Prognostic and Predictive Biomarkers in Patients with Locally Advanced Rectal Cancer (LARC) Treated with Preoperative Chemoradiotherapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
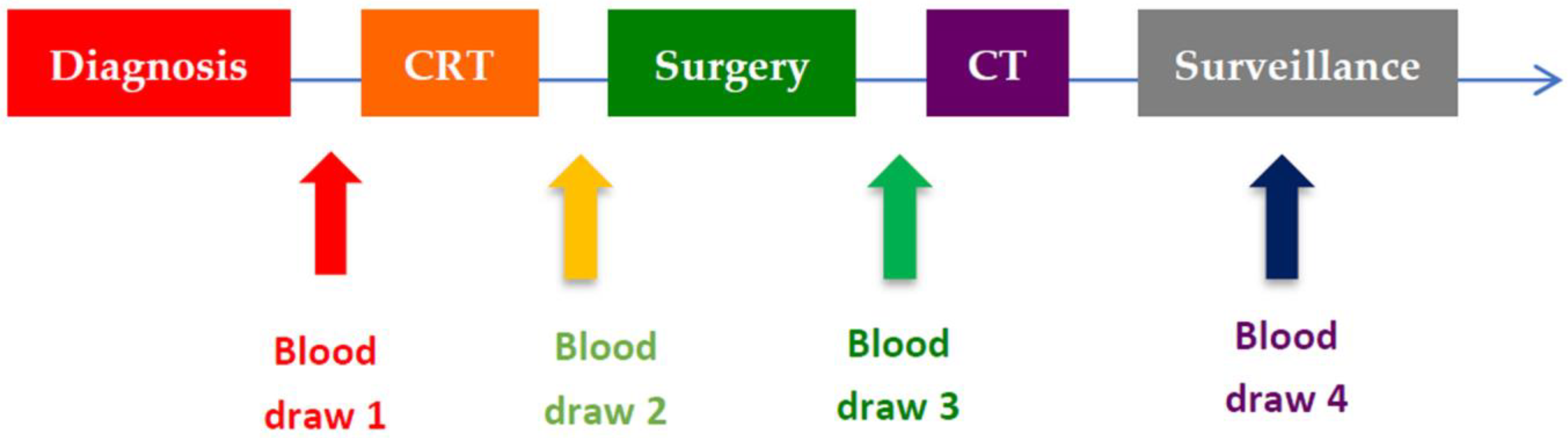
2.2. Treatment Protocol
2.3. Evaluation
2.4. Statistical Analysis
3. Results
3.1. Patients Characteristics
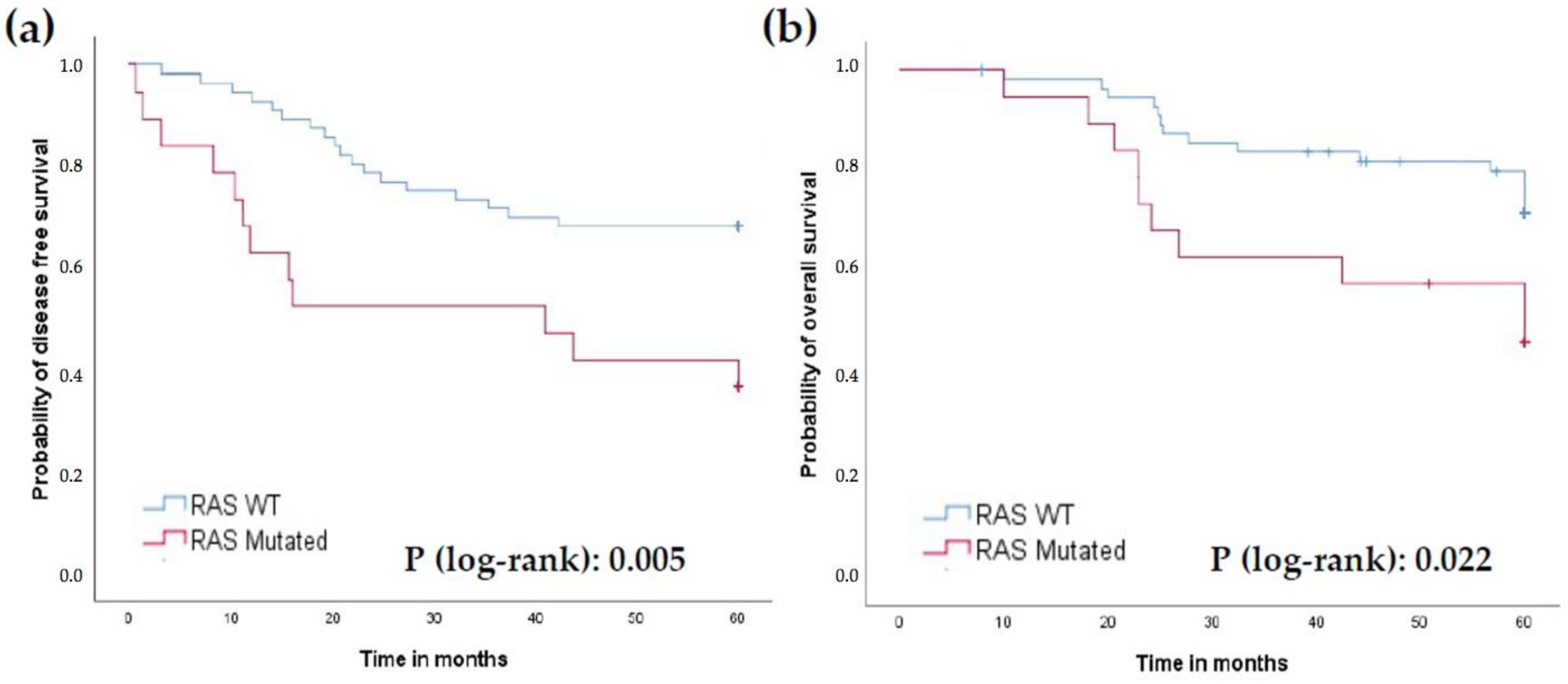
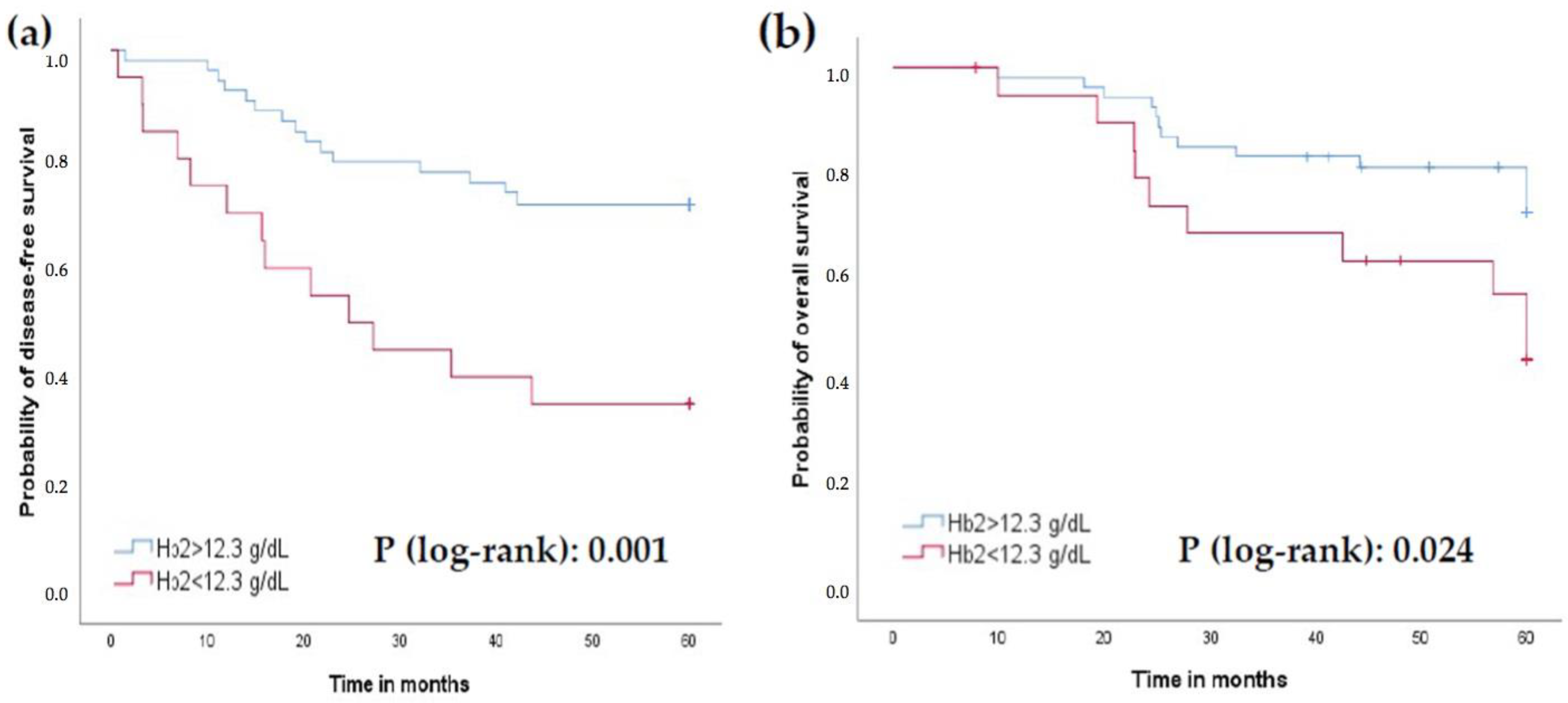
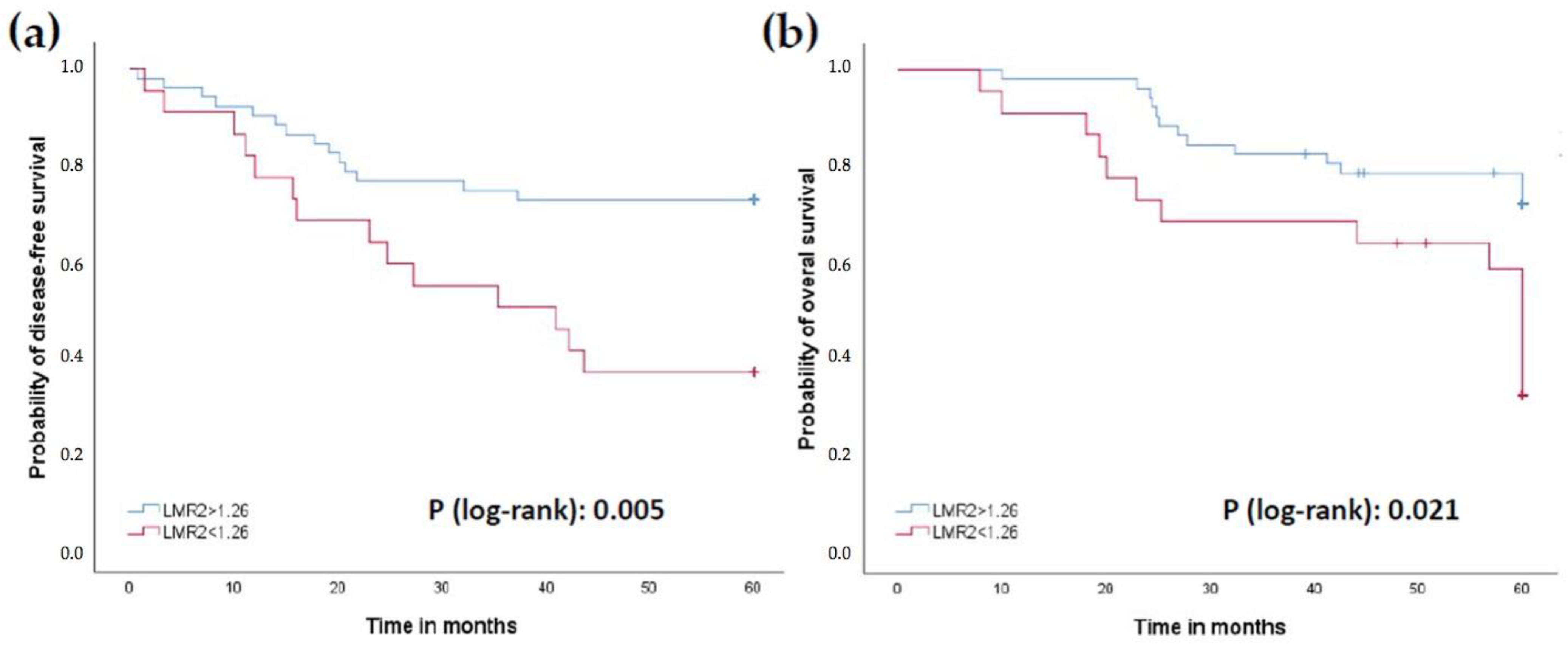
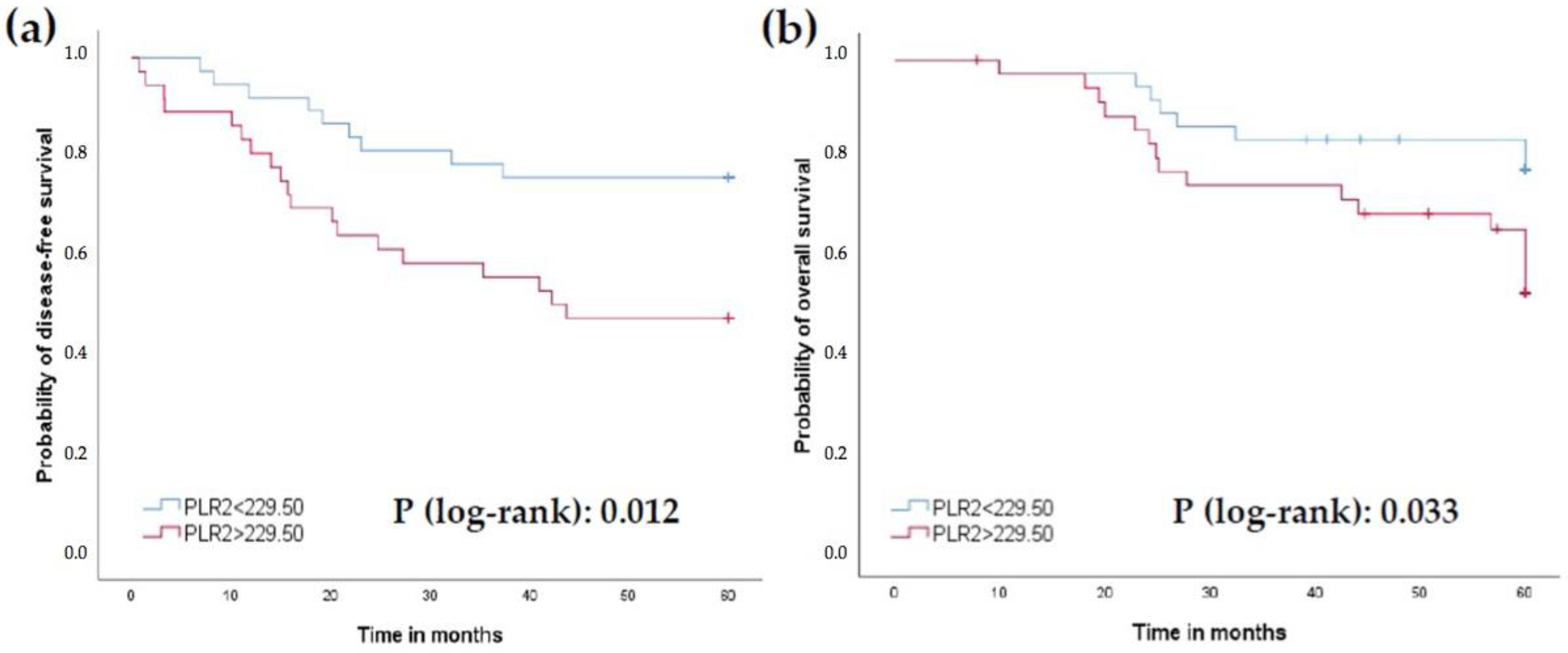
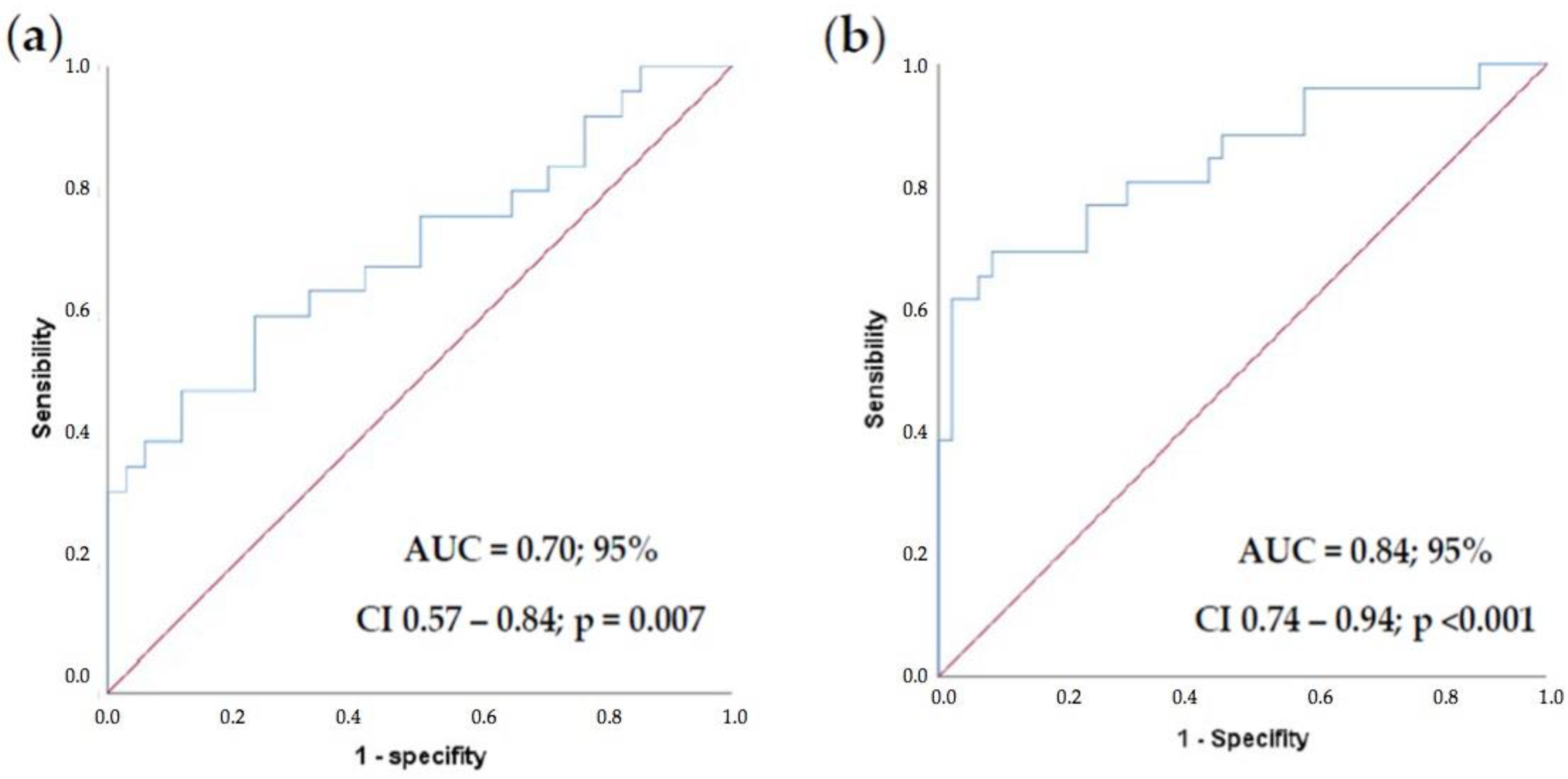
3.2. Prognosis Factors
3.3. Predictive Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Esti-mates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Sauer, R.; Becker, H.; Hohenberger, W.; Rödel, C.; Wittekind, C.; Fietkau, R.; Martus, P.; Tschmelitsch, J.; Hager, E.; Hess, C.F.; et al. Preoperative versus postoperative chemoradio-therapy for rectal cancer. N. Engl. J. Med. 2004, 351, 1731–1740. [Google Scholar] [CrossRef]
- Sauer, R.; Liersch, T.; Merkel, S.; Fietkau, R.; Hohenberger, W.; Hess, C.; Rödel, C. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: Results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J. Clin. Oncol. 2012, 30, 1926–1933. [Google Scholar] [CrossRef]
- Bosset, J.-F.; Collette, L.; Calais, G.; Mineur, L.; Maingon, P.; Radosevic-Jelic, L.; Daban, A.; Bardet, E.; Beny, A.; Ollier, J.-C. Chemotherapy with Preoperative Radiotherapy in Rectal Cancer. N. Engl. J. Med. 2006, 355, 1114–1123. [Google Scholar] [CrossRef]
- Rödel, C.; Martus, P.; Papadoupolos, T.; Füzesi, L.; Klimpfinger, M.; Fietkau, R.; Liersch, T.; Hohenberger, W.; Raab, R.; Sauer, R.; et al. Prognostic Significance of Tumor Regression After Preoperative Chemoradiotherapy for Rectal Cancer. J. Clin. Oncol. 2005, 23, 8688–8696. [Google Scholar] [CrossRef]
- Park, I.J.; You, Y.N.; Agarwal, A.; Skibber, J.M.; Rodriguez-Bigas, M.A.; Eng, C.; Feig, B.W.; Das, P.; Krishnan, S.; Crane, C.H.; et al. Neoadjuvant Treatment Response As an Early Response Indicator for Patients With Rectal Cancer. J. Clin. Oncol. 2012, 30, 1770–1776. [Google Scholar] [CrossRef]
- Fokas, E.; Liersch, T.; Fietkau, R.; Hohenberger, W.; Beissbarth, T.; Hess, C.; Becker, H.; Ghadimi, M.; Mrak, K.; Merkel, S.; et al. Tumor Regression Grading After Preoperative Chemoradiotherapy for Locally Advanced Rectal Carcinoma Revisited: Updated Results of the CAO/ARO/AIO-94 Trial. J. Clin. Oncol. 2014, 32, 1554–1562. [Google Scholar] [CrossRef]
- Fokas, E.; Ströbel, P.; Fietkau, R.; Ghadimi, M.; Liersch, T.; Grabenbauer, G.G.; Hartmann, A.; Kaufmann, M.; Sauer, R.; Graeven, U.; et al. Tumor Regression Grading After Preoperative Chemoradiotherapy as a Prognostic Factor and Individual-Level Surrogate for Disease-Free Survival in Rectal Cancer. J. Natl. Cancer Inst. 2017, 109, djx095. [Google Scholar] [CrossRef]
- Dworak, O.; Keilholz, L.; Hoffmann, A. Pathological features of rectal cancer after preoperative radiochemotherapy. Int. J. Color. Dis. 1997, 12, 19–23. [Google Scholar] [CrossRef]
- Mandard, A.M.; Dalibard, F.; Mandard, J.C.; Marnay, J.; Henry-Amar, M.; Petiot, J.F.; Roussel, A.; Jacob, J.H.; Segol, P.; Samama, G. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer 1994, 73, 2680–2686. [Google Scholar] [CrossRef]
- Ryan, R.; Gibbons, D.; Hyland, J.M.P.; Treanor, D.; White, A.; Mulcahy, H.E.; O’Donoghue, D.P.; Moriarty, M.; Fennelly, D.; Sheahan, K. Pathological response following long-course neo-adjuvant chemoradiotherapy for locally advanced rectal cancer. Histopathology 2005, 47, 141–146. [Google Scholar] [CrossRef]
- AJCC Cancer Staging Manual. Available online: https://link.springer.com/book/9783319406176 (accessed on 16 August 2022).
- Protocol for the Examination of Resection Specimens from Patients with Primary Carcinoma of the Colon and Rectum Version: Colon and Rectum Resection 4.1.0.0. Protocol Posting Date: February 2020. Available online: https://documents.cap.org/protocols/cp-gilower-colonrectum-resection-20-4100.pdf (accessed on 15 July 2021).
- Quah, H.; Chou, J.F.; Gonen, M.; Shia, J.; Schrag, D.; Saltz, L.; Goodman, K.A.; Minsky, B.D.; Wong, W.D.; Weiser, M.R. Pathologic stage is most prognostic of disease-free survival in locally advanced rectal cancer patients after preoperative chemoradiation. Cancer 2008, 113, 57–64. [Google Scholar] [CrossRef]
- Dayde, D.; Tanaka, I.; Jain, R.; Tai, M.C.; Taguchi, A. Predictive and Prognostic Molecular Biomarkers for Response to Neoadjuvant Chemoradiation in Rectal Cancer. Int. J. Mol. Sci. 2017, 18, 573. [Google Scholar] [CrossRef]
- Bedin, C.; Crotti, S.; D’Angelo, E.; D’Aronco, S.; Pucciarelli, S.; Agostini, M. Circulating Biomarkers for Response Prediction of Rectal Cancer to Neoadjuvant Chemoradiotherapy. Curr. Med. Chem. 2020, 27, 4274–4294. [Google Scholar] [CrossRef]
- Rodríguez-Tomàs, E.; Arenas, M.; Gómez, J.; Acosta, J.; Trilla, J.; López, Y.; Árquez, M.; Torres, L.; Araguas, P.; Hernández-Aguilera, A.; et al. Identification of potential metabolic biomarkers of rectal cancer and of the effect of neoadjuvant radiochemotherapy. PLoS ONE 2021, 16, e0250453. [Google Scholar] [CrossRef]
- Schisterman, E.F.; Perkins, N.J.; Liu, A.; Bondell, H. Optimal cut-point and its corresponding Youden Index to discriminate individuals using pooled blood samples. Epidemiol. Camb. Mass. 2005, 16, 73–81. [Google Scholar] [CrossRef]
- Rasmy, A.; Fayed, A.; Omar, A.; Fahmy, N. Effect of KRAS mutational status on disease behavior and treatment outcome in patients with metastatic colorectal cancer: Intratumor heterogeneity and mutational status. J. Gastrointest. Oncol. 2019, 10, 886–895. [Google Scholar] [CrossRef]
- Yang, J.; Lin, Y.; Huang, Y.; Jin, J.; Zou, S.; Zhang, X.; Li, H.; Feng, T.; Chen, J.; Zuo, Z.; et al. Genome landscapes of rectal cancer before and after preoperative chemo-radiotherapy. Theranostics 2019, 9, 6856–6866. [Google Scholar] [CrossRef]
- Jo, P.; Bernhardt, M.; Nietert, M.; König, A.; Azizian, A.; Schirmer, M.A.; Grade, M.; Kitz, J.; Reuter-Jessen, K.; Ghadimi, M.; et al. KRAS mutation status concordance between the primary tumor and the corresponding metastasis in patients with rectal cancer. PLoS ONE 2020, 15, e0239806. [Google Scholar] [CrossRef]
- Bahnassy, A.A.; Abdel-Azim, Y.A.; Ezzat, S.; Abdellateif, M.S.; Zekri, A.-R.N.; Mohanad, M.; Salama, A.; Khaled, H. The role of circulating tumor cells and K-ras mutations in patients with locally advanced rectal cancer: A prospective study. Mol. Biol. Rep. 2020, 47, 9645–9657. [Google Scholar] [CrossRef]
- Peng, J.; Lv, J.; Peng, J. KRAS mutation is predictive for poor prognosis in rectal cancer patients with neoadjuvant chemoradio-therapy: A systemic review and meta-analysis. Int. J. Colorectal. Dis. 2021, 36, 1781–1790. [Google Scholar] [CrossRef]
- Rades, D.; Kuhn, H.; Schultze, J.; Homann, N.; Brandenburg, B.; Schulte, R.; Krull, A.; Schild, S.E.; Dunst, J. Prognostic Factors Affecting Locally Recurrent Rectal Cancer and Clinical Significance of Hemoglobin. Int. J. Radiat. Oncol. 2008, 70, 1087–1093. [Google Scholar] [CrossRef]
- McGrane, J.M.; Humes, D.J.; Acheson, A.G.; Minear, F.; Wheeler, J.M.; Walter, C.J. Significance of Anemia in Outcomes After Neoadjuvant Chemoradiotherapy for Locally Advanced Rectal Cancer. Clin. Colorectal. Cancer. 2017, 16, 381–385. [Google Scholar] [CrossRef]
- Chan, J.C.Y.; Chan, D.L.; Diakos, C.I.; Engel, A.; Pavlakis, N.; Gill, A.; Clarke, S.J. The Lymphocyte-to-Monocyte Ratio is a Superior Predictor of Overall Survival in Comparison to Established Biomarkers of Resectable Colorectal Cancer. Ann. Surg. 2017, 265, 539–546. [Google Scholar] [CrossRef]
- Tan, D.; Fu, Y.; Tong, W.; Li, F. Prognostic significance of lymphocyte to monocyte ratio in colorectal cancer: A meta-analysis. Int. J. Surg. 2018, 55, 128–138. [Google Scholar] [CrossRef]
- Yamamoto, A.; Toiyama, Y.; Okugawa, Y.; Oki, S.; Ide, S.; Saigusa, S.; Araki, T.; Kusunoki, M. Clinical Implications of Pretreatment: Lympho-cyte-to-Monocyte Ratio in Patients With Rectal Cancer Receiving Preoperative Chemoradiotherapy. Dis. Colon. Rectum. 2019, 62, 171–180. [Google Scholar] [CrossRef]
- Gui, W.; Wang, X.; Luo, Y.; Wang, J. Platelet to lymphocyte ratio as a prognostic factor in patients with advanced colorectal cancer undergoing palliative treatment. Ann. Palliat. Med. 2020, 9, 3271–3277. [Google Scholar] [CrossRef]
- Ergen, Ş.A.; Barlas, C.; Yıldırım, C.; Öksüz, D.Ç. Prognostic Role of Peripheral Neutrophil-Lymphocyte Ratio (NLR) and Platelet-Lymphocyte Ratio (PLR) in Patients with Rectal Cancer Undergoing Neoadjuvant Chemoradiotherapy. J. Gastrointest. Cancer 2022, 53, 151–160. [Google Scholar] [CrossRef]
- Ke, T.-M.; Lin, L.-C.; Huang, C.-C.; Chien, Y.-W.; Ting, W.-C.; Yang, C.-C. High neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio predict poor survival in rectal cancer patients receiving neoadjuvant concurrent chemoradiotherapy. Medicine 2020, 99, e19877. [Google Scholar] [CrossRef]
- Dudani, S.; Marginean, H.; Tang, P.A.; Monzon, J.G.; Raissouni, S.; Asmis, T.R.; Goodwin, R.A.; Gotfrit, J.; Cheung, W.Y.; Vickers, M.M. Neutrophil-to-lymphocyte and plate-let-to-lymphocyte ratios as predictive and prognostic markers in patients with locally advanced rectal cancer treated with neoadjuvant chemoradiation. BMC Cancer 2019, 19, 664. [Google Scholar] [CrossRef]
- Li, Z.; Zhao, R.; Cui, Y.; Zhou, Y.; Wu, X. The dynamic change of neutrophil to lymphocyte ratio can predict clinical outcome in stage I–III colon cancer. Sci. Rep. 2018, 8, 9453. [Google Scholar] [CrossRef]
- Ashizawa, N.; Furuya, S.; Katsutoshi, S.; Sudo, M.; Akaike, H.; Hosomura, N.; Kawaguchi, Y.; Amemiya, H.; Kawaida, H.; Inoue, S.; et al. Clinical Significance of Dynamic Neutrophil-lymphocyte Ratio Changes in Patients with Colorectal Cancer. Anticancer Res. 2020, 40, 2311–2317. [Google Scholar] [CrossRef]
- Nemoto, T.; Endo, S.; Isohata, N.; Takayanagi, D.; Nemoto, D.; Aizawa, M.; Utano, K.; Togashi, K. Change in the neutrophil-to-lymphocyte ratio during chemotherapy may predict prognosis in patients with advanced or metastatic colorectal cancer. Mol. Clin. Oncol. 2021, 14, 107. [Google Scholar] [CrossRef]
- Herold, Z.; Herold, M.; Lohinszky, J.; Szasz, A.M.; Dank, M.; Somogyi, A. Longitudinal changes in personalized platelet count metrics are good indicators of initial 3-year outcome in colorectal cancer. World J. Clin. Cases 2022, 10, 6825–6844. [Google Scholar] [CrossRef]
- McCoy, M.J.; Hemmings, C.; Hillery, S.; Penter, C.; Bulsara, M.K.; Zeps, N.; Platell, C.F. Neoadjuvant chemoradiotherapy for rectal cancer: How important is tumour regression? ANZ J. Surg. 2017, 87, E233–E239. [Google Scholar] [CrossRef]
- Xu, L.; Cai, S.; Xiao, T.; Chen, Y.; Qiu, H.; Wu, B.; Lin, G.; Sun, X.; Lu, J.; Zhou, W.; et al. Prognostic significance of tumour regression grade after neoadjuvant chemo-radiotherapy for a cohort of patients with locally advanced rectal cancer: An 8-year retrospective single-institutional study. Color. Dis. 2017, 19, O263–O271. [Google Scholar] [CrossRef]
- Tominaga, T.; Akiyoshi, T.; Yamamoto, N.; Oba, K.; Nagasaki, T.; Yamaguchi, T.; Konishi, T.; Fukunaga, Y.; Ueno, M. Prognostic value of metastatic lymph node regression grade after neoadjuvant chemoradiotherapy in patients with locally advanced rectal cancer. Surgery 2019, 166, 1061–1067. [Google Scholar] [CrossRef]
- Gao, C.; Fang, L.; Li, J.-T.; Zhao, H.-C. Significance and prognostic value of increased serum direct bilirubin level for lymph node metastasis in Chinese rectal cancer patients. World J. Gastroenterol. 2016, 22, 2576–2584. [Google Scholar] [CrossRef]
- Gao, C.; Li, J.-T.; Fang, L.; Wen, S.-W.; Zhang, L.; Zhao, H.-C. Pre-operative Predictive Factors for Intra-operative Pathological Lymph Node Metastasis in Rectal Cancers. Asian Pac. J. Cancer Prev. 2013, 14, 6293–6299. [Google Scholar] [CrossRef]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef]
- Hardiman, K.M.; Ulintz, P.J.; Kuick, R.D.; Hovelson, D.; Gates, C.M.; Bhasi, A.; Grant, A.; Liu, J.; Cani, A.K.; Greenson, J.K.; et al. Intra-tumor genetic heterogeneity in rectal cancer. Lab. Investig. 2016, 96, 4–15. [Google Scholar] [CrossRef]
- Frydrych, L.M.; Ulintz, P.; Bankhead, A.; Sifuentes, C.; Greenson, J.; Maguire, L.; Irwin, R.; Fearon, E.R.; Hardiman, K.M. Rectal cancer sub-clones respond differentially to neoadjuvant therapy. Neoplasia 2019, 21, 1051–1062. [Google Scholar] [CrossRef]
| Factor | Relapse Group | No Relapse Group | p-Value |
|---|---|---|---|
| Number of patients, n (%) | 31 (40) | 46 (60) | |
| Age at diagnosis (median/sd) | 63.5/9.5 | 61.7/10.5 | 0.445 |
| Male:Female (n) | 23:8 | 34:12 | 1.000 |
| cTNM ≥ T3N0, n (%) | 29 (40) | 44 (60) | 1.000 |
| MSI, n (%) | 2 (22) | 7 (78) | 0.301 |
| KRAS mutations, n (%) | 12 (63) | 7 (37) | 0.028 |
| Low LARC (0–5 cm), n (%) | 11 (34) | 22 (66) | 0.350 |
| Medium LARC (6–10 cm), n (%) | 15 (43) | 20 (57) | 0.816 |
| Upper LARC (11–15 cm), n (%) | 5 (56) | 4 (44) | 0.472 |
| Smoking history, n (%) | 16 (39) | 25 (61) | 0.821 |
| CEA levels, ng/mL (median/sd) | 14.9/18.3 | 7.4/13.6 | 0.057 |
| Neoadjuvant 5-FU/LVci, n (%) | 20 (38) | 32 (62) | 0.619 |
| TDSNT, days (mean/sd) | 53.1/18.7 | 54.3/15.9 | 0.762 |
| TENTS, days (mean/sd) | 48.4/9.2 | 47.6/11.3 | 0.732 |
| TDS, days (mean/sd) | 140.8/22.6 | 141.2/21.4 | 0.943 |
| TSAC, days (mean/sd) | 59.7/38.0 | 46.33/17.1 | 0.112 |
| APA, n (%) | 16 (48) | 17 (52) | 0.236 |
| ypTNM ≥ T3N0, n (%) | 20 (56) | 16 (44) | 0.019 |
| TRG0, n (%) | 2 (29) | 5 (71) | 0.703 |
| TRG1, n (%) | 7 (33) | 14 (67) | 0.791 |
| TRG2, n (%) | 11 (33) | 22 (67) | 0.630 |
| TRG3, n (%) | 8 (62) | 5 (38) | 0.065 |
| EMVI, n (%) | 6 (75) | 2 (25) | 0.048 |
| Lymphatic invasion, n (%) | 7 (78) | 2 (12) | 0.023 |
| Perineural invasion, n (%) | 13 (87) | 2 (13) | <0.001 |
| Lymph node involved, n (%) | 14 (70) | 6 (30) | 0.001 |
| Positive lymph nodes (mean/sd) | 3/5.8 | 0.3/1.2 | 0.001 |
| Resected lymph nodes (mean/sd) | 10.0/7.0 | 8.8/5.5 | 0.600 |
| Characteristics | Relapse Group | No Relapse Group | p-Value |
|---|---|---|---|
| Leukocyte 1, c/mm3 (mean/sd) | 8146.0/3413.2 | 7697.5/1914.1 | 0.930 |
| Leukocyte 2, c/mm3 (mean/sd) | 5927.1/3491.2 | 5195.5/1277.0 | 0.781 |
| Leukocyte 3, c/mm3 (mean/sd) | 6448.1/2129.8 | 6733.3/2567.8 | 0.754 |
| Leukocyte 4, c/mm3 (mean/sd) | 5305/1599.1 | 5488.1/1755.5 | 0.694 |
| Neutrophil 1, c/mm3 (mean/sd) | 5124.6/2872.8 | 4500/1390.6 | 0.493 |
| Neutrophil 2, c/mm3 (mean/sd) | 4262.5/3173.8 | 3364.4/1085.0 | 0.812 |
| Neutrophil 3, c/mm3 (mean/sd) | 4576.6/1887.2 | 4912.1/2500.6 | 0.839 |
| Neutrophil 4, c/mm3 (mean/sd) | 3555/1396.4 | 3590.4/1535.2 | 0.898 |
| Lymphocyte 1, c/mm3 (mean/sd) | 2140/798.2 | 2300/850.6 | 0.437 |
| Lymphocyte 2, c/mm3 (mean/sd) | 859.2/382.0 | 1051.1/486.4 | 0.076 |
| Lymphocyte 3, c/mm3 (mean/sd) | 1007.0/529.0 | 1004.0/506.0 | 0.981 |
| Lymphocyte 4, c/mm3 (mean/sd) | 1070/432.9 | 1178.5/481.1 | 0.395 |
| Monocyte 1, c/mm3 (mean/sd) | 654.6/256.9 | 630/224.4 | 0.746 |
| Monocyte 2, c/mm3 (mean/sd) | 599.6/236.0 | 520/173.9 | 0.267 |
| Monocyte 3, c/mm3 (mean/sd) | 592.2/298.8 | 579.0/188.9 | 0.433 |
| Monocyte 4, c/mm3 (mean/sd) | 490/137.2 | 535.7/193.5 | 0.451 |
| Hemoglobin 1, g/dL (mean/sd) | 13.3/1.9 | 14.1/1.6 | 0.055 |
| Hemoglobin 2, g/dL (mean/sd) | 12.5/1.7 | 13.5/1.3 | 0.008 |
| Hemoglobin 3, g/dL (mean/sd) | 10.9/1.5 | 11.9/1.5 | 0.007 |
| Hemoglobin 4, g/dL (mean/sd) | 13.4/1.7 | 13.4/1.3 | 0.792 |
| Platelets 1, c/mm3 (mean/sd) | 267,285.7/114,369.7 | 238,700/53,993.4 | 0.231 |
| Platelets 2, c/mm3 (mean/sd) | 264,428.5/133,926.5 | 206,844.4/40,279.6 | 0.200 |
| Platelets 3, c/mm3 (mean/sd) | 326,851.8/144,934.3 | 272,285.7/97,952.2 | 0.176 |
| Platelets 4, c/mm3 (mean/sd) | 205,100/78,874.9 | 201,119.0/41,163.0 | 0.834 |
| Characteristics | Relapse Group | No Relapse Group | p-Value |
|---|---|---|---|
| Neutrophil-Lymphocyte Ratio 1 (mean/sd) | 2.5/1.2 | 2.2/1.3 | 0.118 |
| Neutrophil-Lymphocyte Ratio 2 (mean/sd) | 5.8/4.7 | 3.8/2.2 | 0.075 |
| Neutrophil-Lymphocyte Ratio 3 (mean/sd) | 5.9/4.1 | 6.4/5.4 | 0.912 |
| Neutrophil-Lymphocyte Ratio 4 (mean/sd) | 3.8/2.0 | 3.5/2.2 | 0.503 |
| Lymphocyte-Monocyte Ratio 1 (mean/sd) | 3.5/1.6 | 3.8/1.4 | 0.448 |
| Lymphocyte-Monocyte Ratio 2 (mean/sd) | 1.5/0.6 | 2.2/1.5 | 0.011 |
| Lymphocyte-Monocyte Ratio 3 (mean/sd) | 1.8/0.8 | 1.8/0.8 | 0.956 |
| Lymphocyte-Monocyte Ratio 4 (mean/sd) | 2.2/0.8 | 2.4/1.3 | 0.786 |
| Platelet-Lymphocyte Ratio 1 (mean/sd) | 137.8/68.4 | 117.9/54.2 | 0.206 |
| Platelet-Lymphocyte Ratio 2 (mean/sd) | 386.2/290.9 | 236.4/114.7 | 0.029 |
| Platelet-Lymphocyte Ratio 3 (mean/sd) | 386.3/213.6 | 331.5/187.8 | 0.238 |
| Platelet-Lymphocyte Ratio 4 (mean/sd) | 217.5/103.1 | 200.9/89.7 | 0.519 |
| Predictor | Β | SE β | Χ2 | p | OR | 95%CI | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| KRAS status | 0.803 | 1.047 | 0.588 | 0.443 | 2.232 | 0.287 | 17.381 |
| EMVI | 1.382 | 2.269 | 0.371 | 0.543 | 3.983 | 0.047 | 340.268 |
| LVI | −0.946 | 2.578 | 0.135 | 0.714 | 0.388 | 0.002 | 60.708 |
| PNI | 3.282 | 1.261 | 6.775 | 0.009 | 26.619 | 2.249 | 315.037 |
| ypN | 3.461 | 1.287 | 7.230 | 0.007 | 31.851 | 2.555 | 397.000 |
| Hb2 < 12.3 | 2.006 | 1.017 | 3.892 | 0.049 | 7.432 | 1.013 | 54.509 |
| LMR2 < 1.26 | 1.827 | 0.877 | 4.343 | 0.037 | 6.214 | 1.115 | 34.636 |
| PLR2 > 229.50 | 1.867 | 1.006 | 3.448 | 0.063 | 6.469 | 0.901 | 46.425 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martín-Carnicero, A.; Ramalle-Gomara, E.; Rubio-Mediavilla, S.; Alonso-Lago, M.; Zorrilla-Larraga, M.; Manrique-Abós, I.; de las Heras-Dueña, M.E.; Larrayoz, I.M.; Martínez, A. Prognostic and Predictive Biomarkers in Patients with Locally Advanced Rectal Cancer (LARC) Treated with Preoperative Chemoradiotherapy. J. Clin. Med. 2022, 11, 6091. https://doi.org/10.3390/jcm11206091
Martín-Carnicero A, Ramalle-Gomara E, Rubio-Mediavilla S, Alonso-Lago M, Zorrilla-Larraga M, Manrique-Abós I, de las Heras-Dueña ME, Larrayoz IM, Martínez A. Prognostic and Predictive Biomarkers in Patients with Locally Advanced Rectal Cancer (LARC) Treated with Preoperative Chemoradiotherapy. Journal of Clinical Medicine. 2022; 11(20):6091. https://doi.org/10.3390/jcm11206091
Chicago/Turabian StyleMartín-Carnicero, Alfonso, Enrique Ramalle-Gomara, Susana Rubio-Mediavilla, Martina Alonso-Lago, Miriam Zorrilla-Larraga, Isabel Manrique-Abós, María E. de las Heras-Dueña, Ignacio M. Larrayoz, and Alfredo Martínez. 2022. "Prognostic and Predictive Biomarkers in Patients with Locally Advanced Rectal Cancer (LARC) Treated with Preoperative Chemoradiotherapy" Journal of Clinical Medicine 11, no. 20: 6091. https://doi.org/10.3390/jcm11206091
APA StyleMartín-Carnicero, A., Ramalle-Gomara, E., Rubio-Mediavilla, S., Alonso-Lago, M., Zorrilla-Larraga, M., Manrique-Abós, I., de las Heras-Dueña, M. E., Larrayoz, I. M., & Martínez, A. (2022). Prognostic and Predictive Biomarkers in Patients with Locally Advanced Rectal Cancer (LARC) Treated with Preoperative Chemoradiotherapy. Journal of Clinical Medicine, 11(20), 6091. https://doi.org/10.3390/jcm11206091







