Association between Germline Single-Nucleotide Variants in ADME Genes and Major Molecular Response to Imatinib in Chronic Myeloid Leukemia Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Response Definition and Patient Classification
2.3. Genotype Analysis in the Discovery Set and in the Extended Cohort
2.4. Statistical and Bioinformatics Analysis
3. Results
3.1. gSNVs Associated with MMR Achievement in the Discovery Set
3.2. gSNVs Associated with MMR Achievement in the Extended Cohort
3.3. Validation of the Results Obtained in the Extended Cohort by Cross-Validation Analysis and Permutation Test
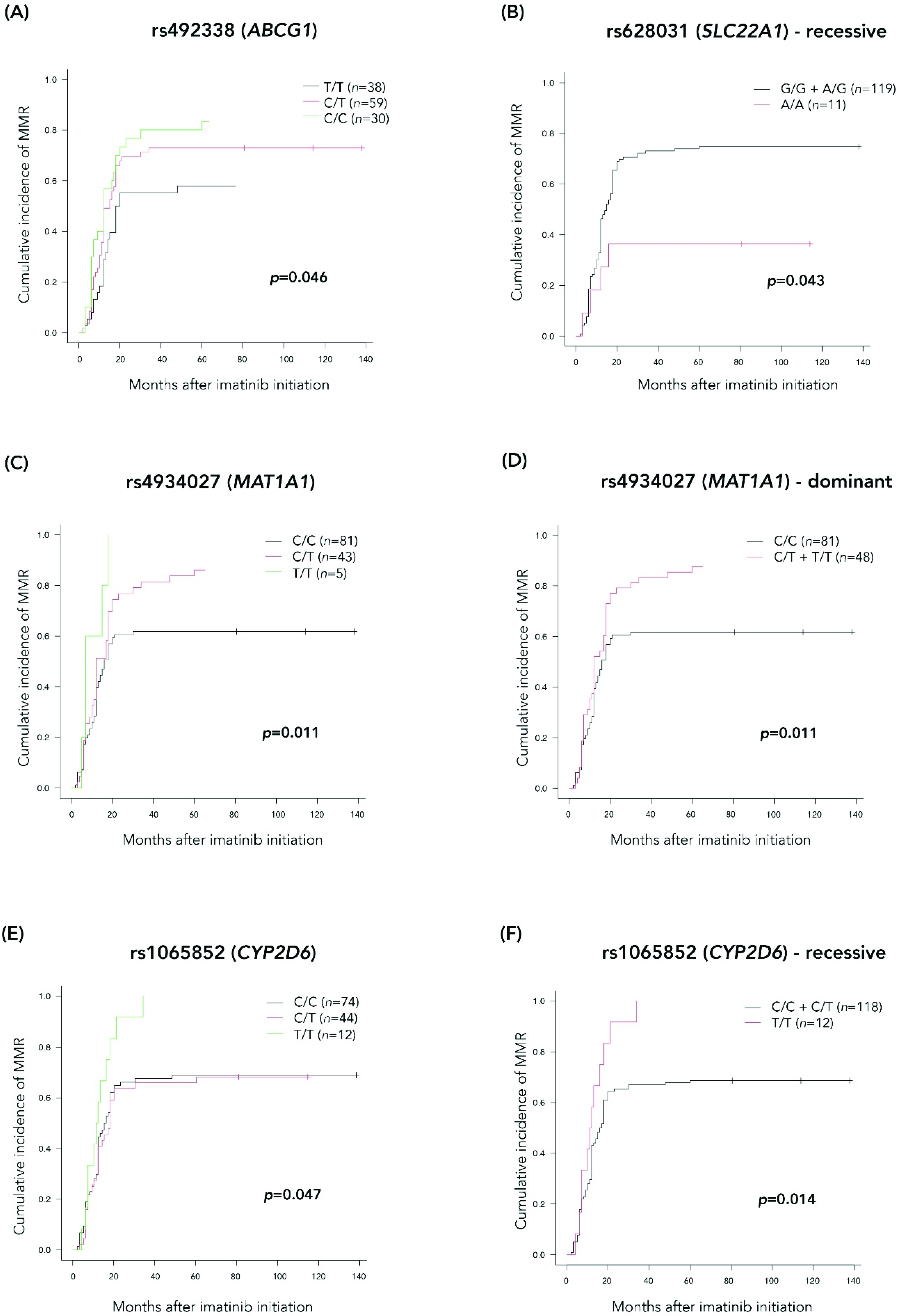
3.4. Cumulative Incidences of MMR Achievement for the Selected Significant gSNVs Obtained in the Extended Cohort
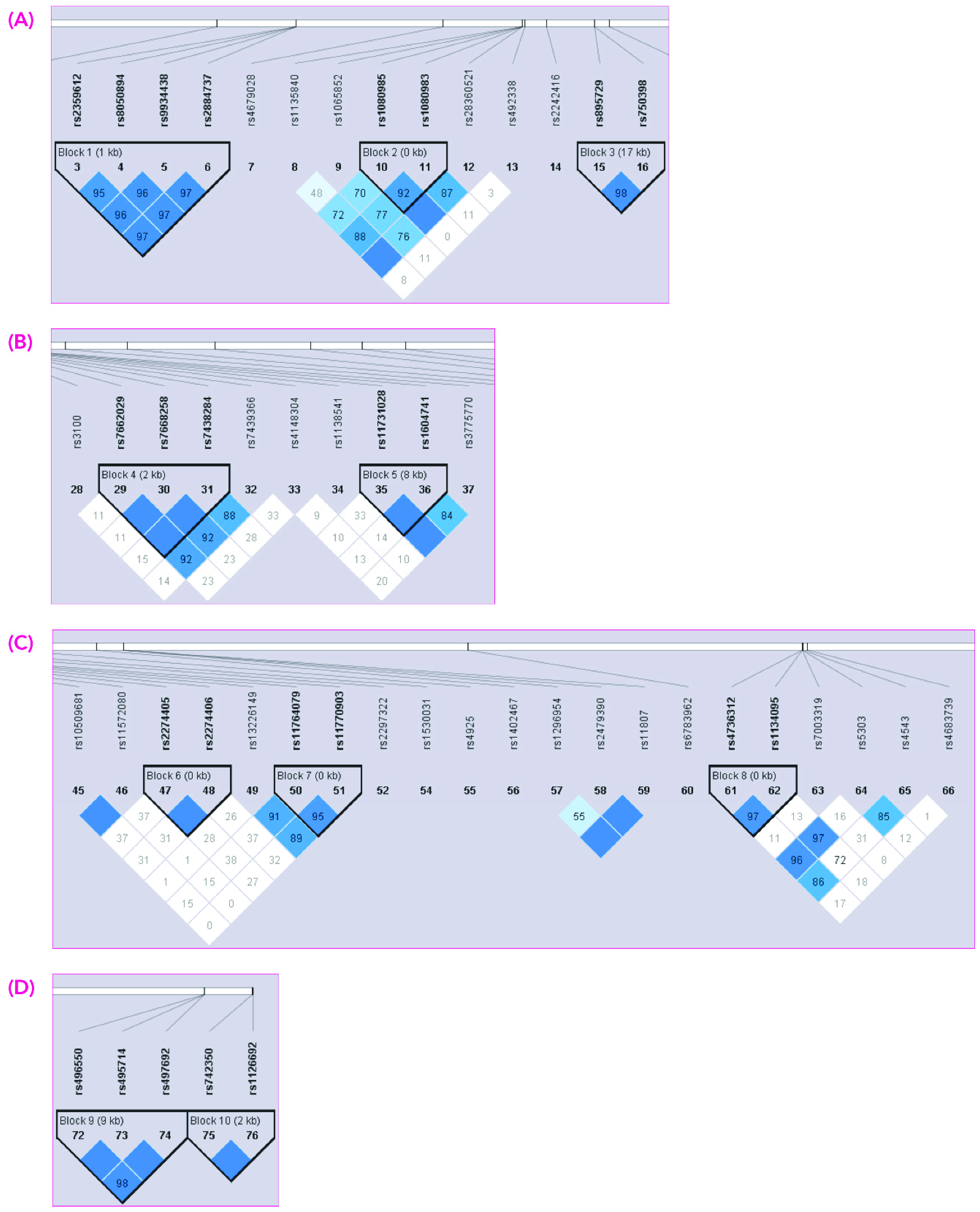
3.5. Haplotype Analysis and Association with MMR Achievement
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mahon, F.X. Treatment-free remission in CML: Who, how, and why? Hematol. Am. Soc. Hematol. Educ. Program 2017, 1, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Hochhaus, A.; Baccarani, M.; Silver, R.T.; Schiffer, C.; Apperley, J.F.; Cervantes, F.; Clark, R.E.; Cortes, J.E.; Deininger, M.W.; Guilhot, F.; et al. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia 2020, 34, 966–984. [Google Scholar] [CrossRef]
- Etienne, G.; Dulucq, S.; Huguet, F.; Schmitt, A.; Lascaux, A.; Hayette, S.; Fort, M.P.; Sujobert, P.; Bijou, F.; Morisset, S.; et al. Incidence and outcome of BCR-ABL mutated chronic myeloid leukemia patients who failed to tyrosine kinase inhibitors. Cancer Med. 2019, 8, 5173–5182. [Google Scholar] [CrossRef] [PubMed]
- Soverini, S.; Branford, S.; Nicolini, F.E.; Talpaz, M.; Deininger, M.W.; Martinelli, G.; Müller, M.C.; Radich, J.P.; Shah, N.P. Implications of BCR-ABL1 kinase domain-mediated resistance in chronic myeloid leukemia. Leuk. Res. 2014, 38, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q.; Lu, A.Y. Pharmacogenetics, pharmacogenomics, and individualized medicine. Pharmacol. Rev. 2011, 63, 437–459. [Google Scholar] [CrossRef]
- Hu, S.; Franke, R.M.; Filipski, K.K.; Hu, C.; Orwick, S.J.; de Bruijn, E.A.; Burger, H.; Baker, S.D.; Sparreboom, A. Interaction of imatinib with human organic ion carriers. Clin. Cancer Res. 2008, 14, 3141–3148. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.; Wang, L.; Clark, R.E.; Pirmohamed, M. Active transport of imatinib into and out of cells: Implications for drug resistance. Blood 2004, 104, 3739–3745. [Google Scholar] [CrossRef] [PubMed]
- Burger, K.; Nooter, K. Pharmacokinetic Resistance to Imatinib Mesylate: Role of the ABC Drug Pumps ABCG2 (BCRP) and ABCB1 (MDR1) in the Oral Bioavailability of Imatinib. Cell Cycle 2004, 3, 1502–1505. [Google Scholar] [CrossRef] [PubMed]
- Peng, B.; Hayes, M.; Resta, D.; Racine-Poon, A.; Druker, B.J.; Talpaz, M.; Sawyers, C.L.; Rosamilia, M.; Ford, J.; Lloyd, P.; et al. Pharmacokinetics and pharmacodynamics of imatinib in a phase I trial with chronic myeloid leukemia patients. J. Clin. Oncol. 2004, 22, 935–942. [Google Scholar] [CrossRef]
- Dulucq, S.; Bouchet, S.; Turcq, B.; Lippert, E.; Etienne, G.; Reiffers, J.; Molimard, M.; Krajinovic, M.; Mahon, F.X. Multidrug resistance gene (MDR1) polymorphisms are associated with major molecular responses to standard-dose imatinib in chronic myeloid leukemia. Blood 2008, 112, 2024–2027. [Google Scholar] [CrossRef]
- Kim, D.H.; Sriharsha, L.; Xu, W.; Kamel-Reid, S.; Liu, X.; Siminovitch, K.; Messner, H.A.; Lipton, J.H. Clinical Relevance of a Pharmacogenetic Approach Using Multiple Candidate Genes to Predict Response and Resistance to Imatinib Therapy in Chronic Myeloid Leukemia. Clin. Cancer Res. 2009, 15, 4750–4758. [Google Scholar] [CrossRef]
- Ni, L.N.; Li, J.Y.; Miao, K.R.; Qiao, C.; Zhang, S.J.; Qiu, H.R.; Qian, S.X. Multidrug resistance gene (MDR1) polymorphisms correlate with imatinib response in chronic myeloid leukemia. Med. Oncol. 2011, 28, 265–269. [Google Scholar] [CrossRef]
- Maffioli, M.; Camós, M.; Gaya, A.; Hernández-Boluda, J.C.; Alvarez-Larrán, A.; Domingo, A.; Granell, M.; Guillem, V.; Vallansot, R.; Costa, D.; et al. Correlation between genetic polymorphisms of the hOCT1 and MDR1 genes and the response to imatinib in patients newly diagnosed with chronic-phase chronic myeloid leukemia. Leuk. Res. 2011, 35, 1014–1019. [Google Scholar] [CrossRef] [PubMed]
- Ben Hassine, I.; Gharbi, H.; Soltani, I.; Ben Hadj Othman, H.; Farrah, A.; Amouri, H.; Teber, M.; Ghedira, H.; Ben Youssef, Y.; Safra, I.; et al. Molecular study of ABCB1 gene and its correlation with imatinib response in chronic myeloid leukemia. Cancer Chemother. Pharmacol. 2017, 80, 829–839. [Google Scholar] [CrossRef] [PubMed]
- Angelini, S.; Soverini, S.; Ravegnini, G.; Barnett, M.; Turrini, E.; Thornquist, M.; Pane, F.; Hughes, T.P.; White, D.L.; Radich, J.; et al. Association between imatinib transporters and metabolizing enzymes genotype and response in newly diagnosed chronic myeloid leukemia patients receiving imatinib therapy. Haematologica 2013, 98, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Koren-Michowitz, M.; Buzaglo, Z.; Ribakovsky, E.; Schwarz, M.; Pessach, I.; Shimoni, A.; Beider, K.; Amariglio, N.; le Coutre, P.; Nagler, A. OCT1 genetic variants are associated with long term outcomes in imatinib treated chronic myeloid leukemia patients. Eur. J. Haematol. 2014, 92, 283–288. [Google Scholar] [CrossRef] [PubMed]
- de Lima, L.T.; Bueno, C.T.; Vivona, D.; Hirata, R.D.; Hirata, M.H.; Hungria, V.T.; Chiattone, C.S.; Zanichelli, M.A.; Chauffaille, M.L.; Guerra-Shinohara, E.M. Relationship between SLCO1B3 and ABCA3 polymorphisms and imatinib response in chronic myeloid leukemia patients. Hematology 2015, 20, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, S.; Ghosh, K.; Shanmukhaiah, C.; Vundinti, B.R. Genetic variations of hOCT1 gene and CYP3A4/A5 genes and their association with imatinib response in Chronic Myeloid Leukemia. Eur. J. Pharmacol. 2015, 765, 124–130. [Google Scholar] [CrossRef]
- Di Martino, M.T.; Arbitrio, M.; Leone, E.; Guzzi, P.H.; Rotundo, M.S.; Ciliberto, D.; Tomaino, V.; Fabiani, F.; Talarico, D.; Sperlongano, P.; et al. Single nucleotide polymorphisms of ABCC5 and ABCG1 transporter genes correlate to irinotecan-associated gastrointestinal toxicity in colorectal cancer patients: A DMET microarray profiling study. Cancer Biol. Ther. 2011, 12, 780–787. [Google Scholar] [CrossRef] [PubMed]
- Nieuweboer, A.J.; Smid, M.; de Graan, A.J.; Elbouazzaoui, S.; de Bruijn, P.; Martens, J.W.; Mathijssen, R.H.; van Schaik, R.H. Predicting paclitaxel-induced neutropenia using the DMET platform. Pharmacogenomics 2015, 16, 1231–1241. [Google Scholar] [CrossRef]
- Arbitrio, M.; Di Martino, M.T.; Barbieri, V.; Agapito, G.; Guzzi, P.H.; Botta, C.; Iuliano, E.; Scionti, F.; Altomare, E.; Codispoti, S.; et al. Identification of polymorphic variants associated with erlotinib-related skin toxicity in advanced non-small cell lung cancer patients by DMET microarray analysis. Cancer Chemother. Pharmacol. 2016, 77, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Arbitrio, M.; Di Martino, M.T.; Scionti, F.; Agapito, G.; Guzzi, P.H.; Cannataro, M.; Tassone, P.; Tagliaferri, P. DMET™ (Drug Metabolism Enzymes and Transporters): A pharmacogenomic platform for precision medicine. Oncotarget 2016, 7, 54028–54050. [Google Scholar] [CrossRef] [PubMed]
- Branford, S.; Hughes, T.P.; Rudzki, Z. Monitoring chronic myeloid leukaemia therapy by real-time quantitative PCR in blood is a reliable alternative to bone marrow cytogenetics. Br. J. Haematol. 1999, 107, 587–599. [Google Scholar] [CrossRef]
- Baccarani, M.; Deininger, M.W.; Rosti, G.; Hochhaus, A.; Soverini, S.; Apperley, J.F.; Cervantes, F.; Clark, R.E.; Cortes, J.E.; Guilhot, F.; et al. European LeukemiaNet recommendations for the managemen of chronic myeloid leukemia: 2013. Blood 2013, 122, 872–884. [Google Scholar] [CrossRef]
- González, J.R.; Armengol, L.; Solé, X.; Guinó, E.; Mercader, J.M.; Estivill, X.; Moreno, V. SNPassoc: An R package to perform whole genome association studies. Bioinformatics 2007, 23, 654–655. [Google Scholar] [CrossRef] [PubMed]
- Barrett, J.; Fry, B.; Maller, J.; Daly, M. Haploview: Analysis and visualization of LD and haplotype maps. Bioinformatics 2005, 21, 263–265. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.C.; Hu, W.X.; Liu, Q.X.; Li, W.K.; Chen, F.Z.; Rao, Z.Z.; Liu, X.F.; Luo, Y.P.; Cao, Y.F. Genetic polymorphisms of metabolic enzymes CYP1A1, CYP2D6, GSTM1 and GSTT1 and leukemia susceptibility. Eur. J. Cancer Prev. 2008, 17, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Polillo, M.; Galimberti, S.; Baratè, C.; Petrini, M.; Danesi, R.; Di Paolo, A. Pharmacogenetics of BCR/ABL inhibitors in chronic myeloid leukemia. Int. J. Mol. Sci. 2015, 16, 22811–22829. [Google Scholar] [CrossRef] [PubMed]
- Hochhaus, A.; Larson, R.A.; Guilhot, F.; Radich, J.P.; Branford, S.; Hughes, T.P.; Baccarani, M.; Deininger, M.W.; Cervantes, F.; Fujihara, S.; et al. (IRIS Investigators). Long-Term Outcomes of Imatinib Treatment for Chronic Myeloid Leukemia. N. Engl. J. Med. 2017, 376, 917–927. [Google Scholar] [CrossRef]
- Takahashi, N.; Miura, M.; Scott, S.A.; Kagaya, H.; Kameoka, Y.; Tagawa, H.; Saitoh, H.; Fujishima, N.; Yoshioka, T.; Hirokawa, M.; et al. Influence of CYP3A5 and drug transporter polymorphisms on imatinib trough concentration and clinical response among patients with chronic phase chronic myeloid leukemia. J. Hum. Genet. 2010, 55, 731–737. [Google Scholar] [CrossRef] [PubMed]
- Cargnin, S.; Ravegnini, G.; Soverini, S.; Angelini, S.; Terrazzino, S. Impact of SLC22A1 and CYP3A5 genotypes on imatinib response in chronic myeloid leukemia: A systematic review and meta-analysis. Pharmacol. Res. 2018, 131, 244–254. [Google Scholar] [CrossRef] [PubMed]
- Shikata, E.; Yamamoto, R.; Takane, H.; Shigemasa, C.; Ikeda, T.; Otsubo, K.; Ieiri, I. Human organic cation transporter (OCT1 and OCT2) gene polymorphisms and therapeutic effects of metformin. J. Hum. Genet. 2017, 52, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Eechoute, K.; Sparreboom, A.; Burger, H.; Franke, R.M.; Schiavon, G.; Verweij, J.; Loos, W.J.; Wiemer, E.A.; Mathijssen, R.H. Drug Transporters and Imatinib Treatment: Implications for Clinical Practice. Clin. Cancer Res. 2011, 17, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.A.; Barrera, G.C.; Nakamura, K.; Baldán, A.; Tarr, P.; Fishbein, M.C.; Frank, J.; Francone, O.L.; Edwards, P.A. ABCG1 has a critical role in mediating cholesterol efflux to HDL and preventing cellular lipid accumulation. Cell Metab. 2005, 1, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Tarling, E.J.; Edwards, P.A. ATP binding cassette transporter G1 (ABCG1) is an intracellular sterol transporter. Proc. Nat. Acad. Sci. USA 2011, 108, 19719–19724. [Google Scholar] [CrossRef]
- Glodkowska-Mrowka, E.; Mrowka, P.; Basak, G.W.; Niesiobedzka-Krezel, J.; Seferynska, I.; Wlodarski, P.K.; Jakobisiak, M.; Stoklosa, T. Statins inhibit ABCB1 and ABCG2 drug transporter activity in chronic myeloid leukemia cells and potentiate antileukemic effects of imatinib. Exp. Hematol. 2014, 42, 439–447. [Google Scholar] [CrossRef]
- Bandyopadhyay, S.; Li, J.; Traer, E.; Tyner, J.W.; Zhou, A.; Oh, S.T.; Cheng, J.X. Cholesterol esterification inhibition and imatinib treatment synergistically inhibit growth of BCR-ABL mutation-independent resistant chronic myelogenous leukemia. PLoS ONE 2017, 12, e0179558. [Google Scholar] [CrossRef]
- Harivenkatesh, N.; Kumar, L.; Bakhshi, S.; Sharma, A.; Kabra, M.; Velpandian, T.; Gogia, A.; Shastri, S.S.; Biswas, N.R.; Gupta, Y.K. Influence of MDR1 and CYP3A5 genetic polymorphisms on trough levels and therapeutic response of imatinib in newly diagnosed patients with chronic myeloid leukemia. Pharmacol. Res. 2017, 120, 138–145. [Google Scholar] [CrossRef]
- Barratt, D.T.; Cox, H.K.; Menelaou, A.; Yeung, D.T.; White, D.L.; Hughes, T.P.; Somogyi, A.A. CYP2C8 Genotype Significantly Alters Imatinib Metabolism in Chronic Myeloid Leukaemia Patients. Clin. Pharmacokinet. 2017, 56, 977–985. [Google Scholar] [CrossRef]
- Ravegnini, G.; Urbini, M.; Simeon, V.; Genovese, C.; Astolfi, A.; Nannini, M.; Gatto, L.; Saponara, M.; Ianni, M.; Indio, V.; et al. An exploratory study by DMET array identifies a germline signature associated with imatinib response in gastrointestinal stromal tumor. Pharmacogenomics J. 2019, 19, 390–400. [Google Scholar] [CrossRef]
- Wittke-Thompson, J.K.; Pluzhnikov, A.; Cox, N.J. Rational Inferences about Departures from Hardy-Weinberg Equilibrium. Am. J. Hum. Genet. 2005, 76, 967–986. [Google Scholar] [CrossRef] [PubMed]

| Clinical Characteristics | Discovery Set (n = 45) | Extended Cohort (n = 137) | |
|---|---|---|---|
| Median age at diagnosis, y (range) | 52 (19–73) | 52 (23–86) | |
| Sex, n (%) | Female | 21 (47) | 57 (42) |
| Male | 24 (53) | 80 (58) | |
| Sokal, n (%) | Low risk | 20/42 (48) | 61/127 (48) |
| Int 1 risk | 18/42 (43) | 47/127 (37) | |
| High risk | 4/42 (9) | 19/127 (15) | |
| ELTS 2, n (%) | Low risk | 26/39 (67) | 53/84 (63) |
| Int risk | 11/39 (28) | 23/84 (27) | |
| High risk | 2/39 (5) | 8/84 (10) | |
| Imatinib treatment duration, m (range) | 52 (6–142) | 78 (6–208) | |
| Median follow-up, y (range) | 13 (5–18) | 13 (1–19) | |
| Exitus, n (%) | 5 (9) | 21 (15) | |
| Gene | RefSNP ID | Location | Model a | Genotype | N Cases b (%)/ N Controls c (%) | OR (95% CI) | p |
|---|---|---|---|---|---|---|---|
| SLC22A1 | rs628031 | Met408Leu | Recessive | G/G–A/G A/A | 30 (24)/94 (76) 7 (58)/5 (42) | 4.52 (1.33–15.43) | 0.015 |
| ABCG1 | rs492338 | Intron | Log-additive | 0: T/T 1: C/T 2: C/C | 16 (39)/25 (61) 16 (27)/43 (73) 5 (15)/28 (85) | 0.54 (0.31–0.92) | 0.021 |
| ABCB11 | rs496550 | Intron | Log-additive | 0: G/G 1: A/G 2: A/A | 15 (38)/24 (62) 19 (26)/55 (74) 3 (13)/20 (87) | 0.51 (0.28–0.94) | 0.027 |
| ABCB11 | rs497692 | Ala1028Ala | Log-additive | 0: G/G 1: A/G 2: A/A | 15 (38)/25 (62) 18 (25)/53 (75) 3 (13)/21 (87) | 0.51 (0.28–0.94) | 0.027 |
| CYP2D6 | rs1135840 d | Ser486Thr | Log-additive | 0: C/C 1: C/G 2: G/G | 12 (22)/43 (78) 12 (24)/39 (76) 13 (46)/15 (54) | 1.70 (1.03–2.82) | 0.037 |
| CYP11B1 | rs7003319 | 3′UTR | Dominant | C/C A/C–A/A | 11 (19)/48 (81) 26 (34)/51 (66) | 2.32 (1.02–5.25) | 0.038 |
| MAT1A | rs4934027 | Intron | Dominant | C/C C/T–T/T | 31 (36)/55(64) 6 (12)/43 (88) | 0.25 (0.1–0.65) | 0.002 |
| Group | Gene | RefSNP ID | Model a | Genotype | N Cases b (%)/ N Controls c (%) | OR (95% CI) | p |
|---|---|---|---|---|---|---|---|
| A | MAT1A | rs4934027 | Dominant | C/C C/T–T/T | 26 (36)/46 (64) 3 (8)/34 (92) | 0.16 (0.04–0.56) | 0.001 |
| B | CYP11B1 | rs7003319 | Dominant | C/C C/A–A/A | 6 (13)/39 (87) 24 (36)/42 (64) | 3.71 (1.37–10) | 0.006 |
| B | MAT1A | rs4934027 | Dominant | C/C C/T–T/T | 24 (36)/43 (64) 6 (14)/37 (86) | 0.29 (0.11–0.79) | 0.009 |
| C | ABCG1 | rs492338 | Log-additive | 0: T/T 1: C/T 2: C/C | 13 (38)/21 (62) 12 (27)/33 (73) 4 (15)/23 (85) | 0.54 (0.3–0.99) | 0.039 |
| C | CYP2D6 | rs1135840 | Log-additive | 0: C/C 1: C/G 2: G/G | 8 (19)/33 (81) 9 (21)/33 (79) 12 (52)/11 (48) | 2.11 (1.18–3.79) | 0.010 |
| C | MAT1A | rs4934027 | Dominant | C/C C/T–T/T | 26 (35)/48 (65) 3 (9)/30 (91) | 0.18 (0.05–0.66) | 0.003 |
| C | ABCB11 | rs495714 | Log-additive | 0: A/A 1: A/G 2: G/G | 13 (43)/17 (57) 14 (24)/45 (76) 2 (10)/19 (90) | 0.38 (0.19–0.77) | 0.005 |
| C | SLC22A1 | rs628031 | Log-additive | 0: G/G 1: A/G 2: A/A | 9 (21)/34 (79) 14 (25)/42 (75) 6 (67)/3 (33) | 2.14 (1.05–4.35) | 0.032 |
| C | ABCB11 | rs496550 | Log-additive | 0: G/G 1: G/A 2: A/A | 13 (43)/17 (57) 15 (25)/46 (75) 1 (6)/16 (94) | 0.35 (0.17–0.74) | 0.004 |
| C | ABCB11 | rs497692 | Log-additive | 0:G/G 1: G/A 2: A/A | 13 (42)/18 (58) 15 (25)/44 (75) 1 (6)/17 (94) | 0.37 (0.18–0.76) | 0.004 |
| D | ABCG1 | rs492338 | Log-additive | 0: T/T 1: C/T 2: C/C | 13 (38)/21 (62) 14 (29)/35 (71) 3 (13)/20 (87) | 0.53 (0.28–0.98) | 0.038 |
| D | CYP2D6 | rs1135840 | Log-additive | 0: C/C 1: C/G 2: G/G | 10 (21)/37 (79) 9 (23)/30 (77) 11 (50)/11 (50) | 1.86 (1.07–3.25) | 0.026 |
| D | MAT1A | rs4934027 | Dominant | C/C C/T–T/T | 24 (37)/40 (63) 6 (14)/37 (86) | 0.27 (0.1–0.73) | 0.006 |
| D | ABCB11 | rs496550 | Log-additive | 0: G/G 1: A/G 2: A/A | 12 (38)/20 (62) 16 (28)/41 (72) 2 (11)/17 (89) | 0.51 (0.26–0.99) | 0.04 |
| D | ABCB11 | rs497692 | Log-additive | 0: G/G 1: A/G 2: A/A | 12 (36)/21 (64) 15 (28)/39 (72) 2 (10)/18 (90) | 0.51 (0.26–0.99) | 0.04 |
| E | ABCG1 | rs492338 | Log-additive | 0: T/T 1: C/T 2: C/C | 14 (48)/15 (52) 13 (27)/36 (73) 3 (11)/24 (89) | 0.37 (0.19–0.71) | 0.002 |
| E | MAT1A | rs4934027 | Dominant | C/C C/T–T/T | 24 (36)/43 (64) 6 (15)/34 (85) | 0.32 (0.12–0.86) | 0.017 |
| E | SLC22A1 | rs628031 | Log-additive | 0: G/G 1: A/G 2: A/A | 8 (18)/37 (82) 16 (30)/37 (70) 6 (60)/4 (40) | 2.44 (1.22–4.88) | 0.009 |
| Gene | RefSNP ID | Model a | p |
|---|---|---|---|
| ABCG1 | rs492338 | Log-additive | 0.023 |
| CYP2D6 | rs1135840 | Log-additive Recessive | 0.032 0.016 |
| UGT2A1 | rs4148304 | Recessive | 0.012 |
| CYP11B1 | rs7003319 | Dominant | 0.047 |
| MAT1A | rs4934027 | Log-additive Dominant | 0.003 0.002 |
| CYP2D6 | rs1065852 | Recessive | 0.003 |
| SLC22A1 | rs628031 | Recessive | 0.017 |
| ABCB11 | rs496550 | Log-additive | 0.027 |
| ABCB11 | rs497692 | Log-additive | 0.027 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Estrada, N.; Zamora, L.; Ferrer-Marín, F.; Palomo, L.; García, O.; Vélez, P.; De la Fuente, I.; Sagüés, M.; Cabezón, M.; Cortés, M.; et al. Association between Germline Single-Nucleotide Variants in ADME Genes and Major Molecular Response to Imatinib in Chronic Myeloid Leukemia Patients. J. Clin. Med. 2022, 11, 6217. https://doi.org/10.3390/jcm11206217
Estrada N, Zamora L, Ferrer-Marín F, Palomo L, García O, Vélez P, De la Fuente I, Sagüés M, Cabezón M, Cortés M, et al. Association between Germline Single-Nucleotide Variants in ADME Genes and Major Molecular Response to Imatinib in Chronic Myeloid Leukemia Patients. Journal of Clinical Medicine. 2022; 11(20):6217. https://doi.org/10.3390/jcm11206217
Chicago/Turabian StyleEstrada, Natalia, Lurdes Zamora, Francisca Ferrer-Marín, Laura Palomo, Olga García, Patricia Vélez, Iris De la Fuente, Miguel Sagüés, Marta Cabezón, Montserrat Cortés, and et al. 2022. "Association between Germline Single-Nucleotide Variants in ADME Genes and Major Molecular Response to Imatinib in Chronic Myeloid Leukemia Patients" Journal of Clinical Medicine 11, no. 20: 6217. https://doi.org/10.3390/jcm11206217
APA StyleEstrada, N., Zamora, L., Ferrer-Marín, F., Palomo, L., García, O., Vélez, P., De la Fuente, I., Sagüés, M., Cabezón, M., Cortés, M., Vallansot, R. O., Senín-Magán, M. A., Boqué, C., & Xicoy, B. (2022). Association between Germline Single-Nucleotide Variants in ADME Genes and Major Molecular Response to Imatinib in Chronic Myeloid Leukemia Patients. Journal of Clinical Medicine, 11(20), 6217. https://doi.org/10.3390/jcm11206217






