Randomized Feasibility Pilot Trial of Adding a New Three-Dimensional Adjustable Posture-Corrective Orthotic to a Multi-Modal Program for the Treatment of Nonspecific Neck Pain
Abstract
1. Introduction
2. Methods
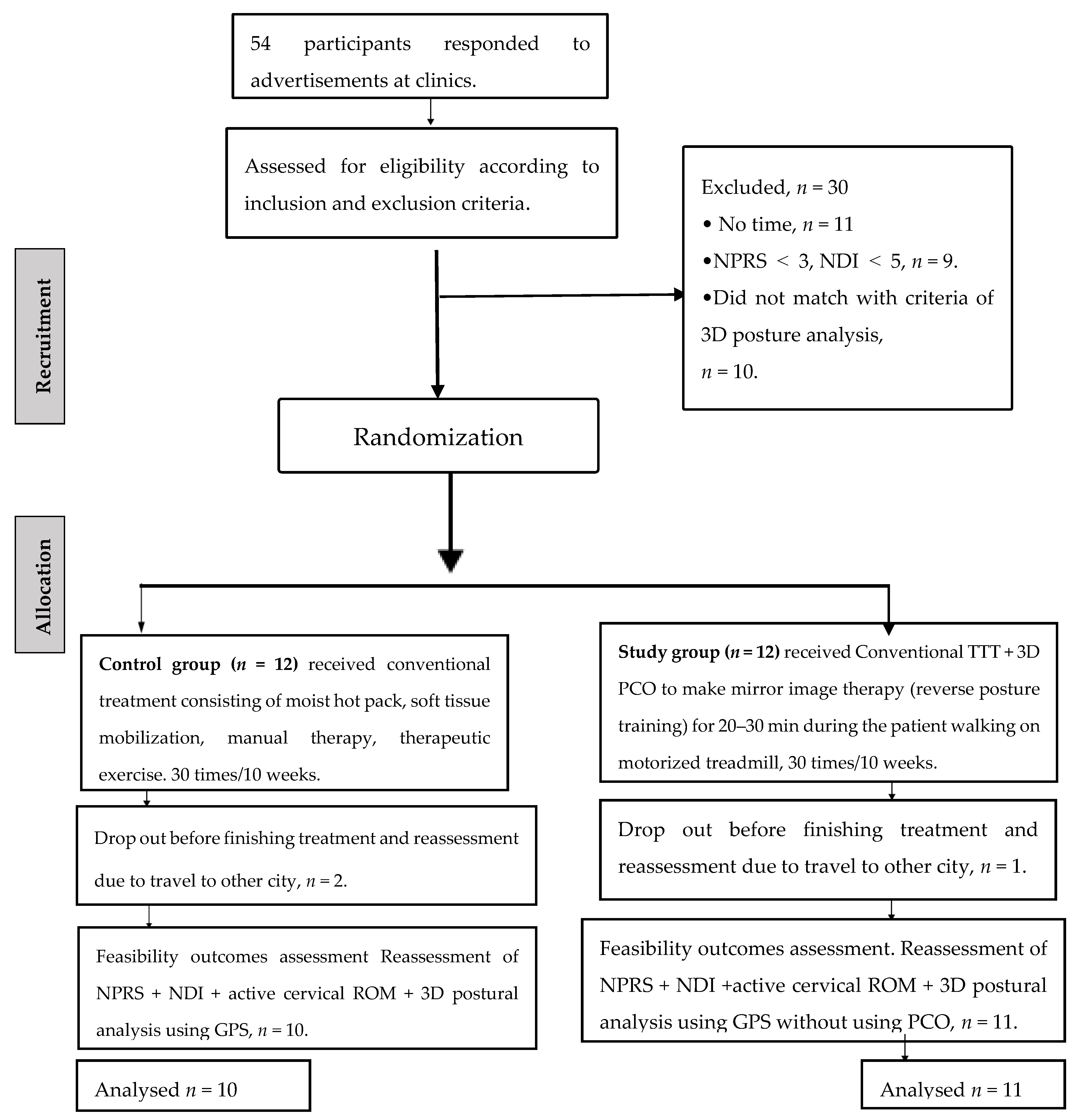
2.1. Study Design
2.2. Procedures
2.3. Participants
2.3.1. Inclusion Criteria
2.3.2. Posture Translations Displacements Included the Following
2.3.3. Posture Rotations Displacements Included the Following
2.3.4. Exclusion Criteria
2.4. Examination Procedures
2.4.1. Primary Outcomes
2.4.2. Secondary Outcomes
- (1)
- Numeric pain rating scale (NPRS)
- (2)
- Neck disability index (NDI)
- (3)
- Active cervical range of motion (CROM)
- (4)
- Three-dimensional posture parameters of the head in relation to the thoracic region
2.4.3. Assessment Procedures
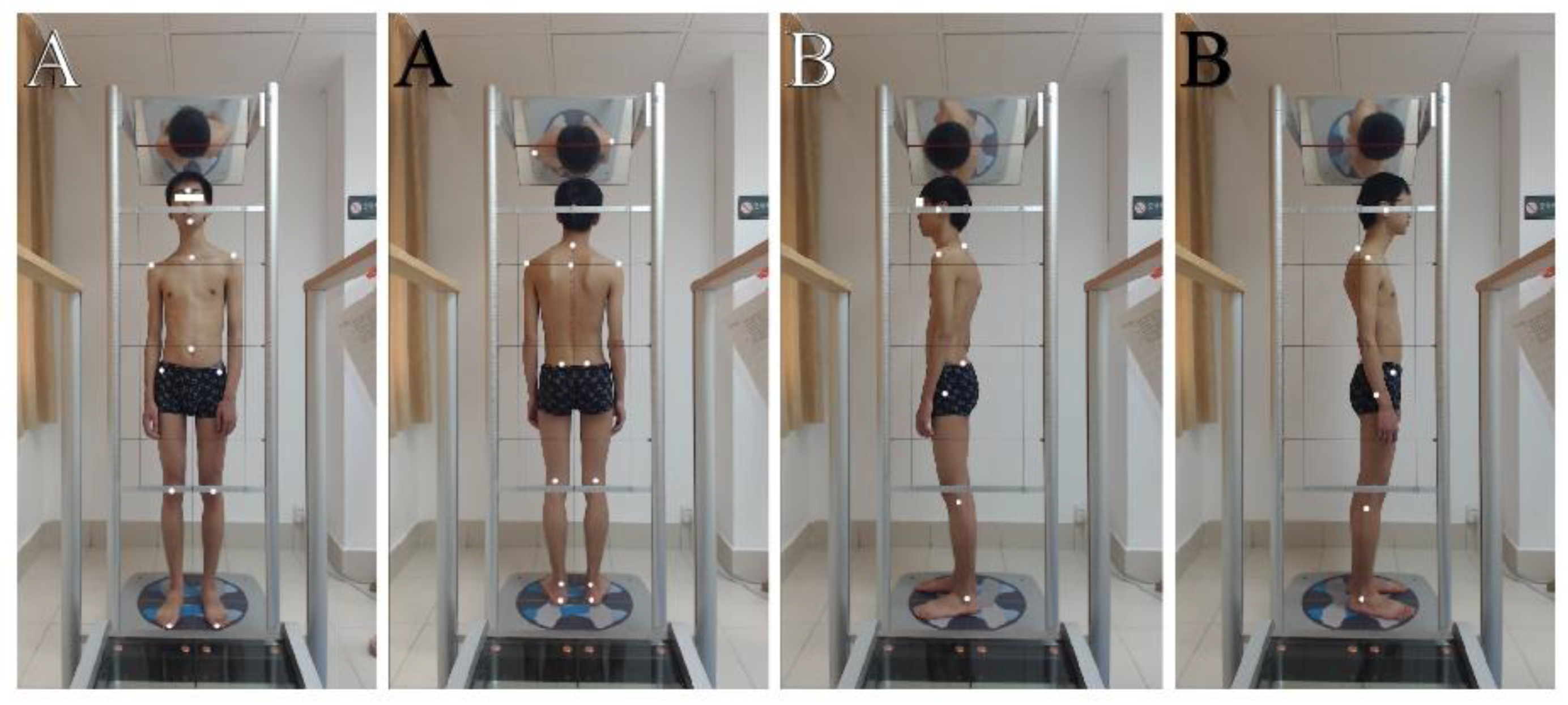
- A.
- Preparation of patients:
- B.
- Marker placement:
- C.
- Starting position of the patients:
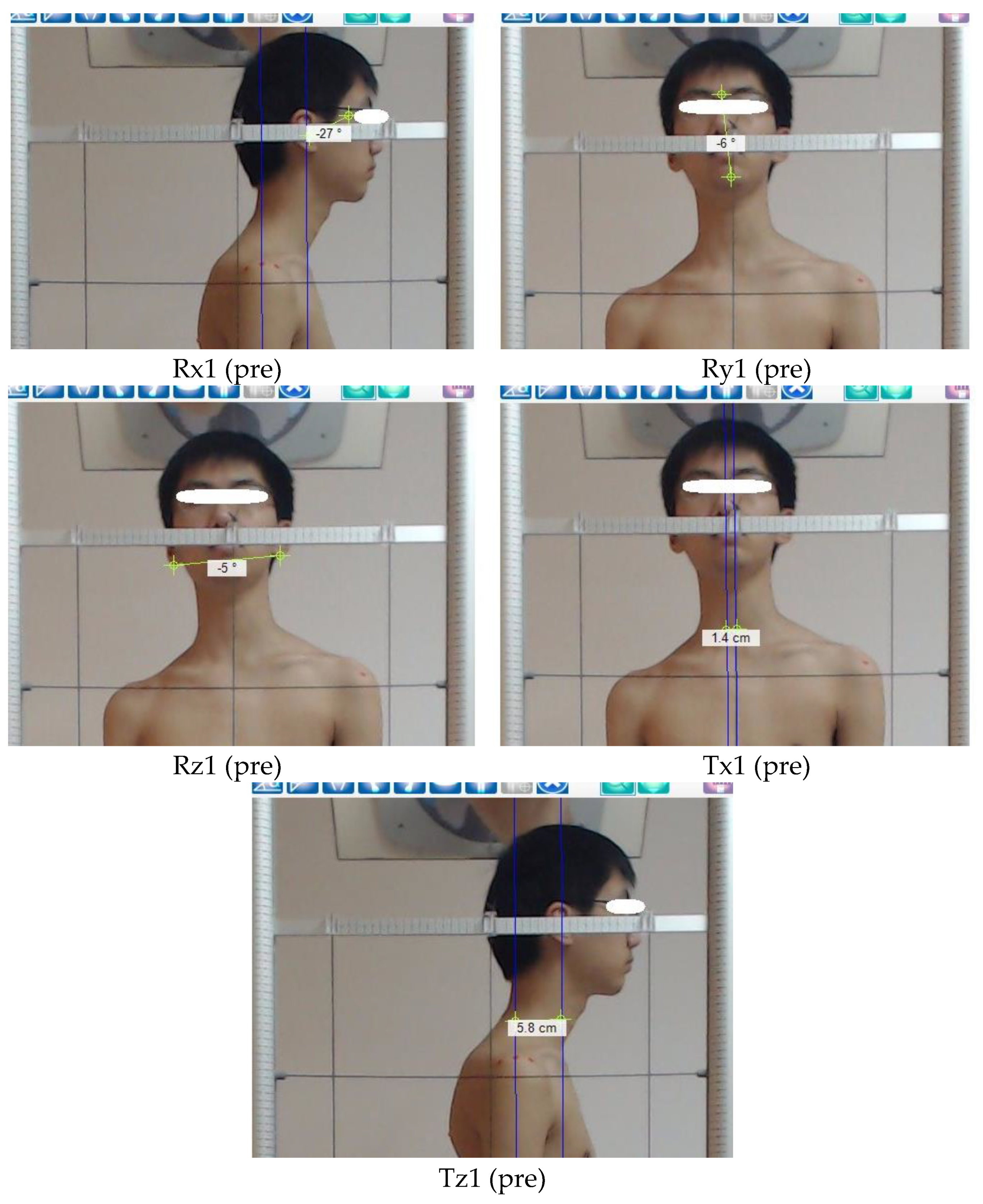
2.4.4. Measured Items (the Postural Parameters) of the Head Region in Relation to the Thoracic Region
2.4.5. Postural Translations of the Head in Relation to the Thoracic Region
2.4.6. Postural Rotations of the Head in Relation to the Thoracic Region
2.5. Interventions
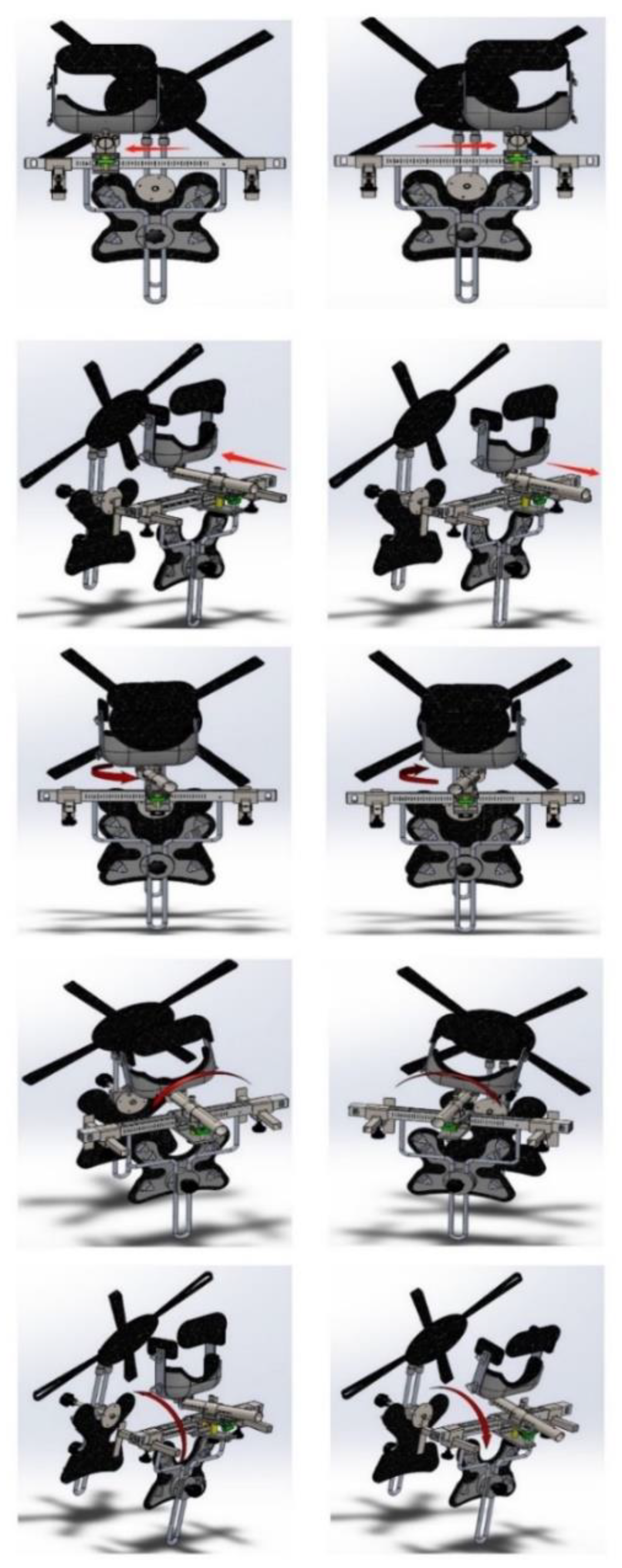
Study Group 3D PCO Performed the Mirror Image® Therapy (Reverse Posture Training) While the Patient Was Walking on Motorized Treadmill
2.6. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Trial Registration
Abbreviations
References
- Hay, S.I.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; Aboyans, V.; et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1260–1344. [Google Scholar] [CrossRef]
- Salomon, J.A.; Haagsma, J.A.; Davis, A.; de Noordhout, C.M.; Polinder, S.; Havelaar, A.H.; Cassini, A.; Devleesschauwer, B.; Kretzschmar, M.; Speybroeck, N.; et al. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob. Health 2015, 3, e712–e723. [Google Scholar] [CrossRef]
- Childs, J.D.; Cleland, J.A.; Elliott, J.M.; Teyhen, D.S.; Wainner, R.S.; Whitman, J.M.; Sopky, B.J.; Godges, J.J.; Flynn, T.W. Neck pain: Clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the american physical therapy association. J. Orthop. Sports Phys. Ther. 2008, 38, A1–A34. [Google Scholar] [CrossRef] [PubMed]
- Bernal-Utrera, C.; Gonzalez-Gerez, J.J.; Anarte-Lazo, E.; Rodriguez-Blanco, C. Manual therapy versus therapeutic exercise in non-specific chronic neck pain: A randomized controlled trial. Trials 2020, 21, 682. [Google Scholar] [CrossRef]
- Peolsson, A.; Marstein, E.; McNamara, T.; Nolan, D.; Sjaaberg, E.; Peolsson, M.; Jull, G.; O’Leary, S. Does posture of the cervical spine influence dorsal neck muscle activity when lifting? Man. Ther. 2014, 19, 32–36. [Google Scholar] [CrossRef]
- Quek, J.; Pua, Y.H.; Clark, R.A.; Bryant, A.L. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man. Ther. 2013, 18, 65–71. [Google Scholar] [CrossRef]
- Park, S.Y.; Yoo, W.G. Effect of sustained typing work on changes in scapular position, pressure pain sensitivity and upper trapezius activity. J. Occup. Health 2013, 55, 167–172. [Google Scholar] [CrossRef]
- Park, J.-H.; Kang, S.-Y.; Lee, S.-G.; Jeon, H.-S. The effects of smart phone gaming duration on muscle activation and spinal posture: Pilot study. Physiother. Theory Pract. 2017, 33, 661–669. [Google Scholar] [CrossRef]
- Szczygieł, E.; Fudacz, N.; Golec, J.; Golec, E. The impact of the position of the head on the functioning of the human body: A systematic review. Int. J. Occup. Med. Environ. Health 2020, 33, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.G.; Punt, T.D.; Sharples, P.; Vilas-Boas, J.P.; Johnson, M.I. Head posture assessment for patients with neck pain: Is it useful? Int. J. Ther. Rehabil. 2009, 16, 43–53. [Google Scholar] [CrossRef]
- Edmondston, S.J.; Chan, H.Y.; Chi Wing Ngai, G.; Warren, M.L.R.; Williams, J.M.; Glennon, S.; Netto, K. Postural neck pain: An investigation of habitual sitting posture, perception of “good” posture and cervicothoracic kinaesthesia. Man. Ther. 2007, 12, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Szeto, G.P.Y.; Straker, L.M.; O’Sullivan, P.B. A comparison of symptomatic and asymptomatic office workers performing monotonous keyboard work-2: Neck and shoulder kinematics. Man. Ther. 2005, 10, 281–291. [Google Scholar] [CrossRef]
- Straker, L.; Smith, A.; Campbell, A.; O’Sullivan, P. Are neck pain and posture related? Phys. Ther. Rev. 2010, 15, 115–116. [Google Scholar] [CrossRef]
- Harrison, D.D.; Janik, T.J.; Harrison, G.R.; Troyanovich, S.; Harrison, D.E.; Harrison, S.O. Chiropractic biophysics technique: A linear algebra approach to posture in chiropractic. J. Manip. Physiol. Ther. 1996, 19, 525–535. [Google Scholar]
- Harrison, D.D. Abnormal postural permutations calculated as rotations and translations from an ideal normal upright static spine. In Chiropractic Family Practice; Sweere, J., Ed.; Aspen Publishers: Gaitherburg, MD, USA, 1992. [Google Scholar]
- Harrison, D.E.; Cailliet, R.; Betz, J.; Haas, J.W.; Harrison, D.D.; Janik, T.J.; Holland, B. Conservative methods for reducing lateral translation postures of the head: A nonrandomized clinical control trial. J. Rehabil. Res. Dev. 2004, 41, 631–639. [Google Scholar] [CrossRef]
- Diab, A.A.; Moustafa, I.M. New Bracing Concept in the Treatment of Chronic Mechanical Low Back Pain: A Randomized Trial. Bull. Fac. Phys. Ther. 2009, 14, 63–74. [Google Scholar]
- Kovacs, F.M.; Abraira, V.; Royuela, A.; Corcoll, J.; Alegre, L.; Tomás, M.; Mir, M.A.; Cano, A.; Muriel, A.; Zamora, J.; et al. Minimum detectable and minimal clinically important changes for pain in patients with nonspecific neck pain. BMC Musculoskelet. Disord. 2008, 9, 43. [Google Scholar] [CrossRef] [PubMed]
- Beltran-Alacreu, H.; López-de-Uralde-Villanueva, I.; Fernández-Carnero, J.; La Touche, R. Manual therapy, therapeutic patient education, and therapeutic exercise, an effective multimodal treatment of nonspecific chronic neck pain: A randomized controlled trial. Am. J. Phys. Med. Rehabil. 2015, 94, 887–897. [Google Scholar] [CrossRef]
- MacDermid, J.C.; Walton, D.M.; Avery, S.; Blanchard, A.; Etruw, E.; McAlpine, C.; Goldsmith, C.H. Measurement Properties of the Neck Disability Index: A Systematic Review. J. Orthop. Sport. Phys. Ther. 2009, 39, 400–417. [Google Scholar] [CrossRef]
- Lee, H.S.; Chung, H.K.; Park, S.W. Correlation between trunk posture and neck reposition sense among subjects with forward head neck postures. Biomed Res. Int. 2015, 2015, 689610. [Google Scholar] [CrossRef][Green Version]
- Yeom, H.; Lim, J.; Yoo, S.H.; Lee, W. A new posture-correcting system using a vector angle model for preventing forward head posture. Biotechnol. Biotechnol. Equip. 2014, 28, S6–S13. [Google Scholar] [CrossRef]
- Normand, M.C.; Descarreaux, M.; Harrison, D.D.; Harrison, D.E.; Perron, D.L.; Ferrantelli, J.R.; Janik, T.J. Three dimensional evaluation of posture in standing with the PosturePrint: An intra- and inter-examiner reliability study. Chiropr. Osteopat. 2007, 15, 15. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Katz, R.S.; Mease, P.; Yunus, M.B. The American College of Rheumatology Preliminary Diagnostic Criteria for Fibromyalgia and Measurement of Symptom Severity. Arthritis Care Res. 2010, 62, 600–610. [Google Scholar] [CrossRef]
- Silva, A.G.; Punt, T.D.; Sharples, P.; Vilas-Boas, J.P.; Johnson, M.I. Head Posture and Neck Pain of Chronic Nontraumatic Origin: A Comparison Between Patients and Pain-Free Persons. Arch. Phys. Med. Rehabil. 2009, 90, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Solow, B.; Ovesen, J.; Nielsen, P.W.; Wildschiødtz, G.; Tallgren, A. Head posture in obstructive sleep apnoea. Eur. J. Orthod. 1993, 15, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Fruhmann Berger, M.; Proß, R.; Ilg, U.; Karnath, H.-O. Deviation of eyes and head in acute cerebral stroke. BMC Neurol. 2006, 6, 23. [Google Scholar] [CrossRef]
- Scientifique, B.B.-K. Undefined Posture Normale et Postures Pathologiques. 2004. Available online: ciesitaliaposturology.it (accessed on 1 September 2022).
- Magee, D. Orthopedic Physical Assessment; Saunders: Philadelphia, PA, USA, 2007; 1152p. [Google Scholar]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How We Design Feasibility Studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, G.A.; Dodd, S.; Williamson, P.R. Design and analysis of pilot studies: Recommendations for good practice. J. Eval. Clin. Pract. 2004, 10, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Julious, S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Young, I.A.; Dunning, J.; Butts, R.; Mourad, F.; Cleland, J.A. Reliability, construct validity, and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptoms. Physiother. Theory Pract. 2019, 35, 1328–1335. [Google Scholar] [CrossRef]
- Wu, S.; Ma, C.; Wu, S. Validity and reliability of the neck disability index for cervical spondylopathy patients. Chin. J. Rehabil. Med. 2008, 23, 625–628. [Google Scholar]
- Prushansky, T.; Dvir, Z. Cervical Motion Testing: Methodology and Clinical Implications. J. Manip. Physiol. Ther. 2008, 31, 503–508. [Google Scholar] [CrossRef]
- Audette, I.; Dumas, J.P.; Côté, J.N.; De Serres, S.J. Validity and between-day reliability of the cervical range of motion (CROM) device. J. Orthop. Sports Phys. Ther. 2010, 40, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Gps 600 Postural Lab. Available online: http://www.globalposturalsystem.com/hardware/03008-gps-600-postural-lab/ (accessed on 1 September 2022).
- Gobbi, G.; Galli, D.; Carubbi, C.; Pelosi, A.; Lillia, M.; Gatti, R.; Queirolo, V.; Costantino, C.; Vitale, M.; Saccavini, M.; et al. Assessment of body plantar pressure in elite athletes: An observational study. Sport Sci. Health 2013, 9, 13–18. [Google Scholar] [CrossRef]
- Toprak, M.; Alptekin, H.K.; Turhan, D. Correction to: P-12 Assessment of Symmetrigraph and Global Postural System Results for the Posture Analysis of the Healthy Individuals. Chiropr. Man. Therap. 2018, 26, 20. [Google Scholar] [CrossRef] [PubMed]
- Xia, N.; Zhang, T.; Wang, C.; Zheng, Q.; Huang, J. Three indicators from two-dimensional body surface photographic measurements to assess the posture of patients with non- specific neck pain: A reliability and validity research. Chin. J. Rehabil. Med. 2019, 34, 1168–1172. [Google Scholar]
- Zheng, Q.; Huang, X.L.; Wang, L.; Xie, L.F. A preliminary study on the reliability of quantitative evaluation of static upright posture. Chin. J. Rehabil. Med. 2019, 34, 1178–1182. [Google Scholar]
- Maitland, G.D.; Hengeveld, E.; Banks, K.; English, K. Maitland’s Vertebral Manipulation, 7th ed.; Elsevier Butterworth-Heinemann: New York, NY, USA, 2005; pp. 320–321. [Google Scholar]
- Jull, G.; Trott, P.; Potter, H.; Zito, G.; Niere, K.; Shirley, D.; Emberson, J.; Marschner, I.; Richardson, C. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine 2002, 27, 1835–1842. [Google Scholar] [CrossRef]
- Beer, A.; Treleaven, J.; Jull, G. Can a functional postural exercise improve performance in the cranio-cervical flexion test?-A preliminary study. Man. Ther. 2012, 17, 219–224. [Google Scholar] [CrossRef]
- Jull, G.; Sterling, M.; Falla, D.; Treleaven, J.; O’Leary, S. Whiplash, Headache, and Neck Pain, 1st ed.; Elsevier: Amsterdam, The Netherlands, 2008; ISBN 9780443100475. [Google Scholar]
- Harrison, D.E.; Cailliet, R.; Betz, J.W.; Harrison, D.D.; Colloca, C.J.; Haas, J.W.; Janik, T.J.; Holland, B. A non-randomized clinical control trial of Harrison mirror image methods for correcting trunk list (lateral translations of the thoracic cage) in patients with chronic low back pain. Eur. Spine J. 2005, 14, 155–162. [Google Scholar] [CrossRef]
- Youssef, A.S.A.; Xia, N.; Emara, S.T.E.; Moustafa, I.M.; Huang, X. Addition of a new three-dimensional adjustable cervical thoracic orthosis to a multi-modal program in the treatment of nonspecific neck pain: Study protocol for a randomised pilot trial. Trials 2019, 20, 248. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2012, 10, 28–55. [Google Scholar] [CrossRef] [PubMed]
- Oliver, M.J.; Twomey, L.T. Extension creep in the lumbar spine. Clin. Biomech. 1995, 10, 363–368. [Google Scholar] [CrossRef]
- Burstein, A.H. Biomechanics in the Musculoskeletal System; Churchill Livingstone: London, UK, 2001; Volume 83, ISBN 0443065853. [Google Scholar]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A.; O’Cathain, A.; Altman, D.; Bretz, F.; et al. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016, 2, 64. [Google Scholar] [CrossRef] [PubMed]

| Conventional Treatment | Description |
|---|---|
| Moist hot pack | Applied to the area of pain at neck region muscles, such as the upper part of the trapezius, levator scapulae, splenius capitis, and cervicis muscles, for 15 min. |
| Soft tissue mobilization | Deep stroking massage performed along the entire length of the taut band within the painful or tight muscles. |
| Cervical mobilization | Low-velocity passive mobilization techniques to the symptomatic cervical segments as determined by the physiotherapist’s clinical examination. Physiotherapists could be able to select from what were termed passive accessory and physiological movement techniques as believed appropriate to the individual participant based on the initial and progressive reassessments. |
| Therapeutic exercises Cervical flexors | Level 1 Re-education of CCF movement pattern 1. Supine, knees bent -Gentle and controlled nodding action facilitated with eye movement 10 reps Holding. 2. Supine, knees bent -Repeated and sustained CCF 10 s holds × 10 reps Level 2 Interaction between the deep/superficial cervical flexors 1. Sitting -Controlled head movement through range of extension and return to neutral 10 reps Co-contraction of the deep cervical flexors/extensors. Level 3 Strength/endurance of the cervical flexors 1. Sitting -Isometric CCF in a range of cervical extension 10 s holds × 10 reps -Lifting the head off the wall (with the chair up to 30 cm away from the wall) 10 s holds × 10 reps 2. Supine -Lifting the head off a pillow (2 or 1 then 0 pillows as per participant’s capacity) 10 s holds × 10 reps. |
| Cervical extensors | Level 1 Re-education of extension movement pattern 1. Prone on elbows/four-point kneeling positions -Cranio cervical extension 3 sets of 5 reps. -Cranio cervical rotation (<45°) 3 sets of 5 reps. -Cervical extension while keeping the cranio cervical region in a neutral position 3 sets of 5 reps. Level 2 Co-contraction of the deep cervical flexors/extensors 1. Sitting -Isometric cervical rotation facilitated with eye movement (left/right sides) 5 s holds × 5 reps. Level 3 Strength/endurance of the cervical extensors 1. Prone on elbows/four-point kneeling positions -Isometric hold in range of cervical extension 10 s holds × 10 reps. |
| Cervico Scapular control | Level 1-Re-education of scapular movement control Cervico scapular muscle control 1. Sitting -Arm movement without load (external rotation/abduction/flexion < 30°) 10 reps -Arm movement without load throughout range 10 reps 2. Prone on elbows/four-point kneeling position -Thoracic lift (serratus anterior) and isometric hold 5 s holds × 5 reps. Level 2 Strength/endurance of cervico scapular muscles 1. Sitting -Arm movement with load using Thera-band (external rotation/abduction/flexion < 30°) 10 reps. -Arm movement with load throughout the range 10 reps. 2. Prone -Lift the shoulder off the bed and hold without arm load 10 s holds × 10 reps. -Lift the shoulder off the bed and hold with arm load using Thera-band 10 s holds × 10 reps. |
| Postural correction | Level 1 Correction of spinal posture Sitting -Active upright sitting initiated with lumbo-pelvic movement 10 s holds × 10 reps Level 2 Correction of spinal posture and scapular orientation Sitting -Actively positioning the scapular in a neutral posture while maintaining spinal posture 10 s holds × 10 reps Level 3 Spinal and scapular correction plus occipital lift Sitting -Actively lengthen the back of the neck while maintaining spinal and scapular posture 10 s holds × 10 reps. Standing on wall Actively extend spine then chin in cervical with squeezing abdomen 10 s holds × 10 reps. |
| 3D Posture Analysis of Head in Relation to Thoracic | Reverse 3D Posture Data by PCO (Mirror Image Therapy) |
|---|---|
| 1. Rx (extension position of the head) = 25° − 18° = 7° extension. | 7° flexion of the head. |
| 2. Ry (right or left rotation of the head) = 6° left rotation. | 6° right rotation of the head. |
| 3. Tz (anterior head translation = 5.8 cm anterior head translation. | 5.8 cm posterior head translation. |
| 4. Rz (right or left side bending) = 5° right side bending. | 5° left side bending. |
| 5. Tx (side shifting of the head = 1.4 cm right side shifting. | 1.4 cm left side shifting. |
| Primary Aim/Criteria | Description |
|---|---|
| Integrity of the study protocol • Recruitment: minimum requirement of 80% of eligible participants entering study. | With 45% of interested participants being eligible. 100% of eligible participants enrolled in the study. Inclusion criteria of the study protocol appeared acceptable. |
| Validity of eligibility criteria | The eligibility criteria were followed with another published paper [19], and our protocol that was published previously [47]. |
| Understanding and integrity of intervention for treating physical therapists | During the post-study interview, physical therapists said that one-week training before study was appropriate and enough, continuous communication with the study authors was essential to ensure that the protocol was followed throughout the study. |
| Convenience of intervention for participants | During the post-study interview, participants upraised the concern that with one treating physical therapist, appointments availability were limited. They felt that more availability of appointments would enhance recruitment and retention or more than treating physical therapist for every participant. |
| Integrity and suitability of intervention to participants | During the post-study interview, participants in both groups said that they believed the intervention was valuable, and they would participate in the study again. Only one issue was that the treatment period was too long and, hope to reduce treatment period of intervention in the future, and none expressed offense about being randomized to the control intervention. |
| Feasibility of study time requirement and study facilities for participants | During the post-study interview, while participants stated that a large time commitment was required to participate in the study, they all acknowledged that this was necessary for improvement. However, they advised us to reduce treatment sessions to less than 30 times although ten weeks was good time to make improvement in posture deviations. All participants felt that the services in which the interventions were delivered were appropriate. |
| Recruitment and retention procedures • Goals for minimum requirement for adequate recruitment and retention: at least 80% of participants attended 75% of appointments and completed 75% of the prescribed exercises | Fifty-four people responded to recruitment at rehabilitation clinic over a 9-months inclusion period. Of these, 45% fulfilled inclusion criteria, and all were included in the study at rehabilitation clinic. Of the 24 participants, 21 attended all treatment sessions and 3 lost before finishing treatment. No adverse events were recorded. Exercise intervention compliance was measured using either record sheet diaries or via WeChat application. |
| Testing of outcome measurement collection • Determined by completeness of outcome data collected, and through post-study interview | At the end of the study, all 21 participants who finished the study completed patient-reported outcome questionnaires, neck ROM and 3D posture parameters. The blinded outcome assessor, with no missing data, collected it for all participants. |
| Suitability of randomization procedure and methods used to ensure blinding • Determined during post-study interviews of treating physical therapist, blinded outcome assessor. Selection of the most appropriate primary outcome measure for a full-scale RCT Determined based on outcome measure with largest between group effect size | The randomization procedure was appropriate, with the treating physical therapist informed of group allocation but outcome measurement assessor was not aware of group allocation of any participants. All participants knew group allocation because of heterogeneity of interventions. NDI (0.79), as a measure of neck disability and quality of life, and 3D posture parameters of head in relation to thoracic (Tx, Tz, Rx, Rz, Ry) were selected. |
| Estimation of required sample size for a fully powered study • Based on NDI | A sample size of 42 participants (21 in each group) provides a minimum of 80% power (α = 0.05) and is required for an effect size of 0.79. To account for an estimated 20% dropout, the recommended sample size is 50 participants (25 in each group). |
| Study Group (n = 12) | Control Group (n = 12) | p-Value | |
|---|---|---|---|
| Age (y) mean ± SD | 27.4 ± 5.5 | 27.2 ± 4.7 | 0.7 |
| Weight (kg) mean ± SD | 64.58 ± 6.9 | 67.2 ± 5.8 | 0.3 |
| Height (m) mean ± SD | 1.65 ± 0.5 | 1.67 ± 0.6 | 0.6 |
| BMI (kg/m2), mean ± SD | 23.5 ± 1.2 | 24.2 ± 0.97 | 0.2 |
| Male, n (%) | 8 (66.7%) | 7 (58%) | 0.5 |
| Female, n (%) | 4 (33.3%) | 5 (42%) | 0.5 |
| Participants Employment | |||
| University student, n (%) | 7 (58%) | 6 (50%) | 0.6 |
| Desk office worker n (%) | 4 (33.3%) | 4 (33.3%) | 0.5 |
| House wife, n (%) | 1 (8.3%) | 2 (16.7%) | 0.6 |
| Married, n (%) | 4 (33.3%) | 3 (25%) | 0.7 |
| Duration of Pain, n (%) | |||
| 3–24 months | 8 (66.7%) | 9 (75%) | 0.6 |
| >24 months | 4 (33.3%) | 3 (25%) | 0.7 |
| Current use of Medications, n (%) | |||
| Yes | 2 | 3 | 0.6 |
| No | 10 | 9 | 0.7 |
| Referred pain, n (%) | 6 (50%) | 7 (58%) | 0.5 |
| Current smoker, n (%) | 2 (16.7%) | 3 (25%) | 0.6 |
| Baseline | Post Intervention | MD † (p Value 95% CI) | ES (d) | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| NDI (0–50) Study G | 12.42 ± 4.54 | 3.33 ± 2.42 | 9.1 ± 4.3 <0.001 * (6.4, 11.8) | 2.5 |
| Control G | 12.41 ± 3.02 | 5.41 ± 2.35 | 7 ± 1.13 <0.001 * (6.4, 7.7) | 2.5 |
| NPRS (0–10) Study G | 5 ± 1.4 | 1.8 ± 1.03 | 3.2 ± 1.26 <0.001 * (2.4, 3.9) | 2.6 |
| Control G | 4.91 ± 1.2 | 2.29 ± 0.87 | 2.6 ± 0.4 <0.001 * (2.4, 2.9) | 2.49 |
| Tx Study G | 0.97 ± 0.4 | 0.41 ± 0.13 | 0.56 ± 0.37 <0.001 * (0.3, 0.8) | 1.87 |
| Tx Control G | 0.75 ± 0.35 | 0.68 ± 0.31 | 0.075 ± 0.05 0.29 (0.04, 0.1) | 0.2 |
| Tz Study G | 3 ± 1.3 | 1.34 ± 1.1 | 1.6 ± 1.05 <0.001 * (0.9, 2.4) | 1.2 |
| Tz Control G | 3.1 ± 1.4 | 2.85 ± 1.6 | 0.24 ± 0.28 0.23(0.06, 0.4) | 0.15 |
| Rx Study G | 24.8 ± 4.17 | 19.41 ± 2.54 | 5.4 ± 3.2 <0.001 * (3.4, 7.45) | 1.56 |
| Control G | 23.8 ± 3.95 | 22.3 ± 3.98 | 1.5 ± 2.3 0.013 (0.03, 2.96) | 0.38 |
| Ry Study G | 3.5 ± 1.6 | 1.58 ± 0.67 | 2 ± 1.88 <0.001 * (0.7, 3.1) | 1.35 |
| Ry Control G | 3 ± 1.3 | 2.33 ± 1.4 | 0.5 ± 0.52 0.16 (0.2, 0.8) | 0.29 |
| Rz Study G | 3.3 ± 1.5 | 1.5 ± 0.79 | 1.83 ± 1.8 <0.001 * (0.7, 2.97) | 1.34 |
| Rz Control G | 3 ± 1.4 | 2.33 ± 1.4 | 0.5 ± 0.52 0.2 (0.2, 0.8) | 0.29 |
| ROM flex and extension Study G | 87.1 ± 4.18 | 108.1 ± 4 | −21 ± 0.18 <0.001 * (−21.3, −20.7) | 5 |
| Control G | 86.7 ± 4.37 | 100.6 ± 4 | −13.9 ± 0.37 <0.001 * (−14.4, −13.5) | 3.3 |
| ROM lateral flexion Study G | 65.75 ± 4.5 | 80.25 ± 4 | −14.5 ± 0.5 <0.001 * (−14.7, −14.3) | 3.4 |
| Control G | 63.91 ± 4.6 | 73.41 ± 4.2 | −9.5 ± 0.4 <0.001 * (−9.8, −9.4) | 2.1 |
| ROM rotation Study G | 101.8 ± 2.33 | 118.8 ± 2 | −17 ± 0.33 <0.001 * (−17.1, −16.96) | 7.8 |
| Control G | 101.58 ± 2.2 | 117.48 ± 2 | −15.9 ± 0.02 <0.001 * (−16, −15.8) | 7.5 |
| Study Group Change Score * (Baseline to Posttreatment) | Control Group Change Score * (Baseline to Posttreatment) | MD † (p Value 95% CI) | ES (d) | Estimated Total Sample Size for Outcome Measure, n ‡ | |
|---|---|---|---|---|---|
| NDI (0–50) | 9.1 ± 4.3 | 7 ± 1.13 | 2.08 <0.001 * (4.11, 0.06) | 0.79 | 42 |
| NPRS (0–10) | 3.2 ± 1.26 | 2.6 ± 0.4 | 0.458 <0.001 * (1.26, 0.35) | 0.58 | 76 |
| ROM flex and exten. | −21 ± 0.18 | −13.9 ± 0.37 | 7.42 <0.001 * (3.79, 11.1) | 1.78 | 14 |
| ROM lateral flexion | −14.5 ± 0.5 | −9.5 ± 0.4 | 6.8 <0.001 * (2.97, 10.7) | 1.26 | 22 |
| ROM rotation | −17 ± 0.33 | −15.9 ± 0.02 | 1.35 <0.001 * (−0.49, 3.2) | 0.56 | 80 |
| Study Group Change Score * | Control Group Change Score * | MD † (p Value 95% CI) | ES (d) | Estimated Total Sample Size for Outcome Measure, n ‡ | |
|---|---|---|---|---|---|
| Tx (side shifting of head) | 0.56 ± 0.37 | 0.07 ± 0.04 | .48 <0.001 * (−0.48, −0.05) | 1.70 | 18 |
| Tz (Ant. H. Translation) | 1.6 ± 1.05 | 0.24 ± 0.28 | 1.36 <0.001 * (−2.6, −0.28) | 1.1 | 38 |
| Rx (upper extension of head) | 5.4 ± 3.2 | 1.5 ± 2.3 | 3.9 <0.001 * (−5.75, −0.09) | 1.12 | 36 |
| Ry (rot. R.t or l.t of head) | 2 ± 1.88 | 0.5 ± 0.52 | 1.5 <0.001 * (−1.72, 0.22) | 0.96 | 48 |
| Rz (side bending R.t or l.t of head) | 1.83 ± 1.8 | 0.5 ± 0.52 | 1.33 <0.001 * (−1.8, 0.15) | 0.90 | 52 |
| Change in Neck Pain | Changes in NDI | Changes in ROM Flex and Exten | Changes in ROM Lateral Flexion | Changes in ROM Rotation | |
|---|---|---|---|---|---|
| Change in Tx (side shifting of head) | 0.5 <0.001 * | 0.5 | −0.48 <0.001 * | −0.51 <0.001 * | −0.41 0.01 |
| Change in Tz (Ant. H. Translation) | 0.6 <0.001 * | 0.31 0.06 | −0.53 <0.001 * | −0.43 0.04 | −0.33 0.05 |
| Change in Rx (upper extension of head) | 0.3 0.06 | 0.49 <0.001 * | −0.51 <0.001 * | −0.32 0.05 | −0.3 0.06 |
| Change in Ry (rot. R.t or l.t of head) | 0.5 <0.001 * | 0.62 <0.001 * | −0.4 0.01 | −0.56 <0.001 * | −0.71 <0.001 * |
| Change in Rz (side bending R.t or l.t of head) | 0.4 0.01 | 0.46 <0.001 * | −0.3 0.06 | −0.51 <0.001 * | −0.54 <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Youssef, A.S.A.; Moustafa, I.M.; El Melhat, A.M.; Huang, X.; Oakley, P.A.; Harrison, D.E. Randomized Feasibility Pilot Trial of Adding a New Three-Dimensional Adjustable Posture-Corrective Orthotic to a Multi-Modal Program for the Treatment of Nonspecific Neck Pain. J. Clin. Med. 2022, 11, 7028. https://doi.org/10.3390/jcm11237028
Youssef ASA, Moustafa IM, El Melhat AM, Huang X, Oakley PA, Harrison DE. Randomized Feasibility Pilot Trial of Adding a New Three-Dimensional Adjustable Posture-Corrective Orthotic to a Multi-Modal Program for the Treatment of Nonspecific Neck Pain. Journal of Clinical Medicine. 2022; 11(23):7028. https://doi.org/10.3390/jcm11237028
Chicago/Turabian StyleYoussef, Ahmed S. A., Ibrahim M. Moustafa, Ahmed M. El Melhat, Xiaolin Huang, Paul A. Oakley, and Deed E. Harrison. 2022. "Randomized Feasibility Pilot Trial of Adding a New Three-Dimensional Adjustable Posture-Corrective Orthotic to a Multi-Modal Program for the Treatment of Nonspecific Neck Pain" Journal of Clinical Medicine 11, no. 23: 7028. https://doi.org/10.3390/jcm11237028
APA StyleYoussef, A. S. A., Moustafa, I. M., El Melhat, A. M., Huang, X., Oakley, P. A., & Harrison, D. E. (2022). Randomized Feasibility Pilot Trial of Adding a New Three-Dimensional Adjustable Posture-Corrective Orthotic to a Multi-Modal Program for the Treatment of Nonspecific Neck Pain. Journal of Clinical Medicine, 11(23), 7028. https://doi.org/10.3390/jcm11237028








