Comparison of Three Common Intervertebral Disc Discectomies in the Treatment of Lumbar Disc Herniation: A Systematic Review and Meta-Analysis Based on Multiple Data
Abstract
1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Inclusion Criteria
- Study design: comparison of randomized controlled clinical trials of MED and MED and traditional open surgery for lumbar intervertebral disc herniation, as well as prospective or retrospective controlled studies.
- Patients: patients were diagnosed with lumbar intervertebral disc herniation, not limited by age or sex, and initial onset or recurrent disease.
- Intervention: in the case of patients, MED, traditional open surgery, and other interventions; the premise is that these interventions are consistent across groups.
- Outcomes: the included studies must include at least 3 of the evaluation indicators studied.
2.3. Exclusion Criteria
- Meeting summaries and meta-analysis summaries, among others, are not included in this study.
- Incomplete outcome indicators in the literature, such as the average number of results but absence of the standard deviation.
- No control group in the study, such as case series and other observational studies, among others.
- Combination of other diseases affecting the curative effect, such as spondylolisthesis and intervertebral disc calcification, among others.
2.4. Search Strategy
2.5. Literature Screening and Quality Evaluation
2.6. Data Extraction
2.7. Statistical Approach
3. Results
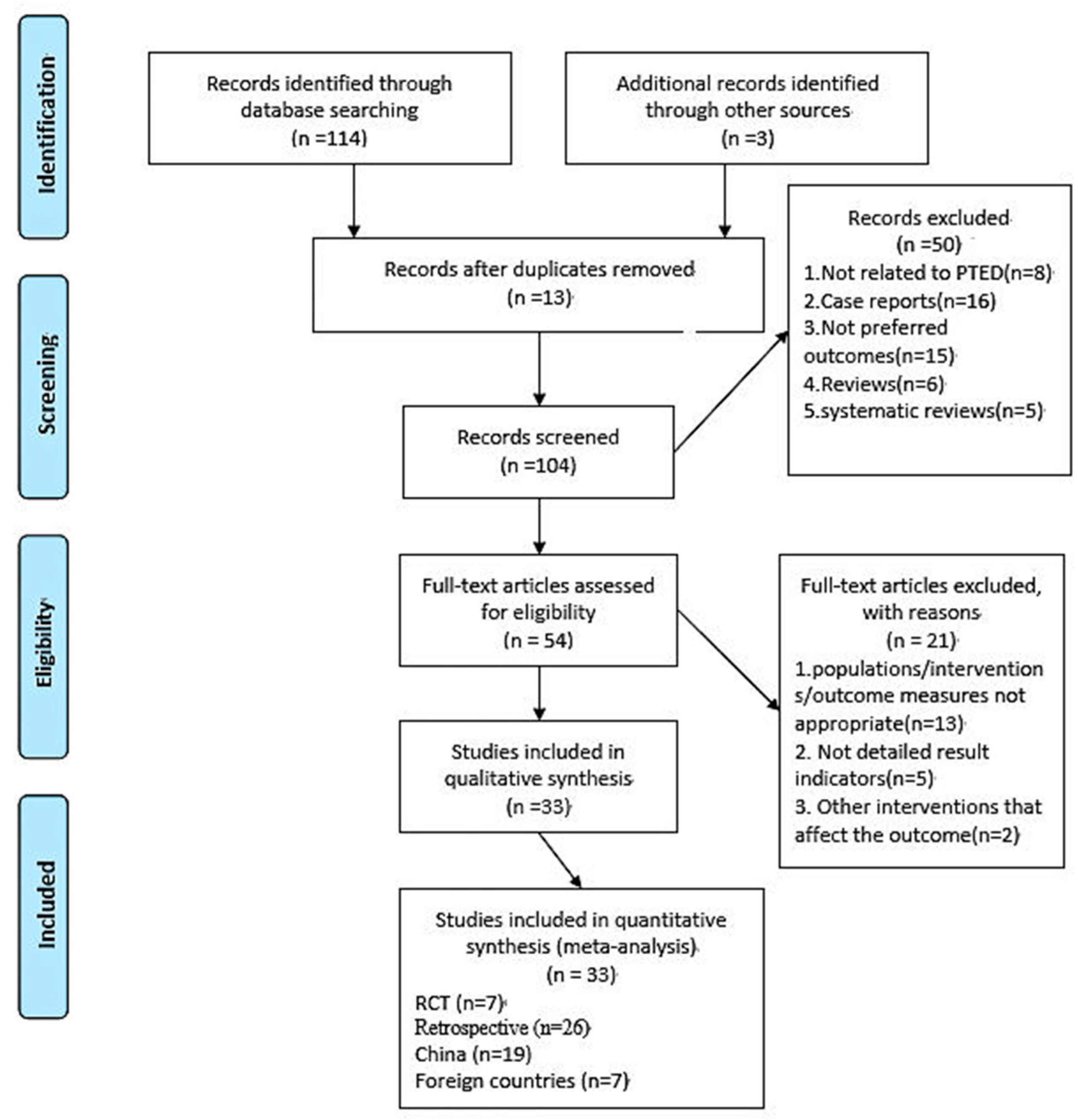
3.1. Literature Search
3.2. Study Characteristics
3.3. Literature Quality Evaluation
3.4. Outcomes
3.4.1. Average Operative Time (min)
3.4.2. Intraoperative Blood Loss (mL)
3.4.3. Size of the Incision (cm)
3.4.4. Postoperative Bed Rest Time (Day)
3.4.5. Hospitalization Time (Day)
3.4.6. Leg Pain
3.4.7. Low Back Pain
3.4.8. Postoperative Comprehensive Pain
3.4.9. Postoperative ODI Index
3.4.10. Incidence of Complications
3.4.11. Incidence of Recurrence
3.4.12. Revision Rate
3.4.13. Rates of Successful Operation
3.5. Sensitivity Analysis
3.6. Publication Bias Analysis
4. Discussion
4.1. PTED vs. MED
4.2. PTED vs. OD
4.3. Discussion Regarding the Application of PTED in China
- Why is it so popular in China and less applied in related fields abroad?
- 2.
- Defects of PTED
4.4. Strengths and Weaknesses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OD | open surgery |
| MED | microendoscopic discectomy |
| PTED | percutaneous transforaminal discectomy |
| PLIF | posterior lumbar interbody fusion surgery |
| TLIF | transforaminal lumbar interbody fusion surgery |
| MIS-TLIF | minimally invasive transforaminal lumbar interbody fusion surgery |
| PEID | percutaneous endoscopic interlaminar discectomy |
| PRISMA | Preferred Reporting Items For Systematic Reviews and Meta-Analyses |
| RCT | randomized controlled trials |
| NOS | Newcastle–Ottawa Scale |
| VAS | visual analogue scale |
| ODI | Oswestry Disability Index |
| OR | odds ratio |
| CI | confidence interval |
| MD | mean difference |
| SMD | standard mean difference |
References
- Mixter, W. Rupture of the intervertebral disc with involvement of the spinal canal. N. Engl. J. Med. 1964, 211, 1632–1638. [Google Scholar] [CrossRef]
- Ahn, S.-S.; Kim, S.-H.; Kim, D.-W.; Lee, B.-H. Comparison of Outcomes of Percutaneous Endoscopic Lumbar Discectomy and Open Lumbar Microdiscectomy for Young Adults: A Retrospective Matched Cohort Study. World Neurosurg. 2015, 86, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Cloward, R.B. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J. Neurosurg. 1953, 10, 154–168. [Google Scholar] [CrossRef] [PubMed]
- Blume, H.G. Unilateral posterior lumbar interbody fusion: Simplified dowel technique. Clin. Orthop. Relat. Res. 1985, 193, 75–84. [Google Scholar] [CrossRef]
- Foley, K.T.; Holly, L.T.; Schwender, J.D. Minimally invasive lumbar fusion. Spine 2003, 28, S26–S35. [Google Scholar] [CrossRef] [PubMed]
- Pan, Z.; Ha, Y.; Yi, S.; Cao, K. Efficacy of Transforaminal Endoscopic Spine System (TESSYS) Technique in Treating Lumbar Disc Herniation. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2016, 22, 530–539. [Google Scholar] [CrossRef]
- Perez-Cruet, M.J.; Foley, K.T.; Isaacs, R.E.; Rice-Wyllie, L.; Wellington, R.; Smith, M.M.; Fessler, R.G. Microendoscopic lumbar discectomy: Technical note. Neurosurgery 2002, 51, S129–S136. [Google Scholar] [CrossRef]
- Garg, B.; Nagraja, U.B.; Jayaswal, A. Microendoscopic versus open discectomy for lumbar disc herniation: A prospective randomised study. J. Orthop. Surg. 2011, 19, 30–34. [Google Scholar] [CrossRef]
- Fontanella, A. Endoscopic microsurgery in herniated cervical discs. Neurol. Res. 1999, 21, 31–38. [Google Scholar] [CrossRef]
- Williams, R.W. Microlumbar discectomy: A conservative surgical approach to the virgin herniated lumbar disc. Spine 1978, 3, 175–182. [Google Scholar] [CrossRef]
- Yeung, A.T.; Tsou, P.M. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine 2002, 27, 722–731. [Google Scholar] [CrossRef] [PubMed]
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine 2008, 33, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.C.; Kim, J.S.; Park, C.K. Percutaneous Endoscopic Lumbar Discectomy as an Alternative to Open Lumbar Microdiscectomy for Large Lumbar Disc Herniation. Pain Physician 2016, 19, E291–E300. [Google Scholar]
- Kafadar, A.; Kahraman, S.; Akboru, M. Percutaneous endoscopic transforaminal lumbar discectomy: A critical appraisal. Minim. Invasive Neurosurg. 2006, 49, 74–79. [Google Scholar] [CrossRef]
- Zhao, X.M.; Yuan, Q.L.; Liu, L.; Shi, Y.M.; Zhang, Y.G. Is It Possible to Replace Microendoscopic Discectomy with Percutaneous Transforaminal Discectomy for Treatment of Lumbar Disc Herniation? A Meta-Analysis Based on Recurrence and Revision Rate. J. Korean Neurosurg. Soc. 2020, 63, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Open Med. 2009, 3, e123–e130. [Google Scholar]
- Richardson, W.S.; Wilson, M.C.; Nishikawa, J.; Hayward, R.S. The well-built clinical question: A key to evidence-based decisions. ACP J. Club 1995, 123, A12–A13. [Google Scholar] [CrossRef]
- Farace, D.J.; Frantzen, J. Perspectives on the design and transfer of scientific and technical information: Third international conference on grey literature. Minerva Ginecol. 1998, 48, 501–504. [Google Scholar]
- van Tulder, M.; Furlan, A.; Bombardier, C.; Bouter, L. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 2003, 28, 1290–1299. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Pfirrmann, C.W.; Metzdorf, A.; Zanetti, M.; Hodler, J.; Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 2001, 26, 1873–1878. [Google Scholar] [CrossRef] [PubMed]
- Johnsen, L.G.; Hellum, C.; Nygaard, O.P.; Storheim, K.; Brox, J.I.; Rossvoll, I.; Leivseth, G.; Grotle, M. Comparison of the SF6D, the EQ5D, and the oswestry disability index in patients with chronic low back pain and degenerative disc disease. BMC Musculoskelet. Disord. 2013, 14, 148. [Google Scholar] [CrossRef] [PubMed]
- Macnab, I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J. Bone Joint Surg. Am. 1971, 53, 891–903. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.G. The jackknife-a review. Biometrika 1974, 61, 1–15. [Google Scholar]
- Mayer, H.M.; Brock, M. Percutaneous endoscopic discectomy: Surgical technique and preliminary results compared to microsurgical discectomy. J. Neurosurg. 1993, 78, 216–225. [Google Scholar] [CrossRef]
- Kim, M.J.; Lee, S.H.; Jung, E.S.; Son, B.G.; Choi, E.S.; Shin, J.H.; Sung, J.K.; Chi, Y.C. Targeted percutaneous transforaminal endoscopic diskectomy in 295 patients: Comparison with results of microscopic diskectomy. Surg. Neurol. 2007, 68, 623–631. [Google Scholar] [CrossRef]
- Li, H.; Jiang, C.; Mu, X.; Lan, W.; Zhou, Y.; Li, C. Comparison of MED and PELD in the Treatment of Adolescent Lumbar Disc Herniation: A 5-Year Retrospective Follow-Up. World Neurosurg. 2018, 112, e255–e260. [Google Scholar] [CrossRef]
- Hsu, H.T.; Chang, S.J.; Yang, S.S.; Chai, C.L. Learning curve of full-endoscopic lumbar discectomy. Eur. Spine J. 2013, 22, 727–733. [Google Scholar] [CrossRef]
- Liu, X.; Yuan, S.; Tian, Y.; Wang, L.; Gong, L.; Zheng, Y.; Li, J. Comparison of percutaneous endoscopic transforaminal discectomy, microendoscopic discectomy, and microdiscectomy for symptomatic lumbar disc herniation: Minimum 2-year follow-up results. J. Neurosurg. Spine 2018, 28, 317–325. [Google Scholar] [CrossRef]
- Chen, Z.; Zhang, L.; Dong, J.; Xie, P.; Liu, B.; Wang, Q.; Chen, R.; Feng, F.; Yang, B.; Shu, T.; et al. Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial. J. Neurosurg. Spine 2018, 28, 300–310. [Google Scholar] [CrossRef]
- Wang, S.F.; Hung, S.F.; Tsai, T.T.; Li, Y.D.; Chiu, P.Y.; Hsieh, M.K.; Kao, F.C. Better Functional Outcome and Pain Relief in the Far-Lateral-Outside-in Percutaneous Endoscopic Transforaminal Discectomy. J. Pain Res. 2021, 14, 3927–3934. [Google Scholar] [CrossRef] [PubMed]
- Rajamani, P.A.; Goparaju, P.; Kulkarni, A.G.; Bhojraj, S.Y.; Rajasekaran, S.; Chhabra, H.S.; Acharya, S.; Rajamani, A.; Nene, A.; Shetty, A.P.; et al. A 2-Year Outcomes and Complications of Various Techniques of Lumbar Discectomy: A Multicentric Retrospective Study. World Neurosurg. 2021, 156, e319–e328. [Google Scholar] [CrossRef] [PubMed]
- Jing, Z.; Li, L.; Song, J. Percutaneous transforaminal endoscopic discectomy versus microendoscopic discectomy for upper lumbar disc herniation: A retrospective comparative study. Am. J. Transl. Res. 2021, 13, 3111–3119. [Google Scholar] [PubMed]
- Wang, H.; Cheng, J.; Xiao, H.; Li, C.; Zhou, Y. Adolescent lumbar disc herniation: Experience from a large minimally invasive treatment centre for lumbar degenerative disease in Chongqing, China. Clin. Neurol. Neurosurg. 2013, 115, 1415–1419. [Google Scholar] [CrossRef] [PubMed]
- Song, H.P.; Sheng, H.F.; Xu, W.X. A case-control study on the treatment of protrusion of lumbar intervertebral disc through PELD and MED. Exp. Ther. Med. 2017, 14, 3708–3712. [Google Scholar] [CrossRef]
- Sinkemani, A.; Hong, X.; Gao, Z.X.; Zhuang, S.Y.; Jiang, Z.L.; Zhang, S.D.; Bao, J.P.; Zhu, L.; Zhang, P.; Xie, X.H.; et al. Outcomes of Microendoscopic Discectomy and Percutaneous Transforaminal Endoscopic Discectomy for the Treatment of Lumbar Disc Herniation: A Comparative Retrospective Study. Asian Spine J. 2015, 9, 833–840. [Google Scholar] [CrossRef]
- Lee, D.Y.; Shim, C.S.; Ahn, Y.; Choi, Y.G.; Kim, H.J.; Lee, S.H. Comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for recurrent disc herniation. J. Korean Neurosurg. Soc. 2009, 46, 515–521. [Google Scholar] [CrossRef]
- Li, J.; Ma, C.; Li, Y.; Liu, G.; Wang, D.; Dai, W.; Tian, J. A comparison of results between percutaneous transforaminal endoscopic discectomy and fenestration discectomy for lumbar disc herniation in the adolscents. Zhonghua Yi Xue Za Zhi 2015, 95, 3852–3855. [Google Scholar]
- Chen, H.C.; Lee, C.H.; Wei, L.; Lui, T.N.; Lin, T.J. Comparison of percutaneous endoscopic lumbar discectomy and open lumbar surgery for adjacent segment degeneration and recurrent disc herniation. Neurol. Res. Int. 2015, 2015, 791943. [Google Scholar] [CrossRef]
- Yao, Y.; Zhang, H.; Wu, J.; Liu, H.; Zhang, Z.; Tang, Y.; Zhou, Y. Minimally Invasive Transforaminal Lumbar Interbody Fusion Versus Percutaneous Endoscopic Lumbar Discectomy: Revision Surgery for Recurrent Herniation After Microendoscopic Discectomy. World Neurosurg. 2017, 99, 89–95. [Google Scholar] [CrossRef]
- Jeong, J.S.; Lee, S.H.; Lee, S.J.; Hwang, B.W. The Clinical Comparison between Open Surgery and Percutaneous Endoscopic Lumbar Discectomy in Extraforaminal Lumbar Disc Herniation. J. Korean Neurosurg. Soc. 2006, 39, 413–418. [Google Scholar]
- Li, Y.W.; Wang, H.J.; Wang, Y.S.; Cui, W.; Zhou, P.; Li, C. Comparison of percutaneous endoscopic lumbar discectomy versus transforaminal lumbar interbody fusion in treating upper lumbar disc herniation. Zhonghua Yi Xue Za Zhi 2018, 98, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.; Zhang, T.; Gao, G.; Yu, C.; Liu, P.; Zuo, G.; Huang, X. Therapeutic effect of percutaneous endoscopic lumbar discectomy on lumbar disc herniation and its effect on oxidative stress in patients with lumbar disc herniation. Exp. Ther. Med. 2018, 15, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Ding, Z.M.; Tao, Y.Q. Clinical Outcomes of Percutaneous Transforaminal Endoscopic Discectomy Versus Fenestration Discectomy in Patients with Lumbar Disc Herniation. Int. J. Transl. Med. 2017, 5, 29–33. [Google Scholar]
- Sun, Y.; Zhang, W.; Qie, S.; Zhang, N.; Ding, W.; Shen, Y. Comprehensive comparing percutaneous endoscopic lumbar discectomy with posterior lumbar internal fixation for treatment of adjacent segment lumbar disc prolapse with stable retrolisthesis: A retrospective case-control study. Medicine 2017, 96, e7471. [Google Scholar] [CrossRef]
- Ahn, Y.; Lee, S.G.; Son, S.; Keum, H.J. Transforaminal Endoscopic Lumbar Discectomy Versus Open Lumbar Microdiscectomy: A Comparative Cohort Study with a 5-Year Follow-Up. Pain Physician 2019, 22, 295–304. [Google Scholar] [CrossRef]
- Pan, L.; Zhang, P.; Yin, Q. Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: A randomised controlled trial. Int. J. Surg. 2014, 12, 534–537. [Google Scholar] [CrossRef]
- Jarebi, M.; Awaf, A.; Lefranc, M.; Peltier, J. A matched comparison of outcomes between percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for the treatment of lumbar disc herniation: A 2-year retrospective cohort study. Spine J. Off. J. N. Am. Spine Soc. 2020, 21, 114–121. [Google Scholar] [CrossRef]
- Gibson, J.N.A.; Subramanian, A.S.; Scott, C.E.H. A randomised controlled trial of transforaminal endoscopic discectomy vs microdiscectomy. Eur. Spine J. 2016, 26, 847–856. [Google Scholar] [CrossRef]
- Meyer, G.; Da Rocha, I.D.; Cristante, A.F.; Marcon, R.M.; Coutinho, T.P.; Torelli, A.G.; Petersen, P.A.; Letaif, O.B.; Filho, T.E.P.D.B. Percutaneous Endoscopic Lumbar Discectomy Versus Microdiscectomy for the Treatment of Lumbar Disc Herniation: Pain, Disability, and Complication Rate-A Randomized Clinical Trial. Int. J. Spine Surg. 2020, 14, 72–78. [Google Scholar] [CrossRef]
- Chen, Z.; Zhang, L.; Dong, J.; Xie, P.; Liu, B.; Wang, Q.; Chen, R.; Shu, T.; Li, S.; Feng, F.; et al. Percutaneous Transforaminal Endoscopic Discectomy Versus Microendoscopic Discectomy for Lumbar Disc Herniation: Two-Year Results of a Randomized Controlled Trial. Spine 2020, 45, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Zhou, Y. Percutaneous Endoscopic Lumbar Diskectomy and Minimally Invasive Transforaminal Lumbar Interbody Fusion for Recurrent Lumbar Disk Herniation. World Neurosurg. 2016, 98, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Li, H.; Zhang, T.; Wei, Y.; Zhang, H.; Yu, F.; Lv, Y.; Ren, Y. Comparison of Percutaneous Endoscopic Interlaminar Discectomy and Open Fenestration Discectomy for Single-Segment Huge Lumbar Disc Herniation: A Two-year Follow-up Retrospective Study. J. Pain Res. 2022, 15, 1061–1070. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.H.; Chung, C.K.; Choi, Y.; Kim, M.J.; Yim, D.; Yang, S.H.; Lee, C.H.; Jung, J.M.; Hwang, S.H.; Kim, D.H.; et al. The Long-term Reoperation Rate Following Surgery for Lumbar Herniated Intervertebral Disc Disease: A Nationwide Sample Cohort Study With a 10-year Follow-up. Spine 2019, 44, 1382–1389. [Google Scholar] [CrossRef]
- Wang, S.J.; Chen, B.H.; Wang, P.; Liu, C.S.; Yu, J.M.; Ma, X.X. The effect of percutaneous endoscopic lumbar discectomy under different anesthesia on pain and immunity of patients with prolapse of lumbar intervertebral disc. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 2793–2799. [Google Scholar]
- Liu, C.; Chu, L.; Yong, H.C.; Chen, L.; Deng, Z.L. Percutaneous Endoscopic Lumbar Discectomy for Highly Migrated Lumbar Disc Herniation. Pain Physician 2017, 20, E75–E84. [Google Scholar]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2952, discussion 2952. [Google Scholar] [CrossRef]
- Breivik, H.; Borchgrevink, P.C.; Allen, S.M.; Rosseland, L.A.; Romundstad, L.; Hals, E.K.; Kvarstein, G.; Stubhaug, A. Assessment of pain. Br. J. Anaesth. 2008, 101, 17–24. [Google Scholar] [CrossRef]
- Ahn, Y.; Lee, S.H.; Park, W.M.; Lee, H.Y.; Shin, S.W.; Kang, H.Y. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: Surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine 2004, 29, E326–E332. [Google Scholar] [CrossRef]
- Choi, G.; Modi, H.N.; Prada, N.; Ahn, T.J.; Myung, S.H.; Gang, M.S.; Lee, S.H. Clinical results of XMR-assisted percutaneous transforaminal endoscopic lumbar discectomy. J. Orthop. Surg. Res. 2013, 8, 14. [Google Scholar] [CrossRef]
- Choi, K.C.; Kim, J.S.; Ryu, K.S.; Kang, B.U.; Ahn, Y.; Lee, S.H. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: Transforaminal versus interlaminar approach. Pain Physician 2013, 16, 547–556. [Google Scholar] [PubMed]
- Heo, J.H.; Kim, C.H.; Chung, C.K.; Choi, Y.; Seo, Y.G.; Kim, D.H.; Park, S.B.; Moon, J.H.; Heo, W.; Jung, J.M. Quantity of Disc Removal and Radiological Outcomes of Percutaneous Endoscopic Lumbar Discectomy. Pain Physician 2017, 20, E737–E746. [Google Scholar] [PubMed]
- Sclafani, J.A.; Kim, C.W. Complications associated with the initial learning curve of minimally invasive spine surgery: A systematic review. Clin. Orthop. Relat. Res. 2014, 472, 1711–1717. [Google Scholar] [CrossRef]
- Hao, Y.; Liu, T.; Yu, L.; Ma, C.; Liu, Y.; Li, Z.; Zhang, D. Percutaneous transforaminal endoscopic discectomy combined with Coflex interspinous process dynamic reconstruction system in treatment of youth lumbar disc herniation. Chin. J. Reparative Reconstr. Surg. 2017, 31, 191–196. [Google Scholar]
- Fan, G.; Guan, X.; Sun, Q.; Hu, A.; Zhu, Y.; Gu, G.; Zhang, H.; He, S. Puncture Reduction in Percutaneous Transforaminal Endoscopic Discectomy with HE’s Lumbar LOcation (HELLO) System: A Cadaver Study. PLoS ONE 2015, 10, e0144939. [Google Scholar] [CrossRef][Green Version]
- Ahn, Y.; Kim, C.H.; Lee, J.H.; Lee, S.H.; Kim, J.S. Radiation exposure to the surgeon during percutaneous endoscopic lumbar discectomy: A prospective study. Spine 2013, 38, 617–625. [Google Scholar] [CrossRef]
- Ye, C.P.; Zhu, J.J. Treatment of senile lumbar nerve root canal stenosis with micro-endoscope discectomy. Zhongguo Gu Shang 2013, 26, 805–809. [Google Scholar]
- Goldfield, N.; Gnani, S.; Majeed, A. Primary care in the United States: Profiling performance in primary care in the United States. BMJ 2003, 326, 744–747. [Google Scholar] [CrossRef]
- Hoogland, T.; Schubert, M.; Miklitz, B.; Ramirez, A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: A prospective randomized study in 280 consecutive cases. Spine 2006, 31, E890–E897. [Google Scholar] [CrossRef]
- Clavien, P.A.; Puhan, M.A. Biased reporting in surgery. Br. J. Surg. 2014, 101, 591–592. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6; John Wiley & Sons: Hoboken, NJ, USA, 2006. [Google Scholar]
- Terrin, N.; Schmid, C.H.; Lau, J. In an empirical evaluation of the funnel plot, researchers could not visually identify publication bias. J. Clin. Epidemiol. 2005, 58, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.; Ioannidis, J.P.; Terrin, N.; Schmid, C.H.; Olkin, I. The case of the misleading funnel plot. BMJ 2006, 333, 597–600. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.G.; Fu, Q. Percutaneous transforaminal endoscopic discectomy through different approaches for lumbar disc herniation. Zhongguo Gu Shang 2012, 25, 1057–1060. [Google Scholar] [PubMed]
| Article (Author and Year) | Study Type | Operation Method | Number of Patients | Age (Year) | Follow-Up Time (Month) | Outcome Indicators |
|---|---|---|---|---|---|---|
| Ma et al., 2022 | Retrospective | PTED | 46 | 45.80 ± 17.15 | 24 | 8 9 10 11 |
| OD | 45 | 40.49 ± 15.21 | 24 | |||
| Wang et al., 2021 | Retrospective | PTED | 69 | 51.25 ± 17.26 | 6 | 1 2 5 6 7 9 10 |
| MED | 86 | 47.26 ± 16.49 | 6 | |||
| Rajamani et al., 2021 | Retrospective | PTED | 86 | 39.4 ± 12.38 | 24 | 1 2 3 5 6 7 10 |
| MED | 351 | 44.3 + 12.76 | 24 | |||
| OD | 145 | 37.6 + 7.39 | 24 | |||
| Jing et al., 2021 | Retrospective | PTED | 31 | 51.32 + 8.99 | 27.71 + 1.92 | 1 2 3 5 8 9 |
| MED | 31 | 50.19 + 9.36 | 27.26 + 1.53 | |||
| Jarebi et al., 2021 | Retrospective | PTED | 29 | 47.21 ± 12.55 | 24 | 5 6 7 8 9 10 |
| MED | 29 | 46.97 ± 12.55 | 24 | |||
| Meyer et al., 2020 | RCT | PTED | 23 | 47.2 ± 10.6 | 12 | 6 8 9 10 |
| MED | 24 | 45.2 ± 10.6 | 12 | |||
| Chen et al., 2020 | RCT | PTED | 119 | 40.9 + 11.9 | 24 | 6 7 8 9 10 |
| MED | 122 | 41.0 + 10.8 | 24 | |||
| Kim et al., 2019 | Retrospective | PTED | 173 | 46.49 + 14.28 | 120 | 10 |
| OD | 1683 | 46.49 + 14.28 | 120 | |||
| Ahn et al., 2019 | Retrospective | PTED | 146 | 32.7 (16–70) | 60 | 1 5 6 7 9 10 |
| OD | 152 | 35.4 (14–77) | 60 | |||
| Chen et al., 2018 | RCT | PTED | 80 | 40 ± 11.4 | 12 | 1 4 5 6 7 8 9 10 |
| MED | 73 | 40.7 ± 11.1 | 12 | |||
| Liu et al., 2018 | Retrospective | PTED | 60 | 36.2 ± 5.9 | 28.2 ± 2.5 | 1 2 3 6 7 8 9 |
| MED | 63 | 33.1 ± 6.7 | 29.6 ± 3.7 | |||
| Gibson et al., 2016 | RCT | PTED | 70 | 42 ± 9 | 24 | 6 7 8 10 |
| MED | 70 | 39 ± 9 | 24 | |||
| Sun et al., 2017 | Retrospective | PTED | 11 | 54.91 ± 8. 28 | 12 | 1 2 4 5 6 7 |
| OD | 13 | 58.08 ± 11.30 | 12 | |||
| Ahn et al., 2015 | Retrospective | PTED | 32 | 22.41 ± 1.68 | 13.69 ± 1.26 | 1 5 6 7 8 9 |
| OD | 34 | 22.18 ± 1.51 | 13.41 ± 1.02 | |||
| Pan et al., 2016 | Retrospective | PTED | 48 | 39.5 | 12 | 1 2 5 6 7 |
| OD | 58 | 42.8 | 12 | |||
| Ariun et al., 2015 | Retrospective | PTED | 36 | 44.17 ± 6.54 | 12 | 1 5 7 11 |
| MED | 50 | 41.46 ± 7.22 | 12 | |||
| Hsien-TA et al., 2012 | Retrospective | PTED | 57 | 44.2 | 20.4 (12–24) | 1 7 8 9 10 |
| MED | 66 | 50.4 | 20.4 (12–24) | |||
| Lee et al., 2009 | Retrospective | PTED | 25 | 42.0 ± 11.4 | 34.0 ± 4.4 | 1 5 6 7 8 9 |
| MED | 29 | 47.7 ± 12.2 | 34.3 ± 4.6 | |||
| Li et al., 2018 | Retrospective | PTED | 48 | 18.96 ± 1.99 | 68.87 ± 7.03 | 1 2 5 6 7 9 |
| MED | 30 | 19.40 ± 1.50 | 67.07 ± 6.76 | |||
| Ding et al., 2017 | RCT | PTED | 50 | 41.32 ± 11.53 | 41.32 ± 11.53 | 1 3 4 5 6 7 11 |
| OD | 50 | 43.90 ± 11.8 | 43.90 ± 11.8 | |||
| Chang et al., 2017 | Retrospective | PTED | 60 | 52.54 ± 4.12 | 52.54 ± 4.12 | 1 2 3 4 6 |
| OD | 50 | 53.67 ± 4.28 | 53.67 ± 4.28 | |||
| Li et al., 2018 | Retrospective | PTED | 33 | 43.9 ± 11.6 | 43.9 ± 11.6 | 1 2 5 6 |
| OD | 30 | 46.1 ± 13.2 | 46.1 ± 13.2 | |||
| Jeoug et al., 2006 | Retrospective | PTED | 22 | 56 ± 9.12 | 12 | 1 6 11 |
| OD | 25 | 56.45 ± 10.89 | 12 | |||
| Pan et al., 2014 | RCT | PTED | 10 | No discussion | 6 | 2 3 5 6 11 |
| OD | 10 | No discussion | 6 | |||
| Song et al., 2017 | Retrospective | PTED | 30 | 54.8 ± 6.5 | 18 | 1 2 3 4 7 11 |
| MED | 30 | 53.6 ± 6.4 | 18 | |||
| Liu et al., 2016 | Retrospective | PTED | 209 | 57.2 | 46.5 (12–69) | 6 7 9 11 |
| OD | 192 | 55.9 | 46.5 (12–69) | |||
| Choi et al., 2016 | Retrospective | PTED | 20 | 33.9 ± 11.1 | 27.5 ± 5.7 | 1 5 6 7 9 10 |
| MED | 23 | 38 ± 11.6 | 27.5 ± 5.7 | |||
| Yao et al., 2016 | Retrospective | PTED | 47 | 47.91 ± 14.77 | 47.91 ± 14.77 | 1 5 6 7 9 |
| OD | 58 | 46.76 ± 12.37 | 46.76 ± 12.37 | |||
| Kim et al., 2007 | Retrospective | PTED | 301 | 34.9 | 23.6 (18–36) | 1 8 9 10 11 |
| MED | 614 | 44.4 | 23.6 (18–36) | |||
| Wang et al., 2013 | Retrospective | PTED | 25 | 17.9 ± 1.9 | No discussion | 1 2 5 8 9 |
| MED | 80 | 17.9 ± 1.9 | No discussion | |||
| OD | 16 | 17.9 ± 1.9 | No discussion | |||
| Chen et al., 2015 | Retrospective | PTED | 18 | 57.4 ± 12.4 | 24 | 1 5 8 |
| OD | 25 | 54.9 ± 16. 6 | 24 | |||
| Li et al., 2015 | Retrospective | PTED | 30 | 17.9 ± 10.4 | 12 | 1 2 5 7 11 |
| OD | 26 | 18.8 ± 10.4 | 12 | |||
| Mayer et al., 1993 | RCT | PTED | 20 | 39.8 ± 10.4 | 24 | 1 8 9 10 |
| MED | 20 | 42.7 ± 10 | 24 |
| Included Studies (Author and Year) | Study Type | Rated Items | Quality Score | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Selection (4) | Comparability (2) | Outcomes (3) | ||||||||
| ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | |||
| Ma et al., 2022 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Wang et al., 2021 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Rajamani et al., 2021 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Jing et al., 2021 | Retrospective | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (Hi-Q) |
| Jarebi et al., 2021 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Kim et al., 2019 | Retrospective | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (Hi-Q) |
| Ahn et al., 2019 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Liu et al., 2018 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Sun et al., 2017 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Ahn et al., 2015 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Pan et al., 2016 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Ariun et al., 2015 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Hsien-Ta et al., 2012 | Retrospective | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 (Hi-Q) |
| Lee et al., 2009 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Li et al., 2018 | Retrospective | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (Hi-Q) |
| Chang et al., 2017 | Retrospective | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (Hi-Q) |
| Li et al., 2018 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Jeoug et al., 2006 | Retrospective | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (Hi-Q) |
| Song et al., 2017 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Liu et al., 2016 | Retrospective | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Choi et al., 2016 | Retrospective | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (Hi-Q) |
| Yao et al., 2016 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Kim et al., 2007 | Retrospective | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (Hi-Q) |
| Wang et al., 2013 | Retrospective | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 (Hi-Q) |
| Chen et al., 2015 | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Li et al., 2015 | Retrospective | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 (Hi-Q) |
| Studies (Author and Year) | Study Type | Randomization (2) | Concealment of Allocation (2) | Double Blinding (2) | Withdrawals and Dropouts (1) | Quality Evaluation |
|---|---|---|---|---|---|---|
| Meyer et al., 2020 | RCT | 2 | 1 | 0 | 1 | 4 (high quality) |
| Chen et al., 2020 | RCT | 2 | 2 | 2 | 1 | 7 (high quality) |
| Chen et al., 2016 | RCT | 2 | 2 | 2 | 1 | 7 (high quality) |
| Gibson et al., 2016 | RCT | 2 | 2 | 1 | 1 | 7 (high quality) |
| Ding et al., 2017 | RCT | 1 | 0 | 0 | 1 | 3 (low quality) |
| Pan et al., 2014 | RCT | 1 | 1 | 0 | 1 | 3 (low quality) |
| Mayer et al., 1993 | RCT | 2 | 1 | 0 | 1 | 4 (Igh quality) |
| Outcome | Control Group | Treatment Effects Difference | p for Treatment Effects Difference | I2 for Heterogeneity | p for Heterogeneity |
|---|---|---|---|---|---|
| Average operative time (min) | PTED vs. MED | MD = −8.74, −24.15 to 6.66 | p = 0.27 | I2 = 99% | p < 0.00001 |
| PTED vs. OD | MD = −22.50, −41.03 to −3.98 | p = 0.02 | I2 = 99% | p < 0.00001 | |
| Intraoperative blood loss (ml) | PTED vs. MED | MD = −24.96, −34.12 to −15.81 | p < 0.00001 | I2 = 99% | p < 0.00001 |
| PTED vs. OD | MD = −89.29, −111.80 to −66.79 | p <0.00001 | I2 = 99% | p < 0.00001 | |
| Size of the incision (cm) | PTED vs. MED | MD =−1.56, −2.63 to −0.50 | p = 0.004 | I2 = 100% | p < 0.00001 |
| PTED vs. OD | MD = −3.11, −3.99 to −2. 22 | p < 0.00001 | I2 = 99% | p < 0.00001 | |
| Postoperative bed rest time (day) | PTED vs. MED | MD = −2.45, −4.13 to −0.76 | p = 0.004 | I2 = 97% | p < 0.00001 |
| PTED vs. OD | MD = −5.00, −6.27 to −3.73 | p < 0.00001 | I2 = 91% | p < 0.0001 | |
| Hospitalization time (day) | PTED vs. MED | MD = −2.42, −3.21 to −1.63 | p < 0.00001 | I2 = 95% | p < 0.00001 |
| PTED vs. OD | MD = −6.38, −7.69 to −5.08 | p < 0.00001 | I2 = 96% | p < 0.00001 | |
| Leg pain | PTED vs. MED | MD = −0.23, −0.61 to 0.15 | p = 0.60 | I2 = 51% | p = 0.03 |
| PTED vs. OD | MD = −0.05, −0.13 to 0.04 | p = 0.28 | I2 = 29% | p = 0.22 | |
| Low back pain | PTED vs. MED | MD = −0.49, −0.84 to −0.14 | p = 0.006 | I2 = 90% | p < 0.00001 |
| PTED vs. OD | MD = 0.30, −0.28 to 0.88 | p = 0.31 | I2 = 98% | p < 0.00001 | |
| Postoperative comprehensive pain | PTED vs. OD | MD = −0.81, −1.71 to 0.08 | p = 0.07 | I2 = 93% | p < 0.00001 |
| Postoperative ODI index | PTED vs. MED | MD = −2.21, −4.17 to −0.25 | p = 0.03 | I2 = 88% | p < 0.00001 |
| PTED vs. OD | MD = −0.62, −1.25 to 0.01 | p = 0.05 | I2 = 68% | p = 0.002 | |
| Incidence of complications | PTED vs. MED | OR = 0.94, 0.67 to 1.32 | p = 0.71 | I2 = 0% | p = 0.65 |
| PTED vs. OD | OR = 0.81, 0.50 to 1.31 | p = 0.39 | I2 = 0% | p = 0.47 | |
| Incidence of recurrence | PTED vs. MED | OR = 1.55, 1.07 to 2.24 | p = 0.02 | I2 = 0% | p = 0.93 |
| PTED vs. OD | OR = 1.72, 1.02 to 2.90 | p = 0.04 | I2 = 41% | p = 0.11 | |
| Revision rate | PTED vs. MED | OR = 1.67, 1.17 to 2.36 | p = 0.004 | I2 = 0% | p = 0.89 |
| PTED vs. OD | OR = 2.15, 1.25 to 3.70 | p= 0.006 | I2 = 0% | p = 0.55 | |
| Rates of successful operation | PTED vs. MED | OR = 0.64, 0.33 to 1.25 | p = 0.16 | I2 = 0% | p = 0.98 |
| PTED VS OD | OR = 0.75, 0.43 to 1.33 | p = 0.33 | I2 = 0% | p = 0.76 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, X.-m.; Chen, A.-f.; Lou, X.-x.; Zhang, Y.-g. Comparison of Three Common Intervertebral Disc Discectomies in the Treatment of Lumbar Disc Herniation: A Systematic Review and Meta-Analysis Based on Multiple Data. J. Clin. Med. 2022, 11, 6604. https://doi.org/10.3390/jcm11226604
Zhao X-m, Chen A-f, Lou X-x, Zhang Y-g. Comparison of Three Common Intervertebral Disc Discectomies in the Treatment of Lumbar Disc Herniation: A Systematic Review and Meta-Analysis Based on Multiple Data. Journal of Clinical Medicine. 2022; 11(22):6604. https://doi.org/10.3390/jcm11226604
Chicago/Turabian StyleZhao, Xiao-ming, An-fa Chen, Xiao-xiao Lou, and Yin-gang Zhang. 2022. "Comparison of Three Common Intervertebral Disc Discectomies in the Treatment of Lumbar Disc Herniation: A Systematic Review and Meta-Analysis Based on Multiple Data" Journal of Clinical Medicine 11, no. 22: 6604. https://doi.org/10.3390/jcm11226604
APA StyleZhao, X.-m., Chen, A.-f., Lou, X.-x., & Zhang, Y.-g. (2022). Comparison of Three Common Intervertebral Disc Discectomies in the Treatment of Lumbar Disc Herniation: A Systematic Review and Meta-Analysis Based on Multiple Data. Journal of Clinical Medicine, 11(22), 6604. https://doi.org/10.3390/jcm11226604





