Can the Duration of In-Hospital Ventilation in Patients with Sepsis Help Predict Long-Term Survival?
Abstract
1. Introduction
2. Methods
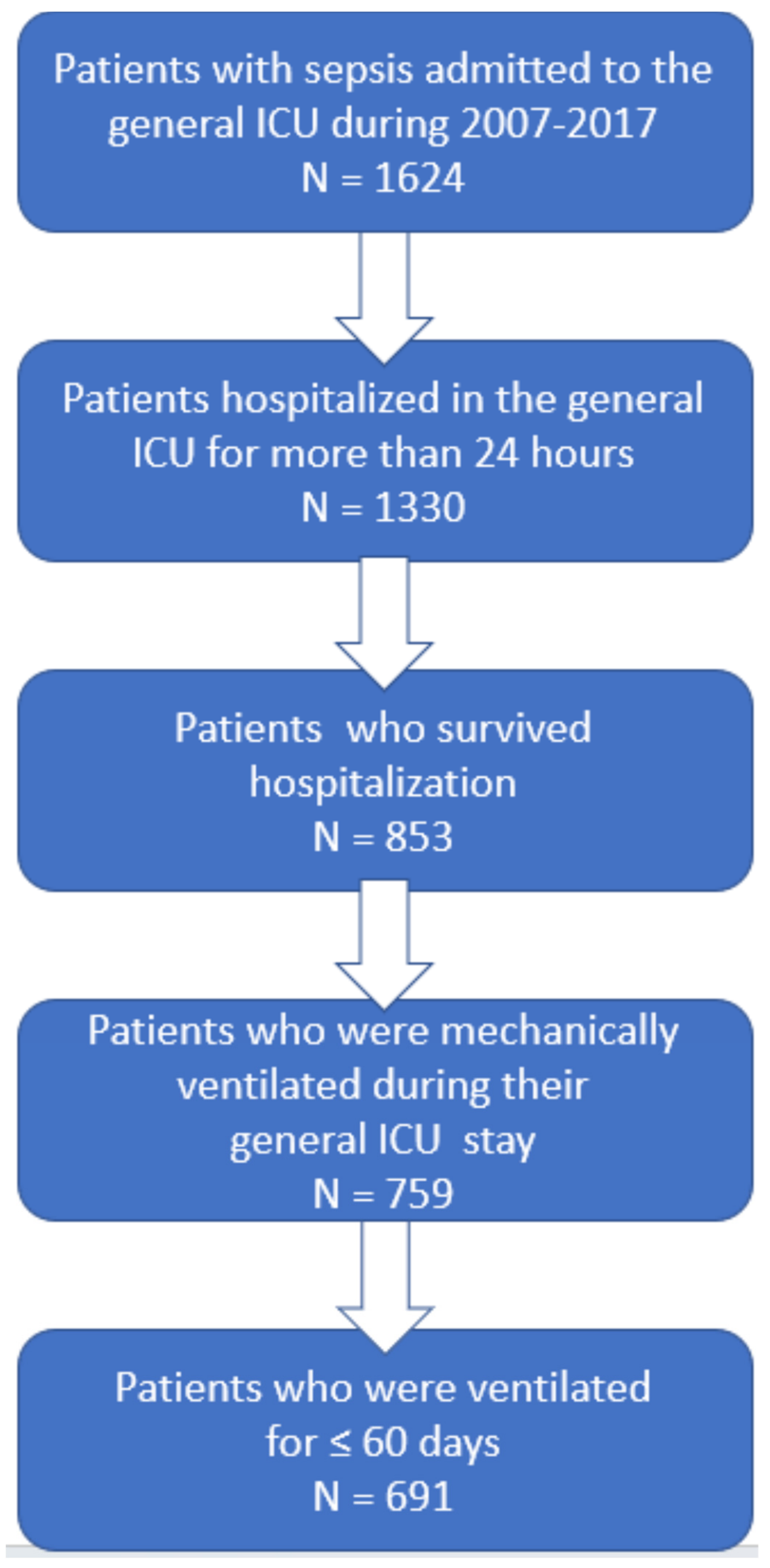
2.1. Study Population
2.2. Primary Exposure and Outcome Assessment—Study Design
2.3. Statistical Analysis
3. Results
3.1. Study Population
3.2. Hospitalization Data
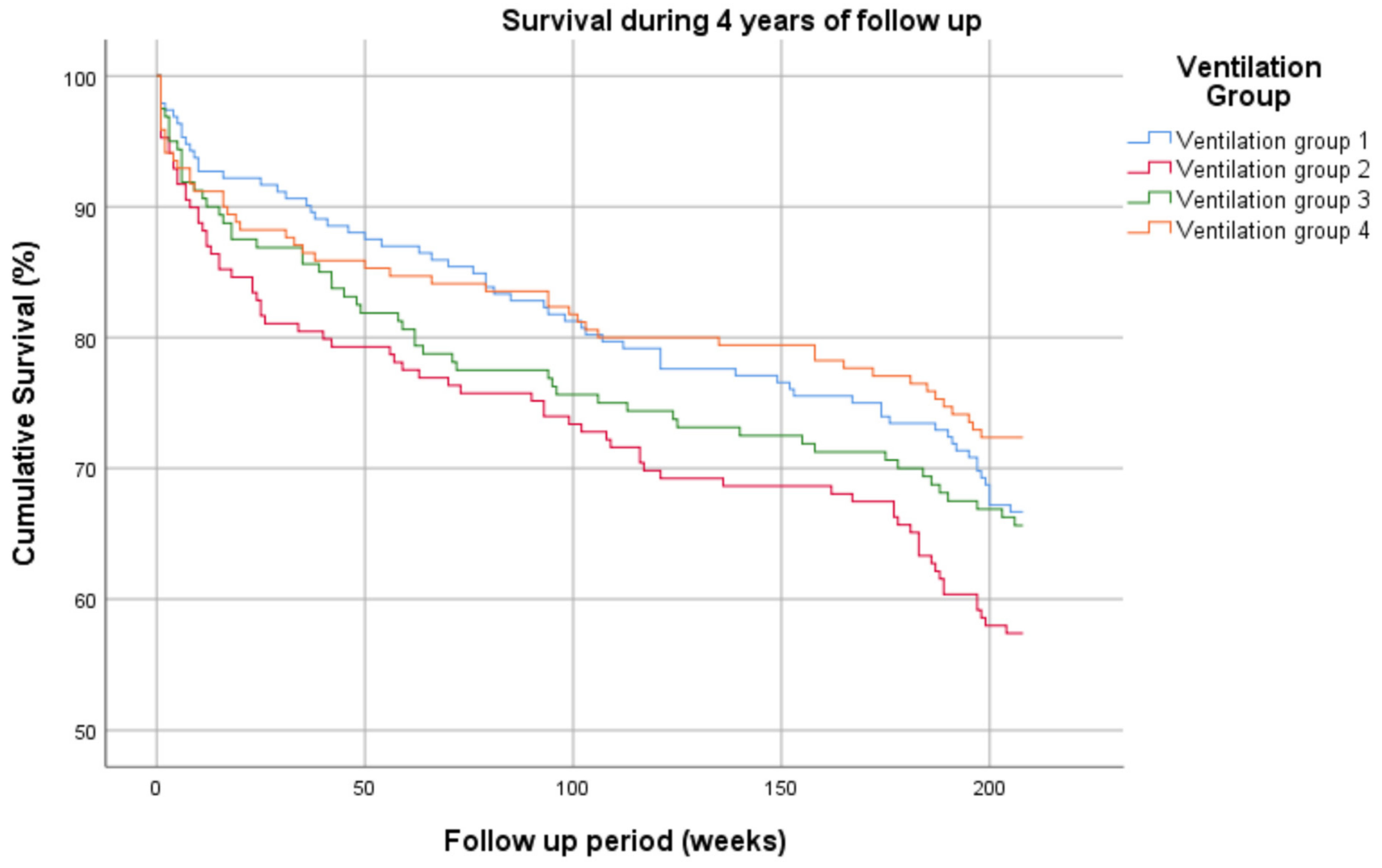
3.3. Survival
3.4. Multivariable Regression Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mohamed, A.K.S.; Mehta, A.A.; James, P. Predictors of Mortality of Severe Sepsis among Adult Patients in the Medical Intensive Care Unit. Lung India Off. Organ Indian Chest Soc. 2017, 34, 330. [Google Scholar]
- Pittet, D.; Thiévent, B.; Wenzel, R.P.; Li, N.; Auckenthaler, R.; Suter, P.M. Bedside Prediction of Mortality from Bacteremic Sepsis. A Dynamic Analysis of ICU Patients. Am. J. Respir. Crit. Care Med. 1996, 153, 684–693. [Google Scholar] [CrossRef] [PubMed]
- MacIntyre, N.R.; Epstein, S.K.; Carson, S.; Scheinhorn, D.; Christopher, K.; Muldoon, S. Management of Patients Requiring Prolonged Mechanical Ventilation: Report of a NAMDRC Consensus Conference. Chest 2005, 128, 3937–3954. [Google Scholar] [CrossRef] [PubMed]
- Wunsch, H.; Linde-Zwirble, W.T.; Angus, D.C.; Hartman, M.E.; Milbrandt, E.B.; Kahn, J.M. The Epidemiology of Mechanical Ventilation Use in the United States. Crit. Care Med. 2010, 38, 1947–1953. [Google Scholar] [CrossRef] [PubMed]
- Carson, S.S.; Bach, P.B. The Epidemiology and Costs of Chronic Critical Illness. Crit. Care Clin. 2002, 18, 461–476. [Google Scholar] [CrossRef]
- Damuth, E.; Mitchell, J.A.; Bartock, J.L.; Roberts, B.W.; Trzeciak, S. Long-Term Survival of Critically Ill Patients Treated with Prolonged Mechanical Ventilation: A Systematic Review and Meta-Analysis. Lancet Respir. Med. 2015, 3, 544–553. [Google Scholar] [CrossRef]
- Cox, C.E.; Carson, S.S. Medical and Economic Implications of Prolonged Mechanical Ventilation and Expedited Post–Acute Care. In Seminars in Respiratory and Critical Care Medicine; Thieme Medical Publishers: New York, NY, USA, 2012; Volume 33, pp. 357–361. [Google Scholar]
- Carson, S.S.; Bach, P.B.; Brzozowski, L.; Leff, A. Outcomes after Long-Term Acute Care: An Analysis of 133 Mechanically Ventilated Patients. Am. J. Respir. Crit. Care Med. 1999, 159, 1568–1573. [Google Scholar] [CrossRef] [PubMed]
- Jameson, J.L.; Kasper, D.L.; Fauci, A.S.; Hauser, S.L.; Longo, D.L.; Loscalzo, J. Harrison’s Principles of Internal Medicine; McGraw-hill Education: New York, NY, USA, 2018; ISBN 1259644049. [Google Scholar]
- Hill, A.D.; Fowler, R.A.; Burns, K.E.; Rose, L.; Pinto, R.L.; Scales, D.C. Long-Term Outcomes and Health Care Utilization after Prolonged Mechanical Ventilation. Ann. Am. Thorac. Soc. 2017, 14, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Lambden, S.; Laterre, P.F.; Levy, M.M.; Francois, B. The SOFA Score—Development, Utility and Challenges of Accurate Assessment in Clinical Trials. Crit. Care 2019, 23, 374. [Google Scholar] [CrossRef] [PubMed]
- Lopes Ferreira, F.; Peres Bota, D.; Bross, A.; Mélot, C.; Vincent, J.-L. Serial Evaluation of the SOFA Score to Predict Outcome in Critically Ill Patients. JAMA J. Am. Med. Assoc. 2001, 286, 1754–1758. [Google Scholar] [CrossRef] [PubMed]
| Group 1 (n = 192) | Group 2 (n = 169) | Group 3 (n = 160) | Group 4 (n = 170) | p Value | |
|---|---|---|---|---|---|
| Age (Mean ± SD) | 54.97 (19.95) | 56.34 (19.23) | 55.31 (19.23) | 49.94 (20.78) | 0.015 |
| Male gender | 108 (56.3%) | 108 (63.9%) | 94 (58.8%) | 120 (70.6%) | 0.029 |
| Hypertension | 62 (32.3%) | 52 (30.8%) | 43 (26.9%) | 39 (22.9%) | 0.206 |
| CVA | 7 (3.6%) | 5 (3%) | 5 (3.1%) | 4 (2.4%) | 0.915 |
| Diabetes mellitus | 50 (26%) | 48 (28.4%) | 34 (21.3%) | 27 (15.9%) | 0.030 |
| Ischemic heart disease | 22 (11.5%) | 13 (7.7%) | 8 (5%) | 7 (4.1%) | 0.032 |
| Chronic kidney disease | 10 (5.2%) | 11 (6.5%) | 10 (6.3%) | 4 (2.4%) | 0.283 |
| Solid tumor | 3 (1.6%) | 0 (0%) | 1 (0.6%) | 0 (0%) | 0.157 |
| Smoking | 53 (27.6%) | 42 (24.9%) | 38 (23.8%) | 34 (20%) | 0.303 |
| COPD | 22 (11.5%) | 18 (10.7%) | 6 (3.8%) | 13 (7.6%) | 0.047 |
| Group 1 (n = 192) | Group 2 (n = 169) | Group 3 (n = 160) | Group 4 (n = 170) | p Value | |
|---|---|---|---|---|---|
| SOFA score—Median (IQR) | 7 (5–8) | 9 (7–11) | 9 (7–11) | 9 (7–11) | <0.001 |
| ICU hospitalization duration (days) Median (IQR) | 2 (1–4) | 8 (6–10) | 16 (13–20) | 31 (26.75–38.25) | <0.001 |
| Invasive ventilation duration (days) Median (IQR) | 1 (1–1.18) | 5.17 (3.8–6.7) | 13.7 (10.65–17.74) | 36.58 (28.74–46.43) | <0.001 |
| Use of tracheostomy | 11 (5.7%) | 15 (8.9%) | 72 (45%) | 161 (94.7%) | <0.001 |
| Group 1 (n = 192) | Group 2 (n = 169) | Group 3 (n = 160) | Group 4 (n = 170) | ||
|---|---|---|---|---|---|
| 1-year survival | Estimate (std.) | 87.0% (0.024) | 78.7% (0.031) | 81.9% (0.03) | 85.3% (0.027) |
| 2-year survival | 80.2% (0.029) | 72.8% (0.034) | 75.0% (0.034) | 80.6% (0.30) | |
| 3-year survival | 75.5% (0.031) | 68.0% (0.036) | 71.9% (0.036) | 78.2% (0.032) | |
| 4-year survival | 66.7% (0.034) | 57.4% (0.038) | 65.6% (0.038) | 72.4% (0.034) | |
| p values Kaplan–Meier test | 0.035 | ||||
| Hazard Ratio | 95% Confidence Interval | p Value | |
|---|---|---|---|
| Age (per year) | 1.03 | 1.02–1.04 | <0.001 |
| Gender (male) | 0.78 | 0.59–1.02 | 0.073 |
| Diabetes mellitus | 1.45 | 1.09–1.94 | 0.01 |
| Ischemic heart disease | 1.2 | 0.79–1.79 | 0.397 |
| VG, when the reference is VG1 (1–2 ventilation days) | 0.544 | ||
| VG2 (3–8 ventilation days) | 1.12 | 0.74–1.69 | 0.582 |
| VG3 (9–21 ventilation days) | 1.31 | 0.90–1.91 | 0.157 |
| VG4 (22–60 ventilation days) | 1.12 | 0.75–1.66 | 0.569 |
| SOFA groups, when the reference is group 1 (SOFA scores 0–6) | 0.362 | ||
| SOFA group 2 (SOFA scores 7–8) | 0.69 | 0.43–1.13 | 0.144 |
| SOFA group 3 (SOFA scores 9–10) | 0.74 | 0.47–1.18 | 0.209 |
| SOFA group 4(SOFA scores 11–12) | 0.99 | 0.63–1.54 | 0.975 |
| SOFA group 5 (SOFA scores 13–19) | 0.89 | 0.56–1.42 | 0.892 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klein, M.; Israeli, A.; Hassan, L.; Binyamin, Y.; Frank, D.; Boyko, M.; Novack, V.; Frenkel, A. Can the Duration of In-Hospital Ventilation in Patients with Sepsis Help Predict Long-Term Survival? J. Clin. Med. 2022, 11, 5995. https://doi.org/10.3390/jcm11205995
Klein M, Israeli A, Hassan L, Binyamin Y, Frank D, Boyko M, Novack V, Frenkel A. Can the Duration of In-Hospital Ventilation in Patients with Sepsis Help Predict Long-Term Survival? Journal of Clinical Medicine. 2022; 11(20):5995. https://doi.org/10.3390/jcm11205995
Chicago/Turabian StyleKlein, Moti, Adir Israeli, Lior Hassan, Yair Binyamin, Dmitry Frank, Matthew Boyko, Victor Novack, and Amit Frenkel. 2022. "Can the Duration of In-Hospital Ventilation in Patients with Sepsis Help Predict Long-Term Survival?" Journal of Clinical Medicine 11, no. 20: 5995. https://doi.org/10.3390/jcm11205995
APA StyleKlein, M., Israeli, A., Hassan, L., Binyamin, Y., Frank, D., Boyko, M., Novack, V., & Frenkel, A. (2022). Can the Duration of In-Hospital Ventilation in Patients with Sepsis Help Predict Long-Term Survival? Journal of Clinical Medicine, 11(20), 5995. https://doi.org/10.3390/jcm11205995






