Effect of the Age-Adjusted Charlson Comorbidity Index on the Survival of Esophageal Squamous Cell Carcinoma Patients after Radical Esophagectomy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Surgical Procedure and Other Treatments
2.4. Definition of the Comorbidities
2.5. Survival Data
2.6. Statistical Analysis
3. Results
3.1. Comorbidity
3.2. Demographic and Clinical Baseline Characteristics
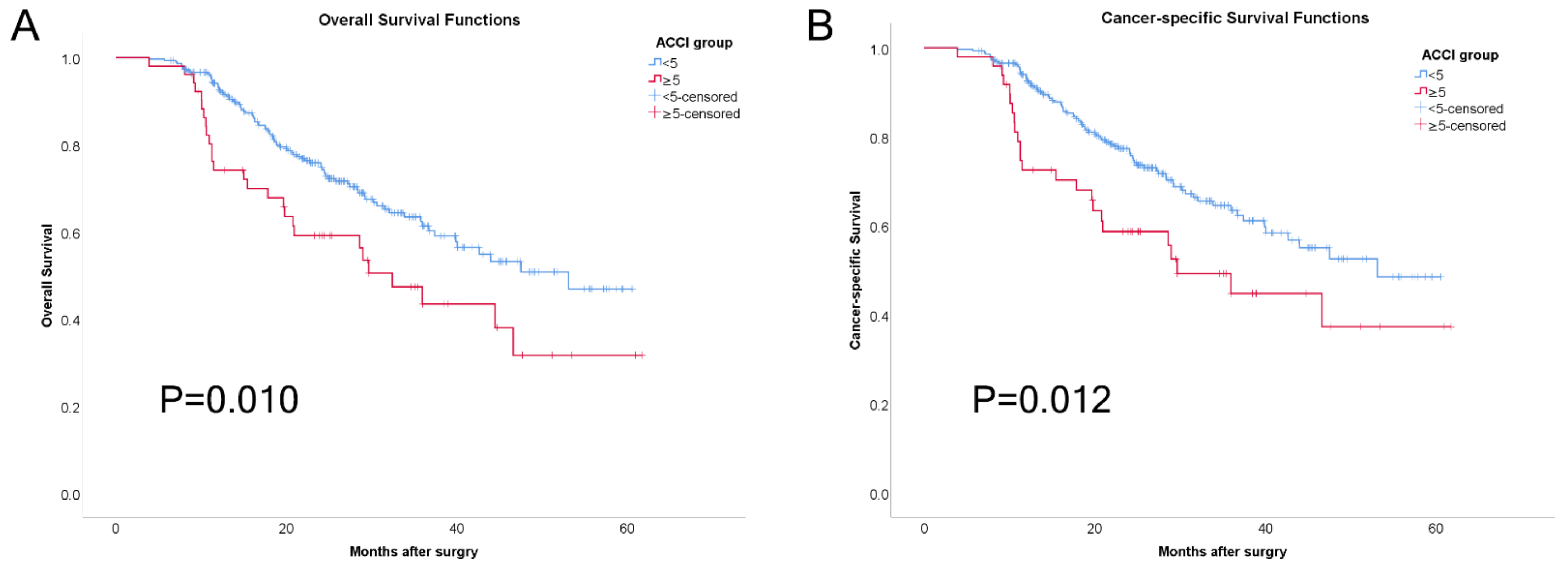
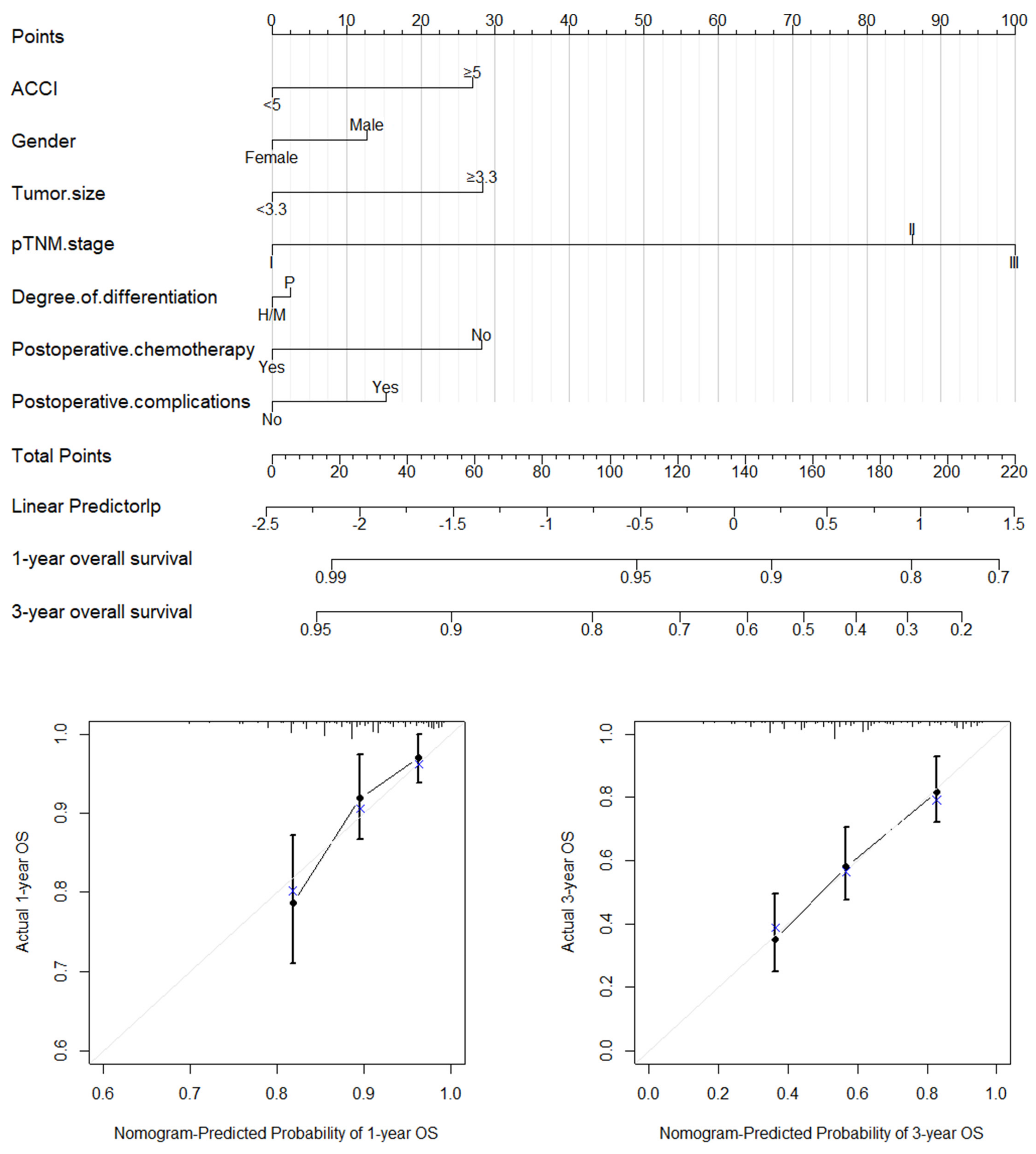
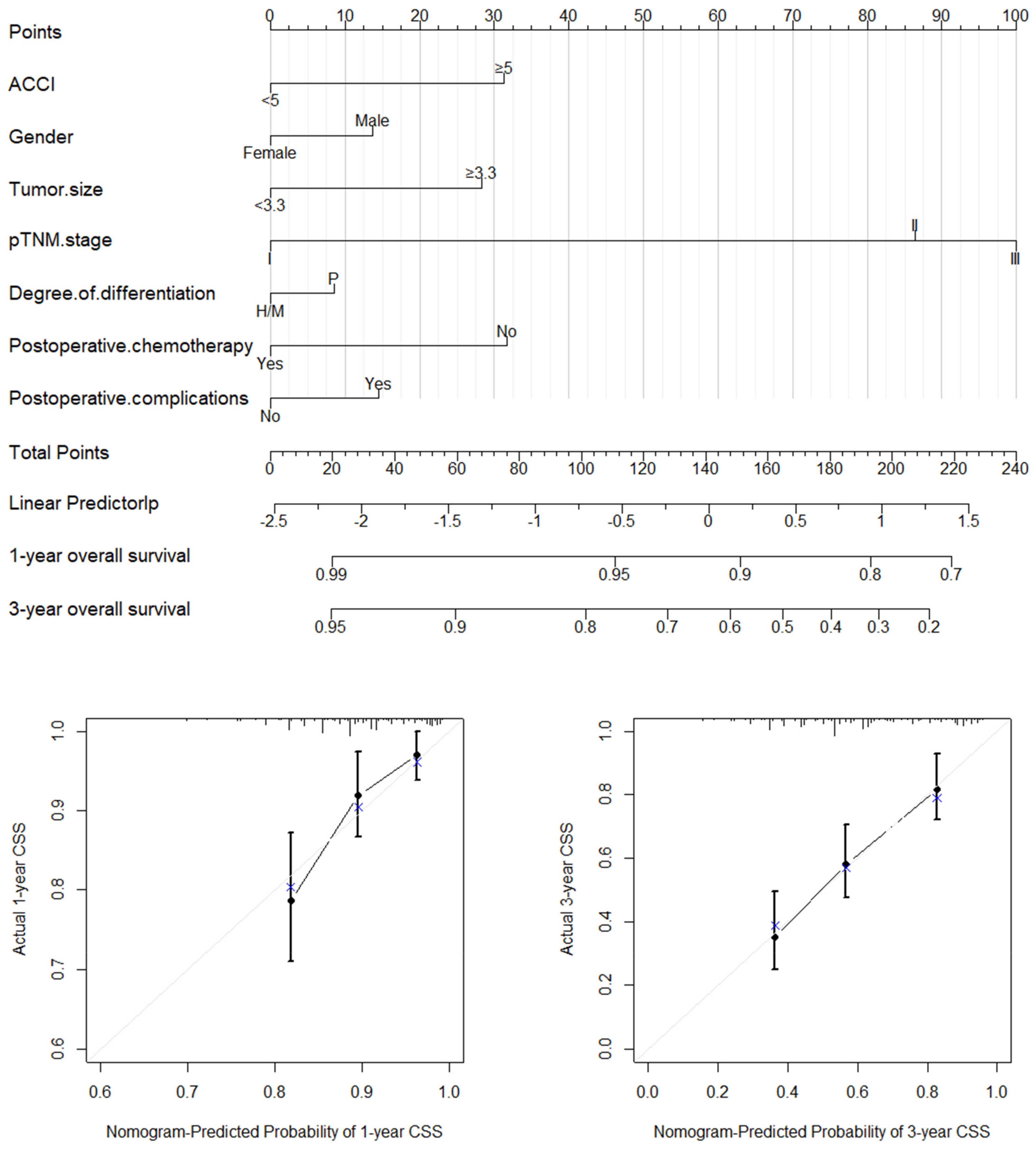
3.3. Survival Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Yip, H.C.; Shirakawa, Y.; Cheng, C.Y.; Huang, C.L.; Chiu, P.W.Y. Recent advances in minimally invasive esophagectomy for squamous esophageal cancer. Ann. N. Y. Acad. Sci. 2020, 1482, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Li, C.; Huang, L.; Niu, S.; Lu, Q.; Gong, D.; Huang, S.; Yuan, Y.; Chen, H. Prognostic value of association of OCT4 with LEF1 expression in esophageal squamous cell carcinoma and their impact on epithelial-mesenchymal transition, invasion, and migration. Cancer Med. 2018, 7, 3977–3987. [Google Scholar] [CrossRef] [PubMed]
- Van Workum, F.; Klarenbeek, B.R.; Baranov, N.; Rovers, M.M.; Rosman, C. Totally minimally invasive esophagectomy versus hybrid minimally invasive esophagectomy: Systematic review and meta-analysis. Dis. Esophagus 2020, 33, doaa021. [Google Scholar] [CrossRef]
- He, Z.; Ke, Y. Precision screening for esophageal squamous cell carcinoma in China. Chin. J. Cancer Res. 2020, 32, 673–682. [Google Scholar] [CrossRef]
- Chang, J.; Tan, W.; Ling, Z.; Xi, R.; Shao, M.; Chen, M.; Luo, Y.; Zhao, Y.; Liu, Y.; Huang, X.; et al. Genomic analysis of oesophageal squamous-cell carcinoma identifies alcohol drinking-related mutation signature and genomic alterations. Nat. Commun. 2017, 8, 15290. [Google Scholar] [CrossRef]
- Huang, F.L.; Yu, S.J. Esophageal cancer: Risk factors, genetic association, and treatment. Asian J. Surg. 2018, 41, 210–215. [Google Scholar] [CrossRef]
- Yang, Y.; Chen, M.; Xie, J.; Ji, Y.; Sheng, L.; Qiu, G.; Du, X.; Wei, Q. Treatment Patterns and Outcomes of Elderly Patients with Potentially Curable Esophageal Cancer. Front. Oncol. 2022, 12, 778898. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Robbins, J.R.; Gayar, O.H.; Zaki, M.; Mahan, M.; Buekers, T.; Elshaikh, M.A. Impact of age-adjusted Charlson comorbidity score on outcomes for patients with early-stage endometrial cancer. Gynecol. Oncol. 2013, 131, 593–597. [Google Scholar] [CrossRef]
- Kahl, A.; du Bois, A.; Harter, P.; Prader, S.; Schneider, S.; Heitz, F.; Traut, A.; Alesina, P.F.; Meier, B.; Walz, M.; et al. Prognostic Value of the Age-Adjusted Charlson Comorbidity Index (ACCI) on Short- and Long-Term Outcome in Patients with Advanced Primary Epithelial Ovarian Cancer. Ann. Surg. Oncol. 2017, 24, 3692–3699. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kang, H.W.; Rha, K.H.; Cho, N.H.; Choi, Y.D.; Hong, S.J.; Cho, K.S. Age-adjusted Charlson comorbidity index is a significant prognostic factor for long-term survival of patients with high-risk prostate cancer after radical prostatectomy: A Bayesian model averaging approach. J. Cancer Res. Clin. Oncol. 2016, 142, 849–858. [Google Scholar] [CrossRef]
- Wu, C.C.; Hsu, T.W.; Chang, C.M.; Yu, C.H.; Lee, C.C. Age-adjusted Charlson comorbidity index scores as predictor of survival in colorectal cancer patients who underwent surgical resection and chemoradiation. Medicine 2015, 94, e431. [Google Scholar] [CrossRef]
- Dias-Santos, D.; Ferrone, C.R.; Zheng, H.; Lillemoe, K.D.; Fernández-Del Castillo, C. The Charlson age comorbidity index predicts early mortality after surgery for pancreatic cancer. Surgery 2015, 157, 881–887. [Google Scholar] [CrossRef]
- Aoyama, T.; Atsumi, Y.; Kawahara, S.; Tamagawa, H.; Tamagawa, A.; Ozawa, Y.; Maezawa, Y.; Kano, K.; Murakawa, M.; Kazama, K.; et al. The Clinical Impact of the Age-adjusted Charlson Comorbidity Index on Esophageal Cancer Patients Who Receive Curative Treatment. In Vivo 2020, 34, 2783–2790. [Google Scholar] [CrossRef]
- Hu, C.; Lin, Z.; Liu, Z.; Tang, X.; Song, J.; Lin, J.; Chen, Y.; Hu, Z. Dietary fatty acid patterns and risk of oesophageal squamous cell carcinoma. PeerJ. 2022, 10, e13036. [Google Scholar] [CrossRef]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. Chinese guidelines for diagnosis and treatment of esophageal carcinoma 2018 (English version). Chin. J. Cancer Res. 2019, 31, 223–258. [Google Scholar] [CrossRef]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Bannay, A.; Chaignot, C.; Blotière, P.O.; Basson, M.; Weill, A.; Ricordeau, P.; Alla, F. The Best Use of the Charlson Comorbidity Index with Electronic Health Care Database to Predict Mortality. Med. Care 2016, 54, 188–194. [Google Scholar] [CrossRef]
- Koseki, Y.; Hikage, M.; Fujiya, K.; Kamiya, S.; Tanizawa, Y.; Bando, E.; Terashima, M. Utility of a modified age-adjusted Charlson Comorbidity Index in predicting cause-specific survival among patients with gastric cancer. Eur. J. Surg. Oncol. 2021, 47, 2010–2015. [Google Scholar] [CrossRef] [PubMed]
- Camp, R.L.; Dolled-Filhart, M.; Rimm, D.L. X-tile: A new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin. Cancer Res. 2004, 10, 7252–7259. [Google Scholar] [CrossRef]
- Harrell, F.E., Jr.; Lee, K.L.; Mark, D.B. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat. Med. 1996, 15, 361–387. [Google Scholar] [CrossRef]
- Raykar, V.C.; Steck, H.; Krishnapuram, B.; Dehing-Oberije, C.; Lambin, P. On ranking in survival analysis: Bounds on the concordance index. In Proceedings of the 20th International Conference on Neural Information Processing Systems, Vancouver, BC, Canada, 3–6 December 2007; pp. 1209–1216. [Google Scholar]
- Chaudhary, K.; Poirion, O.B.; Lu, L.; Garmire, L.X. Deep Learning-Based Multi-Omics Integration Robustly Predicts Survival in Liver Cancer. Clin. Cancer Res. 2018, 24, 1248–1259. [Google Scholar] [CrossRef]
- Takada, Y.; Kawashima, H.; Ohno, E.; Ishikawa, T.; Mizutani, Y.; Iida, T.; Yamamura, T.; Kakushima, N.; Furukawa, K.; Nakamura, M.; et al. The impact of the age-adjusted Charlson comorbidity index as a prognostic factor for endoscopic papillectomy in ampullary tumors. J. Gastroenterol. 2022, 57, 199–207. [Google Scholar] [CrossRef]
- Qu, W.F.; Zhou, P.Y.; Liu, W.R.; Tian, M.X.; Jin, L.; Jiang, X.F.; Wang, H.; Tao, C.Y.; Fang, Y.; Zhou, Y.F.; et al. Age-adjusted Charlson Comorbidity Index predicts survival in intrahepatic cholangiocarcinoma patients after curative resection. Ann. Transl. Med. 2020, 8, 487. [Google Scholar] [CrossRef]
- Pan, C.; Wang, X.; Chen, W.; Tao, C.; Xu, X.; Jin, L.; Chen, Y.; Zhu, L.; Zhou, L.; Pan, Z. Reevaluation of glypican-3 as a prognostic marker in HCC using X-tile software. Med. Oncol. 2015, 32, 359. [Google Scholar] [CrossRef]
- Zhuang, W.; Chen, J.; Li, Y.; Liu, W. Valuation of lymph node dissection in localized high-risk renal cell cancer using X-tile software. Int. Urol. Nephrol. 2020, 52, 253–262. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, Y.; Qu, P.; Liu-Helmersson, J.; Zhao, L.; Zhang, L.; Sang, S. Prognostic Value of Tumor Length for Cause-Specific Death in Resectable Esophageal Cancer. Ann. Thorac. Surg. 2018, 106, 1038–1046. [Google Scholar] [CrossRef]
- Liu, L.; Lu, Z.; Hu, X.; Su, T.; Su, L.; Pu, H. Clinical significance of YAP1 and TAZ in esophageal squamous cell carcinoma. Medicine 2021, 100, e26597. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Tang, P.; Miao, X.; Gao, Y.; Shang, X.; Gong, L.; Ma, Z.; Yang, M.; Jiang, H.; Zhan, Z.; et al. Does tumor size improve the accuracy of prognostic prediction in patients with esophageal squamous cell carcinoma after surgical resection? Oncotarget 2016, 7, 66623–66634. [Google Scholar] [CrossRef] [PubMed]
- Xia, L.; Liang, W.; Que, D.; Xie, Q. Correlation Analysis of circRNA Circ_0071662 in Diagnosis and Prognosis of Esophageal Squamous Cell Carcinoma. Int. J. Gen. Med. 2021, 14, 10423–10428. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.; Wang, W.; Deng, J.Y.; Sun, Z.; Seeruttun, S.R.; Wang, Z.N.; Xu, H.M.; Liang, H.; Zhou, Z.W. Proposal and validation of a modified staging system to improve the prognosis predictive performance of the 8th AJCC/UICC pTNM staging system for gastric adenocarcinoma: A multicenter study with external validation. Cancer Commun. 2018, 38, 67. [Google Scholar] [CrossRef] [PubMed]
- Gu, C.; Shi, X.; Qiu, W.; Huang, Z.; Yu, Y.; Shen, F.; Chen, Y.; Pan, X. Comprehensive Analysis of the Prognostic Role and Mutational Characteristics of m6A-Related Genes in Lung Squamous Cell Carcinoma. Front. Cell Dev. Biol. 2021, 9, 661792. [Google Scholar] [CrossRef]
- Chen, S.B.; Huang, S.J.; Liu, D.T.; Weng, H.R.; Chen, Y.P. Clinicopathological features and prognosis of esophageal squamous cell carcinoma in young patients. Dis. Esophagus 2019, 32, doy070. [Google Scholar] [CrossRef]
- Sohda, M.; Saito, H.; Kuriyama, K.; Yoshida, T.; Kumakura, Y.; Honjyo, H.; Hara, K.; Ozawa, D.; Suzuki, S.; Tanaka, N.; et al. Post-esophagectomy Adjuvant Chemotherapy Benefits Esophageal Cancer Patients. In Vivo 2019, 33, 501–506. [Google Scholar] [CrossRef]
| Comorbidity | Score | n | (%) |
|---|---|---|---|
| Myocardial infarction | 1 | 1 | 0.3% |
| Congestive heart failure | 1 | 3 | 0.9% |
| Peripheral vascular disease | 1 | 100 | 28.4% |
| Cerebrovascular disease | 1 | 36 | 10.2% |
| Dementia | 1 | 1 | 0.3% |
| Chronic pulmonary disease | 1 | 135 | 38.4% |
| Rheumatic disease | 1 | 0 | 0.0% |
| Peptic ulcer disease | 1 | 18 | 5.1% |
| Mild liver disease | 1 | 65 | 18.5% |
| Diabetes mellitus without end-organ damage | 1 | 21 | 6.0% |
| Diabetes mellitus with end-organ damage | 2 | 1 | 0.3% |
| Hemiplegia | 2 | 0 | 0.0% |
| Renal disease | 2 | 3 | 0.9% |
| Any malignancy * | 2 | 0 | 0.0% |
| Lymphoma | 2 | 0 | 0.0% |
| Leukemia | 2 | 0 | 0.0% |
| Moderate liver disease | 3 | 9 | 2.6% |
| Metastatic solid tumor | 6 | 0 | 0.0% |
| Acquired immunodeficiency syndrome (AIDS) | 6 | 0 | 0.0% |
| Variables | All Patients (n = 352) | ACCI < 5 Group (n = 300) | ACCI ≥ 5 Group (n = 52) | p Value |
|---|---|---|---|---|
| Age, median (IQR), years | 63.00 (56.00–68.00) | 61.00 (55.00–75.00) | 72.00 (65.25–76.00) | <0.001 |
| Age group | <0.001 | |||
| <65 years | 225 (63.9%) | 212 (70.7%) | 13 (25.0%) | |
| ≥65 years | 127 (36.1%) | 88 (29.3%) | 39 (75.0%) | |
| Gender | 0.222 | |||
| Female | 91 (25.9%) | 74 (24.7%) | 17 (32.7%) | |
| Male | 261 (74.1%) | 226 (75.3%) | 35 (67.3%) | |
| Tumor size, median (IQR), cm | 4.25 (3.00–6.00) | 4.00 (3.00–5.00) | 3.9 (3.00–5.00) | 0.172 |
| pTNM stage | 0.619 | |||
| I | 82 (23.3%) | 72 (24.0%) | 10 (19.2%) | |
| II | 121 (34.4%) | 104 (34.7%) | 17 (32.7%) | |
| III | 149 (42.3%) | 124 (41.3%) | 25 (48.1%) | |
| Degree of differentiation | 0.056 | |||
| High/Medium | 229 (65.1%) | 190 (63.3%) | 39 (75.0%) | |
| Poor | 92 (26.1%) | 84 (28.0%) | 8 (15.4%) | |
| Postoperative chemotherapy | 0.771 | |||
| No | 243 (69.0%) | 208 (69.3%) | 35 (67.3%) | |
| Yes | 109 (31.0%) | 92 (30.7%) | 17 (32.7%) | |
| Postoperative complications | 0.117 | |||
| No | 143 (40.6%) | 127 (42.3%) | 16 (30.8%) | |
| Yes | 209 (59.4%) | 173 (57.7%) | 36 (69.2%) | |
| Follow-up time, median (IQR, months) | 23.37 (14.08–33.45) | 23.35 (14.55–33.12) | 23.60 (11.27–35.27) | 0.488 |
| Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|
| Variables | Survival/Total (%) | HR (95%CI) | p Value | HR * (95%CI) | p Value |
| Age group, years | |||||
| <65 | 157 (69.8%) | Reference | |||
| ≥65 | 77 (60.6%) | 1.43 (0.99–2.06) | 0.057 | ||
| Gender | |||||
| Female | 63 (69.2%) | Reference | Reference | ||
| Male | 171 (65.5%) | 1.32 (0.86–2.03) | 0.200 | 1.26 (0.80–1.99) | 0.326 |
| ACCI | |||||
| <5 | 209 (69.7%) | Reference | Reference | ||
| ≥5 | 25 (48.1%) | 1.74 (1.13–2.68) | 0.011 | 1.63 (1.04–2.56) | 0.035 |
| Tumor size, cm | |||||
| <3.30 | 102 (79.7%) | Reference | Reference | ||
| ≥3.30 | 123 (57.2%) | 2.79 (1.80–4.33) | <0.001 | 1.67 (1.05–2.66) | 0.032 |
| pTNM | |||||
| I | 77 (93.9%) | Reference | Reference | ||
| II | 78 (64.5%) | 6.50 (2.57–16.41) | <0.001 | 4.74 (1.82–12.32) | 0.001 |
| III | 79 (53.0%) | 9.75 (3.94–24.18) | <0.001 | 6.08 (2.37–15.60) | <0.001 |
| Degree of differentiation | |||||
| High/Medium | 147 (64.2%) | Reference | Reference | ||
| Poor | 60 (65.2%) | 0.94 (0.63–1.42) | 0.644 | 1.04 (0.69–1.58) | 0.835 |
| Postoperative chemotherapy | |||||
| No | 165 (67.9%) | Reference | Reference | ||
| Yes | 69 (63.3%) | 0.98 (0.80–1.18) | 0.787 | 0.60 (0.40–0.91) | 0.015 |
| Postoperative complications | |||||
| No | 112 (78.3%) | Reference | Reference | ||
| Yes | 122 (58.4%) | 1.49 (0.98–2.27) | 0.062 | 1.32 (0.85–2.05) | 0.224 |
| Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|
| Variables | Survival/Total (%) | HR (95%CI) | p Value | HR * (95%CI) | p Value |
| Age group, years | |||||
| <65 | 157 (71.4%) | Reference | |||
| ≥65 | 77 (62.6%) | 1.43 (0.98–2.09) | 0.067 | ||
| Gender | |||||
| Female | 63 (71.6%) | Reference | Reference | ||
| Male | 171 (67,1%) | 1.39 (0.89–2.17) | 0.154 | 1.28 (0.80–2.05) | 0.311 |
| ACCI | |||||
| <5 | 209 (71.1%) | Reference | Reference | ||
| ≥5 | 25 (51.0%) | 1.78 (1.13–2.80) | 0.013 | 1.75 (1.08–2.82) | 0.022 |
| Tumor size, cm | |||||
| <3.30 | 102 (80.3%) | Reference | Reference | ||
| ≥3.30 | 123 (59.4%) | 2.70 (1.72–4.23) | <0.001 | 1.66 (1.03–2.69) | 0.039 |
| pTNM | |||||
| I | 77 (93.9%) | Reference | Reference | ||
| II | 78 (66.1%) | 6.16 (2.43–15.62) | <0.001 | 4.70 (1.80–12.23) | 0.002 |
| III | 79 (55.2%) | 9.28 (3.71–22.93) | <0.001 | 5.99 (2.33–15.40) | <0.000 |
| Degree of differentiation | |||||
| High/Medium | 147 (65.6%) | Reference | Reference | ||
| Poor | 60 (66.7%) | 0.96 (0.63–1.47) | 0.853 | 1.17 (0.75–1.80) | 0.494 |
| Postoperative chemotherapy | |||||
| No | 165 (69.0%) | Reference | Reference | ||
| Yes | 69 (66.3%) | 0.89 (0.60–1.33) | 0.573 | 0.57 (0.37–0.87) | 0.009 |
| Postoperative complications | |||||
| No | 112 (78.3%) | Reference | Reference | ||
| Yes | 122 (61.0%) | 1.40 (0.91–2.14) | 0.125 | 1.30 (0.83–2.03) | 0.256 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, J.; Lin, Y.; Zhang, J.; Liu, S.; Zhou, J.; Zeng, Q.; Lin, Z.; Fu, R.; Qiu, M.; Hu, Z. Effect of the Age-Adjusted Charlson Comorbidity Index on the Survival of Esophageal Squamous Cell Carcinoma Patients after Radical Esophagectomy. J. Clin. Med. 2022, 11, 6737. https://doi.org/10.3390/jcm11226737
Song J, Lin Y, Zhang J, Liu S, Zhou J, Zeng Q, Lin Z, Fu R, Qiu M, Hu Z. Effect of the Age-Adjusted Charlson Comorbidity Index on the Survival of Esophageal Squamous Cell Carcinoma Patients after Radical Esophagectomy. Journal of Clinical Medicine. 2022; 11(22):6737. https://doi.org/10.3390/jcm11226737
Chicago/Turabian StyleSong, Jianyu, Yulan Lin, Juwei Zhang, Shuang Liu, Jinsong Zhou, Qiaoyan Zeng, Zheng Lin, Rong Fu, Minglian Qiu, and Zhijian Hu. 2022. "Effect of the Age-Adjusted Charlson Comorbidity Index on the Survival of Esophageal Squamous Cell Carcinoma Patients after Radical Esophagectomy" Journal of Clinical Medicine 11, no. 22: 6737. https://doi.org/10.3390/jcm11226737
APA StyleSong, J., Lin, Y., Zhang, J., Liu, S., Zhou, J., Zeng, Q., Lin, Z., Fu, R., Qiu, M., & Hu, Z. (2022). Effect of the Age-Adjusted Charlson Comorbidity Index on the Survival of Esophageal Squamous Cell Carcinoma Patients after Radical Esophagectomy. Journal of Clinical Medicine, 11(22), 6737. https://doi.org/10.3390/jcm11226737









