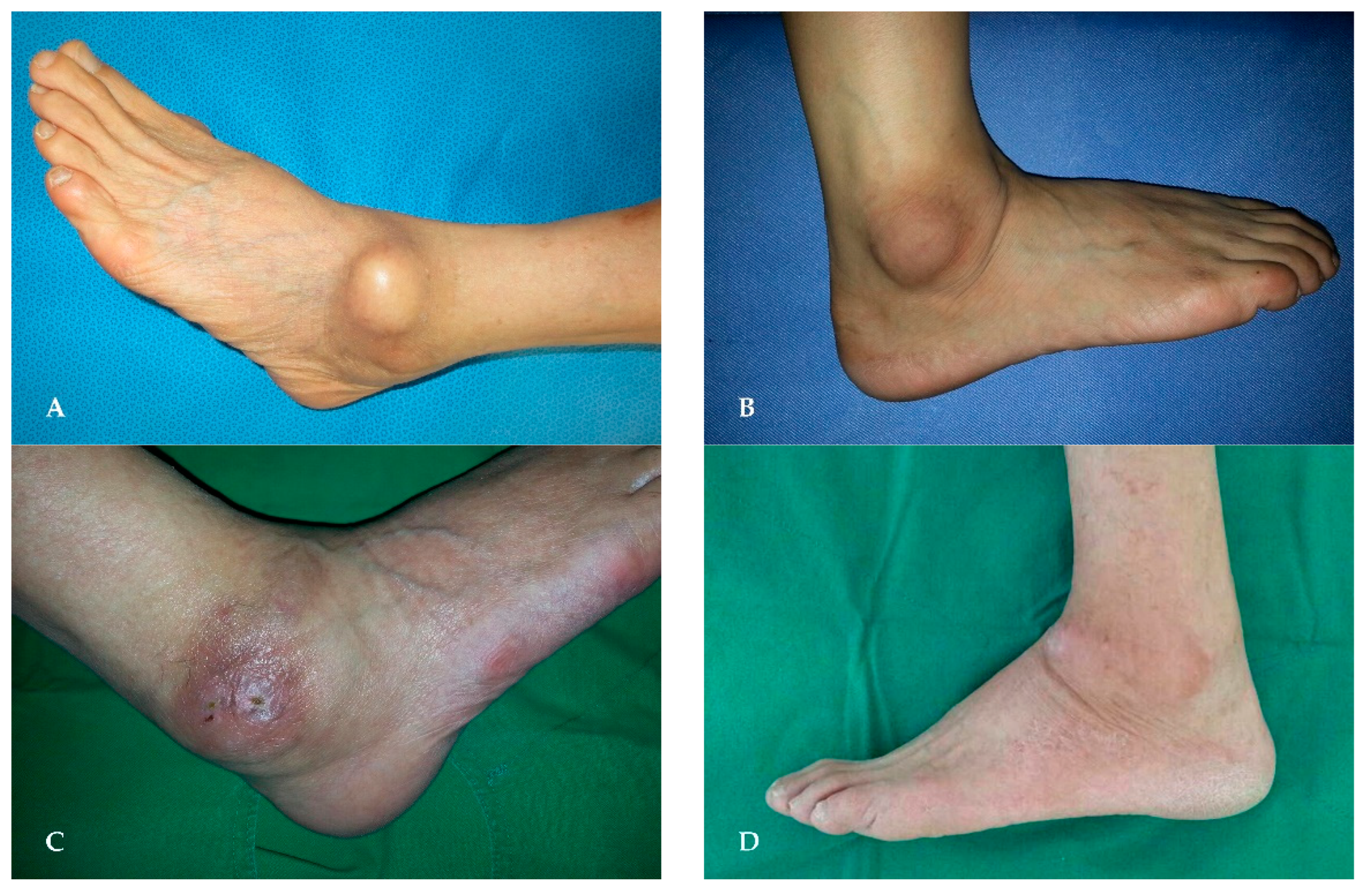
Characteristics of Synovial Fistula of the Ankle Joint: A Case Series
Abstract
1. Introduction
2. Materials and Methods
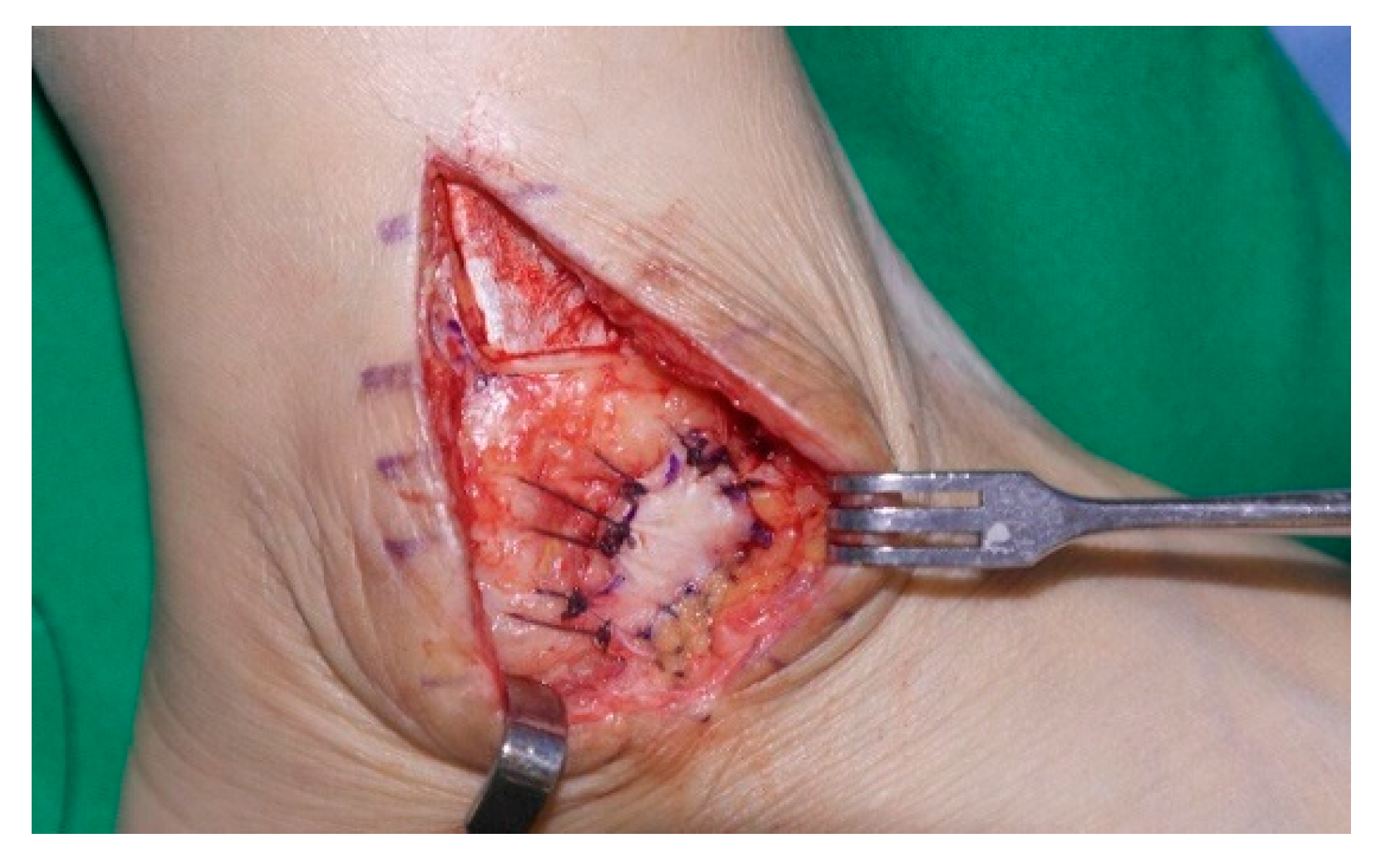
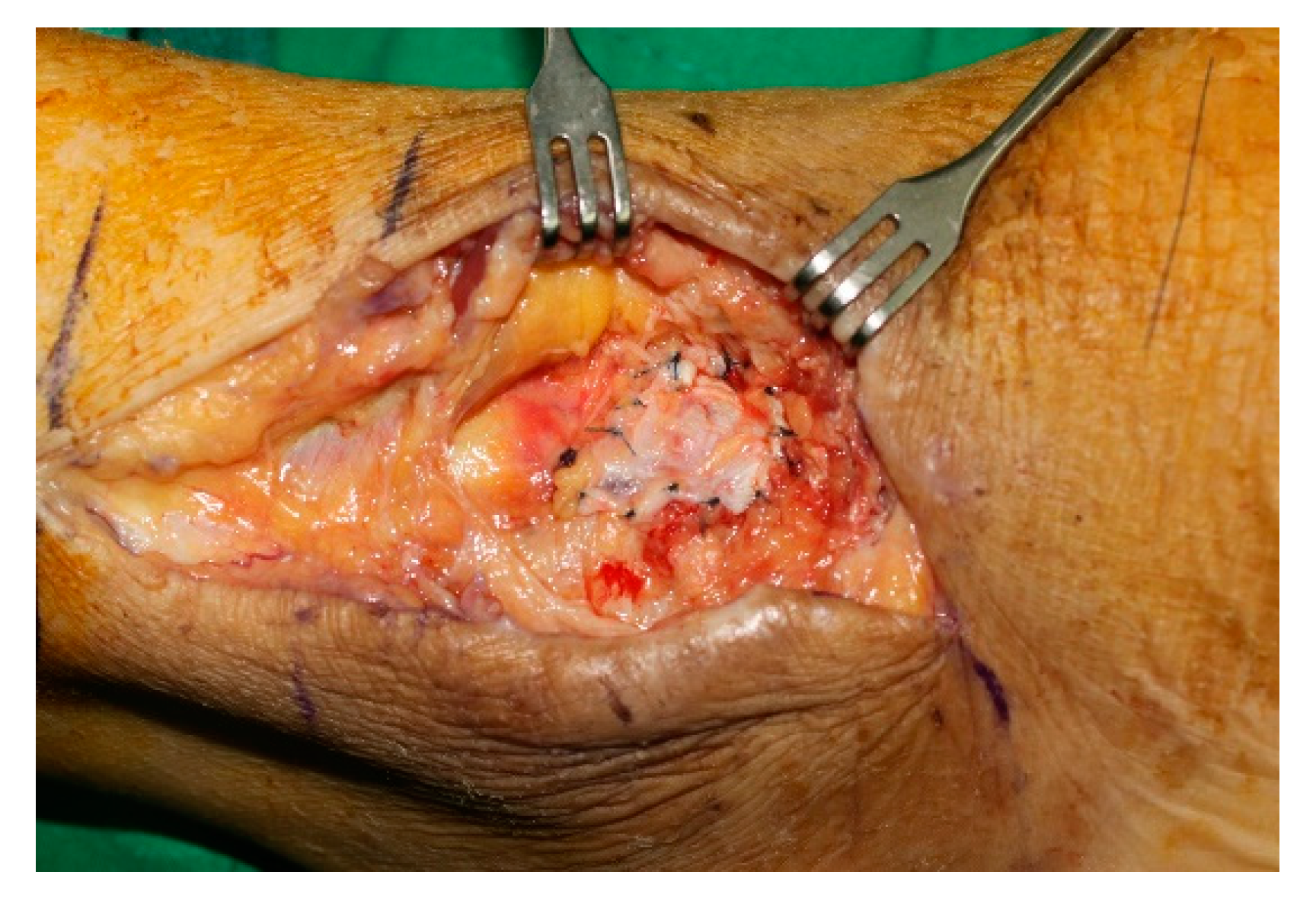
2.1. Surgical Technique
2.2. Postoperative Care
2.3. Statistical Analysis
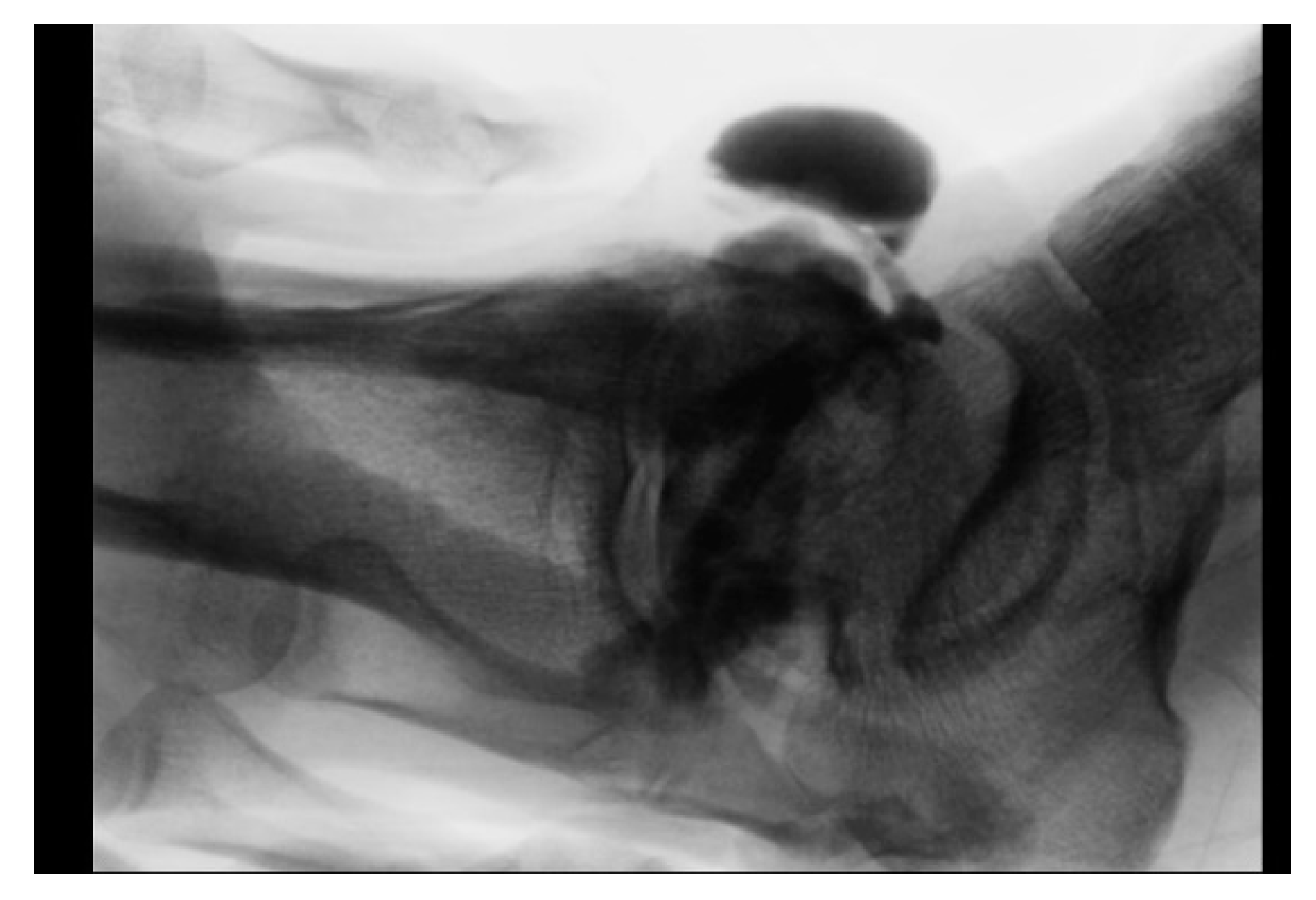
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, W.C.; Kim, J.H.; Song, J.K.; Moon, J.S. Fistula of the ankle: A complication of ankle sprain. J. Korean Foot Ankle Soc. 2002, 6, 261–264. [Google Scholar]
- Diduch, D.R.; Lee, G.P.; Barr, M. Traumatic articular-bursal fistula in a collegiate football player. Arthroscopy 2005, 21, 1266. [Google Scholar] [CrossRef] [PubMed]
- Feldmann, D.D.; Fanelli, G.C. Development of a synovial cyst following anterior cruciate ligament reconstruction. Arthroscopy 2001, 17, 200–202. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Varma, S.K. External synovial fistula of the knee joint and its treatment with free radial artery fasciocutaneous flap. Eur. J. Plast. Surg. 1999, 22, 190–192. [Google Scholar] [CrossRef]
- Park, K.H.; Kim, D.H.; Jang, S.W.; Ryu, J.H.; Ko, K.Y. Treatment of Recurrent Hemarthrosis Following Total Knee Arthroplasty Using Surgical Interventions. Clin. Orthop. Surg. 2021, 13, 152–159. [Google Scholar] [CrossRef]
- Proffer, D.S.; Drez, D., Jr.; Daus, G.P. Synovial fistula of the knee: A complication of arthroscopy. Arthroscopy 1991, 7, 98–100. [Google Scholar] [CrossRef]
- Smason, J.B. Post-traumatic fistula connecting prepatellar bursa with knee joint. Report of a case. J. Bone Jt. Surg. Am. 1972, 54, 1553–1554. [Google Scholar] [CrossRef]
- Huston, G.; Newman, R.J. Spontaneous rheumatoid fistula of the elbow joint. Postgrad. Med. J. 1990, 66, 674–676. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, D.; Lee, K.H.; Jo, Y.H.; Joo, I.H.; Lee, H.J.; Jeong, S.Y.; Lee, B.G. Correlation between Severity of Synovitis and Clinical Features in Rotator Cuff Tears. Clin. Orthop. Surg. 2021, 13, 88–96. [Google Scholar] [CrossRef]
- Richards, R.S.; Curl, L.A.; Moorman, C.T., 3rd; Mallon, W.J. Sterile synovio-cutaneous fistula: A potential complication of repair of large and massive rotator cuff tears. J. Shoulder Elbow Surg. 2006, 15, 436–439. [Google Scholar] [CrossRef]
- Shirley, D.S.; Mullet, H.; Stanley, J.K. Extensor tendon sheath fistula formation as a complication of wrist arthroscopy. Arthroscopy 2008, 24, 1311–1312. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.A.; Wright, T.W. Synovial cutaneous fistula of the shoulder after failed rotator cuff repair. Orthopedics 1999, 22, 1095–1097. [Google Scholar] [CrossRef] [PubMed]
- Naam, N.H. Flexor tenosynovial fistulas in the palm. J. Hand Surg. Am. 2012, 37, 925–929. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, N.V.; Hui, A. Persistent synovial fistula after arthroscopy in carbon synovitis. ANZ J. Surg. 2001, 71, 128–129. [Google Scholar] [CrossRef] [PubMed]
- Iveson, J.M.; Hill, A.G.; Wright, V. Wrist cysts and fistulae. An arthrographic study of the rheumatoid wrist. Ann. Rheum. Dis. 1975, 34, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Avci, S.; Sayli, U. Lateral premalleolar bursitis as a result of sitting on the foot. Foot Ankle Int. 2001, 22, 64–66. [Google Scholar] [CrossRef]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Park, J. Effect of Modified Brostrom Procedure with Periosteal Flap Augmentation after Subfibular Ossicle Excision on Ankle Stability. Foot Ankle Int. 2019, 40, 656–660. [Google Scholar] [CrossRef] [PubMed]
- Hussein ElGhamry, A. Peroneal tendofascial flap: A new fascial flap for Achilles tendon coverage, a preliminary report. Br. J. Plast. Surg. 2003, 56, 284–288. [Google Scholar] [CrossRef]
- Lee, K.; Jegal, H.; Chung, H.; Park, Y. Return to Play after Modified Brostrom Operation for Chronic Ankle Instability in Elite Athletes. Clin. Orthop. Surg. 2019, 11, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Snook, G.A.; Chrisman, O.D.; Wilson, T.C. Long-term results of the Chrisman-Snook operation for reconstruction of the lateral ligaments of the ankle. J. Bone Jt. Surg. Am. 1985, 67, 1–7. [Google Scholar] [CrossRef]
- Park, C.H.; Lee, W.C. Donor Site Morbidity after Lateral Ankle Ligament Reconstruction Using the Anterior Half of the Peroneus Longus Tendon Autograft. Am. J. Sports Med. 2017, 45, 922–928. [Google Scholar] [CrossRef] [PubMed]
- Yiannakopoulos, C.K. Diagnosis and treatment of postarthroscopic synovial knee fistulae: A report of four cases and review of the literature. J. Knee Surg. 2007, 20, 34–38. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Will, R.; Lubahn, J. Complications of open trigger finger release. J. Hand Surg. Am. 2010, 35, 594–596. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, S.; Hjorth Jensen, C. Arthroscopic treatment of impingement of the ankle reduces pain and enhances function. Scand. J. Med. Sci. Sports 2002, 12, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Bennett, R.M.; Hughes, G.R.; Bywaters, E.G.; Holt, P.J. Studies of a popliteal synovial fistula. Ann. Rheum. Dis. 1972, 31, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Odumala, O.O.; Ayekoloye, C.I.; Perera, S.D. Synovial knee fistula: A cause of prolonged morbidity. Arthroscopy 2001, 17, 640–641. [Google Scholar] [CrossRef] [PubMed]
- van Kampen, A.; Hinten, F. Diagnosis and treatment of postsurgical synovial fistula of the knee. J. Knee Surg. 2011, 24, 295–297. [Google Scholar] [CrossRef] [PubMed]
- Mendez-Fernandez, M.A. Treatment of chronic recurrent synovial fistulae with myofascial flaps. Br. J. Plast. Surg. 1993, 46, 303–306. [Google Scholar] [CrossRef]
- Shaw, A.D.; Ghosh, S.J.; Quaba, A.A. The island posterior calf fasciocutaneous flap: An alternative to the gastrocnemius muscle for cover of knee and tibial defects. Plast. Reconstr. Surg. 1998, 101, 1529–1536. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.; Ning, J.L.; Li, X.J.; Zhang, L.; Zuo, Z.B. Application of modified peroneal tendofascial compound flap with partial tendon of peroneal long muscle in lower leg refractory defects with Achilles tendon rupture. Zhonghua Zheng Xing Wai Ke Za Zhi 2010, 26, 107–109. [Google Scholar] [PubMed]
- Zuo, Z.B.; Cui, H.R.; Li, X.J.; Ning, J.L.; Tang, M.L.; Zhang, L.; Zhu, F. Anatomic study of peroneal tendofascial flap combined with adipofascial flap for the repair of heel tissue defects. Zhonghua Zheng Xing Wai Ke Za Zhi 2008, 24, 434–438. [Google Scholar] [PubMed]



| Scores | Mean | SD | Effect Size (Cohen’s D) | 95% Confidence Interval of the Difference | p Value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| VAS | −4.1 | 0.96 | 2.86 | −4.41 | −3.79 | <0.001 |
| AOFAS | 21.3 | 2.68 | 4.44 | 20.44 | 22.16 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, C.-H.; Park, J.J.; Woo, I.H.; Yan, H.; Lee, W.-C. Characteristics of Synovial Fistula of the Ankle Joint: A Case Series. J. Clin. Med. 2022, 11, 6215. https://doi.org/10.3390/jcm11206215
Park C-H, Park JJ, Woo IH, Yan H, Lee W-C. Characteristics of Synovial Fistula of the Ankle Joint: A Case Series. Journal of Clinical Medicine. 2022; 11(20):6215. https://doi.org/10.3390/jcm11206215
Chicago/Turabian StylePark, Chul-Hyun, Jeong Jin Park, In Ha Woo, Hongfei Yan, and Woo-Chun Lee. 2022. "Characteristics of Synovial Fistula of the Ankle Joint: A Case Series" Journal of Clinical Medicine 11, no. 20: 6215. https://doi.org/10.3390/jcm11206215
APA StylePark, C.-H., Park, J. J., Woo, I. H., Yan, H., & Lee, W.-C. (2022). Characteristics of Synovial Fistula of the Ankle Joint: A Case Series. Journal of Clinical Medicine, 11(20), 6215. https://doi.org/10.3390/jcm11206215







