Management and Clinical Outcome of Aortic Graft Infections: A Single-Center Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
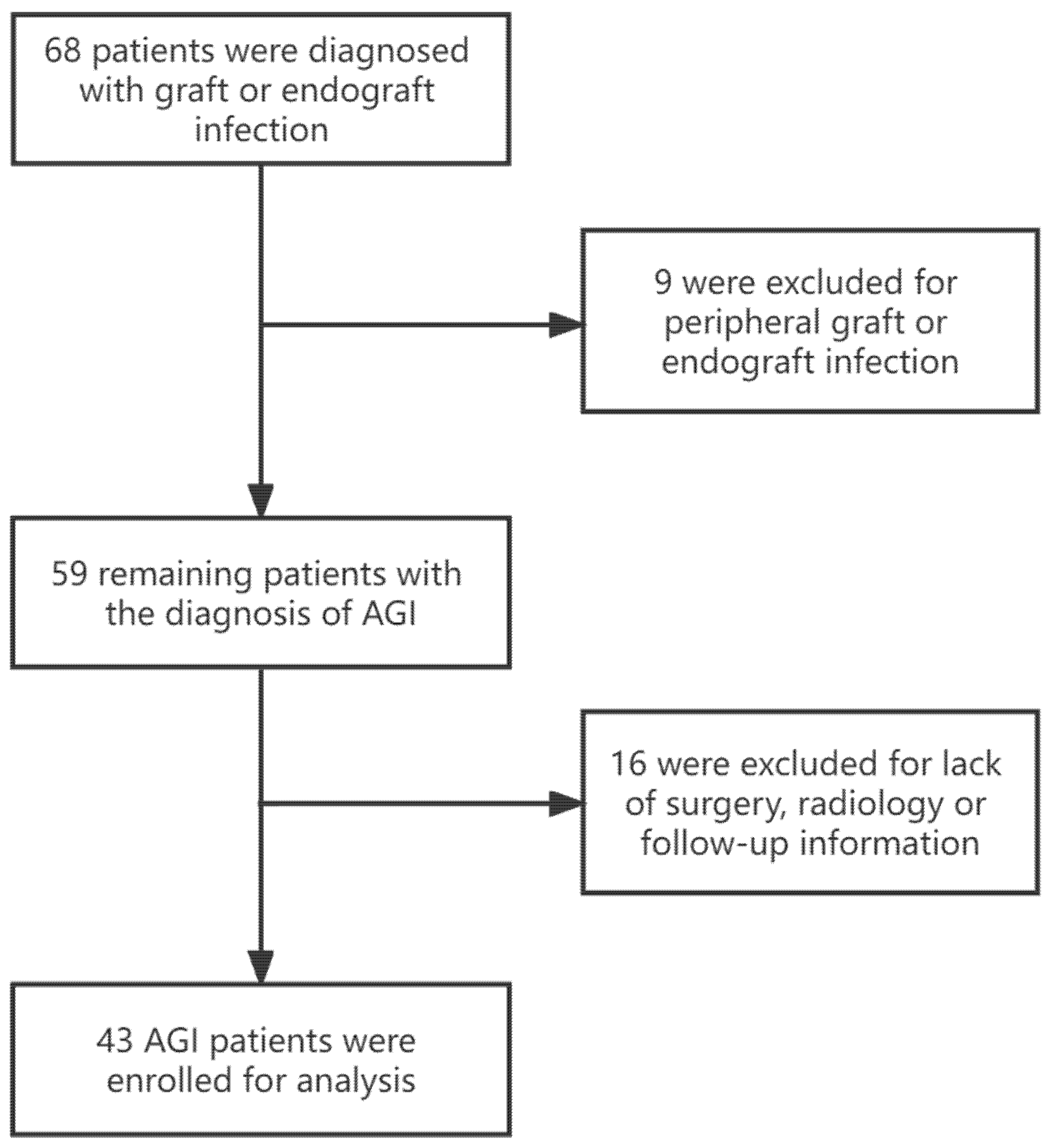
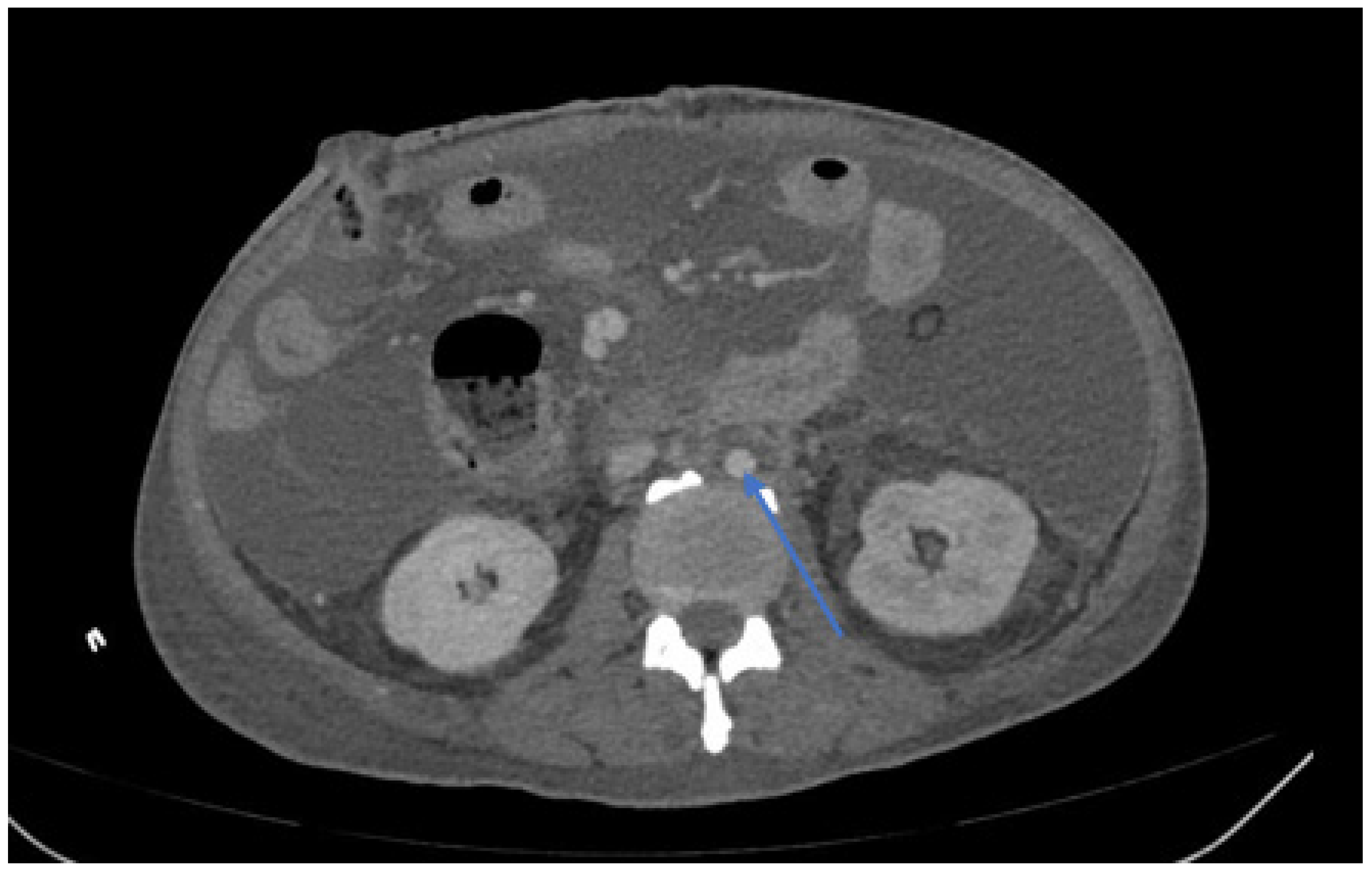
2.1. Study Population and Diagnostic Criteria of AGIs
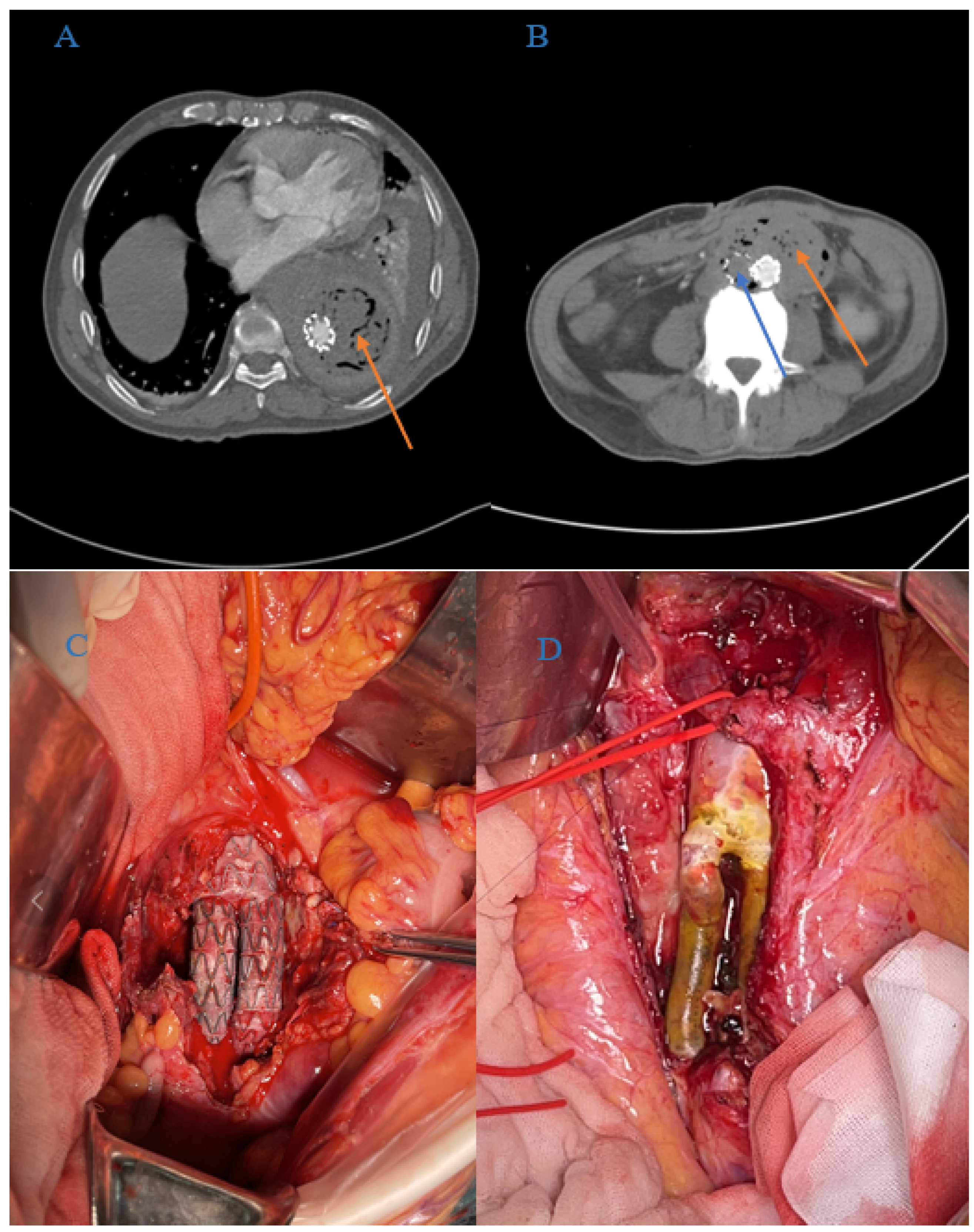
2.2. Peri-Operative Management and Operation Methods
2.3. Post-Operative Treatment and Follow-Up Management
2.4. Primary and Secondary Endpoints
2.5. Statistical Analysis and Ethics Approval
3. Results
3.1. Baseline Characteristics
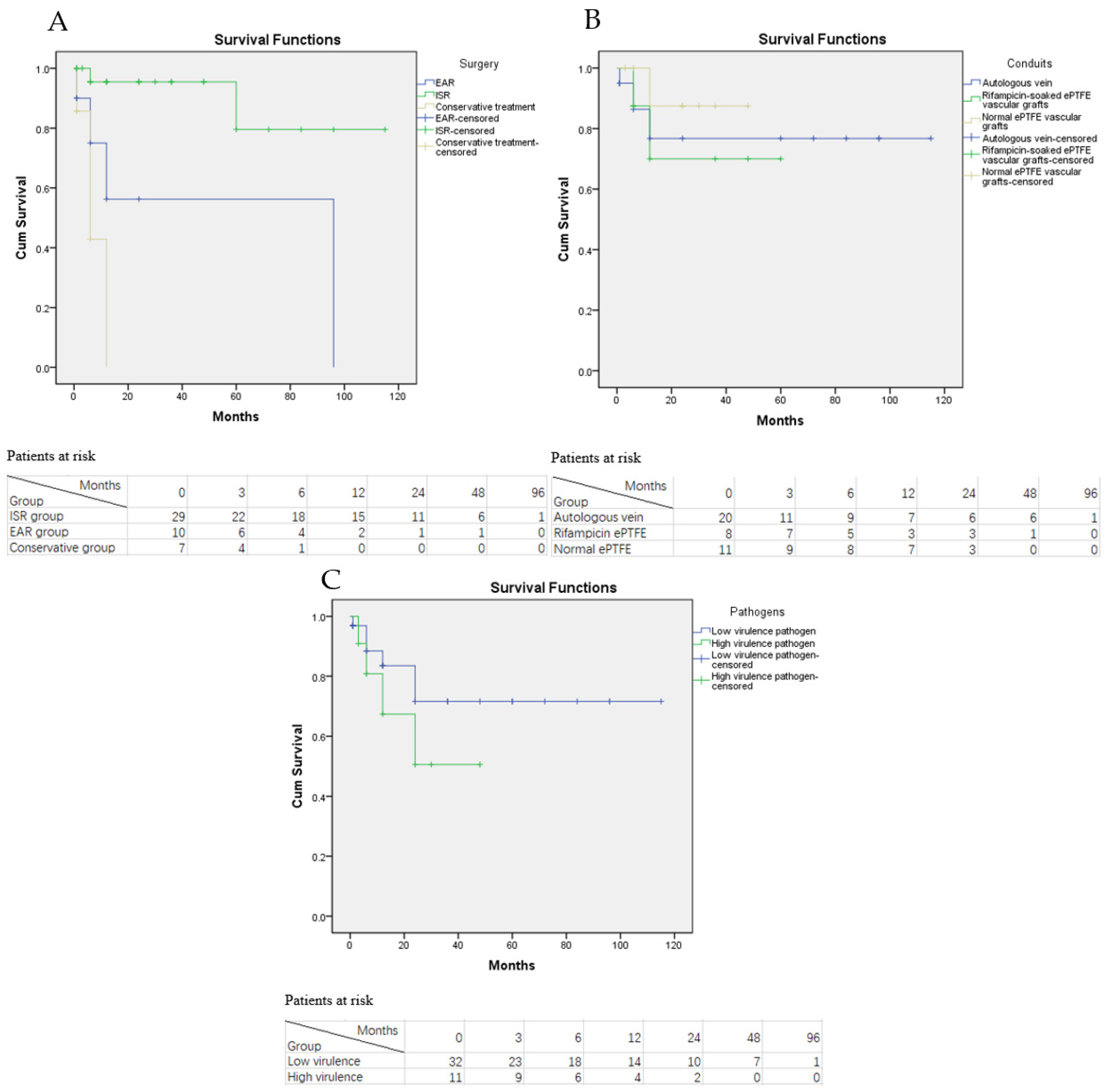
3.2. Outcomes
3.2.1. Early Mortality and Complication-Related Morbidity
3.2.2. RI Rate
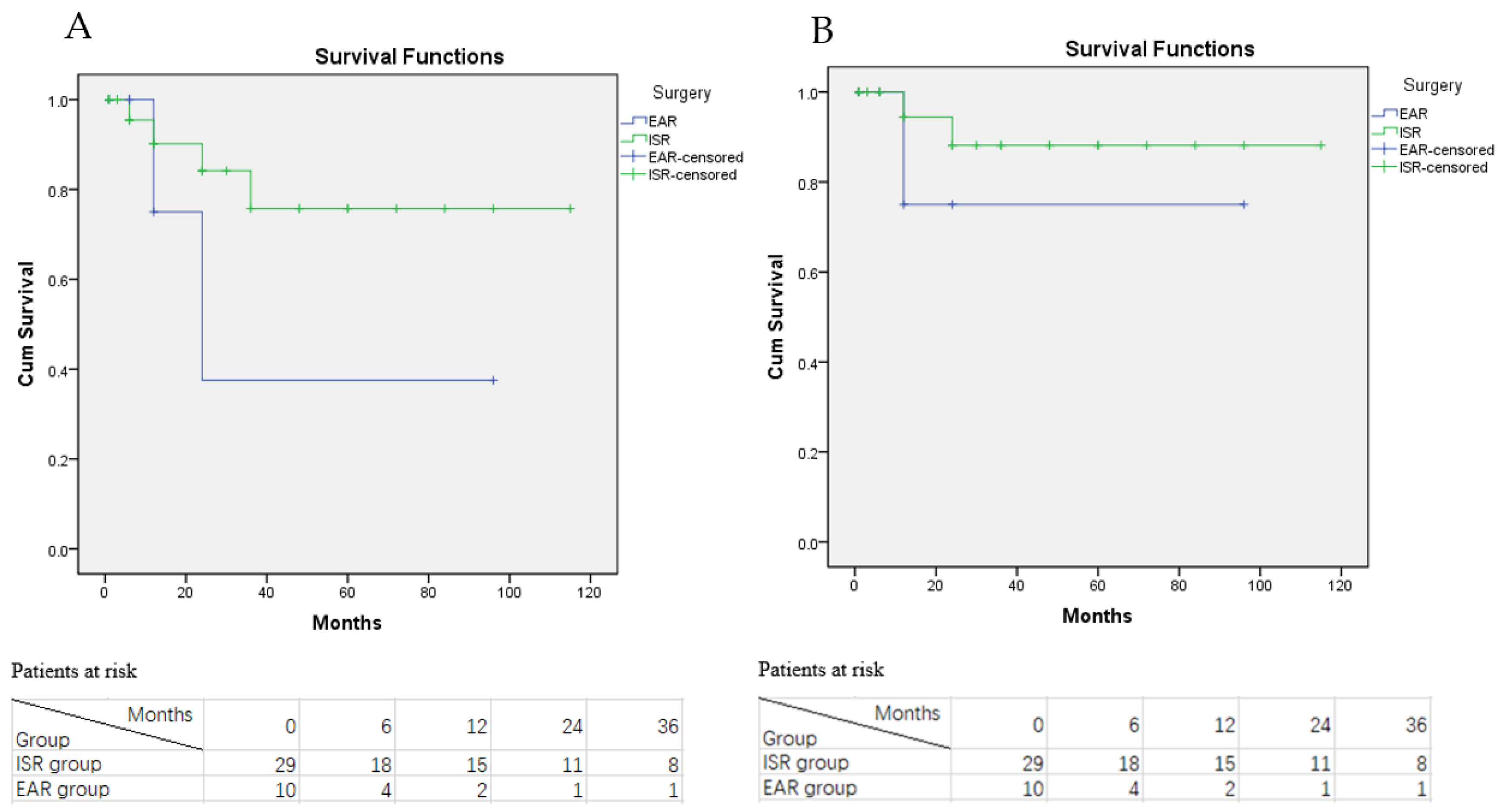
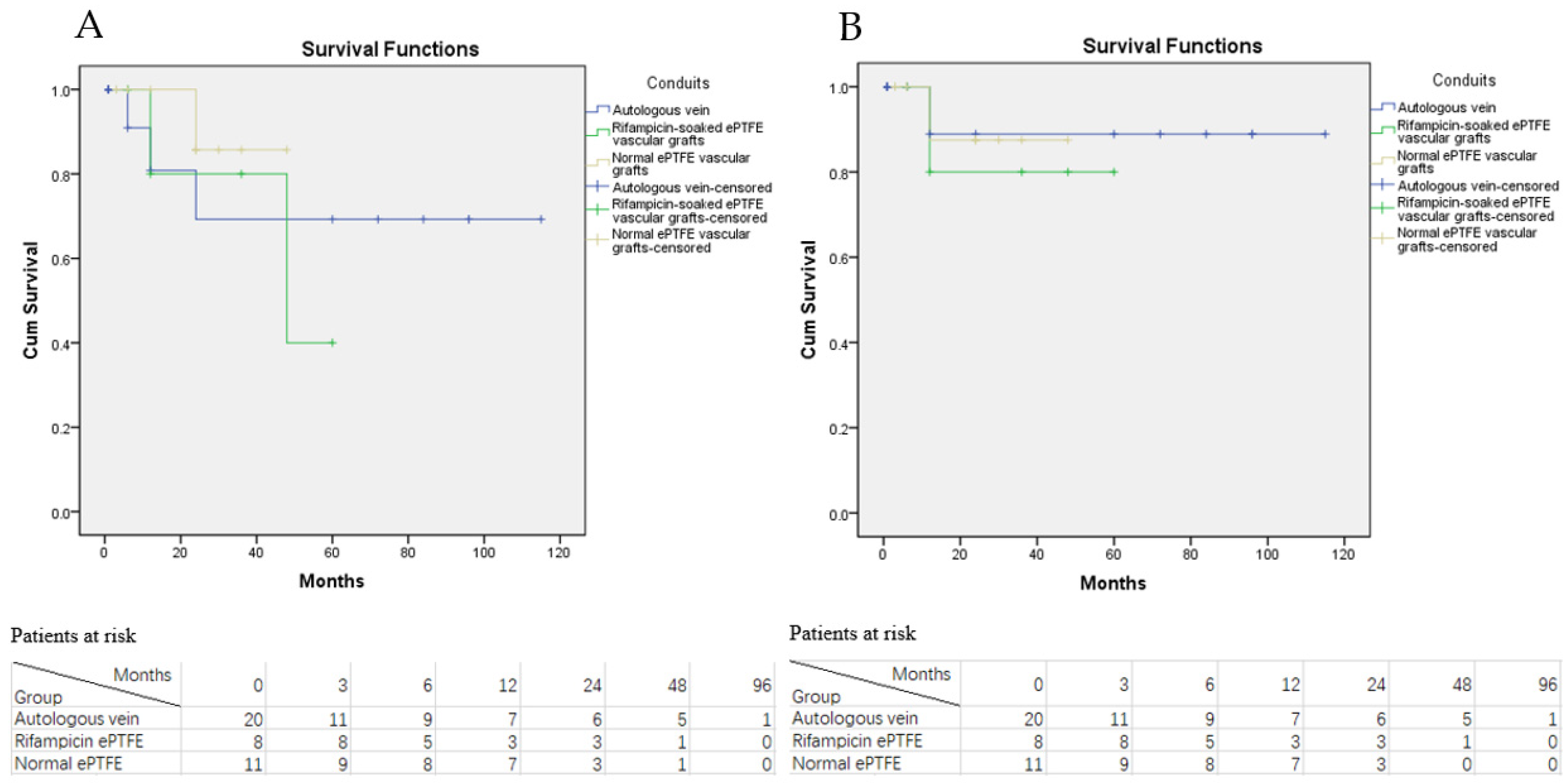
3.2.3. Primary and Secondary Graft Patency
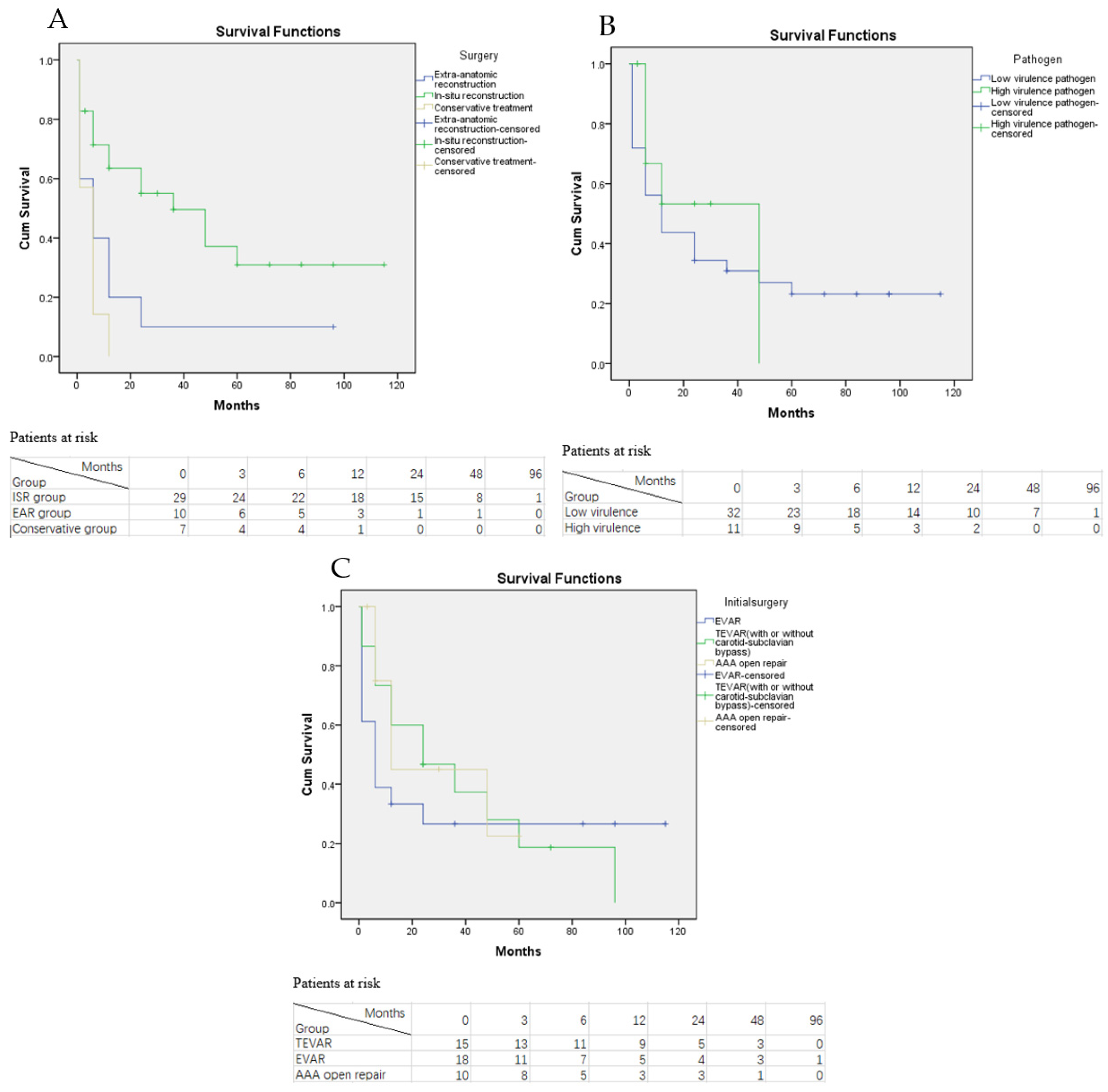
3.2.4. Overall Mortality
3.2.5. Duration of Antibiotic Therapy and Types of Antibiotics Used
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kahlberg, A.; Melissano, G.; Mascia, D.; Loschi, D.; Grandi, A.; Chiesa, R. How to best treat infectious complications of open and endovascular thoracic aortic repairs. Semin. Vasc. Surg. 2017, 30, 95–102. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, P.J.; Hertzer, N.R.; Beven, E.G.; Krajewski, L.P. Surgical management of infected abdominal aortic grafts: Review of a 25-year experience. J. Vasc. Surg. 1986, 3, 725–731. [Google Scholar] [CrossRef]
- Reilly, L.M.; Altman, H.; Lusby, R.J.; Kersh, R.A.; Ehrenfeld, W.K.; Stoney, R.J. Late results following surgical management of vascular graft infection. J. Vasc. Surg. 1984, 1, 36–44. [Google Scholar] [CrossRef]
- Kuestner, L.M.; Reilly, L.M.; Jicha, D.L.; Ehrenfeld, W.K.; Goldstone, J.; Stoney, R.J. Secondary aortoenteric fistula: Contemporary outcome with use of extraanatomic bypass and infected graft excision. J. Vasc. Surg. 1995, 21, 184–195. [Google Scholar] [CrossRef]
- Kahlberg, A.; Grandi, A.; Loschi, D.; Vermassen, F.; Moreels, N.; Chakfé, N.; Melissano, G.; Chiesa, R. A systematic review of infected descending thoracic aortic grafts and endografts. J. Vasc. Surg. 2019, 69, 1941–1951. [Google Scholar] [CrossRef]
- Batt, M.; Jean-Baptiste, E.; O’Connor, S.; Feugier, P.; Haulon, S. Contemporary management of infrarenal aortic graft infection: Early and late results in 82 patients. Vascular 2012, 20, 129–137. [Google Scholar] [CrossRef]
- Oderich, G.S.; Bower, T.C.; Cherry, K.J.; Panneton, J.M.; Sullivan, T.M.; Noel, A.A.; Carmo, M.; Cha, S.; Kalra, M.; Gloviczki, P. Evolution from axillofemoral to in situ prosthetic reconstruction for the treatment of aortic graft infections at a single center. J. Vasc. Surg. 2006, 43, 1166–1174. [Google Scholar] [CrossRef]
- Chakfé, N.; Diener, H.; Lejay, A.; Assadian, O.; Berard, X.; Caillon, J.; Fourneau, I.; Glaudemans, A.W.; Koncar, I.; Lindholt, J.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Vascular Graft and Endograft Infections. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 339–384. [Google Scholar] [CrossRef]
- Batt, M.; Jean-Baptiste, E.; O’Connor, S.; Bouillanne, P.-J.; Haudebourg, P.; Hassen-Khodja, R.; Declemy, S.; Farhad, R. In-situ revascularisation for patients with aortic graft infection: A single centre experience with silver coated polyester grafts. Eur. J. Vasc. Endovasc. Surg. 2008, 36, 182–188. [Google Scholar] [CrossRef]
- Yeager, R.A.; Taylor, L.M.; Moneta, G.L.; Edwards, J.M.; Nicoloff, A.D.; McConnell, D.B.; Porter, J.M. Improved results with conventional management of infrarenal aortic infection. J. Vasc. Surg. 1999, 30, 76–83. [Google Scholar] [CrossRef]
- Walker, W.E.; Cooley, D.A.; Duncan, J.M.; Hallman, G.L.; Ott, D.A.; Reul, G.J. The management of aortoduodenal fistula by In Situ replacement of the infected abdominal aortic graft. Ann. Surg. 1987, 205, 727–732. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, C.R.; Casaca, R.; de Almeida, J.C.M.; Mendes-Pedro, L. Enteric Repair in aortoduodenal fistulas: A forgotten but often lethal player. Ann. Vasc. Surg. 2014, 28, 756–762. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, S.; Andrew, P.; Batt, M.; Becquemin, J.P. A systematic review and meta-analysis of treatments for aortic graft infection. J. Vasc. Surg. 2006, 44, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Siracuse, J.J.; Nandivada, P.; Giles, K.A.; Hamdan, A.D.; Wyers, M.C.; Chaikof, E.L.; Pomposelli, F.B.; Schermerhorn, M.L. Prosthetic graft infections involving the femoral artery. J. Vasc. Surg. 2013, 57, 700–705. [Google Scholar] [CrossRef]
- Andriolo, B.N.; Andriolo, R.B.; Salomão, R.; Atallah, N. Effectiveness and safety of procalcitonin evaluation for reducing mortality in adults with sepsis, severe sepsis or septic shock. Cochrane Database Syst. Rev. 2017, 1, CD010959. [Google Scholar] [CrossRef]
- Hingorani, A.; Van Der Windt, D.A.; Riley, R.D.; Abrams, K.; Moons, K.G.M.; Steyerberg, E.; Schroter, S.; Sauerbrei, W.; Altman, D.G.; Hemingway, H.; et al. Prognosis research strategy (PROGRESS) 4: Stratified medicine research. BMJ 2013, 346, e5793. [Google Scholar] [CrossRef]
- Tang, B.M.; Eslick, G.D.; Craig, J.C.; McLean, A.S. Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: Systematic review and meta-analysis. Lancet Infect. Dis. 2007, 7, 210–217. [Google Scholar] [CrossRef]
- Schuhmann, M.U.; Ostrowski, K.R.; Draper, E.J.; Chu, J.W.; Ham, S.D.; Sood, S.; McAllister, J.P. The value of C-reactive protein in the management of shunt infections. J. Neurosurg. Pediatrics 2005, 103, 223–230. [Google Scholar] [CrossRef]
- Garot, M.; Delannoy, P.-Y.; Meybeck, A.; Sarraz-Bournet, B.; D’Elia, P.; D’Escrivan, T.; Devos, P.; Leroy, O. Intra-abdominal aortic graft infection: Prognostic factors associated with in-hospital mortality. BMC Infect. Dis. 2014, 14, 215. [Google Scholar] [CrossRef]
- Batt, M.; Jean-Baptiste, E.; O’Connor, S.; Saint-Lebes, B.; Feugier, P.; Patra, P.; Midy, D.; Haulon, S. Early and late results of contemporary management of 37 secondary aortoenteric fistulae. Eur. J. Vasc. Endovasc. Surg. 2011, 41, 748–757. [Google Scholar] [CrossRef]
- Touma, J.; Cochennec, F.; Parisot, J.; Legendre, A.F.; Becquemin, J.-P.; Desgranges, P. In Situ reconstruction in native and prosthetic aortic infections using cryopreserved arterial allografts. Eur. J. Vasc. Endovasc. Surg. 2014, 48, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Spiliotopoulos, K.; Preventza, O.; Green, S.Y.; Price, M.D.; Amarasekara, H.S.; Davis, B.M.; de la Cruz, K.I.; LeMaire, S.A.; Coselli, J.S. Open descending thoracic or thoracoabdominal aortic approaches for complications of endovascular aortic procedures: 19-year experience. J. Thorac. Cardiovasc. Surg. 2018, 155, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Dorweiler, B.; Neufang, A.; Chaban, R.; Reinstadler, J.; Duenschede, F.; Vahl, C.-F. Use and durability of femoral vein for autologous reconstruction with infection of the aortoiliofemoral axis. J. Vasc. Surg. 2014, 59, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Heinola, I.; Kantonen, I.; Jaroma, M.; Albäck, A.; Vikatmaa, P.; Aho, P.; Venermo, M. Editor’s Choice—Treatment of aortic prosthesis infections by graft removal and In Situ replacement with autologous femoral veins and fascial strengthening. Eur. J. Vasc. Endovasc. Surg. 2016, 51, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Batt, M.; Feugier, P.; Camou, F.; Coffy, A.; Senneville, E.; Caillon, J.; Calvet, B.; Chidiac, C.; Laurent, F.; Revest, M.; et al. A meta-analysis of outcomes after In Situ reconstructions for aortic graft infection. Angiology 2017, 69, 370–379. [Google Scholar] [CrossRef]
- Phang, D.; Smeds, M.R.; Abate, M.; Ali, A.; Long, B.; Rahimi, M.; Giglia, J.; Bath, J. Revascularization with obturator or hemi-neoaortoiliac system for partial aortic graft infections. Ann. Vasc. Surg. 2019, 54, 166–175. [Google Scholar] [CrossRef]
- Mirzaie, M.; Schmitto, J.; Tirilomis, T.; Fatehpur, S.; Liakopoulos, O.; Teucher, N.; Dörge, H.; Schöndube, F. Surgical management of vascular graft infection in severely ill patients by partial resection of the infected prosthesis. Eur. J. Vasc. Endovasc. Surg. 2007, 33, 610–613. [Google Scholar] [CrossRef]
- Simmons, C.D.; Ali, A.T.; Foteh, K.; Abate, M.R.; Smeds, M.R.; Spencer, H.J.; Clagett, G.P. Unilateral inline replacement of infected aortofemoral graft limb with femoral vein. J. Vasc. Surg. 2017, 65, 1121–1129. [Google Scholar] [CrossRef]
- Bandyk, D.F.; Novotney, M.L.; Johnson, B.L.; Back, M.R.; Roth, S.R. Use of rifampin-soaked gelatin-sealed polyester grafts for In Situ treatment of primary aortic and vascular prosthetic infections. J. Surg. Res. 2001, 95, 44–49. [Google Scholar] [CrossRef]
- Hayes, P.D.; Nasim, A.; London, N.J.; Sayers, R.D.; Barrie, W.W.; Bell, P.R.; Naylor, A. In situ replacement of infected aortic grafts with rifampicin-bonded prostheses: The Leicester experience (1992 to 1998). J. Vasc. Surg. 1999, 30, 92–98. [Google Scholar] [CrossRef]
| Baseline Information and Clinical Presentations | n (%) |
|---|---|
| Demographics | |
| Male, n (%) | 30 (69%) |
| Median age(IQR) | 70 (57–78) |
| Pre-operative comorbidities, n(%) | |
| Hypertension | 31 (72%) |
| Smoking/Past smoking history | 25 (58%) |
| Diabetes mellitus | 17 (39%) |
| Chronic obstructive pulmonary disease | 11 (25%) |
| Hypoproteinemia | 10 (23%) |
| Coronary artery disease | 6 (13%) |
| Chronic kidney failure | 5 (11%) |
| Clinical presentations | |
| Sepsis(fever, leukocytosis and bacteremia) | 29 (67%) |
| Abdominal/back pain | 23 (53%) |
| Peri-graft/retroperitoneal abscess | 21 (48%) |
| Graft duodenal fistula | 10 (23%) |
| Acute major bleeding | 8 (18%) |
| Lower-limb ischemia | 5 (11%) |
| Pseudoaneurysms | 3 (6%) |
| Highest CRP level during hospital stay | |
| >100 mg/L | 29 (68%) |
| <100 mg/L | 11 (25%) |
| N/A | 3 (6%) |
| Highest PCT level during hospital stay | |
| >1 ng/mL | 31 (72%) |
| <1 ng/mL | 9 (22%) |
| N/A | 3 (6%) |
| Surgery type | |
| Selective surgery | 32 (75%) |
| Emergency surgery | 11 (25%) |
| Total | 43 |
| Initial Treatment | n | % |
|---|---|---|
| EVAR | 18 | 42 |
| TEVAR | 13 | 30 |
| AAA open repair | 10 | 23 |
| TEVAR + carotid-subclavian bypass | 2 | 5 |
| Total | 43 | 100 |
| Pathogen | n | % |
|---|---|---|
| Gram-Positive bacterium | ||
| Staphylococcus aureus | 15 | 34 |
| MRSA | 4 | 9 |
| Streptococcus | 3 | 6 |
| Enterococcus | 3 | 6 |
| Gram-negative bacterium | ||
| Escherichia coli | 12 | 27 |
| Klebsiella pneumoniae | 9 | 20 |
| Pseudomonas aeruginosa | 5 | 11 |
| Enterobacter cloacae | 3 | 6 |
| Salmonella | 1 | 2 |
| Fungus infection | 2 | 6 |
| Polymicrobial infection | 17 | 39 |
| Negative culture results | 6 | 13 |
| Total | 43 | 100 |
| Variables | Survived | Deceased | p |
|---|---|---|---|
| Demographics | |||
| Male | 23 | 7 | 0.71 |
| Age (Mean ± SD) | 70.78 ± 7.05 | 69.55 ± 10.39 | 0.66 |
| Pre-operative comorbidity | |||
| Hypertension | 22 | 9 | 0.46 |
| Smoking | 19 | 6 | 1.00 |
| Diabetes mellitus | 12 | 5 | 0.73 |
| COPD | 8 | 3 | 1.00 |
| Hypoproteinemia | 6 | 4 | 0.25 |
| Coronary artery disease | 4 | 2 | 0.64 |
| CKD | 3 | 2 | 0.59 |
| Clinical Presentations | |||
| Sepsis | 21 | 8 | 1.00 |
| Abdominal/back pain | 17 | 6 | 1.00 |
| Abscesses | 14 | 7 | 0.31 |
| Graft duodenal fistula | 5 | 5 | 0.09 |
| Acute major bleeding | 5 | 3 | 0.40 |
| Lower limb ischemia | 2 | 3 | 0.10 |
| Pseudoaneurysms | 1 | 2 | 0.15 |
| Highest CRP level | |||
| >100 mg/L | 19 | 10 | 0.23 |
| Highest PCT level | |||
| >1 ng/mL | 20 | 11 | 0.04 |
| Surgery type | |||
| Emergency surgery | 5 | 6 | 0.02 |
| Total | 43 | ||
| Variables | p | 95% CI |
|---|---|---|
| Emergency surgery | 0.03 | 1.25–26.57 |
| Highest PCT level | 0.38 | 0.28–29.56 |
| Highest CRP level | 0.08 | 0.78–60.12 |
| Graft duodenal fistula | 0.21 | 0.56–13.95 |
| Total | 43 |
| Treatment Options | Time (Months) | Proportion Surviving for RI | Cumulative Proportion Surviving at the End of RI Interval | Proportion Surviving for Graft Thrombosis | Cumulative Proportion Surviving at End of Graft Thrombosis Interval |
|---|---|---|---|---|---|
| EAR | 0 | 0.75 | 0.75 | 1.00 | 1.00 |
| 10 | 0.71 | 0.54 | 0.71 | 0.71 | |
| 20 | 1.00 | 0.54 | 0.50 | 0.36 | |
| 30 | 1.00 | 0.54 | 1.00 | 0.36 | |
| 40 | 1.00 | 0.54 | 1.00 | 0.36 | |
| 50 | 1.00 | 0.54 | 1.00 | 0.36 | |
| 60 | 1.00 | 0.54 | 1.00 | 0.36 | |
| 70 | 1.00 | 0.54 | 1.00 | 0.36 | |
| 80 | 1.00 | 0.54 | 1.00 | 0.36 | |
| 90 | 0.00 | 0.00 | 1.00 | 0.36 | |
| ISR | 0 | 0.96 | 0.96 | 0.96 | 0.96 |
| 10 | 1.00 | 0.96 | 0.94 | 0.94 | |
| 20 | 1.00 | 0.96 | 0.93 | 0.84 | |
| 30 | 1.00 | 0.96 | 0.90 | 0.75 | |
| 40 | 1.00 | 0.96 | 1.00 | 0.75 | |
| 50 | 1.00 | 0.96 | 1.00 | 0.75 | |
| 60 | 0.82 | 0.78 | 1.00 | 0.75 | |
| 70 | 1.00 | 0.78 | 1.00 | 0.75 | |
| 80 | 1.00 | 0.78 | 1.00 | 0.75 | |
| 90 | 1.00 | 0.78 | 1.00 | 0.75 | |
| 100 | 1.00 | 0.78 | 1.00 | 0.75 | |
| 110 | 1.00 | 0.78 | 1.00 | 0.75 | |
| Conservative | 0 | 0.45 | 0.45 | NA | NA |
| treatment | 10 | 0.00 | 0.00 | NA | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ge, J.; Weng, C.; Zhao, J.; Yuan, D.; Huang, B.; Wang, T. Management and Clinical Outcome of Aortic Graft Infections: A Single-Center Retrospective Study. J. Clin. Med. 2022, 11, 6588. https://doi.org/10.3390/jcm11216588
Ge J, Weng C, Zhao J, Yuan D, Huang B, Wang T. Management and Clinical Outcome of Aortic Graft Infections: A Single-Center Retrospective Study. Journal of Clinical Medicine. 2022; 11(21):6588. https://doi.org/10.3390/jcm11216588
Chicago/Turabian StyleGe, Jinting, Chengxin Weng, Jichun Zhao, Ding Yuan, Bin Huang, and Tiehao Wang. 2022. "Management and Clinical Outcome of Aortic Graft Infections: A Single-Center Retrospective Study" Journal of Clinical Medicine 11, no. 21: 6588. https://doi.org/10.3390/jcm11216588
APA StyleGe, J., Weng, C., Zhao, J., Yuan, D., Huang, B., & Wang, T. (2022). Management and Clinical Outcome of Aortic Graft Infections: A Single-Center Retrospective Study. Journal of Clinical Medicine, 11(21), 6588. https://doi.org/10.3390/jcm11216588






