Abstract
Measuring the quality of information delivered to patients with severe mental illness (SMI), i.e., schizophrenia, bipolar disorders, and major depressive disorders, is essential to improve their quality of care. In this work, we described the different steps of the validation of the PREMIUM computerized adaptive testing (CAT) for measuring the quality of information delivered to patients with SMI. The PREMIUM item bank regarding information included 25 items. A total of 499 patients with schizophrenia (53%), bipolar disorders (26%), and major depressive disorders (22%) were recruited from numerous in- and outpatient settings in France. Unidimensionality, local independence, and monotonicity were verified for 19 items of the item bank. The psychometric properties were satisfactory for both internal (RMSEA = 0.069, CFI = 0.969, TLI = 0.963) and external validity (in particular, significant associations were found with age, educational level, and social functioning). The CAT exhibited satisfactory accuracy and precision (standard error of measurement <0.55 and root mean square error <0.3), with an average administration of eight items. This CAT may be used by healthcare professionals in psychiatric settings to accurately assess the patients’ experience with information.
1. Introduction
Schizophrenia, bipolar disorders, and major depressive disorders are severe mental illnesses (SMI) that are characterized by poor quality of care [1,2,3,4]. Previous studies have reported substantial unmet information needs in patients with SMI [5,6]. For example, the need for information has been reported by more than half of patients with schizophrenia in a recent Brazilian study [7]. Sharing information is particularly challenging in patients with SMI because the nature of mental illness is often difficult to explain, and the treatment options and prognosis may vary considerably [8]. Yet, obtaining information about illness, available treatment and care options, prognosis, are strategies for self-management is an essential issue regarding the quality of care because it can affect the process of shared decision making (i.e., “a decision support model allowing information sharing between doctors and patients concerning different care options and taking into account patient preferences”) [9,10] and treatment adherence [11], leading to improved prognosis, including the patients’ quality of life [8]. Poor adherence to treatment may be partly explained by a patient’s belief that the effect of medications is harmful or that medications are unnecessary [12]. It is therefore essential to provide understandable and appropriate information to patients to improve their treatment adherence [13], which remains a major public health problem.
Measuring the quality of information delivered to patients with SMI is an essential step to improve communication strategies for patients with SMI, as well as their quality of care. The French group Patient-Reported Experience Measure for Improving qUality of care in Mental health (PREMIUM) has developed computerized adaptive tests (CATs) for seven domains of quality of care experienced by patients with SMI [14,15]: interpersonal relationships, care environment, drug therapy, access and care coordination, respect and dignity, psychological care, and information. The patient-reported experience measures (PREMs) developed by PREMIUM are expected to optimize measurement precision, to reduce the length of the questionnaire and completion time, and to improve the relevance and the acceptability of these questionnaires in psychiatric settings [16].
In this work, we described the different steps that led to the validation of the PREMIUM CAT for measuring the quality of information delivered to patients with SMI.
2. Methodology
2.1. Study Setting and Population
We performed a national, multicenter, cross-sectional study between January 2016 and December 2021. Patients were recruited from in- and outpatient psychiatric settings in a French teaching hospital (Assistance Publique-Hôpitaux de Marseille), in the 39 FondaMental academic center of expertise for schizophrenia, bipolar disorders and depression [17] and through social networks, including patients’ associations and with an online web survey. The study protocol was described in more detail elsewhere [14]. All participants gave their informed consent, and the study was carried out in accordance with the Declaration of Helsinki and approved by the local ethics committee (authorization number: 2014-A01152-45).
The inclusion criteria were patients over the age of 18 and under the age of 65, with a DSM-5 diagnosis of schizophrenia, bipolar disorders, or major depressive disorders [18] and having in- or outpatient psychiatric care, informed consent, and speaking/reading French.
2.2. Items Measuring the Quality of Information Delivered to Patients with SMI (PREMIUM Item Bank Regarding Information)
The PREMIUM item bank regarding information included 25 items that were self-administered to patients with SMI. The development of the items was detailed in previous works and is based on a mixed method approach associating qualitative and quantitative methodologies [14,15]. All items are presented in Table 1 and scored on a 5-point Likert scale (“strongly disagree”, “disagree”, “neither agree nor disagree”, “agree”, “strongly agree”) with a “not applicable” response option. In addition to these 25 items, we collected an overall satisfaction item (“Overall, were you satisfied with the information about your illness and your management?”) and a visual analogue scale (VAS) (0 minimum to 10 maximum).

Table 1.
List of items. You have been sufficiently informed about.
2.3. Collected Data
The following sociodemographic and clinical data were collected: sex, age, educational level, marital status, occupational status, diagnosis (schizophrenia, bipolar disorders, or major depressive disorders), duration of illness, the Global Assessment of Functioning scale [19] (GAF, ranging from 0 to 100, with a higher score indicating better functioning), quality of life (QoL) using the medical outcome study 12-item Short Form (SF-12) [20], which describes eight dimensions—physical functioning, social functioning, physical role, emotional role, mental health, vitality, bodily pain, general health—and two composite scores for physical and mental quality of life (ranging from 0 to 100, with higher scores indicating a better quality of life).
2.4. Statistical Analysis
Descriptive statistics of the sample included frequencies and percentages of categorical variables and the means and standard deviations of continuous variables.
All the items of the PREMIUM item bank regarding information were analyzed using descriptive indicators to select the high performing items.
The item response theory (IRT) assumptions were assessed [21]: unidimensionality using confirmatory factor analysis (CFA) or exploratory factor analysis (EFA), followed by bifactor structure (i.e., one general factor and several group factors), local independence using residual correlations from the CFA model, and monotonicity using visual inspection of characteristic item curves. The generalized partial credit model (GPCM) was used to calibrate the responses to the items [22] after having verified its superiority over other models, such as the partial credit model (PCM) [23]. Item parameters (discrimination and thresholds) were estimated using the maximum marginal likelihood estimation (MMLE) and the expectation–maximization (EM) algorithm [24], and then the model fit to the data was evaluated.
Differential item functioning (DIF) analyses were performed using ordinal logistic regression models [25,26] according to sex (male vs. female), age (median split: patients 40 years or younger vs. patients older than 40 years), care setting (outpatient vs. inpatient), and psychiatric diagnosis (schizophrenia vs. bipolar disorders vs. major depressive disorders). Latent trait scores (θ) were estimated by Bayesian expected a posteriori (EAP) estimation [27]. Then, a linear transformation was performed to obtain θ scores ranging from 0 to 100 (the higher the score was, the better the experience regarding information received). All the indicators of psychometric performance are presented in Supplementary Table S1 [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
Convergent validity was investigated by examining the relationships between item bank scores and psychosocial functioning (GAF), quality of life (SF-12), and satisfaction (overall satisfaction item and VAS). Discriminant validity was investigated by comparing the mean scores of the item bank scores, according to sociodemographic and clinical characteristics, using t tests, analysis of variance (ANOVA), and Pearson’s correlation coefficients.
Finally, we developed the item administration algorithm of the CAT. The starting item was the most informative item based on the maximum Fisher information (MFI) criterion [46]. The CAT algorithm then selected the next item with the highest information for the current θ estimate. The CAT algorithm ended when the stopping rule based on the standard error of measurement (SEM) was reached (acceptable range between 0.33 to 0.55 [47]). Three scenarios with different stopping rules corresponding to SEM values of 0.33, 0.44, and 0.55 were simulated and compared to select the best adaptive administration algorithm. The indicators used to assess the performance of the results at each stage of the statistical analyses are provided in Supplementary Table S1 [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
All of the statistical analyses were performed using the following software: IBM PASW SPSS version 20.0 [48], MPlus version 7.0 [49], and R version 4.0.5 [50], using packages “mirt” [51], “lordif” [52], “BifactorIndicesCalculator”, [53] and “mirtCAT” [54].
3. Results
3.1. Sample Characteristics
A total of 499 patients with schizophrenia (53%), bipolar disorders (26%) and major depressive disorders (22%) were recruited. The characteristics of the participants are presented in Table 2.

Table 2.
Sample description (N = 499).
3.2. Descriptive Indicators of the PREMIUM Item Bank Regarding Information
All the indicators are presented in Supplementary Table S2 and were satisfactory, except that six items (i.e., I2, I4, I10, I15, I17, and I21) exhibited inter-item correlations that were too high (>0.70), reflecting redundancy between items, and they were thus removed. The lowest scores were reported for item 24 (information about the possibility to access your medical file), item 21 (information about the possibilities of arranging your working time) and item 25 (information about associations and self-help groups.
3.3. Assumptions Assessment and Calibration of the IRT Model
Unidimensionality, local independence, and monotonicity were inspected for the remaining 19 items. The fit indices of the 1-factor CFA model were not adequate (RMSEA = 0.126, 95% CI [0.117–0.135], CFI = 0.911, and TLI = 0.900) and were improved with a bifactor structure using one general factor and two group factors (RMSEA = 0.076, 95% CI [0.065–0.086], CFI = 0.975, TLI = 0.968). In the EFA, three factors had eigenvalues greater than 1 (9.0, 1.5, and 1.2, respectively), and the ratio of the first to second eigenvalue was 5.9. The scree plot revealed two predominant factors, while the parallel analysis revealed four predominant factors. All items had higher factor loadings for the general factor than for the group factors. The coefficient ωh for the general factor was 0.93, and those on the two group factors were 0.03 and 0.21, respectively. The percentage of ECV attributable to the general factor was 85.4%, whereas the remaining 14.6% was attributable to the two group factors (7.3% and 10.6%, respectively). All items in the bank were then recoded after examination of the item characteristic curves, which led to an improved model fit (Akaike information criterion, AIC = −8726.88 and Bayes information criterion, BIC = −8886.95). Finally, all residuals were lower than 0.20, and the Cronbach’s alpha was 0.94.
3.4. Calibration and Fitting an IRT Model
The GPCM showed a better fit to the data compared to PCM (14,433.67 and 14,539.12 for the AIC and 14,673.79 and 14,703.42 for the BIC, respectively), also supported by the X2 = 141.45, p < 0.001. In addition, all items showed an adequate fit to the GPCM, with infit values ranging from 0.78 (item I14) to 1.15 (item I1). The item parameters are presented in Supplementary Table S3.
3.5. Differential Item Functioning
Of the 76 tests performed (i.e., 19 final items of the item bank with 4 confounding factors), 12 exhibited overall DIF but with negligible magnitudes: 5 items for sex (items 3, 16, 19, 22, and 24), 1 item for age (item 7), 5 items for care setting (items 7, 16, 18, 19, and 22) and 5 items for diagnosis (items 5, 12, 20, 22, and 25). All the DIF results are presented in Supplementary Table S4.
The test information curve of the item bank confirmed that the items have a high measurement precision over a broad spectrum of the latent trait (61.0% of total information is included in the [−2,2] range of the latent continuum values) (Figure 1). Item 13 was the most informative of the bank—“the course of your care (how to take your drug therapy, the frequency of your appointments, etc.”, whereas item 20 was the least informative—“existing medical-social aid (reimbursement of health care costs, access to home help, obtaining the disabled adult allowance, etc.”).
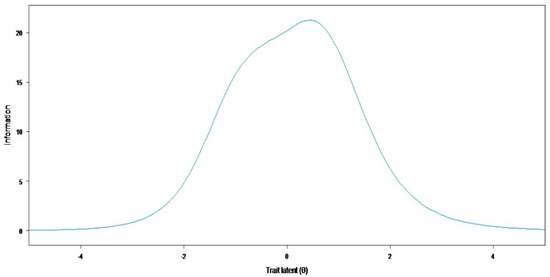
Figure 1.
Test information.
3.6. External Validity of the PREMIUM Item Bank Regarding Information
The mean score was 46.97 ± 19.82. The scores were strongly correlated with overall satisfaction and the corresponding VAS, confirming the convergent validity. All the SF-12 dimensions were significantly correlated with information experience, but the relationships were stronger regarding social and emotional functioning.
Concerning discriminant validity, younger age, higher educational level, and online survey were associated with poorer information experience. No significant differences were found by sex, marital status, employment status, care setting, diagnosis, duration of illness, and psychosocial functioning. The results regarding the external validation are presented in Table 3.

Table 3.
External validity.
3.7. Elaboration of the Item Administration Algorithm
Among the three scenarios tested, the CAT simulation with a level of precision of SEM < 0.33 was the most efficient, with the highest levels of accuracy (r = 0.97) and precision (RMSE = 0.23) while administering eight items, on average. Table 4 provides the results of the CAT simulations.

Table 4.
Mean scores and precision indicators for each CAT simulation.
4. Discussion
In this study, we demonstrated the validity of the PREMIUM-CAT for measuring the quality of information delivered to patients with SMI. This CAT presents interesting characteristics for widespread use in psychiatric settings.
The PREMIUM item bank has been developed based on a literature review and patient interviews, ensuring its content validity [15,55]. Similar to a previous study on information needs in mental health [56], the PREMIUM item bank regarding information explores a broad facet of the information delivered to patients, including: basic facts (e.g., diagnosis, symptoms, etc.), treatment (e.g., side effects, etc.), coping (e.g., lifestyle advice, etc.), medical systems (e.g., possibility of accessing medical file, etc.), social aids, professional accommodations, and peer support. The basic facts are the information needs most frequently reported in the literature in contrast to self-help and peer support [56]. These findings are corroborated by our study in which the item regarding the course of care (I13) was the most informative of the bank, while the item on social aids (I20) was the least informative of the bank. Measurement invariance was demonstrated by the few indications of negligible magnitude DIF, which implies that the psychometric properties of the items are invariant across gender, age, care setting, and diagnosis, and that the item bank scores can be compared between respondents, regardless of their characteristics. The different sampling strategies may also have impacted participants’ information experience at different levels. Response bias is known to affect self-reported data, leading to results biased in a positive direction, as in traditional satisfaction surveys [57]. Participants recruited from healthcare facilities are more likely to provide biased responses due to concerns about the impact on their care and relationships with the healthcare team. Participants recruited from healthcare were invited to participate in the study by a psychologist external to the healthcare team in order to limit this bias. However, the scores were significantly higher for participants from the healthcare facilities than for participants from the online survey. External validity, explored by the use of socio-demographic characteristics and established psychiatric and functioning measures, globally confirmed our assumptions. In particular, we confirmed that information experience was slightly and positively correlated to quality of life, which has been shown in other chronic severe illnesses, such as cancer [58]. Conversely, our results showed no statistical difference in information experience according to psychosocial functioning, even though most participants had poor psychosocial functioning. Our results also showed that participants with high educational level and young age reported a poorer information experience. Patients’ preference about information may vary according to age and education [59]. Health literacy and internet use may also explain these results, in part [60,61,62,63]. Innovative information strategies could be implemented in novel digital adherence-assessment devices [64] and telemedicine interventions [65]. Finally, the item bank offers better precision and accuracy measurement over the [−2;2] range of theta values, while reducing response burden on participants, with an average of 8 items administered.
The analysis of the item scores has yielded three points of information that should be targeted with high priority. First, participants reported poor information experience on the right to access her/his medical file. All physicians are informed during their training of the 2003 Kouchner Law obliging institutions to provide medical records within 8 days to any patient on demand. The reasons for this poorer experience should be explored in future studies. However, it seems necessary to reinforce the information of this right to all patients, perhaps by automatic mailing or phone texting, for instance. Second, participants reported poor information experience regarding social aids and professional accommodations. This information is not directly related to medical care, but rather to medico-social/social/rehabilitation care and occupational medicine. Poor access to medico-social and social care and lack of knowledge regarding these services may explain why patients report poorer information experience regarding this information. All patients could be delivered systematic written information regarding social aids and professional accommodations when receiving her/his first diagnosis. Third, participants reported poorer information experience regarding associations or programs aimed at helping patients. This poor experience may be due to a lack of knowledge. Physicians are themselves poorly informed about all associations, programs, and initiatives concerning all mental illnesses. This information also may vary across time and geographical areas. Caregivers may also estimate that their role is limited to medical care. Future qualitative studies should explore the reasons obehind this poorer experience and how to address this issue.
4.1. Futures Directions
The item bank and its CAT version provide a brief, accurate, and flexible assessment of the information experience of patients with SMI, suitable for research and clinical practice. The systematic and continuous collection of PREMs through a digital platform has great potential to inform quality improvement actions in mental health care [66]. However, the CAT version requires an appropriate information technology (IT) infrastructure to collect data, at the hospital and/or at home, requiring that patients have internet access. Future dissemination and implementation work will need to determine the feasibility of such a device for routine use and its effectiveness in meeting specific research or clinical needs.
4.2. Limitations
Our sample size is large compared to traditional psychiatric studies, but may be limited in the field of psychometric studies. However, our sample size was sufficient, since sample size requirements recommend approximately 500 observations for accurate parameter estimates with multiparameter models (e.g., GPCM) [67,68]. In addition, the sample included a diverse patient population, both inpatient and outpatient, from several facilities in different geographic regions of the country. Future work with a larger and more diverse sample will allow for additional psychometric testing to develop a better understanding of the metric properties, but also to examine the generalizability of this item bank to other populations, such as patients with common mental disorders (e.g., anxiety disorders). Second, in this study, as in previous PREMIUM studies [12,69], we used the GPCM, which showed an adequate fit to the data and whose fit can be compared to the PCM because these are nested models. The graded response model (GRM), which tends to provide similar results, could have been an alternative (e.g., in case of non-convergence) [70]. Third, criterion validity could not be assessed because, to the best of our knowledge, no gold standard was available. In addition, given the cross-sectional study design, responsiveness could not be studied. Fourth, CAT precision depends on the quality of the related item bank, which showed the highest measurement precision in the [−2;2] range of theta values. Future studies should evaluate whether additional items are needed to cover the ends of the latent continuum. Fifth, we did not evaluate health literacy, which may have influenced information experience [71]. Likewise, symptom severity was not measured using psychiatric scales (e.g., PANSS, MADRS, YMRS) due to diagnostic heterogeneity and different recruitment strategies that did not allow for hetero-assessment. By using the GAF, which provides an approximate measure of the severity of these symptoms, we examined the impact of the severity of mental illness on the information experience. Future studies should address these questions. Finally, the precision and accuracy of the CAT should be re-evaluated in an independent sample and under real-world conditions to assess whether the responses may be affected by other factors [72].
5. Conclusions
The PREMIUM item bank regarding information and its CAT version may be used by healthcare professionals in psychiatric settings to accurately assess the experience of patients with information. Particular attention should be paid to informing patients about their right to access their medical files, social aids, professional accommodations, and peer support services.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11226687/s1, Table S1: Indicators of psychometric performance; Table S2: Descriptive statistics of the item bank; Table S3: Parameter estimates (discrimination and threshold) and fit statistics for the 19 items in the final item bank; Table S4: DIF results.
Author Contributions
Conceptualization: L.B.; methodology: L.B.; validation: L.B., S.F., B.X.T. and G.F.; formal analysis: S.F.; data curation: G.F.; writing—original draft preparation: L.B.; writing—review and editing: L.B., S.F. and G.F.; supervision: L.B.; project administration: L.B.; funding acquisition: L.B. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by an institutional grant from The French National Program on the Performance of the Health Care System (PREPS, financed by Direction Générale de l’Offre de Soins, 14, avenue Duquesne, 75350 Paris, France) and the Agence Technique de l’Information sur l’Hospitalisation (ATIH). The sponsors had no role in the study design; collection, analysis, and interpretation of data; report writing; or the decision to submit the article for publication.
Institutional Review Board Statement
The trial registration is NCT02491866. The assessment protocol was approved by the relevant ethical review board (CPP-Sud Méditerranée V, n°2014-A01152-45). All data were collected anonymously.
Informed Consent Statement
Informed consent was given by all participants.
Data Availability Statement
The data are available on demand from the PREMIUM Scientific Committee.
Acknowledgments
We wish to thank the collaborators of the French PREMIUM Group (Patient-Reported Experience Measure for Improving qUality of care in Mental health): Baumstarck Karine, Boucekine Mohamed, Cano Delphine, Coldefy Magali, Lançon Christophe, Michel Pierre, Pascal Auquier, and Pierre-Michel LLorca.
Conflicts of Interest
The authors report no conflict of interest in this work.
References
- Kilbourne, A.M.; Beck, K.; Spaeth-Rublee, B.; Ramanuj, P.; O’Brien, R.W.; Tomoyasu, N.; Pincus, H.A. Measuring and improving the quality of mental health care: A global perspective. World Psychiatry 2018, 17, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Moitra, M.; Santomauro, D.; Collins, P.Y.; Vos, T.; Whiteford, H.; Saxena, S.; Ferrari, A.J. The global gap in treatment coverage for major depressive disorder in 84 countries from 2000–2019: A systematic review and bayesian meta-regression analysis. PLoS Med. 2022, 19, e1003901. [Google Scholar] [CrossRef] [PubMed]
- Borges, G.; Aguilar-Gaxiola, S.; Andrade, L.; Benjet, C.; Cia, A.; Kessler, R.C.; Orozco, R.; Sampson, N.; Stagnaro, J.C.; Torres, Y.; et al. Twelve-month mental health service use in six countries of the Americas: A regional report from the World Mental Health Surveys. Epidemiol. Psychiatr. Sci. 2019, 29, e53. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Mental Health Action Plan 2013–2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/89966/9789241506021_eng.pdf (accessed on 21 October 2022).
- Liebherz, S.; Tlach, L.; Härter, M.; Dirmaier, J. Information and decision-making needs among people with affective disorders—Results of an online survey. Patient Prefer. Adherence 2015, 1, 627–638. [Google Scholar] [CrossRef]
- Fleury, M.J.; Grenier, G.; Bamvita, J.M.; Perreault, M.; Caron, J. Variables associated with perceived unmet need for mental health care in a canadian epidemiologic catchment area. Psychiatry Serv. 2016, 67, 78–85. [Google Scholar] [CrossRef]
- Andrade, M.C.R.; Slade, M.; Bandeira, M.; Evans-Lacko, S.; Martin, D.; Andreoli, S.B. Need for information in a representative sample of outpatients with schizophrenia disorders. Int. J. Soc. Psychiatry 2018, 64, 476–481. [Google Scholar] [CrossRef]
- Farooq, S.; Johal, R.K.; Ziff, C.; Naeem, F. Different communication strategies for disclosing a diagnosis of schizophrenia and related disorders. Cochrane Database Syst. Rev. 2017, 10, CD011707. [Google Scholar] [CrossRef]
- Aoki, Y. Shared decision making for adults with severe mental illness: A concept analysis. Jpn. J. Nurs. Sci. 2020, 17, e12365. [Google Scholar] [CrossRef]
- Thomas, E.C.; Ben-David, S.; Treichler, E.; Roth, S.; Dixon, L.B.; Salzer, M.; Coldefy, M. A systematic review of shared decision–making interventions for service users with serious mental illnesses: State of the science and future directions. Psychiatry Serv. 2021, 72, 1288–1300. [Google Scholar] [CrossRef]
- El-Mallakh, P.; Findlay, J. Strategies to improve medication adherence in patients with schizophrenia: The role of support services. Neuropsychiatr. Dis. Treat. 2015, 11, 1077–1090. [Google Scholar] [CrossRef]
- Fernandes, S.; Fond, G.; Zendjidjian, X.; Michel, P.; Baumstarck, K.; Lançon, C.; Samalin, L.; Llorca, P.-M.; Coldefy, M.; Auquier, P.; et al. Development and calibration of the PREMIUM item bank for measuring respect and dignity for patients with severe mental illness. JCM 2022, 11, 1644. [Google Scholar] [CrossRef] [PubMed]
- Kikkert, M.J.; Schene, A.H.; Koeter, M.W.J.; Robson, D.; Born, A.; Helm, H.; Nose, M.; Goss, C.; Thornicroft, G.; Gray, R.J. Medication adherence in schizophrenia: Exploring patients’, carers’ and professionals’ views. Schizophr. Bull. 2005, 32, 786–794. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, S.; Fond, G.; Zendjidjian, X.; Michel, P.; Baumstarck, K.; Lancon, C.; Berna, F.; Schurhoff, F.; Aouizerate, B.; Henry, C.; et al. The Patient-Reported Experience Measure for Improving quality of care in Mental health (PREMIUM) project in France: Study protocol for the development and implementation strategy. Patient Prefer. Adherence 2019, 13, 165–177. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, S.; Fond, G.; Zendjidjian, X.; Michel, P.; Lançon, C.; Berna, F.; Schurhoff, F.; Aouizerate, B.; Henry, C.; Etain, B.; et al. A conceptual framework to develop a patient-reported experience measure of the quality of mental health care: A qualitative study of the PREMIUM project in France. J. Mark. Access Health Policy 2021, 9, 1885789. [Google Scholar] [CrossRef] [PubMed]
- Cella, D.; Gershon, R.; Lai, J.S.; Choi, S. The future of outcomes measurement: Item banking, tailored short-forms, and computerized adaptive assessment. Qual. Life Res. 2007, 16 (Suppl. 1), S133–S141. [Google Scholar] [CrossRef]
- Schürhoff, F.; Fond, G.; Berna, F.; Bulzacka, E.; Godin, O.; Boyer, L.; Misdrahi, D.; Andrianarisoa, M.; Brunel, L.; Coulon, N.; et al. The 10-year findings from the FondaMental academic center of expertise for schizophrenia (FACE-SZ): Review and recommendations for clinical practice. Encephale 2019, 45, 9–14. [Google Scholar] [CrossRef]
- American Psychiatric Association. DSM-5: Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Endicott, J.; Spitzer, R.; Fleiss, J.; Cohen, J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch. Gen. Psychiatry 1976, 33, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Kosinski, M.; Keller, S.D. How to Score the SF-12 Physical and Mental Health Summary Scales, 2nd ed.; The Health Institute, New England Medical Center: Boston, MA, USA, 1995. [Google Scholar]
- Embretson, S.E.; Reise, S.P. Item Response Theory for Psychologists; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2000. [Google Scholar]
- Muraki, E. A generalized partial credit model: Application of an EM algorithm. Appl. Psychol. Meas. 1992, 16, 159–176. [Google Scholar] [CrossRef]
- Masters, G.N. A rasch model for partial credit scoring. Psychometrika 1982, 47, 149–174. [Google Scholar] [CrossRef]
- Bock, R.D.; Aitkin, M. Marginal maximum likelihood estimation of item parameters: Application of an EM algorithm. Psychometrika 1981, 46, 443–459. [Google Scholar] [CrossRef]
- Zieky, M. Differential item functioning. In Practical Questions in the Use of DIF Statistics in Test Development; Holland, P.W., Wainer, H., Eds.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1993; pp. 337–347. [Google Scholar]
- Rogers, H.J. Differential item functioning. In Encyclopedia of Statistics in Behavioral Science; Everitt, B.S., Howell, D.C., Eds.; John Wiley & Sons, Ltd.: Chichester, UK, 2005; pp. 485–490. [Google Scholar]
- Bock, R.D.; Mislevy, R.J. Adaptive EAP estimation of ability in a microcomputer environment. Appl. Psychol. Meas. 1982, 6, 431–444. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, R.M. Structural equation modelling: Guidelines for determining model fit. Electron J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar]
- Kline, R. Principles and Practice of Structural Equation Modeling, 2nd ed.; Guilford Press: New York, NY, USA, 2005. [Google Scholar]
- Reeve, B.B.; Hays, R.D.; Bjorner, J.B.; Cook, K.F.; Crane, P.K.; Teresi, J.A.; Thissen, D.; Revicki, D.A.; Weiss, D.J.; Hambleton, R.K.; et al. Psychometric evaluation and calibration of health-related quality of life item banks: Plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Med. Care 2007, 45 (Suppl. 1), S22–S31. [Google Scholar] [CrossRef] [PubMed]
- Reise, S.P.; Morizot, J.; Hays, R.D. The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Qual. Life Res. 2007, 16 (Suppl. 1), 19–31. [Google Scholar] [CrossRef]
- Reise, S.P.; Scheines, R.; Widaman, K.F.; Haviland, M.G. Multidimensionality and structural coefficient bias in structural equation modeling: A bifactor perspective. Educ. Psychol. Meas. 2013, 73, 5–26. [Google Scholar] [CrossRef]
- Rodriguez, A.; Reise, S.P.; Haviland, M.G. Applying bifactor statistical indices in the evaluation of psychological measures. J. Personal. Assess. 2016, 98, 223–237. [Google Scholar] [CrossRef]
- Bjorner, J.B.; Kosinski, M.; Ware, J.E., Jr. Calibration of an item pool for assessing the burden of headaches: An application of item response theory to the headache impact test (HIT). Qual. Life Res. 2003, 12, 913–933. [Google Scholar] [CrossRef]
- Fliege, H.; Becker, J.; Walter, O.B.; Bjorner, J.B.; Klapp, B.F.; Rose, M. Development of a computer-adaptive test for depression (D-CAT). Qual. Life Res. 2005, 14, 2277–2291. [Google Scholar] [CrossRef]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Automat. Contr. 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Schwarz, G. Estimating the dimension of a model. Ann. Statist. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Ware, J.E.; Bjorner, J.B.; Kosinski, M. Practical implications of item response theory and computerized adaptive testing: A brief summary of ongoing studies of widely used headache impact scales. Med. Care. 2000, 38 (Suppl. II), 73–82. [Google Scholar] [CrossRef]
- Baker, F.B. The Basics of Item Response Theory, 2nd ed.; ERIC Clearinghouse on Assessment and Evaluation: Washington, DC, USA, 2001.
- Chang, H.H.; Ying, Z. A global information approach to computerized adaptive testing. Appl. Psychol. Meas. 1996, 20, 213–229. [Google Scholar] [CrossRef]
- Bond, T.G.; Fox, C.M. Applying the Rasch Model: Fundamental Measurement in the Human Sciences, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2007. [Google Scholar]
- Wright, B.D.; Linacre, J.M. Reasonable mean-square fit values. Rasch Meas. Trans. 1994, 8, 370. [Google Scholar]
- Zumbo, B. A Handbook on the Theory and Methods of Differential Item Functioning (DIF): Logistic Regression Modeling as a Unitary Framework for Binary and Likert-Type (Ordinal) Item Scores; Directorate of Human Resources Research and Evaluation, Department of National Defense: Ottawa, ON, Canada, 1999.
- Choi, S.W.; Reise, S.P.; Pilkonis, P.A.; Hays, R.D.; Cella, D. Efficiency of static and computer adaptive short forms compared to full-length measures of depressive symptoms. Qual. Life Res. 2010, 19, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.W.; Swartz, R.J. Comparison of CAT item selection criteria for polytomous items. Appl. Psychol. Meas. 2009, 33, 419–440. [Google Scholar] [CrossRef] [PubMed]
- Harvill, L.M. Standard error of measurement. Educ. Meas. Issues 1991, 10, 33–41. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows; Version 20.0; IBM Corp.: Armonk, NJ, USA, 2011. [Google Scholar]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2012. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Chalmers, R.P. Mirt: A multidimensional item response theory package for the R environment. J. Stat. Softw. 2012, 48, 1–29. [Google Scholar] [CrossRef]
- Choi, S.W.; Gibbons, L.E.; Crane, P.K. Lordif: An R package for detecting differential item functioning using iterative hybrid ordinal logistic regression/item response theory and monte carlo simulations. J. Stat. Softw. 2011, 39, 1–30. [Google Scholar] [CrossRef]
- Dueber, D. BifactorIndicesCalculator: A Package for Computing Statistical Indices Relevant to Bifactor Measurement Models. Available online: https://cran.r-project.org/web/packages/BifactorIndicesCalculator/BifactorIndicesCalculator.pdf (accessed on 12 January 2022).
- Chalmers, R.P. Generating adaptive and non-adaptive test interfaces for multidimensional item response theory applications. J. Stat. Softw. 2016, 71, 1–38. [Google Scholar] [CrossRef]
- Fernandes, S.; Fond, G.; Zendjidjian, X.; Baumstarck, K.; Lançon, C.; Berna, F.; Schurhoff, F.; Aouizerate, B.; Henry, C.; Etain, B.; et al. Measuring the patient experience of mental health care: A systematic and critical review of patient-reported experience measures. Patient Prefer. Adherence 2020, 14, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Tlach, L.; Wüsten, C.; Daubmann, A.; Liebherz, S.; Härter, M.; Dirmaier, J. Information and decision-making needs among people with mental disorders: A systematic review of the literature. Health Expect 2015, 18, 1856–1872. [Google Scholar] [CrossRef] [PubMed]
- Mazor, K.M.; Clauser, B.E.; Field, T.; Yood, R.A.; Gurwitz, J.H. A demonstration of the impact of response bias on the results of patient satisfaction surveys. Health Serv. Res. 2002, 37, 1403–1417. [Google Scholar] [CrossRef] [PubMed]
- Husson, O.; Mols, F.; van de Poll-Franse, L.V. The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: A systematic review. Ann. Oncol. 2011, 22, 761–772. [Google Scholar] [CrossRef]
- Borracci, R.A.; Manente, D.; Giorgi, M.A.; Calderón, G.; Ciancio, A.; Doval, H.C. Patients’ preferences for information in health care decision-making. Medicina 2012, 72, 393–398. [Google Scholar] [PubMed]
- Assi, S.; Thomas, J.; Haffar, M.; Osselton, D. Exploring consumer and patient knowledge, behavior, and attitude toward medicinal and lifestyle products purchased from the internet: A web-based survey. JMIR Public Health Surveill. 2016, 2, e34. [Google Scholar] [CrossRef]
- Ilic, D. The role of the internet on patient knowledge management, education, and decision-making. Telemed. J. e-Health 2010, 16, 664–669. [Google Scholar] [CrossRef]
- Fulford, H.; McSwiggan, L.; Kroll, T.; MacGillivray, S. Exploring the use of mobile information and communication technologies by people with mood disorders. Int. J. Ment. Health Nurs. 2019, 28, 1268–1277. [Google Scholar] [CrossRef]
- Villani, M.; Kovess-Masfety, V. How do people experiencing schizophrenia spectrum disorders or other psychotic disorders use the internet to get information on their mental health? Literature review and recommendations. JMIR Ment. Health 2017, 4, e1. [Google Scholar] [CrossRef]
- Papola, D.; Gastaldon, C.; Ostuzzi, G. Can a digital medicine system improve adherence to antipsychotic treatment? Epidemiol. Psychiatr. Sci. 2018, 27, 227–229. [Google Scholar] [CrossRef]
- Basit, S.A.; Mathews, N.; Kunik, M.E. Telemedicine interventions for medication adherence in mental illness: A systematic review. Gen. Hosp. Psychiatry 2020, 62, 28–36. [Google Scholar] [CrossRef]
- De Rosis, S.; Cerasuolo, D.; Nuti, S. Using patient-reported measures to drive change in healthcare: The experience of the digital, continuous and systematic PREMs observatory in Italy. BMC Health Serv. Res. 2020, 20, 315. [Google Scholar] [CrossRef] [PubMed]
- Cappelleri, J.C.; Jason Lundy, J.; Hays, R.D. Overview of classical test theory and item response theory for the quantitative assessment of items in developing patient-reported outcomes measures. Clin. Ther. 2014, 36, 648–662. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.H.; Han, H.R.; Kim, M.T.; Chan, K.S. An introduction to item response theory for patient-reported outcome measurement. Patient 2014, 7, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, S.; Boyer, L.; Zendjidjian, X.; Loundou, A.; Riedberger, J.; Llorca, P.M.; Auquier, P.; Fond, G.; Collaborators of the French PREMIUM Group. Calibration and Validation of a PREMIUM-DT Item Bank to Measure the Experience of Drug Therapy for Patients with Severe Mental Illness. JCM 2022, 11, 4278. [Google Scholar] [CrossRef]
- Dai, S.; Vo, T.T.; Kehinde, O.J.; He, H.; Xue, Y.; Demir, C.; Wang, X. Performance of polytomous IRT Models with rating scale data: An investigation over sample size, instrument length, and missing data. Front. Educ. 2021, 6, 721963. [Google Scholar] [CrossRef]
- Diviani, N.; van den Putte, B.; Giani, S.; van Weert, J.C. Low health literacy and evaluation of online health information: A systematic review of the literature. J. Med. Internet Res. 2005, 17, e112. [Google Scholar] [CrossRef]
- Smits, N.; Cuijpers, P.; van Straten, A. Applying computerized adaptive testing to the CES-D scale: A simulation study. Psychiatry Res. 2011, 188, 147–155. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).