Degree of Pelvic Rotation in the Coronal Plane on Postoperative Radiographs Obtained after Total Hip Arthroplasty
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
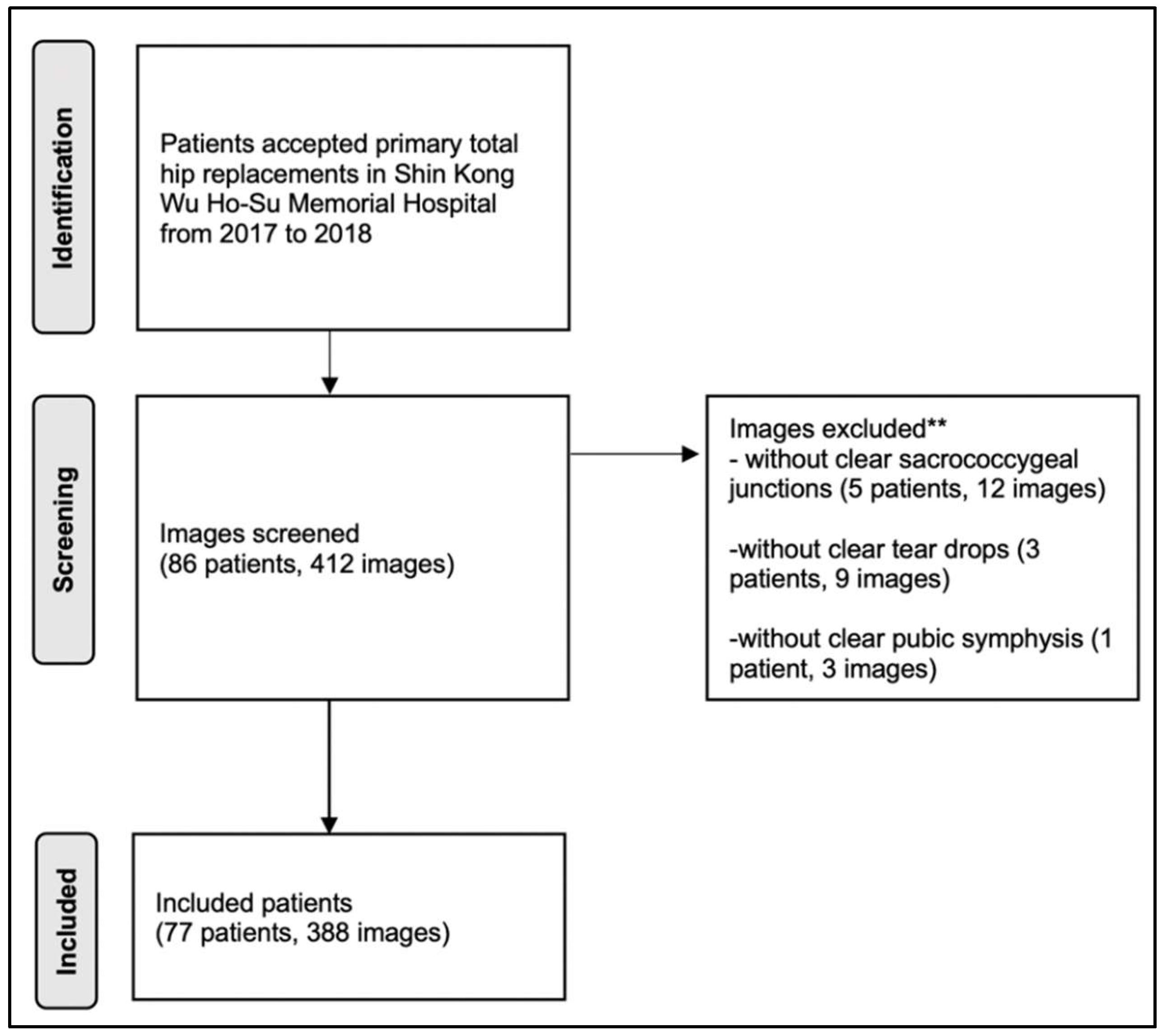
2.2. Participants
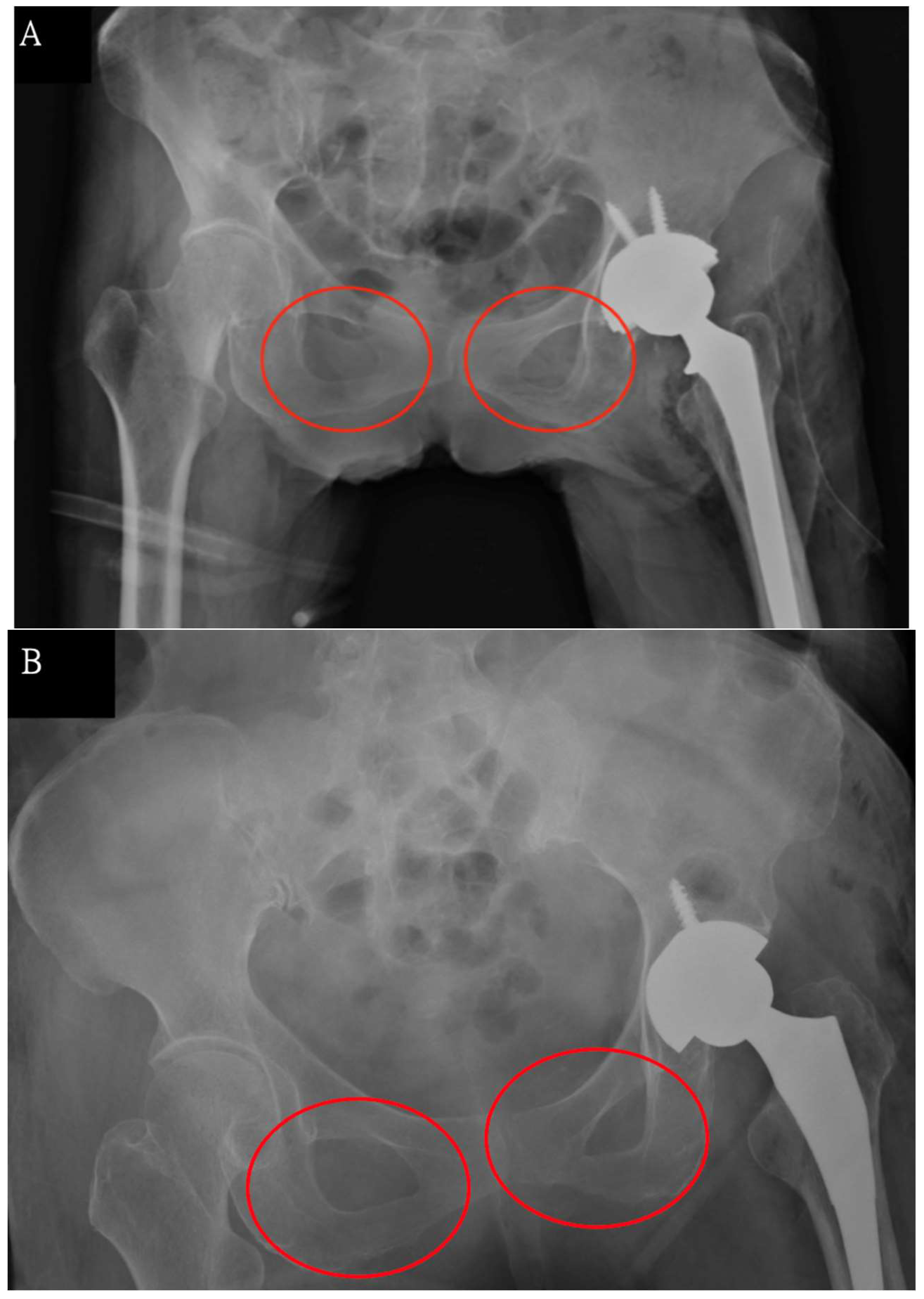
2.3. Anatomical Landmarks on Radiographic Images
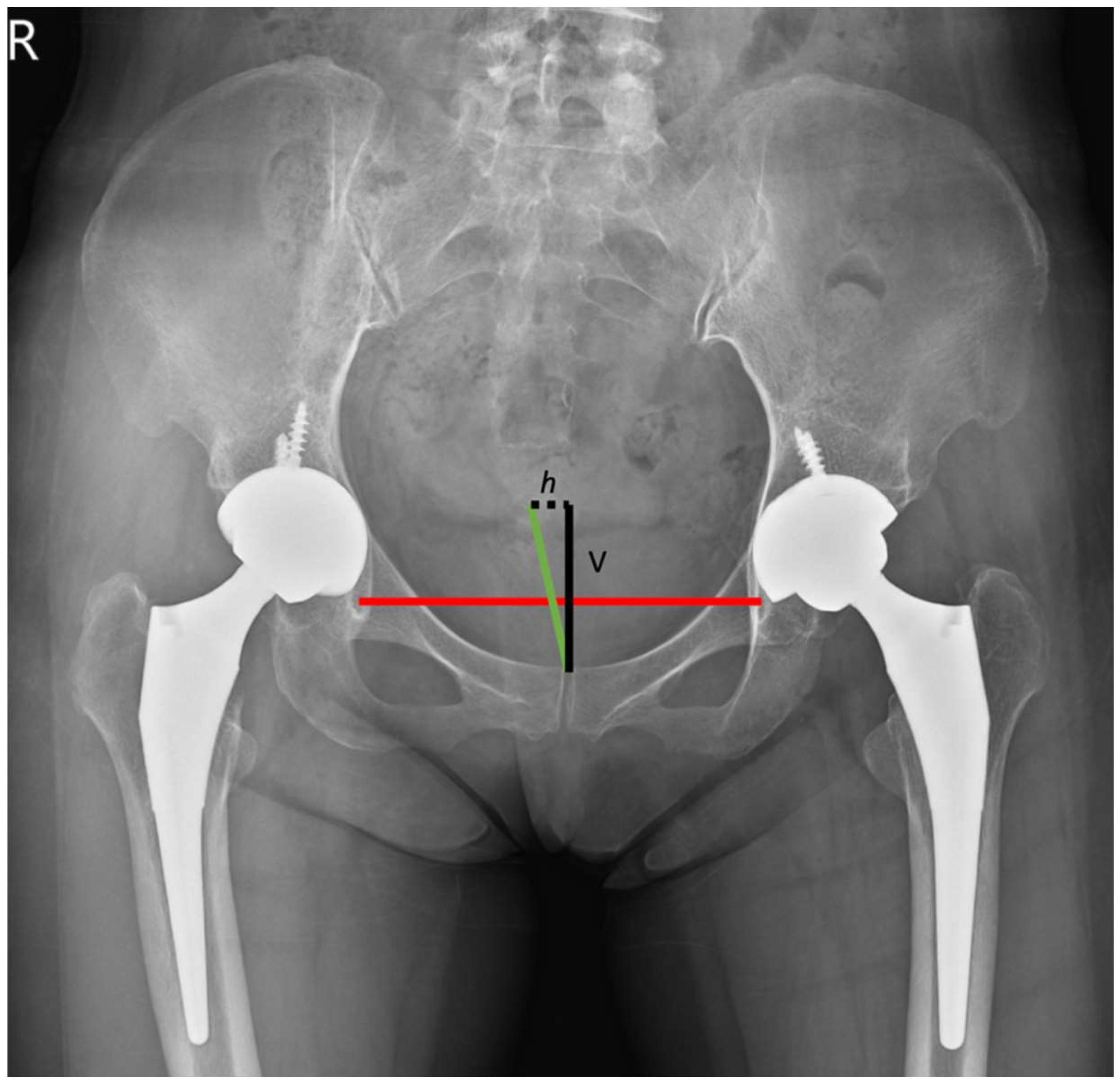
2.4. Pelvic Rotation Equation
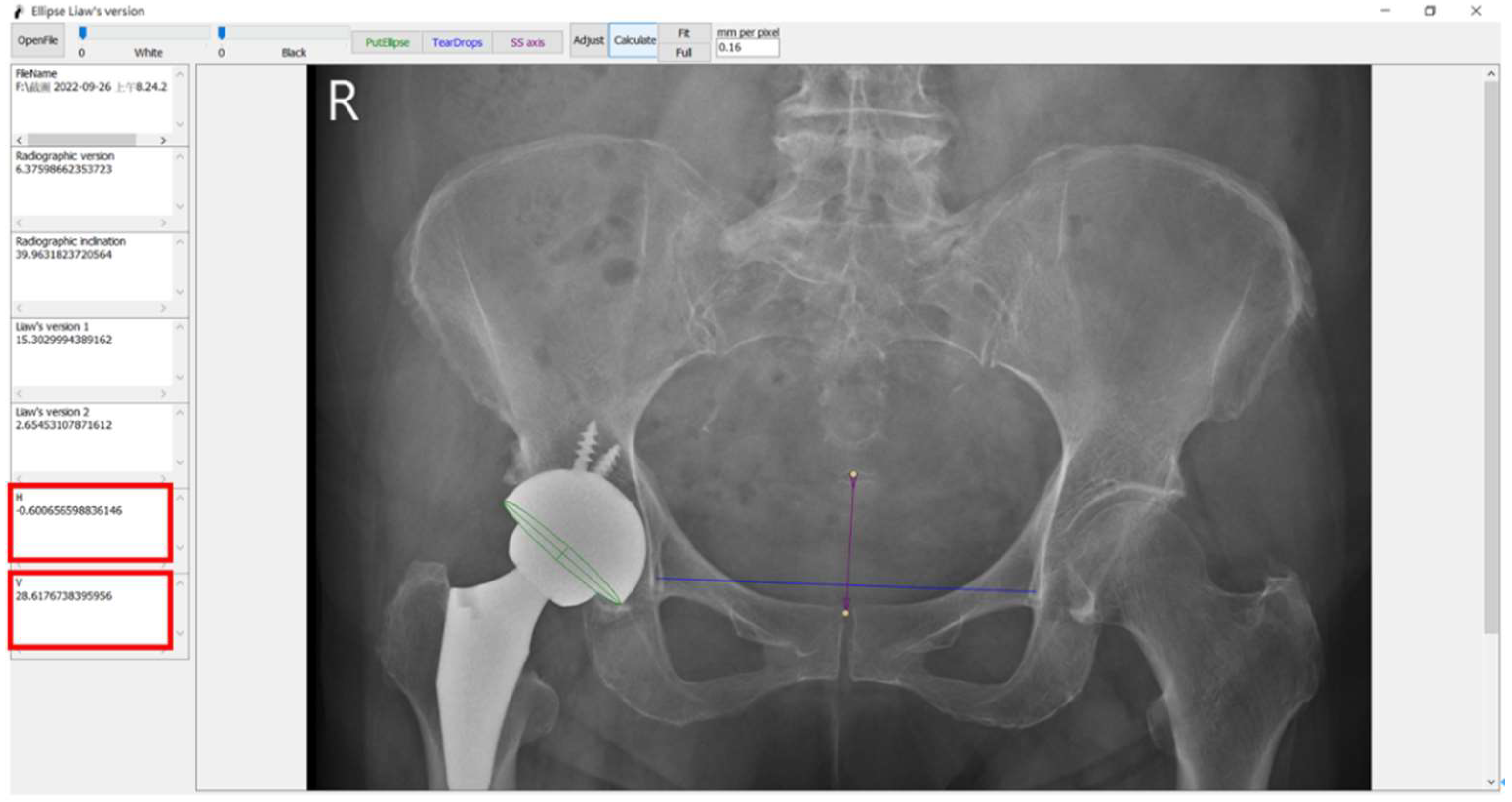
2.5. Software
2.6. Statistical Analyses
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vendittoli, P.-A.; Martinov, S.; Morcos, M.W.; Sivaloganathan, S.; Blakeney, W.G. Personalized hip joint replacement with large diameter head: Current concepts. J. Clin. Med. 2022, 11, 1918. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, I.N.; Soh, S.-E.; de Steiger, R. Actual versus forecast burden of primary hip and knee replacement surgery in Australia: Analysis of data from the Australian Orthopaedic Association National Joint Replacement Registry. J. Clin. Med. 2022, 11, 1883. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.Y.; Yoon, T.-R. Recent updates for biomaterials used in total hip arthroplasty. Biomater. Res. 2018, 22, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeh, K.L.; Wu, T.Y.; Ma, H.H.; Hou, S.M.; Liaw, C.K. Ellipse method for measuring Liaw’s anteversion of the acetabular component after total hip arthroplasty. BMC Musculoskelet. Disord. 2020, 21, 667. [Google Scholar] [CrossRef] [PubMed]
- Liaw, C.K.; Hou, S.M.; Yang, R.S.; Wu, T.Y.; Fuh, C.S. A new tool for measuring cup orientation in total hip arthroplasties from plain radiographs. Clin. Orthop. Relat. Res. 2006, 451, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Song, J.H.; Kim, Y.S.; Kwon, S.Y.; Lim, Y.W.; Jung, J.; Oh, S. Usefulness of intraoperative C-arm image intensifier in reducing errors of acetabular component during primary total hip arthroplasty: An application of Widmer’s method. BMC Musculoskelet. Disord. 2021, 22, 892. [Google Scholar] [CrossRef] [PubMed]
- Liaw, C.-K.; Yang, R.S.; Hou, S.M.; Wu, T.Y.; Fuh, C.S. A simple mathematical standardized measurement of acetabulum anteversion after total hip arthroplasty. Comput. Math. Methods Med. 2008, 9, 219872. [Google Scholar] [CrossRef] [Green Version]
- Murphy, W.S.; Yun, H.H.; Hayden, B.; Kowal, J.H.; Murphy, S.B. The Safe Zone Range for Cup Anteversion Is Narrower than for Inclination in THA. Clin. Orthop. Relat. Res. 2018, 476, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Danaei, B.; McPhee, J. Model-Based Acetabular Cup Orientation Optimization Based on Minimizing the Risk of Edge-Loading and Implant Impingement Following Total Hip Arthroplasty. J. Biomech. Eng. 2022, 144, 111008. [Google Scholar] [CrossRef] [PubMed]
- Biedermann, R. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty. J. Bone Jt. Surg. Am. 2007, 89, 1869. [Google Scholar] [CrossRef] [PubMed]
- Tannast, M.; Langlotz, U.; Siebenrock, K.A.; Wiese, M.; Bernsmann, K.; Langlotz, F. Anatomic referencing of cup orientation in total hip arthroplasty. Clin. Orthop. Relat. Res. 2005, 436, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Lützner, C.; Deckert, S.; Günther, K.P.; Postler, A.E.; Lützner, J.; Schmitt, J.; Limb, D.; Lange, T. Indication criteria for total hip arthroplasty in patients with hip osteoarthritis—Recommendations from a German Consensus Initiative. Medicina 2022, 58, 574. [Google Scholar] [CrossRef] [PubMed]
- Polesello, G.C.; Nakao, T.S.; Queiroz, M.C.D.; Daniachi, D.; Ricioli Junior, W.; Guimarães, R.P.; Honda, E.K. Proposal for standardization of radiographic studies on the hip and pelvis. Rev. Bras. Ortop. 2011, 46, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Becker, L.; Taheri, N.; Haffer, H.; Muellner, M.; Hipfl, C.; Ziegeler, K.; Diekhoff, T.; Pumberger, M. Lumbosacral Transitional Vertebrae Influence on Acetabular Orientation and Pelvic Tilt. J. Clin. Med. 2022, 11, 5153. [Google Scholar] [CrossRef] [PubMed]
- Barrack, R.L. Dislocation after total hip arthroplasty: Implant design and orientation. J. Am. Acad. Orthop. Surg. 2003, 11, 89–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nho, J.H.; Lee, Y.K.; Kim, H.J.; Ha, Y.C.; Suh, Y.S.; Koo, K.H. Reliability and validity of measuring version of the acetabular component. J. Bone Jt. Surg. Br. 2012, 94, 32–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, Y.S.; Shin, W.C.; Lee, S.M.; Kwak, S.H.; Bae, J.Y.; Suh, K.T. The best method for evaluating anteversion of the acetabular component after total hip arthroplasty on plain radiographs. J. Orthop. Surg. Res. 2018, 13, 66. [Google Scholar] [CrossRef] [PubMed]
- Butz, I.; Moser, S.; Nau, S.; Hiermaier, S. Data assimilation of structural deformation using finite element simulations and single-perspective projection data based on the example of X-ray imaging. SN Appl. Sci. 2021, 3, 545. [Google Scholar] [CrossRef]
- Fotouhi, J.; Liu, X.; Armand, M.; Navab, N.; Unberath, M. Reconstruction of Orthographic Mosaics from Perspective X-ray Images. IEEE Trans. Med. Imaging 2021, 40, 3165–3177. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.W.; Seo, J.; Moon, J. TapNet: Neural Network Augmented with Task-Adaptive Projection for Few-Shot Learning. In Proceedings of the 36th International Conference on Machine Learning, Long Beach, CA, USA, 10–15 June 2019; PMLR: New York, NY, USA, 2019; pp. 7115–7123. [Google Scholar]
- Guo, X.; Tang, J.; Li, J.; Shen, C.; Liu, J. Attitude measurement based on imaging ray tracking model and orthographic projection with iteration algorithm. ISA Trans. 2019, 95, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Tjahjadi, M.E.; Agustina, F.D. Single image orientation of UAV’s imagery using orthogonal projection model. In Proceedings of the Symposium on Geoinformatics, Malang, Indonesia, 24–25 November 2017; pp. 18–23. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeh, K.-L.; Wu, T.-Y.; Fuh, C.-S.; Chen, C.-S.; Hou, S.-M.; Chiang, C.-H.; Liaw, C.-K. Degree of Pelvic Rotation in the Coronal Plane on Postoperative Radiographs Obtained after Total Hip Arthroplasty. J. Clin. Med. 2022, 11, 6353. https://doi.org/10.3390/jcm11216353
Yeh K-L, Wu T-Y, Fuh C-S, Chen C-S, Hou S-M, Chiang C-H, Liaw C-K. Degree of Pelvic Rotation in the Coronal Plane on Postoperative Radiographs Obtained after Total Hip Arthroplasty. Journal of Clinical Medicine. 2022; 11(21):6353. https://doi.org/10.3390/jcm11216353
Chicago/Turabian StyleYeh, Kuei-Lin, Tai-Yin Wu, Chiou-Shann Fuh, Chu-Song Chen, Sheng-Mou Hou, Chen-Hao Chiang, and Chen-Kun Liaw. 2022. "Degree of Pelvic Rotation in the Coronal Plane on Postoperative Radiographs Obtained after Total Hip Arthroplasty" Journal of Clinical Medicine 11, no. 21: 6353. https://doi.org/10.3390/jcm11216353
APA StyleYeh, K.-L., Wu, T.-Y., Fuh, C.-S., Chen, C.-S., Hou, S.-M., Chiang, C.-H., & Liaw, C.-K. (2022). Degree of Pelvic Rotation in the Coronal Plane on Postoperative Radiographs Obtained after Total Hip Arthroplasty. Journal of Clinical Medicine, 11(21), 6353. https://doi.org/10.3390/jcm11216353







