (DMFT) | 0.69 (0–1.39) | 0.63 (0.31–0.94) | p = 0.841 |
| Component M (DMFT) | 0.46 (0.03–0.89) | 0.74 (0.38–1.09) | p = 0.396 |
| Component F (DMFT) | 2.23 (1.31–3.15) | 2.44 (1.78–3.11) | p = 0.731 |
| DMFT index | 3.38 (2.42–4.35) | 3.81 (2.94–4.67) | p = 0.589 |
| Prevalence of caries | 84.6% (66.5–93.9) | 84.7% (74.7–91.3) | p = 0.990 OR = 1 (0.3–3.4) |
| Smoker | 17.4% (7.1–37.1) | 7.2% (3.1–15.9) | p = 0.156 OR = 2.7 (0.7–11.0) |
| Variable | Low Birth Weight (LBW) | p Value Test | |
|---|---|---|---|
| YES | NO | ||
| % of bleeding | 18.3% (13.0–23.6) | 15.9% (12.2–19.6) | p = 0.871 |
| Pockets > 3 mm | 11.7 (11.5–16.8) | 8.21 (5.73–10.7) | p = 0.374 |
| Prevalence of pockets > 3 mm | 84.6% (66.5–93.9) | 81.9% (71.5–89.1) | p = 0.758 OR = 1.21 (0.4–4.1) |
| Pockets > 5 mm | 0.85 (0–1.70) | 0.42 (0.11–0.73) | p = 0.233 |
| Prevalence Pockets > 5 mm | 23.1% (11.3–42.0) | 16.7% (9.8–26.9) | p = 0.469 OR = 1.5 (0.49–4.5) |
| Points with CAL > 0 mm | 2.54 (0.48–4.59) | 0.67 (0.40–0.94) | p = 0.138 |
| Prevalence of CAL | 46.2% (28.8–64.5) | 30.6% (21.1–42.2) | p = 0.152 OR = 1.9 (0.8–4.9) |
| Periodontal disease | 30.8% (16.6–50.0) | 23.6% (15.3–34.6) | p = 0.473 OR = 1.43 (0.53–3.88) |
| Component D (DMFT) | 0.85 (0.14–1.56) | 0.57 (0.25–0.88) | p = 0.841 |
| Component M (DMFT) | 0.77 (0.24–1.30) | 0.63 (0.28–0.97) | p = 0.396 |
| Component F (DMFT) | 2.35 (1.35–3.35) | 2.40 (1.75–3.06) | p = 0.731 |
| DMFT index | 3.96 (2.78–5.14) | 3.60 (2.76–4.43) | p = 0.589 |
| Prevalence of caries | 84.6% (66.5–93.9) | 84.7% (74.7–91.3) | p = 0.990 OR = 1 (0.3–2.4) |
| Smoker | 20.8% (9.2–40.5) | 5.9% (2.3–14.2) | p = 0.034 * OR = 4.2 (1.02–17.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gallagher-Cobos, G.; Almerich-Torres, T.; Montiel-Company, J.M.; Iranzo-Cortés, J.E.; Bellot-Arcís, C.; Ortolá-Siscar, J.C.; Almerich-Silla, J.M. Relationship between Periodontal Condition of the Pregnant Woman with Preterm Birth and Low Birth Weight. J. Clin. Med. 2022, 11, 6857. https://doi.org/10.3390/jcm11226857
Gallagher-Cobos G, Almerich-Torres T, Montiel-Company JM, Iranzo-Cortés JE, Bellot-Arcís C, Ortolá-Siscar JC, Almerich-Silla JM. Relationship between Periodontal Condition of the Pregnant Woman with Preterm Birth and Low Birth Weight. Journal of Clinical Medicine. 2022; 11(22):6857. https://doi.org/10.3390/jcm11226857
Chicago/Turabian StyleGallagher-Cobos, Guillermo, Teresa Almerich-Torres, José María Montiel-Company, José Enrique Iranzo-Cortés, Carlos Bellot-Arcís, José Carmelo Ortolá-Siscar, and José Manuel Almerich-Silla. 2022. "Relationship between Periodontal Condition of the Pregnant Woman with Preterm Birth and Low Birth Weight" Journal of Clinical Medicine 11, no. 22: 6857. https://doi.org/10.3390/jcm11226857
APA StyleGallagher-Cobos, G., Almerich-Torres, T., Montiel-Company, J. M., Iranzo-Cortés, J. E., Bellot-Arcís, C., Ortolá-Siscar, J. C., & Almerich-Silla, J. M. (2022). Relationship between Periodontal Condition of the Pregnant Woman with Preterm Birth and Low Birth Weight. Journal of Clinical Medicine, 11(22), 6857. https://doi.org/10.3390/jcm11226857








