Pathophysiology, Diagnosis and Treatment of Spontaneous Coronary Artery Dissection in Peripartum Women
Abstract
1. Introduction
2. Epidemiology
3. Pathophysiology
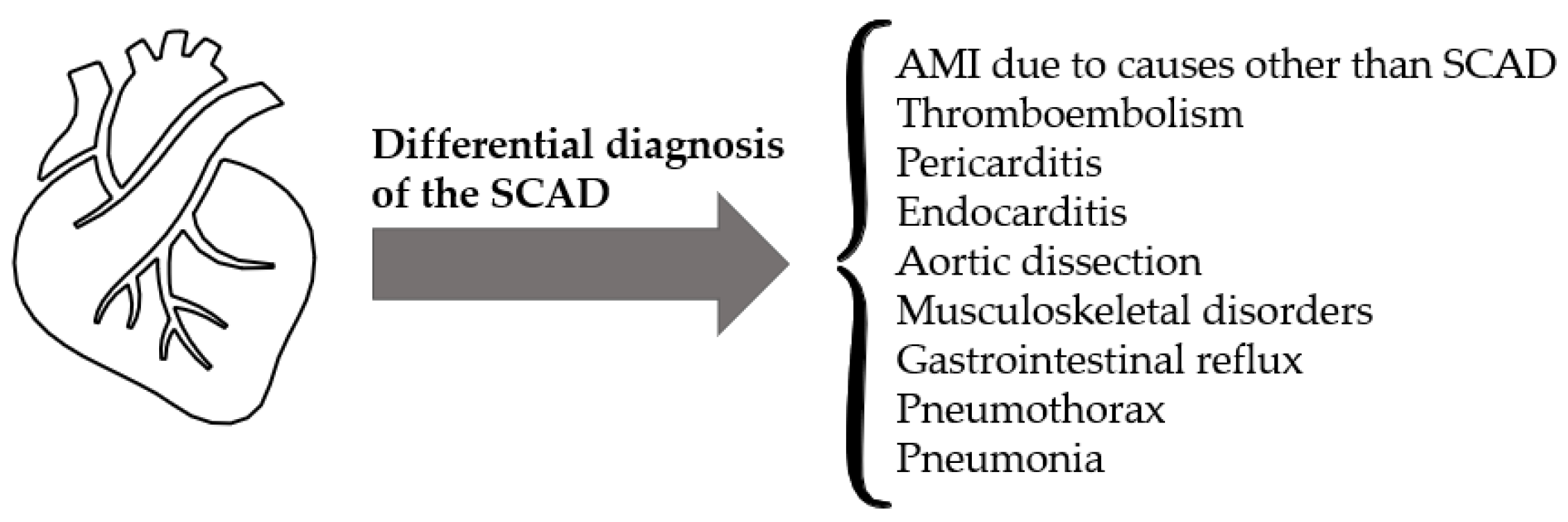
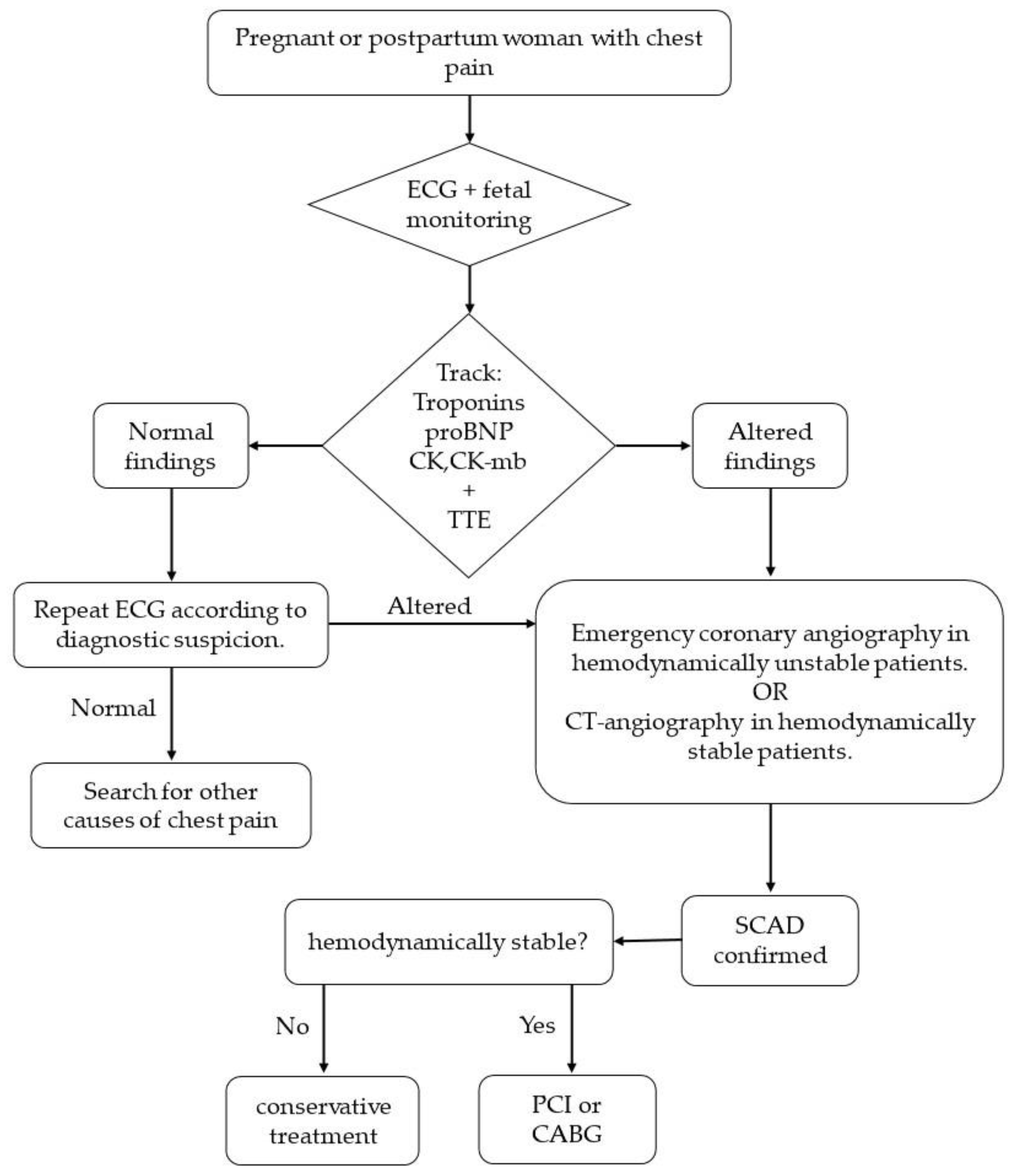
4. Clinical Presentation
5. Diagnosis
6. Treatment
6.1. Conservative Treatment
6.2. Invasive Treatment
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wilkins, E.; Wilson, L.; Wickramasinghe, K.; Bhatnagar, P.; Leal, J.; Luengo-Fernandez, R.; Burns, R.; Rayner, M.; Townsend, N. European Cardiovascular Disease Statistics 2017; European Heart Network: Brussels, Belgium, 2017. [Google Scholar]
- Fernando, L.; Pamela, S.; Alejandra, L. Cardiovascular disease in Latin America: The growing epidemic. Prog. Cardiovasc. Dis. 2014, 57, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Pagliaro, B.R.; Cannata, F.; Stefanini, G.G.; Bolognese, L. Myocardial ischemia and coronary disease in heart failure. Heart Fail. Rev. 2020, 25, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Shahzad, K.; Cao, L.; Ain, Q.T.; Waddy, J.; Khan, N.; Nekkanti, R. Postpartum spontaneous dissection of the first obtuse marginal branch of the left circumflex coronary artery causing acute coronary syndrome: A case report and literature review. J. Med. Case Rep. 2013, 7, 82. [Google Scholar] [CrossRef] [PubMed]
- Pitts, S.R.; Niska, R.W.; Xu, J.; Burt, C.W. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. In National Health Statistics Reports; Inter-University Consortium for Political and Social Research: Ann Arbor, MI, USA, 2008; pp. 1–38. [Google Scholar]
- Mendis, S.; Puska, P.; Norrving, B.; World Health Organization. Global Atlas on Cardiovascular Disease Prevention and Control; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Tsao, C.W.; Vasan, R.S. Cohort Profile: The Framingham Heart Study (FHS): Overview of milestones in cardiovascular epidemiology. Int. J. Epidemiol. 2015, 44, 1800–1813. [Google Scholar] [CrossRef]
- Wilson, P.W.; Garrison, R.J.; Castelli, W.P.; Feinleib, M.; McNamara, P.M.; Kannel, W.B. Prevalence of coronary heart disease in the Framingham Offspring Study: Role of lipoprotein cholesterols. Am. J. Cardiol. 1980, 46, 649–654. [Google Scholar] [CrossRef]
- Shao, C.; Wang, J.; Tian, J.; Tang, Y.D. Coronary Artery Disease: From Mechanism to Clinical Practice. Adv. Exp. Med. Biol. 2020, 1177, 1–36. [Google Scholar] [CrossRef]
- Cayuela, L.; Gómez Enjuto, S.; Olivares Martínez, B.; Rodríguez-Domínguez, S.; Cayuela, A. ¿Se está desacelerando el ritmo de disminución de la mortalidad cardiovascular en España? Rev. Española Cardiol. 2021, 74, 750–756. [Google Scholar] [CrossRef]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. Guía ESC 2020 sobre el diagnóstico y tratamiento del síndrome coronario agudo sin elevación del segmento ST. Rev. Española Cardiol. 2021, 74, e541–e544. [Google Scholar] [CrossRef]
- Lebrun, S.; Bond, R.M. Spontaneous coronary artery dissection (SCAD): The underdiagnosed cardiac condition that plagues women. Trends Cardiovasc. Med. 2018, 28, 340–345. [Google Scholar] [CrossRef]
- Agewall, S.; Beltrame, J.F.; Reynolds, H.R.; Niessner, A.; Rosano, G.; Caforio, A.L.P.; De Caterina, R.; Zimarino, M.; Roffi, M.; Kjeldsen, K.; et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur. Heart J. 2016, 38, 143–153. [Google Scholar] [CrossRef]
- Ito, H.; Taylor, L.; Bowman, M.; Fry, E.T.; Hermiller, J.B.; Van Tassel, J.W. Presentation and therapy of spontaneous coronary artery dissection and comparisons of postpartum versus nonpostpartum cases. Am. J. Cardiol. 2011, 107, 1590–1596. [Google Scholar] [CrossRef] [PubMed]
- Sucato, V.; Madaudo, C.; Galassi, A.R. Classification, Diagnosis, and Treatment of Coronary Microvascular Dysfunction. J. Clin. Med. 2022, 11, 4610. [Google Scholar] [CrossRef] [PubMed]
- García-Guimaraes, M.; Bastante, T.; Macaya, F.; Roura, G.; Sanz, R.; Barahona Alvarado, J.C.; Tizón, H.; Flores-Ríos, X.; Moreu, J.; Ojeda, S.; et al. Spontaneous coronary artery dissection in Spain: Clinical and angiographic characteristics, management, and in-hospital events. Rev. Esp. Cardiol. (Engl. Ed.) 2021, 74, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Naderi, S. Spontaneous coronary artery dissection and pregnancy. Curr. Treat. Options Cardiovasc. Med. 2017, 19, 69. [Google Scholar] [CrossRef] [PubMed]
- Valappil, S.P.; Iype, M.; Viswanathan, S.; Koshy, A.G.; Gupta, P.N.; Velayudhan, R.V. Coronary angioplasty in spontaneous coronary artery dissection—Strategy and outcomes. Indian Heart J. 2018, 70, 843–847. [Google Scholar] [CrossRef] [PubMed]
- Wisecarver, J.; Jones, J.; Goaley, T.; McManus, B. “Spontaneous” coronary artery dissection. The challenge of detection, the enigma of cause. Am. J. Forensic Med. Pathol. 1989, 10, 60–62. [Google Scholar] [CrossRef]
- Bonnet, J.; Aumailley, M.; Thomas, D.; Grosgogeat, Y.; Broustet, J.P.; Bricaud, H. Spontaneous coronary artery dissection: Case report and evidence for a defect in collagen metabolism. Eur. Heart J. 1986, 7, 904–909. [Google Scholar] [CrossRef]
- Mattfeldt, T.; Schwarz, F.; Kübler, W. Isolated spontaneous coronary artery dissection. A report on the differential diagnosis of coronary heart disease. Klin. Wochenschr. 1986, 64, 186–193. [Google Scholar] [CrossRef]
- Werner, G.S.; Wojcik, J.; Wiegand, V.; Kreuzer, H. Spontaneous coronary artery dissection: A rare cause of myocardial infarct. Z. Kardiol. 1990, 79, 32–36. [Google Scholar]
- Nebeski, D.; Basic, C.; Svanvik, T.; Schaufelberger, M.; Ostgard Thunstrom, E.; SWED-PREG. Incidence of spontaneous coronary artery dissection during pregnancy in Swedish women between 1997 to 2019, a retrospective observational cohort study based on national Swedish health-registers. Eur. Heart J. 2022, 43, ehac544-1172. [Google Scholar] [CrossRef]
- Faden, M.S.; Bottega, N.; Benjamin, A.; Brown, R.N. A nationwide evaluation of spontaneous coronary artery dissection in pregnancy and the puerperium. Heart 2016, 102, 1974–1979. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.H. Spontaneous Coronary-Artery Dissection. N. Engl. J. Med. 2020, 383, 2358–2370. [Google Scholar] [CrossRef] [PubMed]
- Sherif, H.M.; Nguyen, H.C.; Sarter, B.H.; West, J.T.; Lucente, E.; Fink, D.M.; Quesada-Rojas, A.; Banbury, M.K. Spontaneous coronary dissection in late pregnancy: A multidisciplinary approach to management. Ann. Thorac. Surg. 2008, 85, 1793–1794. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.N.; Tweet, M.S.; Adlam, D.; Kim, E.S.H.; Gulati, R.; Price, J.E.; Rose, C.H. Spontaneous Coronary Artery Dissection: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 76, 961–984. [Google Scholar] [CrossRef]
- Adlam, D.; Alfonso, F.; Maas, A.; Vrints, C.; Committee, W. European Society of Cardiology, acute cardiovascular care association, SCAD study group: A position paper on spontaneous coronary artery dissection. Eur. Heart J. 2018, 39, 3353–3368. [Google Scholar] [CrossRef]
- Jofré, M.L.; GonzáLez, B. Disección coronaria espontánea post parto: Reporte de un caso clínico y revisión de la literatura. Rev. Médica Chile 2014, 142, 391–394. [Google Scholar] [CrossRef][Green Version]
- Alsleibi, S.; Dweik, M.; Afifi, M.; Marzuqa, B.; Nassar, H. Postpartum multivessel coronary artery dissection treated with coronary artery bypass grafting. J. Cardiol. Cases 2012, 5, e23–e27. [Google Scholar] [CrossRef]
- Roth, A.; Elkayam, U. Acute myocardial infarction associated with pregnancy. J. Am. Coll. Cardiol. 2008, 52, 171–180. [Google Scholar] [CrossRef]
- Kok, S.N.; Hayes, S.N.; Cutrer, F.M.; Raphael, C.E.; Gulati, R.; Best, P.J.M.; Tweet, M.S. Prevalence and Clinical Factors of Migraine in Patients With Spontaneous Coronary Artery Dissection. J. Am. Heart Assoc. 2018, 7, e010140. [Google Scholar] [CrossRef]
- Lettieri, C.; Zavalloni, D.; Rossini, R.; Morici, N.; Ettori, F.; Leonzi, O.; Latib, A.; Ferlini, M.; Trabattoni, D.; Colombo, P.; et al. Management and Long-Term Prognosis of Spontaneous Coronary Artery Dissection. Am. J. Cardiol. 2015, 116, 66–73. [Google Scholar] [CrossRef]
- Saw, J.; Starovoytov, A.; Humphries, K.; Sheth, T.; So, D.; Minhas, K.; Brass, N.; Lavoie, A.; Bishop, H.; Lavi, S.; et al. Canadian spontaneous coronary artery dissection cohort study: In-hospital and 30-day outcomes. Eur. Heart J. 2019, 40, 1188–1197. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Saw, J. Very early antepartum pregnancy-associated spontaneous coronary artery dissection case report. Cardiovasc. Diagn. Ther. 2018, 8, 512–515. [Google Scholar] [CrossRef] [PubMed]
- D’Ovidio, C.; Sablone, S.; Carnevale, A. Spontaneous coronary artery dissection: Case report and literature review. J. Forensic Sci. 2015, 60, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Esenboga, K.; Baskovski, E.; Özyüncü, N.; Tan, T.S.; Tutar, D.E. Recurrent spontaneous right coronary artery dissection in the postpartum period-Think twice before you revascularize. Anatol. J. Cardiol. 2019, 22, 334–335. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Merchant, M.; Mahrer, K.N.; Lundstrom, R.J.; Naderi, S.; Goh, A.C. Spontaneous Coronary Artery Dissection: Clinical Characteristics, Management, and Outcomes in a Racially and Ethnically Diverse Community-Based Cohort. Perm. J. 2019, 23, 18.278. [Google Scholar] [CrossRef]
- Sharma, S.; Kaadan, M.I.; Duran, J.M.; Ponzini, F.; Mishra, S.; Tsiaras, S.V.; Scott, N.S.; Weinberg, I.; Ghoshhajra, B.; Lindsay, M.; et al. Risk Factors, Imaging Findings, and Sex Differences in Spontaneous Coronary Artery Dissection. Am. J. Cardiol. 2019, 123, 1783–1787. [Google Scholar] [CrossRef]
- McNair, P.W.; Parker, A.; Taylor, A.; Battle, R.; Norton, P.; Sharma, A.M. Spontaneous Coronary Artery Dissection and Its Association With Fibromuscular Dysplasia and Other Vascular Abnormalities. Am. J. Cardiol. 2020, 125, 34–39. [Google Scholar] [CrossRef]
- Fryar, C.D.; Ostchega, Y.; Hales, C.M.; Zhang, G.; Kruszon-Moran, D. Hypertension Prevalence and Control Among Adults: United States, 2015–2016. In NCHS Data Brief; CDC: Atlanta, GA, USA, 2017; pp. 1–8. [Google Scholar]
- Cárdenas Fernández, Y.; Sánchez Redonet, E.M.; Ravelo Dopico, R.; Martínez García, G.; Valdés Carrazana, E.; Rodríguez Cruz, L.O. Disección espontánea de arterias coronarias en el puerperio. Presentación de caso. CorSalud 2019, 11, 179–183. [Google Scholar]
- Zipes, D.P.; Libby, P.; Bonow, R.O.; Mann, D.L.; Tomaselli, G.F. Braunwald. Tratado de Cardiología: Texto de Medicina Cardiovascular; Elsevier Health Sciences: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Manhaes, E.d.B.; Gomes, W.F.; Bezerra, C.G.; Horta, P.E.; Gama, M.N.d.; Cesar, L.A.M.; Perin, M.A.; Silva, E.E.R.d.; Caixeta, A.; Cade, J. Dissecção espontânea de artéria coronária: Abordagem terapêutica e desfechos de uma série consecutiva de casos. Rev. Bras. Cardiol. Invasiva 2014, 22, 32–35. [Google Scholar] [CrossRef][Green Version]
- Bitting, C.P.; Zumwalt, R.E. Repeat Coronary Artery Dissection in Pregnancy: A Case Report and Review of the Literature. J. Forensic Sci. 2017, 62, 1389–1394. [Google Scholar] [CrossRef]
- Sanghavi, M.; Rutherford, J.D. Cardiovascular Physiology of Pregnancy. Circulation 2014, 130, 1003–1008. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Würtz, P.; Auro, K.; Mäkinen, V.P.; Kangas, A.J.; Soininen, P.; Tiainen, M.; Tynkkynen, T.; Jokelainen, J.; Santalahti, K.; et al. Metabolic profiling of pregnancy: Cross-sectional and longitudinal evidence. BMC Med. 2016, 14, 205. [Google Scholar] [CrossRef] [PubMed]
- Petrou, E.; Bousoula, E.; Boutsikou, M.; Iakovou, I.; Kolovou, G.; Pavlides, G. Multivessel spontaneous dissection of the left coronary tree in the postpartum period: Case report and review of the literature. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 3743–3746. [Google Scholar]
- Ghossein-Doha, C.; Khalil, A.; Lees, C.C. Maternal hemodynamics: A 2017 update. Ultrasound Obstet. Gynecol. 2017, 49, 10–14. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Butte, N.F. Carbohydrate and lipid metabolism in pregnancy: Normal compared with gestational diabetes mellitus. Am. J. Clin. Nutr. 2000, 71, 1256S–1261S. [Google Scholar] [CrossRef] [PubMed]
- King, J.C. Physiology of pregnancy and nutrient metabolism. Am. J. Clin. Nutr. 2000, 71, 1218s–1225s. [Google Scholar] [CrossRef]
- Alfonso, F.; Bastante, T.; Rivero, F.; Cuesta, J.; Benedicto, A.; Saw, J.; Gulati, R. Spontaneous coronary artery dissection. Circ. J. Off. J. Jpn. Circ. Soc. 2014, 78, 2099–2110. [Google Scholar] [CrossRef]
- Hedayat, M.; Mahmoudi, M.J.; Rose, N.R.; Rezaei, N. Proinflammatory cytokines in heart failure: Double-edged swords. Heart Fail. Rev. 2010, 15, 543–562. [Google Scholar] [CrossRef]
- Golia, E.; Limongelli, G.; Natale, F.; Fimiani, F.; Maddaloni, V.; Pariggiano, I.; Bianchi, R.; Crisci, M.; D’Acierno, L.; Giordano, R.; et al. Inflammation and cardiovascular disease: From pathogenesis to therapeutic target. Curr. Atheroscler. Rep. 2014, 16, 435. [Google Scholar] [CrossRef]
- Zhou, P.; Pu, W.T. Recounting Cardiac Cellular Composition. Circ. Res. 2016, 118, 368–370. [Google Scholar] [CrossRef]
- Kontrogianni-Konstantopoulos, A.; Benian, G.; Granzier, H. Advances in muscle physiology and pathophysiology. J. Biomed. Biotechnol. 2010, 2010, 780417. [Google Scholar] [CrossRef] [PubMed]
- Taegtmeyer, H.; Sen, S.; Vela, D. Return to the fetal gene program: A suggested metabolic link to gene expression in the heart. Ann. N. Y. Acad. Sci. 2010, 1188, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Sadoshima, J. Mechanisms of physiological and pathological cardiac hypertrophy. Nat. Rev. Cardiol. 2018, 15, 387–407. [Google Scholar] [CrossRef] [PubMed]
- Dorn, G.W. The Fuzzy Logic of Physiological Cardiac Hypertrophy. Hypertension 2007, 49, 962–970. [Google Scholar] [CrossRef]
- Mohammed, S.F.; Hussain, S.; Mirzoyev, S.A.; Edwards, W.D.; Maleszewski, J.J.; Redfield, M.M. Coronary Microvascular Rarefaction and Myocardial Fibrosis in Heart Failure With Preserved Ejection Fraction. Circulation 2015, 131, 550–559. [Google Scholar] [CrossRef]
- Olivetti, G.; Capasso, J.M.; Sonnenblick, E.H.; Anversa, P. Side-to-side slippage of myocytes participates in ventricular wall remodeling acutely after myocardial infarction in rats. Circ. Res. 1990, 67, 23–34. [Google Scholar] [CrossRef]
- Ross, J.; Sonnenblick, E.H.; Taylor, R.R.; Spotnitz, H.M.; Covell, J.W. Diastolic Geometry and Sarcomere Lengths in the Chronically Dilated Canine Left Ventricle. Circ. Res. 1971, 28, 49–61. [Google Scholar] [CrossRef]
- Pollock, J.S.; Förstermann, U.; Mitchell, J.A.; Warner, T.D.; Schmidt, H.H.; Nakane, M.; Murad, F. Purification and characterization of particulate endothelium-derived relaxing factor synthase from cultured and native bovine aortic endothelial cells. Proc. Natl. Acad. Sci. USA 1991, 88, 10480–10484. [Google Scholar] [CrossRef]
- Sessa, W.C.; Harrison, J.K.; Barber, C.M.; Zeng, D.; Durieux, M.E.; D’Angelo, D.D.; Lynch, K.R.; Peach, M.J. Molecular cloning and expression of a cDNA encoding endothelial cell nitric oxide synthase. J. Biol. Chem. 1992, 267, 15274–15276. [Google Scholar] [CrossRef]
- Dong, H.; Waldron, G.J.; Cole, W.C.; Triggle, C.R. Roles of calcium-activated and voltage-gated delayed rectifier potassium channels in endothelium-dependent vasorelaxation of the rabbit middle cerebral artery. Br. J. Pharmacol. 1998, 123, 821–832. [Google Scholar] [CrossRef]
- Davies, P.F.; Robotewskyj, A.; Griem, M.L. Quantitative studies of endothelial cell adhesion. Directional remodeling of focal adhesion sites in response to flow forces. J. Clin. Investig. 1994, 93, 2031–2038. [Google Scholar] [CrossRef] [PubMed]
- Dewey, C.F., Jr.; Bussolari, S.R.; Gimbrone, M.A., Jr.; Davies, P.F. The Dynamic Response of Vascular Endothelial Cells to Fluid Shear Stress. J. Biomech. Eng. 1981, 103, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Henderson, A.H. St Cyres lecture. Endothelium in control. Br. Heart J. 1991, 65, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Hsiai, T.K.; Cho, S.K.; Wong, P.K.; Ing, M.; Salazar, A.; Sevanian, A.; Navab, M.; Demer, L.L.; Ho, C.-M. Monocyte recruitment to endothelial cells in response to oscillatory shear stress. FASEB J. 2003, 17, 1648–1657. [Google Scholar] [CrossRef]
- Saitoh, S.-i.; Saito, T.; Ohwada, T.; Ohtake, A.; Onogi, F.; Aikawa, K.; Maehara, K.; Maruyama, Y. Morphological and functional changes in coronary vessel evoked by repeated endothelial injury in pigs. Cardiovasc. Res. 1998, 38, 772–781. [Google Scholar] [CrossRef][Green Version]
- Akimoto, S.; Mitsumata, M.; Sasaguri, T.; Yoshida, Y. Laminar Shear Stress Inhibits Vascular Endothelial Cell Proliferation by Inducing Cyclin-Dependent Kinase Inhibitor p21Sdi1/Cip1/Waf1. Circ. Res. 2000, 86, 185–190. [Google Scholar] [CrossRef]
- Farinacci, M.; Krahn, T.; Dinh, W.; Volk, H.-D.; Düngen, H.-D.; Wagner, J.; Konen, T.; von Ahsen, O. Circulating endothelial cells as biomarker for cardiovascular diseases. Res. Pract. Thromb. Haemost. 2019, 3, 49–58. [Google Scholar] [CrossRef]
- Osol, G.; Ko, N.L.; Mandalà, M. Plasticity of the Maternal Vasculature During Pregnancy. Annu. Rev. Physiol. 2019, 81, 89–111. [Google Scholar] [CrossRef]
- Cipolla, M.; Osol, G. Hypertrophic and hyperplastic effects of pregnancy on the rat uterine arterial wall. Am. J. Obstet. Gynecol. 1994, 171, 805–811. [Google Scholar] [CrossRef]
- Cade, J.R.; Szarf, G.; de Siqueira, M.E.M.; Chaves, Á.; Andréa, J.C.M.; Figueira, H.R.; Gomes, M.M., Jr.; Freitas, B.P.; Filgueiras Medeiros, J.; dos Santos, M.R.; et al. Pregnancy-associated spontaneous coronary artery dissection: Insights from a case series of 13 patients. Eur. Heart J.-Cardiovasc. Imaging 2016, 18, 54–61. [Google Scholar] [CrossRef]
- Elkayam, U.; Jalnapurkar, S.; Barakkat, M.N.; Khatri, N.; Kealey, A.J.; Mehra, A.; Roth, A. Pregnancy-associated acute myocardial infarction: A review of contemporary experience in 150 cases between 2006 and 2011. Circulation 2014, 129, 1695–1702. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, A.S.; O’Sullivan, M. Pregnancy-related Spontaneous Coronary Artery Dissection: Two Case Reports and a Comprehensive Review of Literature. Heart Views Off. J. Gulf Heart Assoc. 2012, 13, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Aliyary, S.; Mariani, M.A.; Verhorst, P.M.J.; Hartmann, M.; Stoel, M.G.; von Birgelen, C. Staged Therapeutic Approach in Spontaneous Coronary Dissection. Ann. Thorac. Surg. 2007, 83, 1879–1881. [Google Scholar] [CrossRef] [PubMed]
- Kearney, P.; Singh, H.; Hutter, J.; Khan, S.; Lee, G.; Lucey, J. Spontaneous coronary artery dissection: A report of three cases and review of the literature. Postgrad. Med. J. 1993, 69, 940–945. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, A.C.; Haddad, A.; Fries, M.H.; Al-Kouatly, H.B. Risk factors, clinical findings, and outcomes in pregnancies with coronary artery dissection: A case series. Eur. J. Prev. Cardiol. 2019, 26, 544–548. [Google Scholar] [CrossRef]
- Moussa, H.N.; Movahedian, M.; Leon, M.G.; Sibai, B.M. Acute Myocardial Infarction Due to Coronary Artery Dissection in the Postpartum Period. AJP Rep. 2015, 5, e093–e096. [Google Scholar] [CrossRef][Green Version]
- Robinson, J.R. Pregnancy-Related Coronary Artery Dissection: Recognition of a Life Threatening Process. Dimens. Crit. Care Nurs. DCCN 2018, 37, 62–68. [Google Scholar] [CrossRef]
- Tweet, M.S.; Hayes, S.N.; Codsi, E.; Gulati, R.; Rose, C.H.; Best, P.J.M. Spontaneous Coronary Artery Dissection Associated With Pregnancy. J. Am. Coll. Cardiol. 2017, 70, 426–435. [Google Scholar] [CrossRef]
- Aragón-Charris, J.; Reyna-Villasmil, E.; De Nobrega-Correa, H.; Santos-Bolívar, J. Disección espontánea aguda de la arteria coronaria durante el puerperio. Clínica Investig. Ginecol. Obstet. 2013, 40, 40–42. [Google Scholar] [CrossRef]
- Wang, X.; Ge, J. Spontaneous Coronary-Artery Dissection. N. Engl. J. Med. 2021, 384, 1077. [Google Scholar] [CrossRef]
- Adlam, D.; Tweet, M.S.; Gulati, R.; Kotecha, D.; Rao, P.; Moss, A.J.; Hayes, S.N. Spontaneous Coronary Artery Dissection: Pitfalls of Angiographic Diagnosis and an Approach to Ambiguous Cases. JACC Cardiovasc. Interv. 2021, 14, 1743–1756. [Google Scholar] [CrossRef] [PubMed]
- Havakuk, O.; Goland, S.; Mehra, A.; Elkayam, U. Pregnancy and the Risk of Spontaneous Coronary Artery Dissection: An Analysis of 120 Contemporary Cases. Circ. Cardiovasc. Interv. 2017, 10, e004941. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, R.R.; Rinaldi, F.S.; Costa, J.R., Jr.; Feres, F.; Abizaid, A.; Sousa, A.G.; Sousa, J.E. Infarto agudo do miocárdio por dissecção espontânea de artérias coronárias: Série de cinco casos. Rev. Bras. Cardiol. Invasiva 2013, 21, 193–198. [Google Scholar] [CrossRef]
- Mark, D.B.; Kong, Y.; Whalen, R.E. Variant angina and spontaneous coronary artery dissection. Am. J. Cardiol. 1985, 56, 485–486. [Google Scholar] [CrossRef]
- Giraldo, F.A.; Piñeros, D.G. Disección coronaria espontánea postparto: Descripción de un caso y revisión de la literatura. Rev. Colomb. De Cardiol. 2013, 20, 122–126. [Google Scholar] [CrossRef][Green Version]
- McGovern, L.; Coughlan, J.J.; Murphy, R.; Edroos, S. Postpartum multi-vessel spontaneous coronary artery dissection in the setting of cocaine and amphetamine use: A case report. Eur. Heart J. Case Rep. 2021, 5, ytaa455. [Google Scholar] [CrossRef]
- Binhomaid, M.A.; Alhusain, F.; Al Deeb, M. Spontaneous Coronary Artery Dissection with Sudden Cardiac Arrest in a Female Patient During Her Postpartum Period: A Case Report and Review. Am. J. Case Rep. 2021, 22, e930380. [Google Scholar] [CrossRef]
- Al-Sadawi, M.; Shaikh, S.; Marmur, J.D.; Salciccioli, L.; Kariyanna, P.T.; McFarlane, I.M. Post-partum Spontaneous Coronary Artery Dissection: A Case Report. Am. J. Med. Case Rep. 2018, 6, 218–221. [Google Scholar] [CrossRef]
- Mantovani, F.; Navazio, A.; Tortorella, G.; Guiducci, V. Unique Case of Spontaneous Left Main Coronary Dissection in Second Trimester of Pregnancy Successfully Treated with Percutaneous Coronary Intervention: A Happy Ending. J. Cardiovasc. Dev. Dis. 2021, 9, 9. [Google Scholar] [CrossRef]
- Tang, A.T.; Cusimano, R.J. Spontaneous coronary artery dissection complicating midterm pregnancy. Ann. Thorac. Surg. 2004, 78, e35. [Google Scholar] [CrossRef]
- Refaie, M.; Alshehri, M.; Gallo, R. Spontaneous coronary artery dissection in puerperium. Asian Cardiovasc. Thorac. Ann. 2016, 24, 464–466. [Google Scholar] [CrossRef] [PubMed]
- Shahabi, S.; Smith, N.A.; Chanana, C.; Abbott, J.D.; Copel, J.; Setaro, J.F. Pregnancy-associated myocardial infarction: A report of two cases and review of the literature. Upsala J. Med. Sci. 2008, 113, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Rensing, B.J.; Kofflard, M.; van den Brand, M.J.; Foley, D.P. Spontaneous dissections of all three coronary arteries in a 33-week-pregnant woman. Catheter. Cardiovasc. Interv. Off. J. Soc. Card. Angiogr. Interv. 1999, 48, 207–210. [Google Scholar] [CrossRef]
- Vrints, C.J. Spontaneous coronary artery dissection. Heart 2010, 96, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Martinez, L.G. Spontaneous coronary artery dissection: A rare threat to young women. Crit. Care Nurse 2012, 32, e19–e26. [Google Scholar] [CrossRef]
- Aqel, R.A.; Zoghbi, G.J.; Iskandrian, A. Spontaneous coronary artery dissection, aneurysms, and pseudoaneurysms: A review. Echocardiography 2004, 21, 175–182. [Google Scholar] [CrossRef]
- Simões, M.V.; Ayres, E.M.; Santos, J.L.; Schmidt, A.; Pintya, A.O.; Maciel, B.C.; Marin-Neto, J.A. Detection of myocardial ischemia in chronic Chagas disease patients with atypic precordial pain by exercise and Holter tests. Arq. Bras. De Cardiol. 1993, 60, 315–319. [Google Scholar]
- Tibaldi, M.A.; Ruiz, C.; Servato, M.L.; Urinovsky, M.; Moreyra, E.A.; Sarmiento, P.E.; Moreyra, C.; Moreyra, E. Left Ventricular Longitudinal Global Strain to Predict Severe Coronary Disease in Patients with Precordial Pain Suggestive of Non-ST-Segment Elevation Acute Coronary Syndrome. J. Cardiovasc. Echogr. 2020, 30, 187–192. [Google Scholar] [CrossRef]
- Wang, R.; Zanon, J.; Neuschwander, F.C. Precordial Pain and Infarction in the Elderly. It’s no so Elementary, My Dear Watson! Arq. Bras. Cardiol. 2021, 116, 1046–1047. [Google Scholar] [CrossRef]
- Maclean, B. Precordial pain. Postgrad. Med. J. 1948, 24, 601–608. [Google Scholar] [CrossRef]
- Weston, L.; Alkhatib, H.; Kotwal, S. Atypical chest pain with precordial T wave inversions. Eur. J. Intern. Med. 2020, 82, 112–113. [Google Scholar] [CrossRef] [PubMed]
- Higgins, G.L., 3rd; Borofsky, J.S.; Irish, C.B.; Cochran, T.S.; Strout, T.D. Spontaneous peripartum coronary artery dissection presentation and outcome. J. Am. Board Fam. Med. 2013, 26, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, M.; Tanaka, M.; Ishii, M.; Honda, T.; Koga, H.; Miyao, Y.; Fujimoto, K.; Murayama, T. A case of postpartum spontaneous coronary artery dissection. Gen. Thorac. Cardiovasc. Surg. 2014, 62, 726–729. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Codsi, E.; Tweet, M.S.; Rose, C.H.; Arendt, K.W.; Best, P.J.M.; Hayes, S.N. Spontaneous Coronary Artery Dissection in Pregnancy: What Every Obstetrician Should Know. Obstet. Gynecol. 2016, 128, 731–738. [Google Scholar] [CrossRef]
- Lee, R.; Carr, D. Pregnancy-associated spontaneous coronary artery dissection (PASCAD): An etiology for chest pain in the young peripartum patient. Cjem 2018, 20, S64–S69. [Google Scholar] [CrossRef]
- Yeo, I.; Feldman, D.N.; Kim, L.K. Spontaneous Coronary Artery Dissection: Diagnosis and Management. Curr. Treat. Options Cardiovasc. Med. 2018, 20, 27. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Hamra, M.; Ali, M.; Abdullah, A.S.; Arnous, S.; Kiernan, T.J. Spontaneous coronary artery dissection, challenges of diagnosis and management. Future Cardiol. 2017, 13, 539–549. [Google Scholar] [CrossRef]
- Al-Hussaini, A.; Abdelaty, A.; Gulsin, G.S.; Arnold, J.R.; Garcia-Guimaraes, M.; Premawardhana, D.; Budgeon, C.; Wood, A.; Natarajan, N.; Mangion, K.; et al. Chronic infarct size after spontaneous coronary artery dissection: Implications for pathophysiology and clinical management. Eur. Heart J. 2020, 41, 2197–2205. [Google Scholar] [CrossRef]
- Macaya, F.; Salinas, P.; Gonzalo, N.; Fernández-Ortiz, A.; Macaya, C.; Escaned, J. Spontaneous coronary artery dissection: Contemporary aspects of diagnosis and patient management. Open Heart 2018, 5, e000884. [Google Scholar] [CrossRef]
- Kermali, M.; Zahra, S.A.; Hewage, S.; Al Nahian, S.; Harky, A. Spontaneous coronary artery dissection: Presentation and management options. Coron. Artery Dis. 2021, 32, 152–163. [Google Scholar] [CrossRef]
- Boulmpou, A.; Kassimis, G.; Zioutas, D.; Meletidou, M.; Mouselimis, D.; Tsarouchas, A.; Tzikas, S.; Vassilikos, V.; Kanonidis, I.; Tsounos, I.; et al. Spontaneous Coronary Artery Dissection (SCAD): Case Series and Mini Review. Cardiovasc. Revascularization Med. Incl. Mol. Interv. 2020, 21, 1450–1456. [Google Scholar] [CrossRef]
- Manasrah, N.; Al Sbihi, A.F.; Bell, K.; Afonso, L.C.; Blank, N. Spontaneous Coronary Artery Dissection: Case Series and Literature Review. Cureus 2021, 13, e13539. [Google Scholar] [CrossRef] [PubMed]
- Lezcano Gort, L.E.; Romani, S.A.; Rodríguez Carreras, C.R. Postpartum Multivessel Spontaneous Coronary Artery Dissection. Rev. Española Cardiol. 2016, 69, 781–782. [Google Scholar] [CrossRef]
- Takeuchi, M.; Okada, T.; Ikegami, Y.; Nakamoto, Y.; Idei, N.; Ohashi, N. A breastfeeding woman with spontaneous coronary artery dissection and possible takotsubo syndrome: A case report. Medicine 2021, 100, e25775. [Google Scholar] [CrossRef]
- Tweet, M.S.; Eleid, M.F.; Best, P.J.; Lennon, R.J.; Lerman, A.; Rihal, C.S.; Holmes, D.R., Jr.; Hayes, S.N.; Gulati, R. Spontaneous coronary artery dissection: Revascularization versus conservative therapy. Circ. Cardiovasc. Interv. 2014, 7, 777–786. [Google Scholar] [CrossRef]
- Hendiri, T.; Bonvini, R.F.; Martin, W.; Doriot, P.A.; Camenzind, E. [Acute myocardial infarction due to spontaneous coronary artery dissection]. Arch. Des Mal. Du Coeur Des Vaiss. 2005, 98, 974–978. [Google Scholar]
- Adams, C.; He, M.; Hughes, I.; Singh, K. Mortality in spontaneous coronary artery dissection: A systematic review and meta-analysis. Catheter. Cardiovasc. Interv. Off. J. Soc. Card. Angiogr. Interv. 2021, 98, 1211–1220. [Google Scholar] [CrossRef]
- Saw, J. Coronary angiogram classification of spontaneous coronary artery dissection. Catheter. Cardiovasc. Interv. 2014, 84, 1115–1122. [Google Scholar] [CrossRef]
- Budoff, M.J.; Dowe, D.; Jollis, J.G.; Gitter, M.; Sutherland, J.; Halamert, E.; Scherer, M.; Bellinger, R.; Martin, A.; Benton, R. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: Results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J. Am. Coll. Cardiol. 2008, 52, 1724–1732. [Google Scholar]
- Koul, A.K.; Hollander, G.; Moskovits, N.; Frankel, R.; Herrera, L.; Shani, J. Coronary artery dissection during pregnancy and the postpartum period: Two case reports and review of literature. Catheter. Cardiovasc. Interv. Off. J. Soc. Card. Angiogr. Interv. 2001, 52, 88–94. [Google Scholar] [CrossRef]
- Copel, J.; El-Sayed, Y.; Heine, R.P.; Wharton, K.R. Guidelines for diagnostic imaging during pregnancy and lactation. Obstet. Gynecol. 2017, 130, E210–E216. [Google Scholar]
- Wain-Hobson, J.; Roule, V.; Dahdouh, Z.; Sabatier, R.; Lognoné, T.; Grollier, G. Spontaneous coronary artery dissection: One entity with several therapeutic options. Cardiovasc. Revascularization Med. 2012, 13, 203.e1–203.e4. [Google Scholar] [CrossRef] [PubMed]
- Shiran, A.; Adawi, S.; Rubinshtein, R.; Bardicef, M.; Gutterman, E. Non-invasive management of post-partum spontaneous left main coronary artery dissection using cardiac computed tomography angiography. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 1152. [Google Scholar] [CrossRef] [PubMed]
- Davlouros, P.; Xanthopoulou, I.; Tsigkas, G.; Mplani, V.; Despotopoulos, S.; Hahalis, G. Complete Healing of Spontaneous Coronary Artery Dissection Demonstrated by Optical Coherence Tomography in a Young Postpartum Female Presenting With Acute Coronary Syndrome. JACC Cardiovasc. Interv. 2017, 10, e89–e90. [Google Scholar] [CrossRef]
- Jackson, R.; Al-Hussaini, A.; Joseph, S.; van Soest, G.; Wood, A.; Macaya, F.; Gonzalo, N.; Cade, J.; Caixeta, A.; Hlinomaz, O.; et al. Spontaneous Coronary Artery Dissection: Pathophysiological Insights From Optical Coherence Tomography. JACC Cardiovasc. Imaging 2019, 12, 2475–2488. [Google Scholar] [CrossRef]
- Franco, C.; Eng, L.; Saw, J. Optical Coherence Tomography in the Diagnosis and Management of Spontaneous Coronary Artery Dissection. Interv. Cardiol. Clin. 2015, 4, 309–320. [Google Scholar] [CrossRef]
- De Clerck, E.E.B.; Schouten, J.; Berendschot, T.; Goezinne, F.; Liesenborghs, I.; Dagnelie, P.C.; Schaper, N.C.; Kroon, A.A.; Henry, R.M.A.; Reesink, K.D.; et al. Vascular risk factors for optical coherence tomography-detected macular cysts: The Maastricht Study. Acta Ophthalmol. 2021, 99, e860–e868. [Google Scholar] [CrossRef]
- Russo, V.; Marrozzini, C.; Zompatori, M. Spontaneous coronary artery dissection: Role of coronary CT angiography. Heart 2013, 99, 672–673. [Google Scholar] [CrossRef]
- Gupta, S.; Meyersohn, N.M.; Wood, M.J.; Steigner, M.L.; Blankstein, R.; Ghoshhajra, B.B.; Hedgire, S.S. Role of Coronary CT Angiography in Spontaneous Coronary Artery Dissection. Radiol. Cardiothorac. Imaging 2020, 2, e200364. [Google Scholar] [CrossRef]
- Paratz, E.D.; Kao, C.; MacIsaac, A.I.; Somaratne, J.; Whitbourn, R. Evolving management and improving outcomes of pregnancy-associated spontaneous coronary artery dissection (P-SCAD): A systematic review. Int. J. Cardiol. Heart Vasc. 2018, 18, 1–6. [Google Scholar] [CrossRef]
- Pinar, E.; Bardají, A. Manejo del infarto agudo de miocardio con elevación del segmento ST. Guías de actuación clínica y el mundo real. Rev. Española Cardiol. 2009, 9, 71–78. [Google Scholar] [CrossRef]
- Expert consensus document on management of cardiovascular diseases during pregnancy. Eur. Heart J. 2003, 24, 761–781. [CrossRef]
- Maeder, M.; Ammann, P.; Drack, G.; Rickli, H. Pregnancy-associated spontaneous coronary artery dissection: Impact of medical treatment. Case report and systematic review. Z. Kardiol. 2005, 94, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002, 324, 71–86. [CrossRef] [PubMed]
- Zheng, S.L.; Roddick, A.J. Association of Aspirin Use for Primary Prevention With Cardiovascular Events and Bleeding Events: A Systematic Review and Meta-analysis. Jama 2019, 321, 277–287. [Google Scholar] [CrossRef]
- Pfeffer, M.A.; Braunwald, E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation 1990, 81, 1161–1172. [Google Scholar] [CrossRef]
- Jia, S.; Liu, Y.; Yuan, J. Evidence in Guidelines for Treatment of Coronary Artery Disease. Adv. Exp. Med. Biol. 2020, 1177, 37–73. [Google Scholar] [CrossRef]
- Cerrato, E.; Giacobbe, F.; Quadri, G.; Macaya, F.; Bianco, M.; Mori, R.; Biolè, C.A.; Boi, A.; Bettari, L.; Rolfo, C.; et al. Antiplatelet therapy in patients with conservatively managed spontaneous coronary artery dissection from the multicentre DISCO registry. Eur. Heart J. 2021, 42, 3161–3171. [Google Scholar] [CrossRef]
- Saw, J.; Humphries, K.; Aymong, E.; Sedlak, T.; Prakash, R.; Starovoytov, A.; Mancini, G.J. Spontaneous coronary artery dissection: Clinical outcomes and risk of recurrence. J. Am. Coll. Cardiol. 2017, 70, 1148–1158. [Google Scholar] [CrossRef]
- Hassan, S.; Samuel, R.; Starovoytov, A.; Lee, C.; Aymong, E.; Saw, J. Outcomes of Percutaneous Coronary Intervention in Patients with Spontaneous Coronary Artery Dissection. J. Interv. Cardiol. 2021, 2021, 6686230. [Google Scholar] [CrossRef]
- Prakash, R.; Starovoytov, A.; Heydari, M.; Mancini, G.B.; Saw, J. Catheter-Induced Iatrogenic Coronary Artery Dissection in Patients With Spontaneous Coronary Artery Dissection. JACC Cardiovasc. Interv. 2016, 9, 1851–1853. [Google Scholar] [CrossRef] [PubMed]
- Sabatine, M.S.; Bergmark, B.A.; Murphy, S.A.; O’Gara, P.T.; Smith, P.K.; Serruys, P.W.; Kappetein, A.P.; Park, S.J.; Park, D.W.; Christiansen, E.H.; et al. Percutaneous coronary intervention with drug-eluting stents versus coronary artery bypass grafting in left main coronary artery disease: An individual patient data meta-analysis. Lancet 2021, 398, 2247–2257. [Google Scholar] [CrossRef]
- Olivares, R.G.; Veas, N. Coronary artery bypass grafting or percutaneous coronary intervention in patients with severe three vessel disease. Rev. Med. Chile 2021, 149, 1182–1188. [Google Scholar] [CrossRef]
- Hayes, S.N.; Kim, E.S.H.; Saw, J.; Adlam, D.; Arslanian-Engoren, C.; Economy, K.E.; Ganesh, S.K.; Gulati, R.; Lindsay, M.E.; Mieres, J.H.; et al. Spontaneous Coronary Artery Dissection: Current State of the Science: A Scientific Statement From the American Heart Association. Circulation 2018, 137, e523–e557. [Google Scholar] [CrossRef]
- Tweet, M.S.; Hayes, S.N.; Pitta, S.R.; Simari, R.D.; Lerman, A.; Lennon, R.J.; Gersh, B.J.; Khambatta, S.; Best, P.J.; Rihal, C.S.; et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation 2012, 126, 579–588. [Google Scholar] [CrossRef]
- Weinberg, L.; Ong, M.; Tan, C.O.; McDonnell, N.J.; Lo, C.; Chiam, E. Spontaneous coronary artery dissection in pregnancy requiring emergency caesarean delivery followed by coronary artery bypass grafting. Anaesth. Intensive Care 2013, 41, 251–255. [Google Scholar] [CrossRef]
- Bac, D.J.; Lotgering, F.K.; Verkaaik, A.P.; Deckers, J.W. Spontaneous coronary artery dissection during pregnancy and post partum. Eur. Heart J. 1995, 16, 136–138. [Google Scholar] [CrossRef]
- Páez, M.; Buisán, F.; Herrero, E. Spontaneous dissection of the left coronary artery trunk during the postpartum period treated with revascularization surgery, ventricular assistance and a successful heart transplant. Acta Anaesthesiol. Scand. 2007, 51, 960–961. [Google Scholar] [CrossRef]
- Evans, R. Post-partum spontaneous coronary artery dissection and the use of veno-arterial extra-corporeal membrane oxygenation. Nurs. Crit. Care 2014, 19, 304–309. [Google Scholar] [CrossRef]
- Knapp, K.E.; Weis, R.A.; Cubillo, E.I.; Chapital, A.B.; Ramakrishna, H. Spontaneous, Postpartum Coronary Artery Dissection and Cardiogenic Shock with Extracorporeal Membrane Oxygenation Assisted Recovery in a 30-Year-Old Patient. Case Rep. Cardiol. 2016, 2016, 1048708. [Google Scholar] [CrossRef]
| Drugs Used in the Conservative Treatment | |||
|---|---|---|---|
| DRUGS | USE | ADVANTAGES | DISADVANTAGES |
| ASPIRIN | First-line treatment. Most-used drug for acute and long-term treatment of SCAD. | Antiaggregant. Low hemorrhagic risk and proven benefit in patients with ACS and in secondary prevention of coronary artery disease [139,140]. | Low hemorrhagic risk [140]. |
| BETA- BLOCKERS | First-line treatment. | Reduce arterial wall stress [141]. | Avoid in patients with severe asthma or COPD [141]. |
| NITRATES | First-line treatment. | Vasodilator [142]. | |
| ACE Inhibitors | They are not a first-line treatment. | Indicated only in patients with a significant decrease in LVEF after ACS (EF < 40%) [142]. | |
| ANTI COAGULANTS (LMWH) | Controversial use; initially administered in patients with ACS. | Not recommended [107]. | They have been shown to increase the risk of dissection spread and intramural hematoma [82]. |
| FIBRINOLYTICS. | Not recommended. | Not recommended [107]. | They have been shown to promote bleeding and increase intraparietal hematoma, enlarge compression of the true arterial lumen, and worsen the clinical picture [107]. |
| Drugs used in the Invasive treatment | |||
| ASPIRIN + CLOPIDOGREL | First-line treatment. | Dual antiplatelet therapy may be beneficial in reducing the false lumen thrombus created for SCAD, thereby reducing the decrease in true lumen caliber [143]. | Increased risk of bleeding [144]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cano-Castellote, M.; Afanador-Restrepo, D.F.; González-Santamaría, J.; Rodríguez-López, C.; Castellote-Caballero, Y.; Hita-Contreras, F.; Carcelén-Fraile, M.d.C.; Aibar-Almazán, A. Pathophysiology, Diagnosis and Treatment of Spontaneous Coronary Artery Dissection in Peripartum Women. J. Clin. Med. 2022, 11, 6657. https://doi.org/10.3390/jcm11226657
Cano-Castellote M, Afanador-Restrepo DF, González-Santamaría J, Rodríguez-López C, Castellote-Caballero Y, Hita-Contreras F, Carcelén-Fraile MdC, Aibar-Almazán A. Pathophysiology, Diagnosis and Treatment of Spontaneous Coronary Artery Dissection in Peripartum Women. Journal of Clinical Medicine. 2022; 11(22):6657. https://doi.org/10.3390/jcm11226657
Chicago/Turabian StyleCano-Castellote, Marta, Diego Fernando Afanador-Restrepo, Jhonatan González-Santamaría, Carlos Rodríguez-López, Yolanda Castellote-Caballero, Fidel Hita-Contreras, María del Carmen Carcelén-Fraile, and Agustín Aibar-Almazán. 2022. "Pathophysiology, Diagnosis and Treatment of Spontaneous Coronary Artery Dissection in Peripartum Women" Journal of Clinical Medicine 11, no. 22: 6657. https://doi.org/10.3390/jcm11226657
APA StyleCano-Castellote, M., Afanador-Restrepo, D. F., González-Santamaría, J., Rodríguez-López, C., Castellote-Caballero, Y., Hita-Contreras, F., Carcelén-Fraile, M. d. C., & Aibar-Almazán, A. (2022). Pathophysiology, Diagnosis and Treatment of Spontaneous Coronary Artery Dissection in Peripartum Women. Journal of Clinical Medicine, 11(22), 6657. https://doi.org/10.3390/jcm11226657











