The Efficacy of Cervical Lordosis Rehabilitation for Nerve Root Function and Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial with 2-Year Follow-Up
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Inclusion and Exclusion Criteria
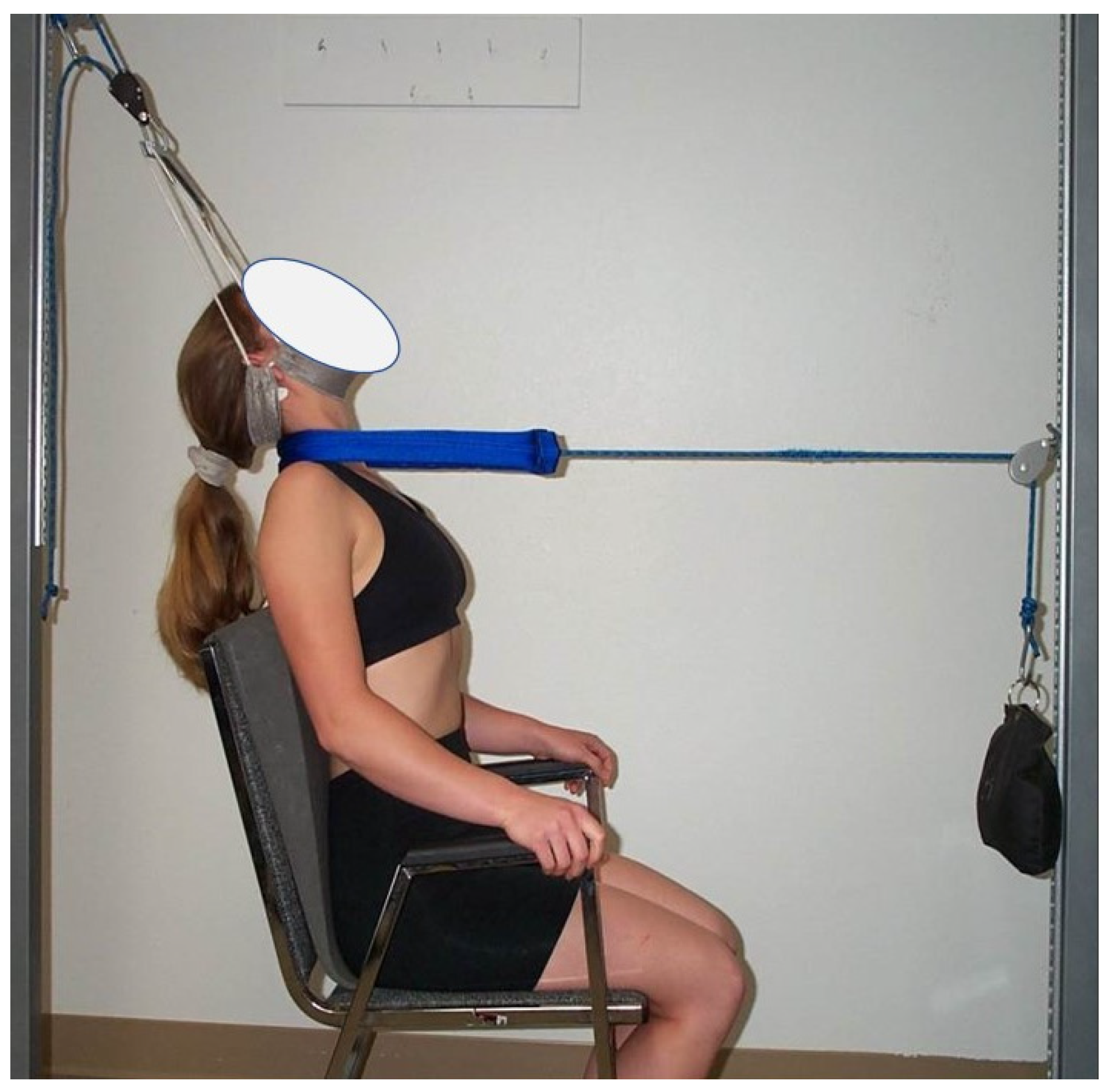
2.3. Treatment Procedures
2.4. Outcome Measures
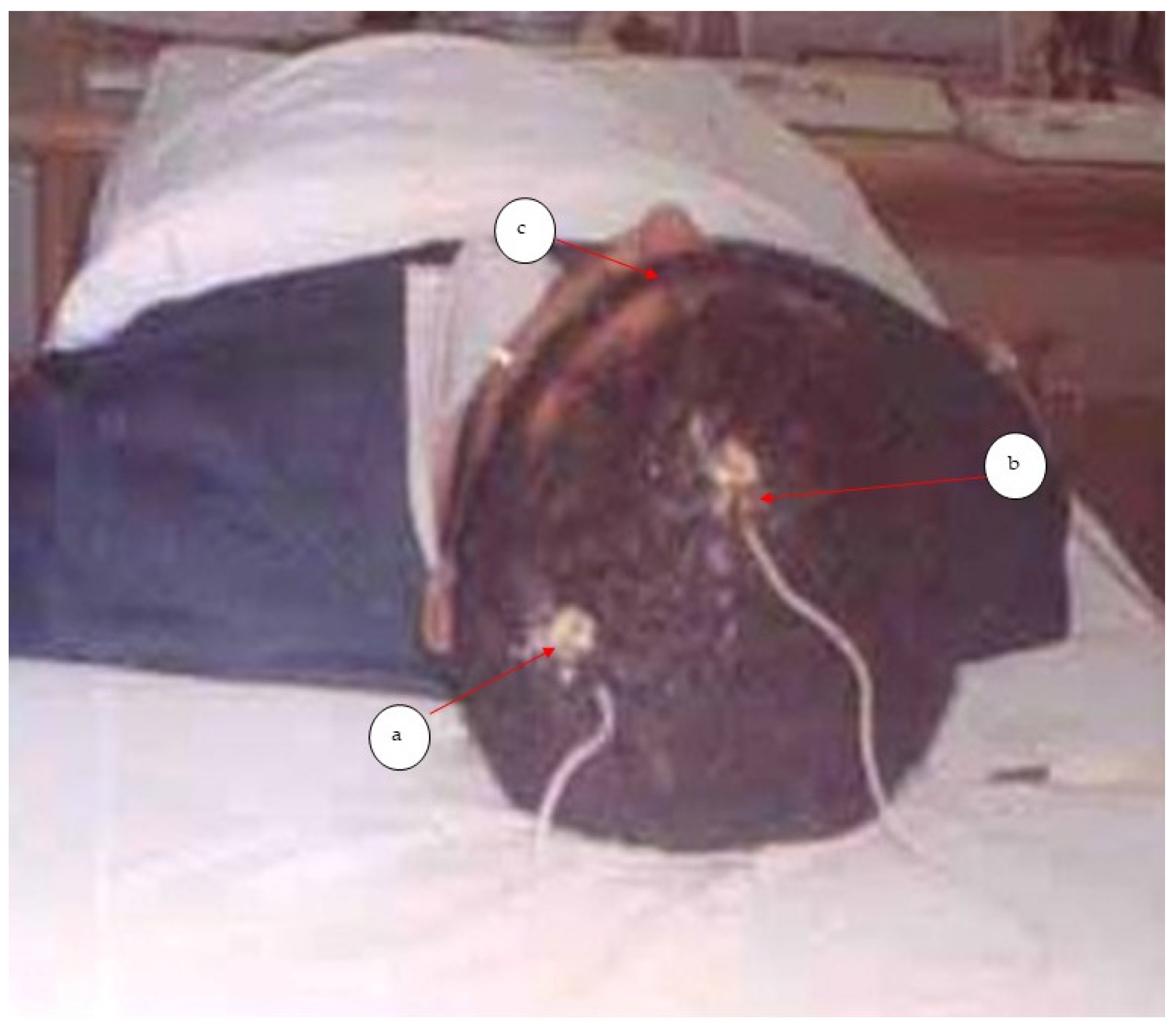
2.5. DSSEPs
2.6. Sample Size Estimation
2.7. Data Analysis
3. Results
3.1. Pain Outcomes
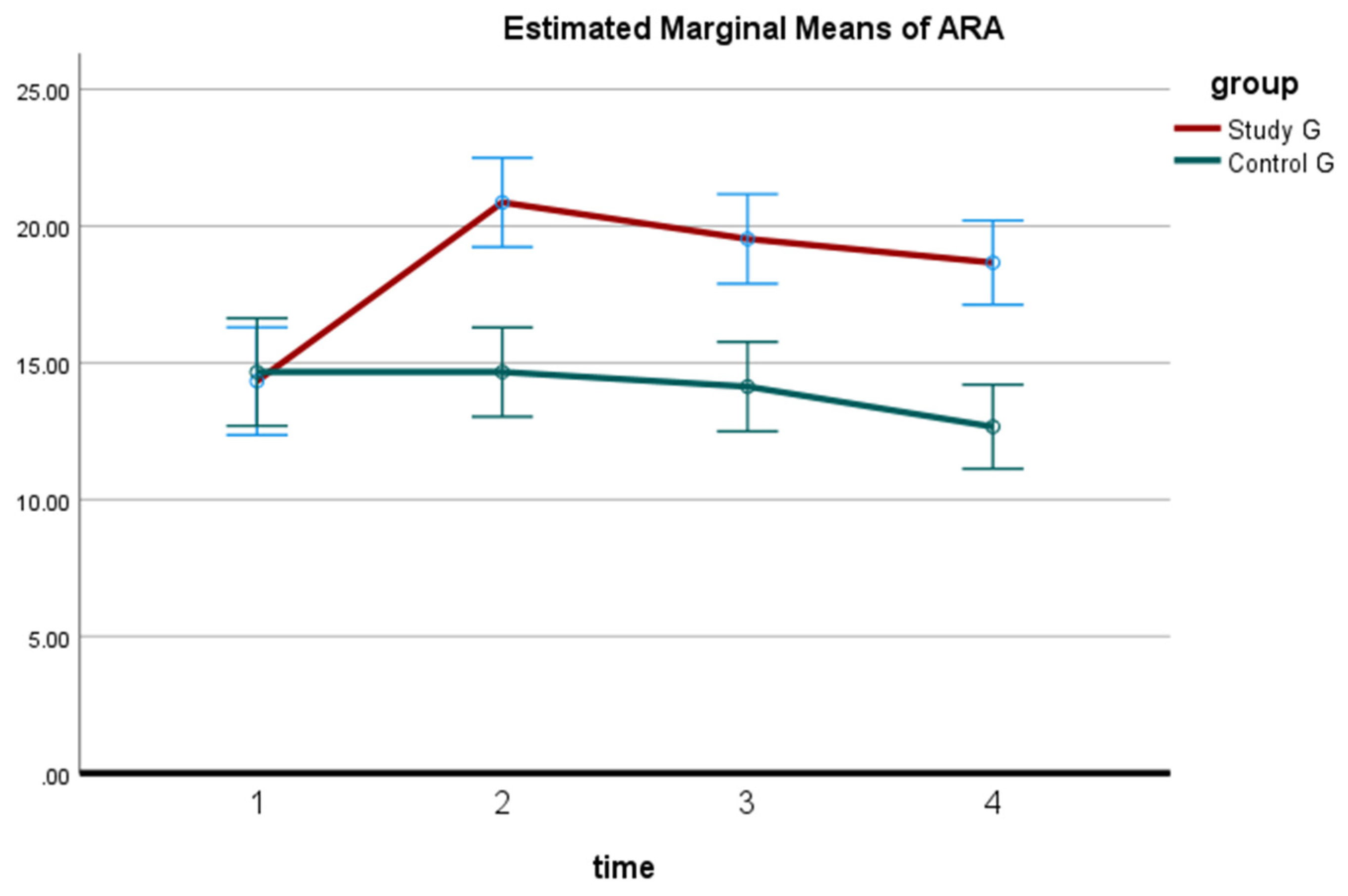
3.2. ARA C2-C7 Cervical Lordosis
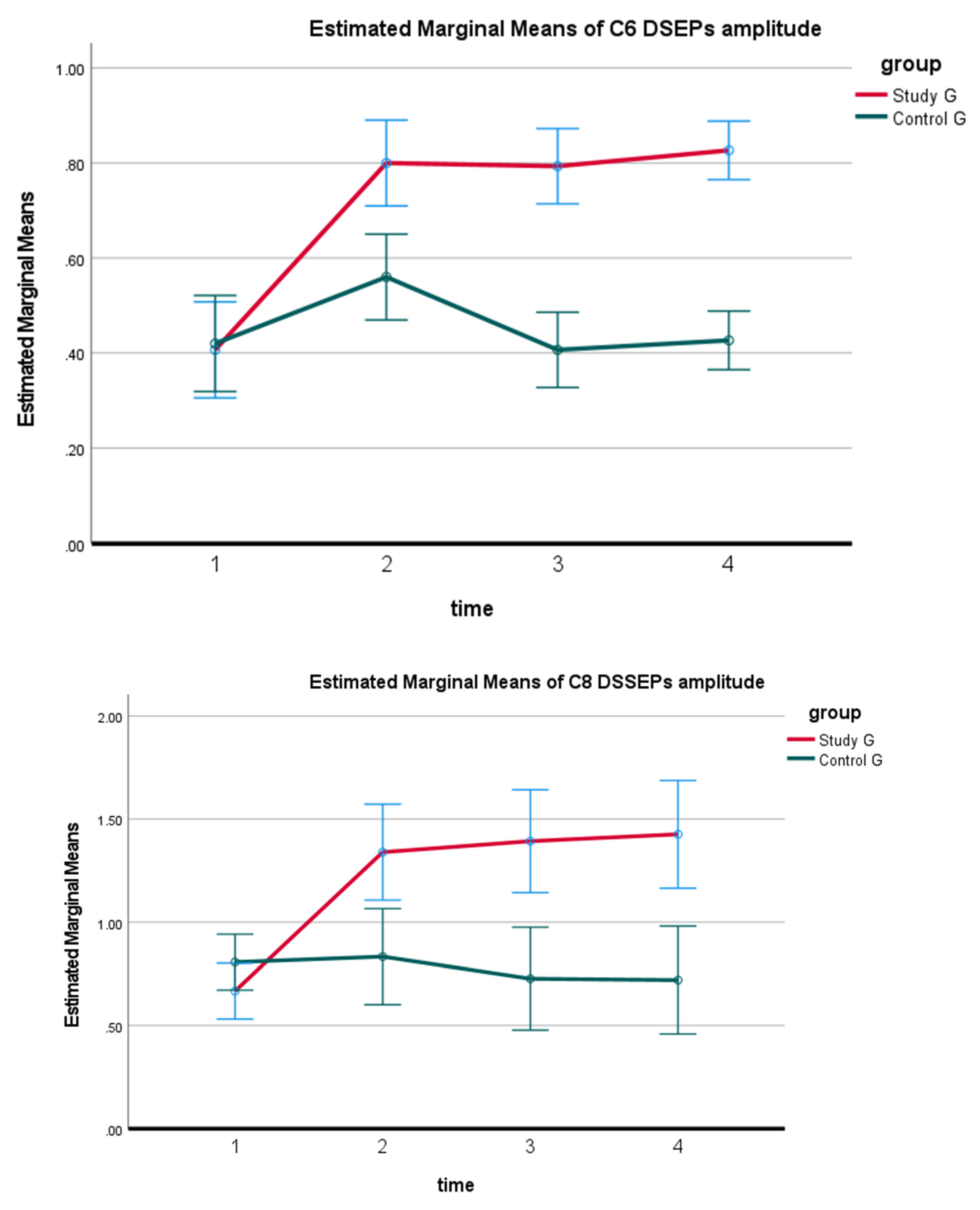
3.3. DSSEPs
3.4. Correlations
3.5. Medication and Alternative Therapy Usage
4. Discussion
4.1. Cervical Lordosis Improvements
4.2. Pain Improvements
4.3. DSSEPs Improvement
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ylinen, J.; Kautiainen, H.; Wirén, K.; Häkkinen, A. A stretching exercises vs manual therapy in treatment of chronic neck pain: A randomized, controlled cross-over trial. J. Rehabil. Med. 2007, 39, 126–132. [Google Scholar] [CrossRef]
- Luyao, H.; Xiaoxiao, Y.; Tianxiao, F.; Yuandong, L.; Wang, P. Management of Cervical Spondylotic Radiculopathy: A Systematic review. Glob. Spine J. 2022, 12, 1912–1924. [Google Scholar] [CrossRef]
- Clark, C.R. Differential diagnosis and non-operative management. In The Adult Spine: Principles and Practice, 2nd ed.; Frrymoyer, J.W., Ed.; Lippicott-Raven: Philadelphia, PA, USA, 1997; Volume 21, pp. 2421–2428. [Google Scholar]
- Alghamdi, A.; Alqahtani, A. Magnetic Resonance Imaging of the Cervical Spine: Frequency of Abnormal Findings with Relation to Age. Medicines 2021, 8, 77. [Google Scholar] [CrossRef]
- Faldini, C.; Pagkrati, S.; Leonetti, D.; Miscione, M.T.; Giannini, S. Sagittal segmental alignment as predictor of adjacent-level degeneration after a cloward procedure. Clin. Orthop. Relat. Res. 2011, 469, 674–681. [Google Scholar] [CrossRef]
- Li, L.; Li, N.; Zhou, J.; Li, H.; Du, X.; He, H.; Rong, P.; Wang, W.; Liu, Y. Effect of cervical alignment change after anterior cervical fusion on radiological adjacent segment pathology. Quant. Imaging Med. Surg. 2022, 12, 2464–2473. [Google Scholar] [CrossRef]
- Harrison, D.E.; Harrison, D.D.; Janik, T.J.; William Jones, E.; Cailliet, R.; Normand, M. Comparison of axial and flexural stresses in lordosis and three buckled configurations of the cervical spine. Clin. Biomech. 2001, 16, 276–284. [Google Scholar] [CrossRef]
- Mallard, F.; Wong, J.J.; Lemeunier, N.; Côté, P. Effectiveness of Multimodal Rehabilitation Interventions for Management of Cervical Radiculopathy in Adults: An Updated Systematic Review from the Ontario Protocol for Traffic Injury Management (Optima) Collaboration. J. Rehabil. Med. 2022, 54, jrm00318. [Google Scholar] [CrossRef]
- Borrella-Andrés, S.; Marqués-García, I.; Lucha-López, M.O.; Fanlo-Mazas, P.; Hernández-Secorún, M.; Pérez-Bellmunt, A.; Tricás-Moreno, J.M.; Hidalgo-García, C. Manual Therapy as a Management of Cervical Radiculopathy: A Systematic Review. Biomed. Res. Int. 2021, 2021, 9936981. [Google Scholar] [CrossRef]
- Kuligowski, T.; Skrzek, A.; Cieślik, B. Manual Therapy in Cervical and Lumbar Radiculopathy: A Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2021, 18, 6176. [Google Scholar] [CrossRef]
- Zhu, L.; Wei, X.; Wang, S. Does cervical spine manipulation reduce pain in people with degenerative cervical radiculopathy? A systematic review of the evidence, and a meta-analysis. Clin. Rehabil. 2016, 30, 145–155. [Google Scholar] [CrossRef]
- Romeo, A.; Vanti, C.; Boldrini, V.; Ruggeri, M.; Guccione, A.A.; Pillastrini, P.; Bertozzi, L. Cervical Radiculopathy: Effectiveness of Adding Traction to Physical Therapy-A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phys. Ther. 2018, 98, 231–242, Erratum in Phys. Ther. 2018, 98, 727. [Google Scholar] [CrossRef] [PubMed]
- Colombo, C.; Salvioli, S.; Gianola, S.; Castellini, G.; Testa, M. Traction Therapy for Cervical Radicular Syndrome is Statistically Significant but not Clinically Relevant for Pain Relief. A Systematic Literature Review with Meta-Analysis and Trial Sequential Analysis. J. Clin. Med. 2020, 9, 3389. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, I.M.; Diab, A.A. Multimodal treatment program comparing 2 different traction approaches for patients with discogenic cervical radiculopathy: A randomized controlled trial. J. Chiropr. Med. 2014, 13, 157–167. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D. Conservative management of cervical spine syndromes. In Dusfuntion in the Cerival Spine; Murphy, D., Ed.; McGraw-Hill: New York, NY, USA, 2000; pp. 71–103. [Google Scholar]
- Moustafa, I.M.; Diab, A.A.; Taha, S.; Harrison, D.E. Addition of a Sagittal Cervical Posture Corrective Orthotic Device to a Multimodal Rehabilitation Program Improves Short- and Long-Term Outcomes in Patients with Discogenic Cervical Radiculopathy. Arch. Phys. Med. Rehabil. 2016, 97, 2034–2044. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Cailliet, R.; Harrison, D.D.; Troyanovich, S.J.; Harrison, S.O. A Review of Biomechanics of the Central Nervous System. PART II: Strains in the Spinal Cord from Postural Loads. J. Manip. Physiol. Ther. 1999, 22, 322–332. [Google Scholar] [CrossRef]
- Breig, A. Adverse Mechanical Tension in the Central Nervous System: An Analysis of Cause and Effect: Relief by Functional Neurosurgery; Almqvist and Wiksell International: Stockholm, Sweden, 1978; p. 130. [Google Scholar]
- Lin, T.; Wang, Z.; Chen, G.; Liu, W. Predictive Effect of Cervical Sagittal Parameters on Conservative Treatment of Single-Segment Cervical Spondylotic Radiculopathy. World Neurosurg. 2020, 134, e1028–e1036. [Google Scholar] [CrossRef]
- Ames, C.P.; Blondel, B.; Scheer, J.K.; Schwab, F.J.; Le Huec, J.C.; Massicotte, E.M.; Patel, A.A.; Traynelis, V.C.; Kim, H.J.; Shaffrey, C.I.; et al. Cervical radiographical alignment: Comprehensive assessment techniques and potential importance in cervical myelopathy. Spine 2013, 38, S149–S160. [Google Scholar] [CrossRef]
- Scheer, J.K.; Tang, J.A.; Smith, J.S.; Acosta, F.L., Jr.; Protopsaltis, T.S.; Blondel, B.; Bess, S.; Shaffrey, C.I.; Deviren, V.; Lafage, V.; et al. Cervical spine alignment, sagittal deformity, and clinical implications: A review. J. Neurosurg. Spine 2013, 19, 141–159. [Google Scholar] [CrossRef]
- Lin, B.J.; Hong, K.T.; Lin, C.; Chung, T.T.; Tang, C.T.; Hueng, D.Y.; Hsia, C.C.; Ju, D.T.; Ma, H.I.; Liu, M.Y.; et al. Impact of global spine balance and cervical regional alignment on determination of postoperative cerviacl alignment after laminoplasty. Medicine 2018, 97, e13111. [Google Scholar] [CrossRef]
- Pope, M. Case studies. In Chiropractic the Physics of Spinal Correection; Harrison, D.D., Ed.; National Library of Medicine: Bethesda, MA, USA, 1988; Volume 92, pp. 12–85. [Google Scholar]
- Harrison, D.E.; Cailliet, R.; Harrison, D.D.; Janik, T.J.; Holland, B.A. New 3-point bending traction method for restoring cervical lordosis and cervical manipulation: A non-randomized clinical controlled trial. Arch. Phys. Med. Rehabil. 2002, 83, 447–453. [Google Scholar] [CrossRef]
- Oakley, P.A.; Ehsani, N.N.; Moustafa, I.M.; Harrison, D.E. Restoring cervical lordosis by cervical extension traction methods in the treatment of cervical spine disorders: A systematic review of controlled trials. J. Phys. Ther. Sci. 2021, 33, 784–794. [Google Scholar] [CrossRef] [PubMed]
- Naguszewski, W.K.; Naguszewski, R.K.; Gose, E.E. Dermatomal somatosensory evoked potential demonstration of nerve root decompression after VAX-D therapy. Neurol. Res. 2001, 23, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Pope, P.H.M.; Oepkes, C.T.; Notermans, S.L.H.; Vlek, N.M.T.; Stegeman, D.F. Dermatomal somatosensory evoked potentials of the lumbar and cervical roots. Method and normal values. Eur. Arch. Psychiatry Clin. Neurosci. 1988, 238, 22–27. [Google Scholar]
- McAviney, J.; Schulz, D.; Bock, R.; Harrison, D.E.; Holland, B. Determining the Relationship between Cervical Lordosis and Neck Complaints. J. Manip. Physiol Ther. 2005, 28, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.D.; Harrison, D.E.; Janik, T.J.; Cailliet, R.; Haas, J.W.; Ferrantelli, J.; Holland, B. Modeling of the Sagittal Cervical Spine as a Method to Discriminate Hypo-Lordosis: Results of Elliptical and Circular Modeling in 72 Asymptomatic Subjects, 52 Acute Neck Pain Subjects, and 70 Chronic Neck Pain Subjects. Spine 2004, 29, 2485–2492. [Google Scholar] [CrossRef]
- Mansoori, S.S.; Moustafa, I.M.; Ahbouch, A.; Harrison, D.E. Optimal duration of stretching exercise in patients with chronic myofascial pain syndrome: A randomized controlled trial. J. Rehabil. Med. 2021, 53, jrm00142. [Google Scholar] [CrossRef]
- Kisner, C.; Colby, L.A. Therapeutic exercise foundations and techniques. In The Spine: Exercise and Manipulation Interventions, Kisner, C., Thorp, J.N., Eds.; 6th ed.; FA Davis: Philadelphia, PA, USA, 2012; pp. 485–538. [Google Scholar]
- Liguori, R.; Taher, G.; Trojaborg, W. Somatosensory evoked potentials from cervical and lumbosacral dermatomes. Acta Neurol. Scand. 1991, 84, 161–166. [Google Scholar] [CrossRef]
- Harrison, D.E.; Harrison, D.D.; Cailliet, R.; Troyanovich, S.J.; Janik, T.J.; Holland, B. Cobb Method or Harrison Posterior Tangent Method: Which is Better for Lateral Cervical Analysis? Spine 2000, 25, 2072–2078. [Google Scholar] [CrossRef]
- Chuds, J.D.; Piva, S.R.; Fritz, J.M. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 2005, 30, 1331–1334. [Google Scholar]
- Helliwell, P.S.; Evans, P.F.; Wright, V. The straight cervical spine: Does it indicate muscle spasm? J. Bone Jt. Surg. Br. 1994, 76, 103–106. [Google Scholar] [CrossRef]
- Fedorchuk, C.A.; McCoy, M.; Lightstone, D.F.; Bak, D.A.; Moser, J.; Kubricht, B.; Packer, J.; Walton, D.; Binongo, J. Impact of Isometric Contraction of Anterior Cervical Muscles on Cervical Lordosis. J. Radiol. Case Rep. 2016, 10, 13–25. [Google Scholar] [CrossRef] [PubMed]
- Levoska, S.; Keinänen-Kiukaanniemi, S. Active or passive physiotherapy for occupational cervicobrachial disorders? A comparison of two treatment methods with a 1-year follow-up. Arch. Phys. Med. Rehabil. 1993, 74, 425–430. [Google Scholar] [PubMed]
- Rulleau, T.; Abeille, S.; Pastor, L.; Planche, L.; Allary, P.; Chapeleau, C.; Moreau, C.; Cormier, G.; Caulier, M. Effect of an intensive cervical traction protocol on mid-term disability and pain in patients with cervical radiculopathy: An exploratory, prospective, observational pilot study. PLoS ONE 2021, 16, e0255998. [Google Scholar] [CrossRef]
- Grob, D.; Frauenfelder, H.; Mannion, A.F. The association between cervical spine curvature and neck pain. Eur. Spine J. 2007, 16, 669–678. [Google Scholar] [CrossRef]
- Wainner, R.S.; Gill, H. Diagnosis and nonoperative management of cervical radiculopathy. J. Orthop. Sports Phys. Ther. 2000, 30, 728–744. [Google Scholar] [CrossRef]
- Schnebel, B.E.; Watkins, R.G.; Dillin, W. The role of spinal flexion and extension in changing nerve root compression in disc herniations. Spine 1989, 14, 835–837. [Google Scholar] [CrossRef]
- Abdulwahab, S.S.; Sabbahi, M. Neck retractions, cervical root decompression, and radicular pain. J. Orthop. Sports Phys. Ther. 2000, 30, 4–12. [Google Scholar]
- Albert, T.J.; Smith, A.; Bresseler, E. An vivo analysis of dimentional changes of the neuro-foramen after anterior cervical discectomy and fusion: A radiologic investigation. J. Spinal Disord. 1997, 10, 229–233. [Google Scholar] [CrossRef]
- Brian, K.; David, H.K.; Andrea, M.; Louis, G.J. Outcomes Following Anterior Cervical Discectomy and Fusion: The Role of Interbody Disc Height, Angulation, and Spinous Process Distance. J. Spinal Disord. Tech. 2005, 18, 304–308. [Google Scholar]
- Wang, X.; Liu, Y.; Zhang, H.; Jin, J.; Ma, Y.; Leng, Y. Sinomenine alleviates dorsal root ganglia inflammation to inhibit neuropathic pain via the p38 MAPK/CREB signalling pathway. Eur. J. Pharmacol. 2021, 897, 173945. [Google Scholar] [CrossRef]





| Study Group (n = 15) | Control Group (n = 15) | p ‡ | |
|---|---|---|---|
| Age (years) | 46.3 ± 2.05 | 45.9 ± 2.1 | 0.5 |
| Weight (kg) | 73.3 ± 8.9 | 77.5 ± 9 | 0.2 |
| Height (cm) | 171.6 ± 5 | 168.3 ± 7.9 | 0.18 |
| Male | 6 | 5 | 0.7 |
| Female | 9 | 10 | |
| Smoker | 5 | 4 | 0.69 |
| Non smoker | 10 | 11 |
| Measures | Pretreatment | At 10 Weeks | At 3 Months | At 2 Years | p | Post Hoc Test (MD) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| G | T | G × T | ||||||||
| ARA | S | 14.3 ± 4.1 | 20.87 ± 3 | 19.5 ± 3.2 | 18.8 ± 2.1 | <0.001 | <0.001 | <0.001 | 1 vs. 2 | −3.26 * |
| C | 14.6 ± 3.5 | 14.7± 3.3 | 14.1 ± 3.1 | 12.3 ± 2.7 | 1 vs. 3 | −2.33 * | ||||
| 0.8 [−3.1–2.5] | <0.001 [3.8–8.5] | <0.001 [3.02–7.7] | <0.001 [3.7–8.2] | 1 vs. 4 | −1.16 * | |||||
| Pain | S | 5.26 ± 0.96 | 3.2 ± 1.26 | 2.8 ± 1.27 | 1.71 ± 1.2 | <0.001 | <0.001 | <0.001 | 1 vs. 2 | 1.7 * |
| C | 5.47 ± 1.18 | 3.9 ± 1.43 | 4.6 ± 1.49 | 4.3 ± 1.2 | 1 vs. 3 | 1.5 * | ||||
| 0.7 [−0.8–0.9] | <0.001 [−1.7–0.29] | <0.001 [−2.9–−0.79] | <0.001 [−3.5–−1.8] | 1 vs. 4 | 2.3 * | |||||
| Measures | Pretreatment | At 10 Weeks | At 3 Months | At 2 Years | p | Post Hoc Test (MD) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| G | T | G × T | ||||||||
| C6 | S | 0.41 ± 0.1 | 0.80 ± 0.19 | 0.79 ± 0.11 | 0.82 ± 0.14 | <0.001 | <0.001 | <0.001 | 1 vs. 2 | −0.267 * |
| C | 0.42 ± 0.2 | 0.56 ± 0.15 | 0.40 ± 0.15 | 0.42 ± 0.17 | 1 vs. 3 | −0.18 * | ||||
| 0.8 [−0.16–0.13] | <0.001 [0.11–0.37] | <0.001 [0.272–0.5] | <0.001 [0.31–0.48] | 1 vs. 4 | −0.21 * | |||||
| C7 | S | 0.4 ± 0.1 | 1.18 ± 0.33 | 1.0 ± 0.37 | 1.1 ± 0.37 | <0.001 | <0.001 | <0.001 | 1 vs. 2 | −0.38 * |
| C | 0.69 ± 0.2 | 0.7 ± 0.18 | 0.52 ± 0.21 | 0.51 ± 0.18 | 1 vs. 3 | −0.24 * | ||||
| 0.05 [−0.26–0.02] | <0.001 [0.32–0.72] | <0.001 [0.30–0.76] | <0.001 [0.36–0.81] | 1 vs. 4 | −0.26 * | |||||
| C8 | S | 0.6 ± 0.2 | 1.3 ± 0.5 | 1.4 ± 0.6 | 1.5 ± 0.6 | <0.001 | <0.001 | <0.001 | 1 vs. 2 | −0.35 * |
| C | 0.8 ± 0.2 | 0.9 ± 0.3 | 0.7 ± 0.3 | 0.7 ± 0.2 | 1 vs. 3 | −0.32 * | ||||
| 0.15 [−0.33–0.05] | 0.005 [0.17–0.84] | <0.001 [0.30–1.1] | <0.001 [0.32–1.08] | 1 vs. 4 | −0.33 * | |||||
| Number of XY Pairs | r | p | |
|---|---|---|---|
| ARA & DSSEP (C6) (baseline data) | 30 | 0.65 | <0.001 * |
| ARA & DSSEP (C7) (baseline data) | 30 | 0.57 | <0.001 * |
| ARA & DSSEP (C8) (baseline data) | 30 | 0.8 | <0.001 * |
| Post-manipulating data (C6) study control | 15 | 0.55 | 0.033 * |
| 15 | 0.19 | 0.49 | |
| Post-manipulating data (C7) study control | 15 | 0.74 | <0.001 * |
| 15 | 0.62 | <0.001 * | |
| Post-manipulating data (C8) study control | 15 | 0.8 | <0.001 * |
| 15 | 0.58 | <0.001 * | |
| ARA C2–C7 and pain Baseline data | 30 | −0.49 | 0.005 * |
| Post-treatment data Study group | 15 | −0.6 | 0.01 * |
| Control group | 15 | −0.17 | 0.05 * |
| Medication Utilization & Therapy Used |
|---|
| Control Group |
| • NSAIDs |
| • Tricyclic antidepressants |
| • NSAIDs, hydrotherapy |
| • NSAIDS, Acupuncture |
| • Tricyclic antidepressants, semi-hard cervical collar |
| • Tricyclic antidepressants, semi-hard cervical collar |
| • Tricyclic antidepressants, soft tissue massage |
| • Opioid medications |
| • NSAIDS, Ultrasound therapy |
| Study Group |
| • NSAIDs |
| • Cervical spine epidural steroids |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moustafa, I.M.; Diab, A.A.; Harrison, D.E. The Efficacy of Cervical Lordosis Rehabilitation for Nerve Root Function and Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial with 2-Year Follow-Up. J. Clin. Med. 2022, 11, 6515. https://doi.org/10.3390/jcm11216515
Moustafa IM, Diab AA, Harrison DE. The Efficacy of Cervical Lordosis Rehabilitation for Nerve Root Function and Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial with 2-Year Follow-Up. Journal of Clinical Medicine. 2022; 11(21):6515. https://doi.org/10.3390/jcm11216515
Chicago/Turabian StyleMoustafa, Ibrahim M., Aliaa A. Diab, and Deed E. Harrison. 2022. "The Efficacy of Cervical Lordosis Rehabilitation for Nerve Root Function and Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial with 2-Year Follow-Up" Journal of Clinical Medicine 11, no. 21: 6515. https://doi.org/10.3390/jcm11216515
APA StyleMoustafa, I. M., Diab, A. A., & Harrison, D. E. (2022). The Efficacy of Cervical Lordosis Rehabilitation for Nerve Root Function and Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial with 2-Year Follow-Up. Journal of Clinical Medicine, 11(21), 6515. https://doi.org/10.3390/jcm11216515








