Inflammatory Cytokines Associated with Diagnosis, Tumor Grade and Prognosis in Patients with Neuroendocrine Tumors
Abstract
1. Introduction
2. Materials and Methods
2.1. Design of Study and Patient Cohort
2.2. Imaging
2.3. Multiplex Evaluation of Serum Cytokines
2.4. Measurement of Standard of Care Biomarkers
2.5. Statistics
3. Results
3.1. Patient Characteristics
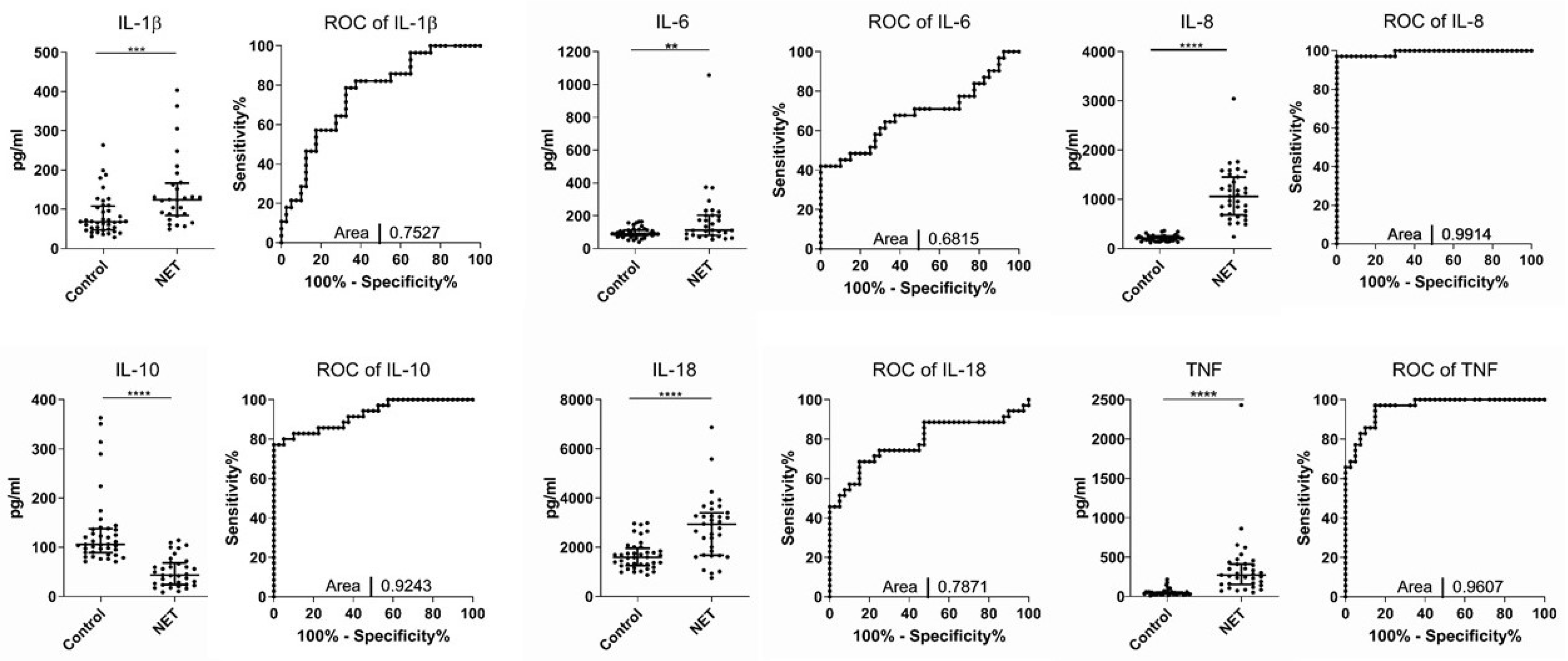
3.2. Serum Levels of IL-1β, IL-6, IL-8, IL-10, IL-18, and TNF Are Altered in Patients with Neuroendocrine Tumors
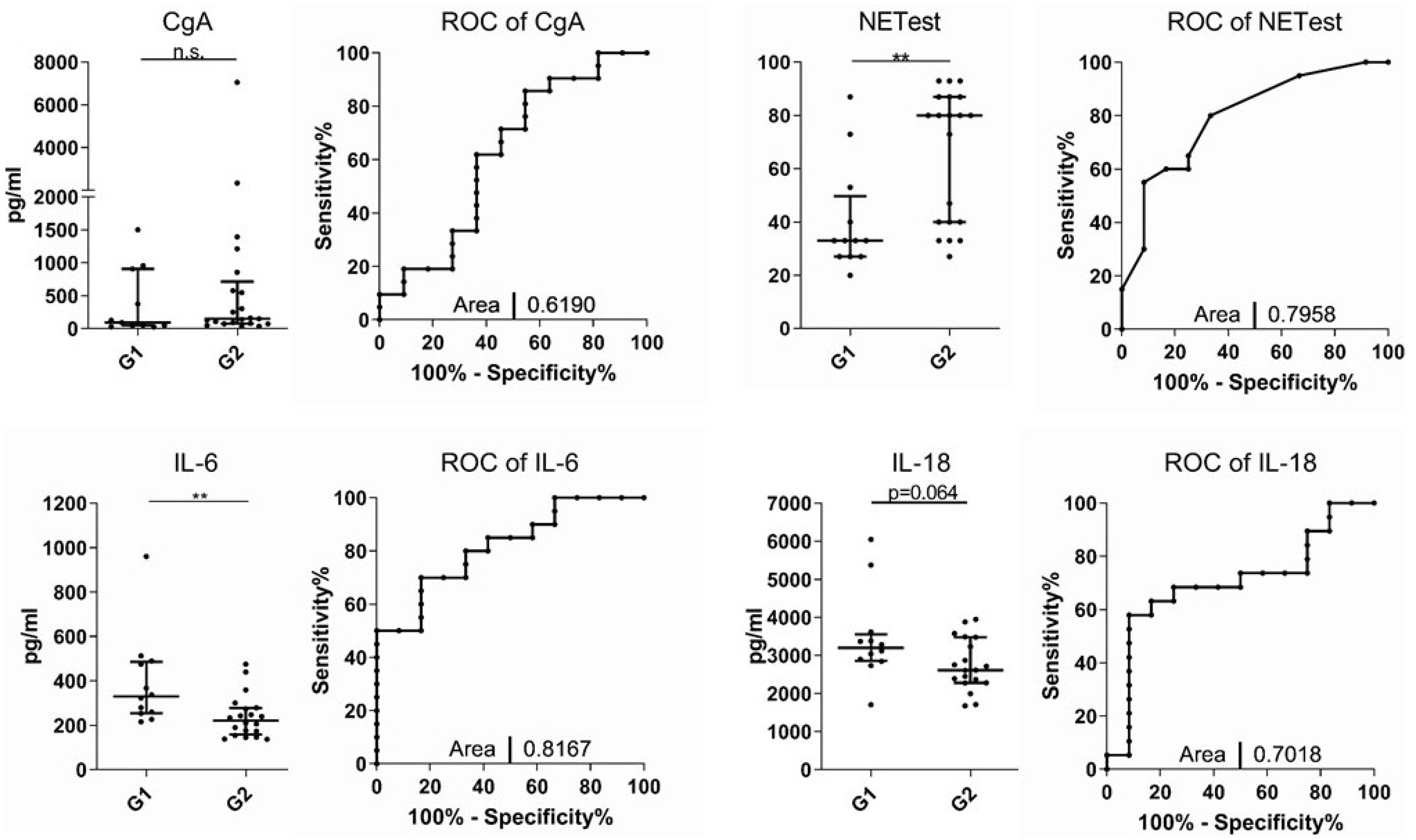
3.3. NETest and IL-6 Levels Can Discriminate between G1 and G2 NET
3.4. Tumor Localization Does Not Influence Inflammatory Cytokine Levels
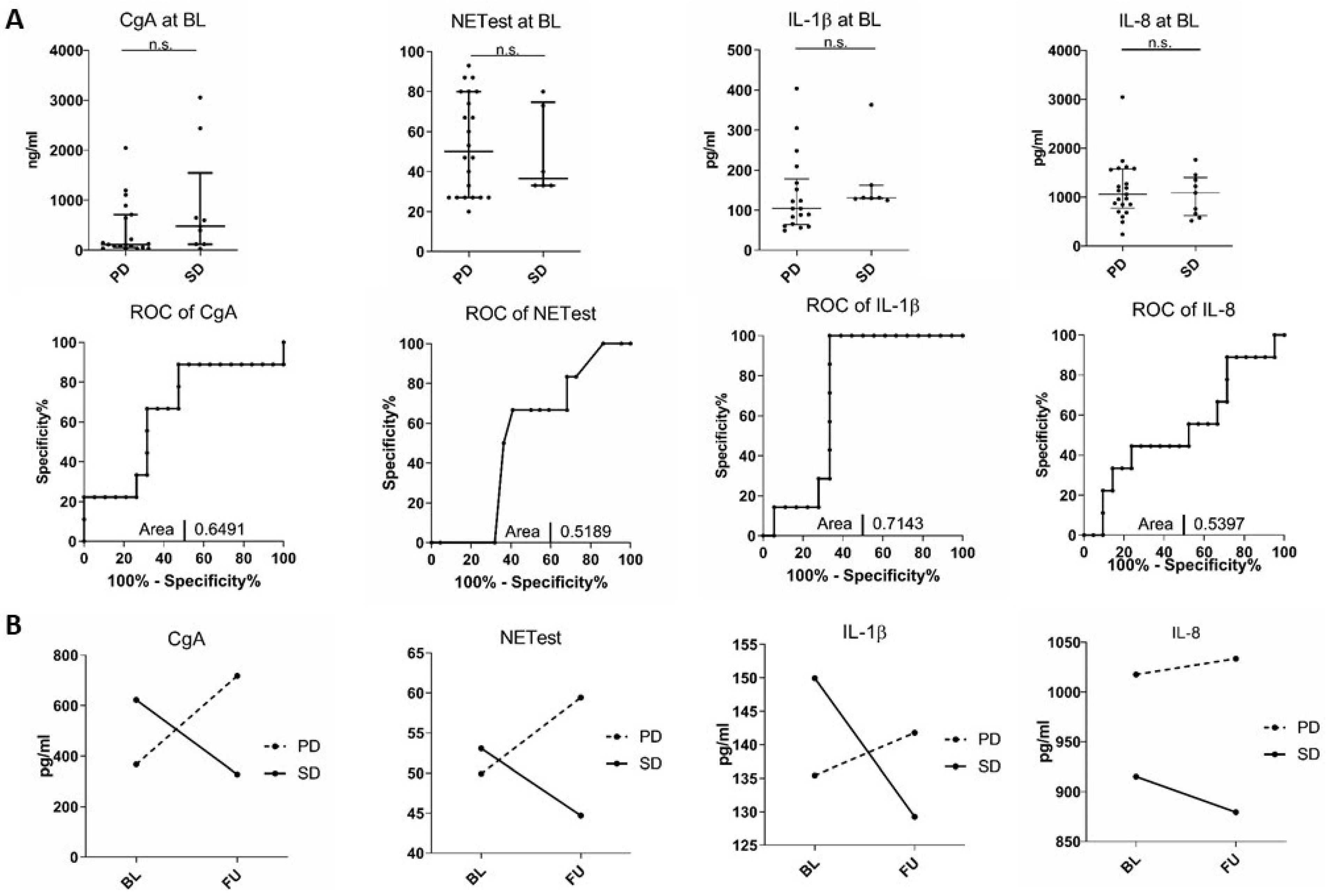
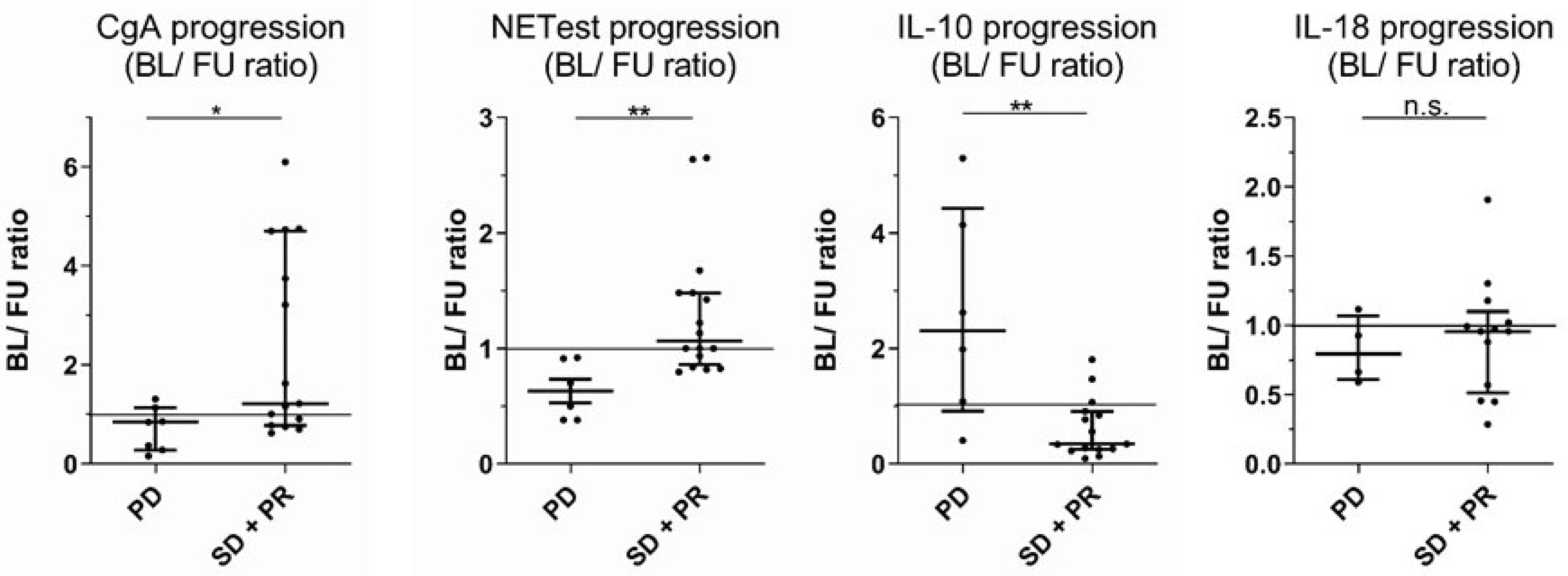
3.5. Inflammatory Cytokines Correlate with the Course of the Disease
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AUC | Area under the curve |
| CgA | Chromogranin A |
| cDNA | Complementary deoxyribonucleic acid |
| GEP | Gastroenteropancreatic |
| IL | Interleukin |
| INF | Interferon |
| IQR | Interquartile range |
| kDa | Kilodalton |
| MCP | Macrophage chemoattractant protein |
| mRNA | Messenger RNA |
| miRNA | MicroRNA |
| MRI | Magnetic resonance imaging |
| MSCT | Multi-slice computed tomography |
| NEC | Neuroendocrine carcinoma |
| NET | Neuroendocrine tumor |
| PCR | Polymerase chain reaction |
| PD | Progressive disease |
| ROC | Receiver-operating characteristic |
| SD | Stable disease |
| SSR | Somatostatin receptor |
| TemCap | Temozolomide plus Capecitabine |
| Th1 | T helper type 1 |
| TNF | Tumor necrosis factor |
| TRACE | Time-resolved amplified cryptate emission |
References
- Yao, J.C.; Hassan, M.; Phan, A.; Dagohoy, C.; Leary, C.; Mares, J.E.; Abdalla, E.K.; Fleming, J.B.; Vauthey, J.N.; Rashid, A.; et al. One hundred years after “carcinoid”: Epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J. Clin. Oncol. 2008, 26, 3063–3072. [Google Scholar] [CrossRef]
- Korse, C.M.; Taal, B.G.; van Velthuysen, M.L.; Visser, O. Incidence and survival of neuroendocrine tumours in the Netherlands according to histological grade: Experience of two decades of cancer registry. Eur. J. Cancer 2013, 49, 1975–1983. [Google Scholar] [CrossRef] [PubMed]
- Bosman, F.T.; Carneiro, F.; Hruban, R.H.; Theise, N.D. WHO Classification of Tumours of the Digestive System, 4th ed.; WHO Press: Geneva, Switzerland, 2010. [Google Scholar]
- Detjen, K.; Hammerich, L.; Ozdirik, B.; Demir, M.; Wiedenmann, B.; Tacke, F.; Jann, H.; Roderburg, C. Models of Gastroenteropancreatic Neuroendocrine Neoplasms: Current Status and Future Directions. Neuroendocrinology 2021, 111, 217–236. [Google Scholar] [CrossRef]
- Puliani, G.; Di Vito, V.; Feola, T.; Sesti, F.; Centello, R.; Pandozzi, C.; Tarsitano, M.G.; Verrico, M.; Lenzi, A.; Isidori, A.M.; et al. NETest: A Systematic Review Focusing on the Prognostic and Predictive Role. Neuroendocrinology 2021, 112, 523–536. [Google Scholar] [CrossRef] [PubMed]
- Dranoff, G. Cytokines in cancer pathogenesis and cancer therapy. Nat. Rev. Cancer 2004, 4, 11–22. [Google Scholar] [CrossRef]
- Cigrovski Berkovic, M.; Cacev, T.; Catela Ivkovic, T.; Zjacic-Rotkvic, V.; Kapitanovic, S. New insights into the role of chronic inflammation and cytokines in the etiopathogenesis of gastroenteropancreatic neuroendocrine tumors. Neuroendocrinology 2014, 99, 75–84. [Google Scholar] [CrossRef]
- Chang, K.T.; Tsai, C.M.; Chiou, Y.C.; Chiu, C.H.; Jeng, K.S.; Huang, C.Y. IL-6 induces neuroendocrine dedifferentiation and cell proliferation in non-small cell lung cancer cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 2005, 289, L446–L453. [Google Scholar] [CrossRef]
- Kumari, N.; Dwarakanath, B.S.; Das, A.; Bhatt, A.N. Role of interleukin-6 in cancer progression and therapeutic resistance. Tumor Biol. 2016, 37, 11553–11572. [Google Scholar] [CrossRef]
- Gregorc, V.; Spreafico, A.; Floriani, I.; Colombo, B.; Ludovini, V.; Pistola, L.; Bellezza, G.; Vigano, M.G.; Villa, E.; Corti, A. Prognostic value of circulating chromogranin A and soluble tumor necrosis factor receptors in advanced nonsmall cell lung cancer. Cancer 2007, 110, 845–853. [Google Scholar] [CrossRef]
- Cruceriu, D.; Baldasici, O.; Balacescu, O.; Berindan-Neagoe, I. The dual role of tumor necrosis factor-alpha (TNF-alpha) in breast cancer: Molecular insights and therapeutic approaches. Cell. Oncol. 2020, 43, 1–18. [Google Scholar] [CrossRef]
- Wang, L.; Du, F.; Wang, X. TNF-alpha induces two distinct caspase-8 activation pathways. Cell 2008, 133, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Mutala, L.B.; Deleine, C.; Karakachoff, M.; Dansette, D.; Ducoin, K.; Oger, R.; Rousseau, O.; Podevin, J.; Duchalais, E.; Fourquier, P.; et al. The Caspase-1/IL-18 Axis of the Inflammasome in Tumor Cells: A Modulator of the Th1/Tc1 Response of Tumor-Infiltrating T Lymphocytes in Colorectal Cancer. Cancers 2021, 13, 189. [Google Scholar] [CrossRef] [PubMed]
- Inoue, N.; Li, W.; Fujimoto, Y.; Matsushita, Y.; Katagiri, T.; Okamura, H.; Miyoshi, Y. High Serum Levels of Interleukin-18 Are Associated with Worse Outcomes in Patients with Breast Cancer. Anticancer Res. 2019, 39, 5009–5018. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.L.; Yao, J.C.; Carnaghi, C.; Buzzoni, R.; Herbst, F.; Ridolfi, A.; Strosberg, J.; Kulke, M.H.; Pavel, M.; Singh, S. Markers of Systemic Inflammation in Neuroendocrine Tumors: A Pooled Analysis of the RADIANT-3 and RADIANT-4 Studies. Pancreas 2021, 50, 130–137. [Google Scholar] [CrossRef]
- Zou, J.; Li, Q.; Kou, F.; Zhu, Y.; Lu, M.; Li, J.; Lu, Z.; Shen, L. Prognostic value of inflammation-based markers in advanced or metastatic neuroendocrine tumours. Curr. Oncol. 2019, 26, e30–e38. [Google Scholar] [CrossRef]
- Herman Mahecic, D.; Cigrovski Berkovic, M.; Zjacic-Rotkvic, V.; Cacev, T.; Kapitanovic, S.; Ulamec, M. Inflammation-related cytokines and their roles in gastroenteropancreatic neuroendocrine neoplasms. Bosn. J. Basic Med. Sci. 2020, 20, 445–450. [Google Scholar] [CrossRef]
- Modlin, I.M.; Drozdov, I.; Kidd, M. Gut neuroendocrine tumor blood qPCR fingerprint assay: Characteristics and reproducibility. Clin. Chem. Lab. Med. 2014, 52, 419–429. [Google Scholar] [CrossRef]
- Alvarez, M.J.; Subramaniam, P.S.; Tang, L.H.; Grunn, A.; Aburi, M.; Rieckhof, G.; Komissarova, E.V.; Hagan, E.A.; Bodei, L.; Clemons, P.A.; et al. A precision oncology approach to the pharmacological targeting of mechanistic dependencies in neuroendocrine tumors. Nat. Genet. 2018, 50, 979–989. [Google Scholar] [CrossRef]
- Kalligeros, M.; Diamantopoulos, L.; Toumpanakis, C. Biomarkers in Small Intestine NETs and Carcinoid Heart Disease: A Comprehensive Review. Biology 2021, 10, 950. [Google Scholar] [CrossRef]
- Kidd, M.; Bodei, L.; Modlin, I.M. Chromogranin A: Any relevance in neuroendocrine tumors? Curr. Opin. Endocrinol. Diabetes Obes. 2016, 23, 28–37. [Google Scholar] [CrossRef]
- Kovesdi, A.; Kurucz, P.A.; Nyiro, G.; Darvasi, O.; Patocs, A.; Butz, H. Circulating miRNA Increases the Diagnostic Accuracy of Chromogranin A in Metastatic Pancreatic Neuroendocrine Tumors. Cancers 2020, 12, 2488. [Google Scholar] [CrossRef] [PubMed]
- Hellberg, T.; Mohr, R.; Geisler, L.; Knorr, J.; Wree, A.; Demir, M.; Benz, F.; Lambrecht, J.; Loosen, S.H.; Tacke, F.; et al. Serum levels of miR-223 but not miR-21 are decreased in patients with neuroendocrine tumors. PLoS ONE 2020, 15, e0244504. [Google Scholar] [CrossRef] [PubMed]
- Soldevilla, B.; Lopez-Lopez, A.; Lens-Pardo, A.; Carretero-Puche, C.; Lopez-Gonzalvez, A.; La Salvia, A.; Gil-Calderon, B.; Riesco-Martinez, M.C.; Espinosa-Olarte, P.; Sarmentero, J.; et al. Comprehensive Plasma Metabolomic Profile of Patients with Advanced Neuroendocrine Tumors (NETs). Diagnostic and Biological Relevance. Cancers 2021, 13, 2634. [Google Scholar] [CrossRef] [PubMed]
- Detjen, K.M.; Otto, R.; Giesecke, Y.; Geisler, L.; Riemer, P.; Jann, H.; Grotzinger, C.; Sers, C.; Pascher, A.; Ludde, T.; et al. Elevated Flt3L Predicts Long-Term Survival in Patients with High-Grade Gastroenteropancreatic Neuroendocrine Neoplasms. Cancers 2021, 13, 4463. [Google Scholar] [CrossRef]
- Wei, M.; Xu, J.; Hua, J.; Meng, Q.; Liang, C.; Liu, J.; Zhang, B.; Wang, W.; Yu, X.; Shi, S. From the Immune Profile to the Immunoscore: Signatures for Improving Postsurgical Prognostic Prediction of Pancreatic Neuroendocrine Tumors. Front. Immunol. 2021, 12, 654660. [Google Scholar] [CrossRef]
- Van Gorp, H.; Lamkanfi, M. The emerging roles of inflammasome-dependent cytokines in cancer development. EMBO Rep. 2019, 20, e47575. [Google Scholar] [CrossRef]
- Mao, X.; Xu, J.; Wang, W.; Liang, C.; Hua, J.; Liu, J.; Zhang, B.; Meng, Q.; Yu, X.; Shi, S. Crosstalk between cancer-associated fibroblasts and immune cells in the tumor microenvironment: New findings and future perspectives. Mol. Cancer 2021, 20, 131. [Google Scholar] [CrossRef]
- Giannetta, E.; La Salvia, A.; Rizza, L.; Muscogiuri, G.; Campione, S.; Pozza, C.; Colao, A.A.L.; Faggiano, A. Are Markers of Systemic Inflammatory Response Useful in the Management of Patients with Neuroendocrine Neoplasms? Front. Endocrinol. 2021, 12, 672499. [Google Scholar] [CrossRef]
- Pozza, A.; Pauletti, B.; Scarpa, M.; Ruffolo, C.; Bassi, N.; Massani, M. Prognostic role of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with midgut neuroendocrine tumors undergoing resective surgery. Int. J. Color. Dis. 2019, 34, 1849–1856. [Google Scholar] [CrossRef]
- Bello, C.; Deprimo, S.E.; Friece, C.; Smeraglia, J.; Sherman, L.; Tye, L.; Baum, C.; Meropol, N.J.; Lenz, H.; Kulke, M.H. Analysis of circulating biomarkers of sunitinib malate in patients with unresectable neuroendocrine tumors (NET): VEGF, IL-8, and soluble VEGF receptors 2 and 3. J. Clin. Oncol. 2006, 24, 189s. [Google Scholar] [CrossRef]
- Yuan, A.; Chen, J.J.; Yao, P.L.; Yang, P.C. The role of interleukin-8 in cancer cells and microenvironment interaction. Front. Biosci. 2005, 10, 853–865. [Google Scholar] [CrossRef] [PubMed]
- Marques, P.; Barry, S.; Carlsen, E.; Collier, D.; Ronaldson, A.; Awad, S.; Dorward, N.; Grieve, J.; Mendoza, N.; Muquit, S.; et al. Chemokines modulate the tumour microenvironment in pituitary neuroendocrine tumours. Acta Neuropathol. Commun. 2019, 7, 172. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.B.; Ma, T.; Li, H.; Jin, X.L.; Xu, H.M. Expression and significance of intratumoral interleukin-12 and interleukin-18 in human gastric carcinoma. World J. Gastroenterol. 2007, 13, 1747–1751. [Google Scholar] [CrossRef] [PubMed]
- Gunel, N.; Coskun, U.; Sancak, B.; Gunel, U.; Hasdemir, O.; Bozkurt, S. Clinical importance of serum interleukin-18 and nitric oxide activities in breast carcinoma patients. Cancer 2002, 95, 663–667. [Google Scholar] [CrossRef] [PubMed]
- Alexandrakis, M.G.; Passam, F.H.; Sfiridaki, K.; Moschandrea, J.; Pappa, C.; Liapi, D.; Petreli, E.; Roussou, P.; Kyriakou, D.S. Interleukin-18 in multiple myeloma patients: Serum levels in relation to response to treatment and survival. Leuk. Res. 2004, 28, 259–266. [Google Scholar] [CrossRef]
- Kleiner, G.; Marcuzzi, A.; Zanin, V.; Monasta, L.; Zauli, G. Cytokine levels in the serum of healthy subjects. Mediat. Inflamm. 2013, 2013, 434010. [Google Scholar] [CrossRef]
- Elhousiny, M.; Miller, K.; Ariyawadana, A.; Nimmo, A. Identification of inflammatory mediators associated with metastasis of oral squamous cell carcinoma in experimental and clinical studies: Systematic review. Clin. Exp. Metastasis 2019, 36, 481–492. [Google Scholar] [CrossRef]
- Kang, J.S.; Bae, S.Y.; Kim, H.R.; Kim, Y.S.; Kim, D.J.; Cho, B.J.; Yang, H.K.; Hwang, Y.I.; Kim, K.J.; Park, H.S.; et al. Interleukin-18 increases metastasis and immune escape of stomach cancer via the downregulation of CD70 and maintenance of CD44. Carcinogenesis 2009, 30, 1987–1996. [Google Scholar] [CrossRef]
- Sheng, T.; Wang, B.; Wang, S.Y.; Deng, B.; Qu, L.; Qi, X.S.; Wang, X.L.; Deng, G.L.; Sun, X. The Relationship Between Serum Interleukin-6 and the Recurrence of Hepatitis B Virus Related Hepatocellular Carcinoma after Curative Resection. Medicine 2015, 94, e941. [Google Scholar] [CrossRef]
- Zhu, Y.; Liu, C.; Cui, Y.; Nadiminty, N.; Lou, W.; Gao, A.C. Interleukin-6 induces neuroendocrine differentiation (NED) through suppression of RE-1 silencing transcription factor (REST). Prostate 2014, 74, 1086–1094. [Google Scholar] [CrossRef]
- Saraiva, M.; O’Garra, A. The regulation of IL-10 production by immune cells. Nat. Rev. Immunol. 2010, 10, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Elenkov, I.J.; Chrousos, G.P.; Wilder, R.L. Neuroendocrine regulation of IL-12 and TNF-alpha/IL-10 balance. Clinical implications. Ann. N. Y. Acad. Sci. 2000, 917, 94–105. [Google Scholar] [CrossRef] [PubMed]
- Samiea, A.; Yoon, J.S.J.; Ong, C.J.; Zoubeidi, A.; Chamberlain, T.C.; Mui, A.L. Interleukin-10 Induces Expression of Neuroendocrine Markers and PDL1 in Prostate Cancer Cells. Prostate Cancer 2020, 2020, 5305306. [Google Scholar] [CrossRef] [PubMed]
| NET Cohort (A) | Control Cohort (B) | ||
|---|---|---|---|
| Age at initial sample (in years) Median/Range Female (Median/Range) Male (Median/Range) | 68.8/42.1–87.9 71.9/60.7–80.5 67/42.1–87.9 | Age at initial sample (in years) Median (Range) Female (Median/Range) Male (Median/Range) | 40/23–77 46/23–77 38/24–68 |
| Sex female male | 22 (51.2%) 21 (48.8%) | Sex female male | 10 (33.3%) 30 (66.6%) |
| Tumor location Illeum Pancreas | 23 (53.5%) 20 (46.5%) | ||
| Grading G1 G2 | 14 (32.6%) 29 (67.4%) | ||
| TNM stage II III IIIB IV | 1 (2.3%) 9 (20.9%) 2 (4.7%) 31 (72.1%) | ||
| Metastasis Lymph node only Distant metastasis | 9 (16%) 34 (84%) | ||
| Treatment at initial sample G1 therapy SSA OP G2 therapy SSA OP PRRT Everolimus Tem/Cap | 14 (100%) 11 (78.5%) 3 (21.4%) 29 (100%) 8 (27.6 %) 10 (34.4%) 1 (3.4%) 7 (24.1%) 3 (10.3) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Geisler, L.; Hellberg, T.; Lambrecht, J.; Jann, H.; Knorr, J.; Eschrich, J.; Loosen, S.H.; Wree, A.; Hammerich, L.; Krieg, A.; et al. Inflammatory Cytokines Associated with Diagnosis, Tumor Grade and Prognosis in Patients with Neuroendocrine Tumors. J. Clin. Med. 2022, 11, 6191. https://doi.org/10.3390/jcm11206191
Geisler L, Hellberg T, Lambrecht J, Jann H, Knorr J, Eschrich J, Loosen SH, Wree A, Hammerich L, Krieg A, et al. Inflammatory Cytokines Associated with Diagnosis, Tumor Grade and Prognosis in Patients with Neuroendocrine Tumors. Journal of Clinical Medicine. 2022; 11(20):6191. https://doi.org/10.3390/jcm11206191
Chicago/Turabian StyleGeisler, Lukas, Teresa Hellberg, Joeri Lambrecht, Henning Jann, Jana Knorr, Johannes Eschrich, Sven H. Loosen, Alexander Wree, Linda Hammerich, Andreas Krieg, and et al. 2022. "Inflammatory Cytokines Associated with Diagnosis, Tumor Grade and Prognosis in Patients with Neuroendocrine Tumors" Journal of Clinical Medicine 11, no. 20: 6191. https://doi.org/10.3390/jcm11206191
APA StyleGeisler, L., Hellberg, T., Lambrecht, J., Jann, H., Knorr, J., Eschrich, J., Loosen, S. H., Wree, A., Hammerich, L., Krieg, A., Luedde, T., Tacke, F., Roderburg, C., & Mohr, R. (2022). Inflammatory Cytokines Associated with Diagnosis, Tumor Grade and Prognosis in Patients with Neuroendocrine Tumors. Journal of Clinical Medicine, 11(20), 6191. https://doi.org/10.3390/jcm11206191









