1. Introduction
The spinal architecture with its reciprocating sagittal curves allows for physiological load absorption and maintenance of an upright posture. Sagittal plane alignment of the thoracolumbar spine has been shown to affect clinical outcomes [
1,
2,
3,
4], and appropriate cervical spine sagittal alignment has increasingly been reported as an important factor affecting postsurgical outcomes, quality of life and rates of cervical spondylosis [
5,
6,
7,
8].
Patients with adolescent idiopathic scoliosis (AIS) typically have reduced sagittal thoracic kyphosis (hypokyphosis) and decreased cervical lordosis [
9,
10,
11,
12]. The loss of kyphosis in the thoracic spine may translate into compensatory kyphosis in the cervical and lumbar spine [
9,
13]. If the sagittal plane is not corrected, scoliosis surgery may perpetuate thoracic hypokyphosis, driving the cervical spine into further compensatory kyphosis [
10,
11,
14,
15,
16]. Loss of cervical lordosis in the adult population has been associated with increased cervical osteoarthritis, increasing deformity, pain and debility [
17,
18,
19]. Rates of cervical spine degenerative changes and surgery for patients with adolescent idiopathic scoliosis have not been thoroughly explored in the literature.
Thus, we sought to evaluate cervical spine alignment, degenerative osteoarthritis, and the need for subsequent cervical spine surgery in a population of AIS patients with long-term follow-up. We hypothesized that thoracic hypokyphosis would be associated with degenerative changes in the cervical spine.
2. Materials and Methods
Between 1975 and 1992, a total of 2661 patients were treated for idiopathic scoliosis at a tertiary referral center. Of these 2661 patients, 733 were aged 0–21 years at the time of their initial scoliosis treatment. Upon medical record review, a total of 344 patients were confirmed with the diagnosis of AIS with childhood curves greater than 35 degrees treated with observation, bracing, or surgery. Patients with associated syndromes, neurologic abnormalities, infantile- or juvenile-onset, or congenital scoliosis were excluded from the study. Only idiopathic scoliosis patients seen before adulthood with appropriate radiographs and medical documentation were included. Medical records and radiographs were reviewed to identify all qualifying patients, demographics, and treatment protocols.
From the cohort of 344 eligible patients, 2 had died–one of unexplained pulmonary failure. A standardized survey was mailed to patients, including requests to describe additional spine or chest wall surgery and a battery of patient-reported outcome measures including Scoliosis Research Society scores, Spinal Appearance Questionnaires, Oswestry Disability Index, and EQ5D. Responses were received from 180 patients (52%). Mean follow-up was 30 years (range, 20–37).
In order to accurately assess sagittal alignment of the spine over time, the study only included patients that had high quality anteroposterior and lateral radiographs following scoliosis treatment at skeletal maturity (Risser 4 or 5) and at final follow-up. Radiographs taken at skeletal maturity for patients that had surgery were postoperative. A total of 33 patients met these criteria and returned for evaluation and follow-up radiographs either at the study center or locally. Childhood treatment included bracing (9), observation (3), and spinal fusion (21). Nonoperative patients (12) were compared to those undergoing childhood operative fusion (21).
Braced patients were treated in a Milwaukee brace. Surgery was typically performed for curves above 45–50 degrees and involved posterior fusion and instrumentation (n = 19) or anterior fusion and instrumentation (n = 2). Posterior instrumentation included 1st and 2nd generation Harrington rods (12) or hooks (7). Patients treated with 1st generation Harrington rods typically had pre- and postoperative casting and/or bracing.
Radiographs at skeletal maturity and most recent follow-up were compared to evaluate both coronal and sagittal curve progression as well as degenerative changes over the follow up period. The childhood radiographs of the patients had their respective curves graded per the Lenke classification with appropriate lumbar modifier [
20]. Coronal thoracic and lumbar Cobb angles at skeletal maturity and at most recent follow up were evaluated for changes. The following sagittal spinal parameters were assessed: (1) C2–C7 lordosis angle (CL), (2) C2–C7 sagittal vertical axis (SVA) (distance between the C2 plumb line and C7), (3) C7 SVA (distance between C7 plumb line and the posterior superior corner of S1), (4) thoracic kyphosis (TK) (angle between T1 and T12), and (5) thoracic slope (angle made between the superior endplate of T1 and the horizontal).
The degree of cervical spine spondylosis was measured on lateral radiographs at final follow up using the commonly used grading system created by Kellgren and Lawrence [
21,
22,
23,
24]. Both disc space narrowing and osteophytes were graded on a score of 0 to 3 as follows: 0—no disease, 1—mild disease, 2—moderate disease and 3—severe disease with disc narrowing with anterior and posterior osteophytes. Cervical disc spaces 2–3 through 6–7 were utilized for this grading. For the purpose of statistics the gross sum of all grades across the 5 cervical disc spaces were used. For categorization analysis, the degree of cervical osteoarthritis per patient was defined as the maximum score across the disc segments.
For all sagittal alignments, a positive reading denotes kyphosis and negative lordosis. Cervical sagittal alignment was split into three groups based on Cobb Angle for comparison: Kyphosis (>10°), Straight or normal (10° to −10°) and lordotic (<−10°). Thoracic alignment was also split into three groups for comparison: hypokyphotic (<20°), normokyphotic (20°–40°), hyperkyphotic (>40°).
Continuous variables were assessed using a student’s two-tailed t-test, and dichotomous variables were analyzed using a Chi-square analysis. Due to the small sample size, multivariate analysis was not undertaken. Statistical significance was set at p < 0.05.
3. Results
Of the 180 patients who responded to the survey, four had undergone a cervical spine procedure during the follow-up period. These procedures included single-level anterior cervical discectomy (ACDF) (2), multilevel ACDF (1), and discectomy (1) (2.2%). One additional patient had cervical radiculopathy and severe degenerative changes. Reported rates for ACDF in the general adult population are 0.03–0.16%. Thus, our population had a ten-fold higher rate of ACDF than expected.
The cohort with adequate radiographs both at skeletal maturity and latest follow-up consisted of 30 women and 3 men with an average age at follow-up of 42.6 ± 6.5 years. The majority of patients had inadequate childhood radiographs that either did not include the cervical spine or had poor image quality for the cervical spine. The average time from radiographs at skeletal maturity to final follow-up was 28.3 ± 5.4 years. There was no difference overall in the sagittal cervical and thoracic alignment between the nonoperative and operative cohorts (
Table 1).
Of these 33 patients in our cohort, 6 patients (18.8%) had additional thoracolumbar spinal surgery and 2 (6.2%) others had cervical spine surgery (one patient underwent C4–C6 anterior fusion and the other underwent C4–C5 anterior fusion). A total of 12 of the 33 (36%) had recently seen a chiropractor or pain specialist for back pain, and 4 of the 33 (9%) had consulted a specialist for neck pain.
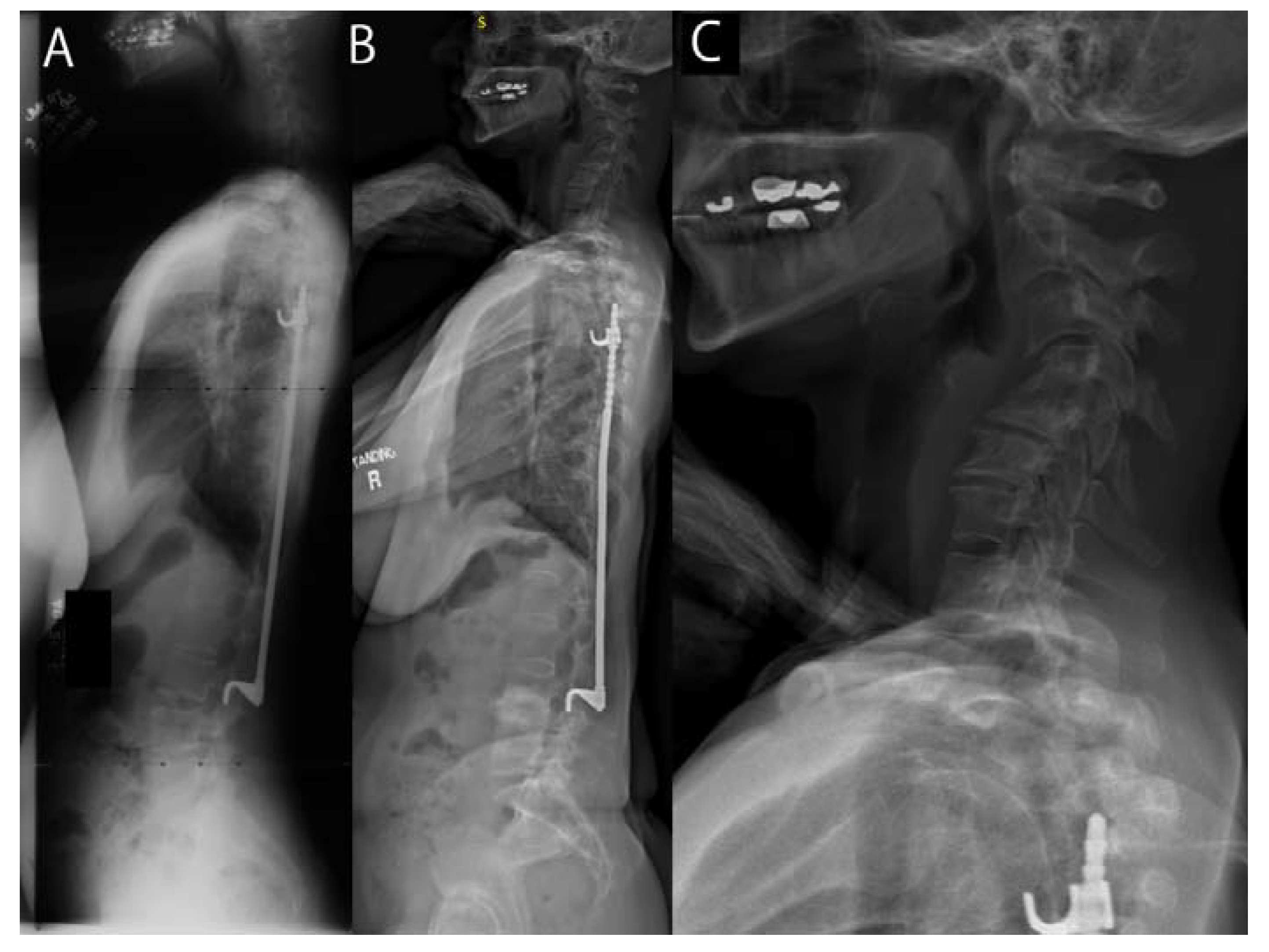
Using Kellgren–Lawrence scoring, we found that 58% of the cohort (19/33) had moderate or severe cervical osteoarthritis (
Figure 1). Those with minimal cervical osteoarthritis had a mean age of 40 ± 4.2 years, moderate had a mean age of 39 ± 5.8, and severe cervical osteo arthritis were 50 ± 3.2 years (
p < 0.01). There was no difference in the degree of cervical osteoarthritis between the surgical and nonoperative cohorts (
Figure 1).
Hypokyphosis of the thoracic spine at skeletal maturity and at latest follow-up compared to normokyphosis or hyperkyphosis correlated with increased adult cervical disc degeneration (
p = 0.028 and 0.0002, respectively) (
Table 2). Cervical osteoarthritis was increased in patients with hypokyphosis at latest follow-up compared to patients with normokyphosis or hyperkyphosis (
p = 0.0085). There was no correlation between the degree of osteoarthritis or disc degeneration versus cervical sagittal alignment at skeletal maturity or at final follow-up.
Sagittal alignment measurements were compared for radiographs taken at skeletal maturity and at final follow-up. There were no significant differences in C7 SVA, C2C7SVA, T1 Slope and cervical or thoracic sagittal alignment between the patient’s radiographs as adolescents and those at follow up (
p > 0.5,
Table 3). Additionally, there was no significant difference between these measurements taken in adolescence and at adulthood when looking at the operative and non-operative patients separately. However, lumbar and pelvic parameters were found to change significantly, including decreased lumbar lordosis, increased pelvic tilt and resultant decreased sacral slope as these two parameters vary inversely (
Table 3). Pelvic incidence did not change significantly as expected.
Analysis of cervical sagittal alignment at follow up found that the amount of the cervical kyphosis did not correlate with thoracic kyphosis or any other spine alignment variable including pelvic parameters (p > 0.5). This held true when looking at the non-operative vs. operative patients.
The data on the patient reported outcome measures (SRS, ODI and EQ5D) did not show any difference based on cervical sagittal alignment. However, the thoracic alignment at follow up was associated with both SRS Function and ODI. For patients with thoracic hypokyphosis, the ODI was 28.7 ± 18.6 in comparison to the patients with normal kyphosis with an ODI of 8.6 ± 8.6 (p = 0.008).
4. Discussion
In the adult spinal deformity literature, cervical kyphosis has been associated with increased degenerative disease and pain [
7,
8,
18]. Cervical sagittal plane alignment after surgery for adolescent idiopathic scoliosis has become an increasingly important topic [
9,
10,
11,
14,
15,
16].
However, the long-term effects of cervical kyphosis in patients with adolescent idiopathic scoliosis are not well defined. This study reviewed a unique cohort of patients with a minimum of 20 years follow up who had undergone childhood treatment for AIS. In particular, we sought to assess the association between cervical sagittal alignment, cervical osteoarthritis, cervical spine surgery, and patient related outcomes.
The prevalence of cervical arthritic changes has been detailed in the literature [
23,
24,
25,
26,
27] and has been reported from 25–46% in people aged 40–49 and 65–73% in people aged 50–59 [
24,
25]. The actual rate of moderate to severe cervical osteoarthritis and progression of disease in the 40–50 age group has been reported from 16–20% [
23,
26]. In comparison, our study cohort had a prevalence of 30% moderate degeneration and 28% severe degeneration with a combined prevalence of 58%. Additionally, the majority of the patients were in the 40–50 age range (81%) with only 5 patients (15%) being above the age of 50. Thus, our cohort may have more advanced cervical osteoarthritis than the average population, although a matched cohort of patients without scoliosis would provide more reliable comparison data.
Two (6.2%) of the patients had undergone cervical spine surgery, which is much higher than the reported incidence of anterior spinal fusion in the general population (0.05–0.2%) [
28,
29]. From our survey cohort, four out of 180 patients (2.2%) reported undergoing cervical spine surgery in adulthood. Interestingly, only 9% of our cohort complained of cervical pain. Edgar et al. in 1988 followed up patients with AIS who had been observed or had posterior spinal fusion at minimum of 10 years from skeletal maturity and found that neck pain was more prevalent (17.6%) in the patients who had fusion versus those who did not (7.8) [
30]. Our cohort’s prevalence of 9% falls within this range but did not show a difference between those patients who were treated nonoperatively (1/12 patients, 8.3%) compared to those who underwent fusion surgery (2/21 patients, 9.5%).
The cervical alignment in patients with AIS has been discussed broadly in the literature as it differs from that of the general population. The natural tendency of the cervical spine in the general population is toward lordosis ranging from 15 to 40 degrees of lordosis with only 9% prevalence of kyphosis [
7,
26,
27]. In AIS, there is a high prevalence of cervical kyphosis which ranges from 34 to 54% [
10,
11,
13,
14,
15,
16]. This number increases to as high as 89% of patients if the “straight” cervical profiles are included [
9]. Our cohort showed an overall prevalence of 48% kyphosis (>10 degrees) and 21% “straight” cervical profile. This phenomenon is postulated to be caused by the three-dimensional deformity of AIS, and a compensatory cervical kyphosis develops secondary to the loss of thoracic kyphosis seen AIS. This has been shown in recent studies evaluating the effect of surgery on the cervical alignment in patients with AIS. Persistent hypokyphosis of the thoracic spine after spinal fusion surgery is thought to result in persistent postoperative cervical spine kyphosis [
10,
11,
14,
15]. In our study, however, there was no correlation between cervical and thoracic sagittal plane alignment. This may be secondary to the use of only postoperative films in comparison or small sample size.
Cervical kyphosis is often maligned in the literature as a cause of pain and degeneration in the adult cervical spine postoperative patient [
5,
18,
31]. These patients however already have pathology or deformity, and studies addressing only healthy populations have not shown that cervical alignment is associated with increased symptoms or degeneration [
7]. Interestingly, we did show that cervical degeneration at follow-up was correlated with the thoracic alignment at skeletal maturity. Thus, increased thoracic spine hypokyphosis was associated with increased cervical degeneration, perhaps due to compensatory changes in the cervical spine.
The limitations of this study include the low number of patients in the cohort. Most of the identified patients had to be excluded due to inadequate imaging of the cervical spine. This may under power the study, especially considering that it includes both operative and nonoperative patients. However, patient numbers in this study are similar to other short-term follow-up studies on cervical alignment in AIS. Similarly, most long-term follow-up studies are for a minimum of 10 years or have numbers similar to our study [
32,
33,
34,
35,
36]. Further, lateral childhood radiographs were taken of the entire spine and thus are subject to parallax. The majority of current lateral radiographs of the entire spine were taken using the EOS, which eliminates parallax and has shown to provide good inter- and intra-observer reliability of cervical spine measurements in scoliosis patients. Further, flexion-extension radiographs were not available. Quality of the childhood radiographs compared to adult radiographs may be variable and may alter radiographic measurements. Patients undergoing nonoperative management less frequently had lateral scoliosis radiographs available for analysis; thus, there were fewer nonoperative patients who could be included in our series. Patients who returned for radiographs may not be representative of the entire cohort. Lastly, this study distributed both thoracic and cervical alignment into separate groups by defining both lordosis and kyphosis using set groupings. This was mitigated using the quantitative variables in these settings in order to confirm any findings in which these groupings were used. This is also reflective of the literature which does not have a set definition of both cervical kyphosis and thoracic hypokyphosis.
In summary, this study provides long-term evaluation of the cervical spine after previous treatment of AIS. Cervical spine degeneration is common in these patients and is likely more severe than patients of similar age without scoliosis. Furthermore, our AIS population had a higher rate of cervical spine surgery in adulthood than expected from other population reports. Both cervical and sagittal alignment did not change with age or treatment, although there was a higher rate of degenerative changes in patients with decreased thoracic kyphosis.
Author Contributions
Conceptualization, A.N.L., M.J.Y., E.Y. and B.L.C.; methodology, A.N.L., M.J.Y., E.Y. and B.L.C.; software, E.Y.; validation, E.Y., C.R., B.L.C., M.J.Y. and A.N.L.; formal analysis, E.Y., C.R., B.L.C., M.J.Y. and A.N.L.; investigation, E.Y., C.R., B.L.C., M.J.Y. and A.N.L.; resources, M.J.Y. and A.N.L.; data curation, E.Y., C.R. and A.N.L.; writing—original draft preparation, E.Y., A.N.L.; writing—review and editing, E.Y., C.R., A.N.L.; visualization, E.Y., C.R. and A.N.L.; supervision, B.L.C., M.J.Y. and A.N.L.; project administration, A.N.L.; funding acquisition, A.N.L. and M.J.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Directed Research Grant sponsored by the Scoliosis Research Society.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Mayo Clinic (protocol 18-008732, 21 November 16, and protocol 12-008308, 5 December 2012) for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
Not applicable.
Acknowledgments
We would like to acknowledge Vickie Treder, CCRP, who assisted in this study.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Glassman, S.D.; Bridwell, K.; Dimar, J.R.; Horton, W.; Berven, S.; Schwab, F. The impact of positive sagittal balance in adult spinal deformity. Spine 2005, 30, 2024–2029. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.P.; McManus, A.C. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine 1994, 19, 1611–1618. [Google Scholar] [CrossRef]
- Vialle, R.; Levassor, N.; Rillardon, L.; Templier, A.; Skalli, W.; Guigui, P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J. Bone Jt. Surg. Am. 2005, 87, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Kuntz, C.; Levin, L.S.; Ondra, S.L.; Shaffrey, C.I.; Morgan, C.J. Neutral upright sagittal spinal alignment from the occiput to the pelvis in asymptomatic adults: A review and resynthesis of the literature. J. Neurosurg. Spine 2007, 6, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Ames, C.P.; Blondel, B.; Scheer, J.K.; Schwab, F.J.; Le Huec, J.C.; Massicotte, E.M.; Patel, A.A.; Traynelis, V.C.; Kim, H.J.; Shaffrey, C.I.; et al. Cervical radiographical alignment: Comprehensive assessment techniques and potential importance in cervical myelopathy. Spine 2013, 38, S149–S160. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, M.; Hymanson, H.J.; Morishita, Y.; He, W.; Zhang, H.; Wu, G.; Kong, M.H.; Tsumura, H.; Wang, J.C. Kinematic analysis of the relationship between sagittal alignment and disc degeneration in the cervical spine. Spine 2008, 33, E870–E876. [Google Scholar] [CrossRef] [PubMed]
- Okada, E.; Matsumoto, M.; Ichihara, D.; Chiba, K.; Toyama, Y.; Fujiwara, H.; Momoshima, S.; Nishiwaki, Y.; Hashimoto, T.; Ogawa, J.; et al. Does the sagittal alignment of the cervical spine have an impact on disk degeneration? Minimum 10-year follow-up of asymptomatic volunteers. Eur. Spine J. 2009, 18, 1644–1651. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.A.; Scheer, J.K.; Smith, J.S.; Deviren, V.; Bess, S.; Hart, R.A.; Lafage, V.; Shaffrey, C.I.; Schwab, F.; Ames, C.P. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2012, 71, 662–669. [Google Scholar] [CrossRef] [PubMed]
- Hilibrand, A.S.; Tannenbaum, D.A.; Graziano, G.P.; Loder, R.T.; Hensinger, R.N. The sagittal alignment of the cervical spine in adolescent idiopathic scoliosis. J. Pediatr. Orthop. 1995, 15, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Roussouly, P.; Labelle, H.; Rouissi, J.; Bodin, A. Pre- and post-operative sagittal balance in idiopathic scoliosis: A comparison over the over the ages of two cohorts of 132 adolescents and 52 adults. Eur. Spine J. 2013, 22, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Sucato, D.J.; Agrawal, S.; O’Brien, M.F.; Lowe, T.G.; Richards, S.B.; Lenke, L. Restoration of thoracic kyphosis after operative treatment of adolescent idiopathic scoliosis: A multicenter comparison of three surgical approaches. Spine 2008, 33, 2630–2636. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Silvestre, C.; Mouton, T.; Rachkidi, R.; Zeng, L.; Roussouly, P. Analysis of the cervical spine sagittal alignment in young idiopathic scoliosis: A morphological classification of 120 cases. Eur. Spine J. 2013, 22, 2372–2381. [Google Scholar] [CrossRef]
- Canavese, F.; Turcot, K.; De Rosa, V.; de Coulon, G.; Kaelin, A. Cervical spine sagittal alignment variations following posterior spinal fusion and instrumentation for adolescent idiopathic scoliosis. Eur. Spine J. 2011, 20, 1141–1148. [Google Scholar] [CrossRef]
- Hwang, S.W.; Samdani, A.F.; Tantorski, M.; Cahill, P.; Nydick, J.; Fine, A.; Betz, R.R.; Antonacci, M.D. Cervical sagittal plane decompensation after surgery for adolescent idiopathic scoliosis: An effect imparted by postoperative thoracic hypokyphosis. J. Neurosurg. Spine 2011, 15, 491–496. [Google Scholar] [CrossRef]
- Ilharreborde, B.; Vidal, C.; Skalli, W.; Mazda, K. Sagittal alignment of the cervical spine in adolescent idiopathic scoliosis treated by posteromedial translation. Eur. Spine J. 2013, 22, 330–337. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Harrison, D.D.; Harrison, D.E.; Janik, T.J.; Cailliet, R.; Ferrantelli, J.R.; Haas, J.W.; Holland, B. Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: Results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine 2004, 29, 2485–2492. [Google Scholar] [CrossRef] [PubMed]
- Katsuura, A.; Hukuda, S.; Saruhashi, Y.; Mori, K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur. Spine J. 2001, 10, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Ofiram, E.; Garvey, T.A.; Schwender, J.D.; Wroblewski, J.M.; Winter, R.B. Cervical degenerative changes in idiopathic scoliosis patients who underwent long fusion to the sacrum as adults: Incidence, severity, and evolution. J. Orthop. Traumatol. 2009, 10, 27–30. [Google Scholar] [CrossRef]
- Lenke, L.G.; Betz, R.R.; Harms, J.; Bridwell, K.H.; Clements, D.H.; Lowe, T.G.; Blanke, K. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J. Bone Jt. Surg. Am. 2001, 83, 1169–1181. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Osteo-arthrosis and disk degeneration in an urban population. Ann. Rheum. Dis. 1958, 17, 388–397. [Google Scholar] [CrossRef] [PubMed]
- Ofiram, E.; Garvey, T.A.; Schwender, J.D.; Denis, F.; Perra, J.H.; Transfeldt, E.E.; Winter, R.B.; Wroblewski, J.M. Cervical degenerative index: A new quantitative radiographic scoring system for cervical spondylosis with interobserver and intraobserver reliability testing. J. Orthop. Traumatol. 2009, 10, 21–26. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wilder, F.V.; Fahlman, L.; Donnelly, R. Radiographic cervical spine osteoarthritis progression rates: A longitudinal assessment. Rheumatol. Int. 2011, 31, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Irvine, D.H.; Foster, J.B.; Newell, D.J.; Klukvin, B.N. Prevalence of Cervical Spondylosis in a General Practice. Lancet 1965, 1, 1089–1092. [Google Scholar] [CrossRef]
- Friedenberg, Z.B.; Miller, W.T. Degenerative Disc Disease of the Cervical Spine. J. Bone Jt. Surg. Am. 1963, 45, 1171–1178. [Google Scholar] [CrossRef]
- Gore, D.R.; Sepic, S.B.; Gardner, G.M. Roentgenographic findings of the cervical spine in asymptomatic people. Spine 1986, 11, 521–524. [Google Scholar] [CrossRef]
- Hardacker, J.W.; Shuford, R.F.; Capicotto, P.N.; Pryor, P.W. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine 1997, 22, 1472–1480. [Google Scholar] [CrossRef]
- Marawar, S.; Girardi, F.P.; Sama, A.A.; Ma, Y.; Gaber-Baylis, L.K.; Besculides, M.C.; Memtsoudis, S.G. National trends in anterior cervical fusion procedures. Spine 2010, 35, 1454–1459. [Google Scholar] [CrossRef] [PubMed]
- Saifi, C.; Fein, A.W.; Cazzulino, A.; Lehman, R.A.; Phillips, F.M.; An, H.S.; Riew, K.D. Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine J. 2018, 18, 1022–1029. [Google Scholar] [CrossRef] [PubMed]
- Edgar, M.A.; Mehta, M.H. Long-term follow-up of fused and unfused idiopathic scoliosis. J. Bone Jt. Surg. Br. 1988, 70, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, M.; Tamaki, T.; Yoshida, M.; Hayashi, N.; Ando, M.; Yamada, H. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. J. Spinal Disord. 1999, 12, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Hansen, M.A.; Kim, H.J.; Van Alstyne, E.M.; Skelly, A.C.; Fehlings, M.G. Does postsurgical cervical deformity affect the risk of cervical adjacent segment pathology? A systematic review. Spine 2012, 37 (Suppl. S22), S75–S84. [Google Scholar] [CrossRef]
- Direito-Santos, B.; Queirós, C.M.; Serrano, P.; Encarnação, A.; Campos, A.; Olivera, A. Long-Term Follow-Up of Anterior Spinal Fusion for Thoracolumbar/Lumbar Curves in Adolescent Idiopathic Scoliosis. Spine 2019, 44, 1137–1143. [Google Scholar] [CrossRef]
- Chiu, C.K.; Tan, C.S.; Chung, W.H.; Mohamad, S.M.; Kwan, M.K.; Chan, C.Y.W. Mid-long-term outcome and degeneration of the remaining unfused lumbar intervertebral disc in adolescent idiopathic scoliosis patients who had posterior spinal fusion surgery. Eur. Spine J. 2021, 30, 1978–1987. [Google Scholar] [CrossRef]
- Jakkepally, S.; Viswanathan, V.K.; Shetty, A.P.; Hajare, S.; Kanna, R.M.; Rajasekaran, S. The analysis of progression of disc degeneration in distal unfused segments and evaluation of long-term functional outcome in adolescent idiopathic scoliosis patients undergoing long-segment instrumented fusion. Spine Deform. 2022, 10, 343–350. [Google Scholar] [CrossRef]
- Darnis, A.; Grobost, P.; Roussouly, P. Very long-term clinical and radiographic outcomes after posterior spinal fusion with pedicular screws for thoracic adolescent idiopathic scoliosis. Spine Deform. 2021, 9, 441–449. [Google Scholar] [CrossRef]
- Lim, J.L.; Hey, H.W.D.; Kumar, N.; Teo, A.Q.A.; Lau, L.L.; Hee, H.T.; Ruiz, J.N.; Kumar, N.S.; Thambiah, J.S.; Liu, G.K.; et al. A 10-Year Radiographic Study Comparing Anterior Versus Posterior Instrumented Spinal Fusion in Patients with Lenke Type 5 Adolescent Idiopathic Scoliosis. Spine 2020, 45, 612–620. [Google Scholar] [CrossRef]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).