Perioperative Predictive Factors for Positive Outcomes in Spine Fusion for Adult Deformity Correction
Abstract
:1. Introduction
2. Materials and Methods
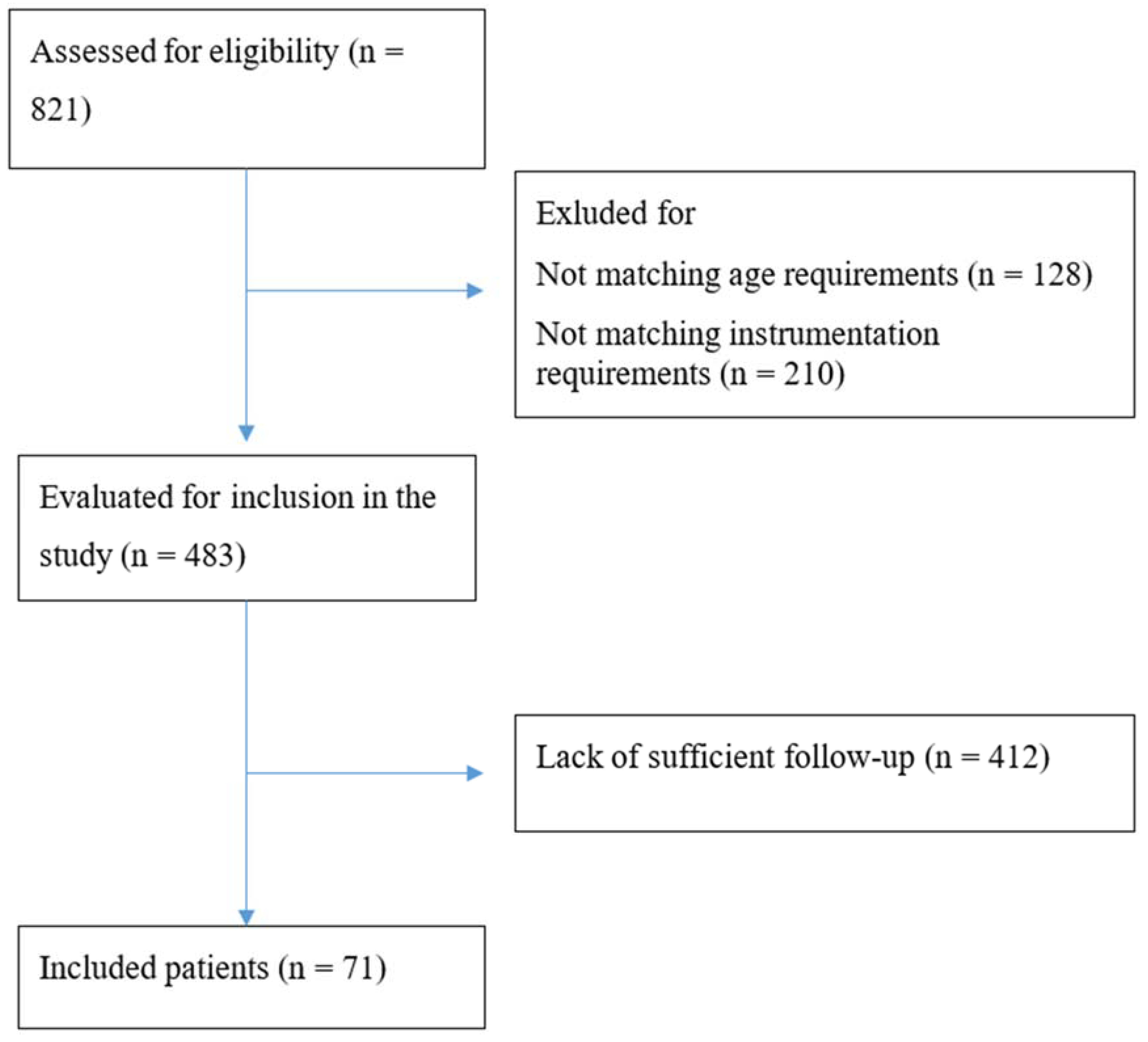
2.1. Patient Recruitment
2.2. Outcomes of Interest
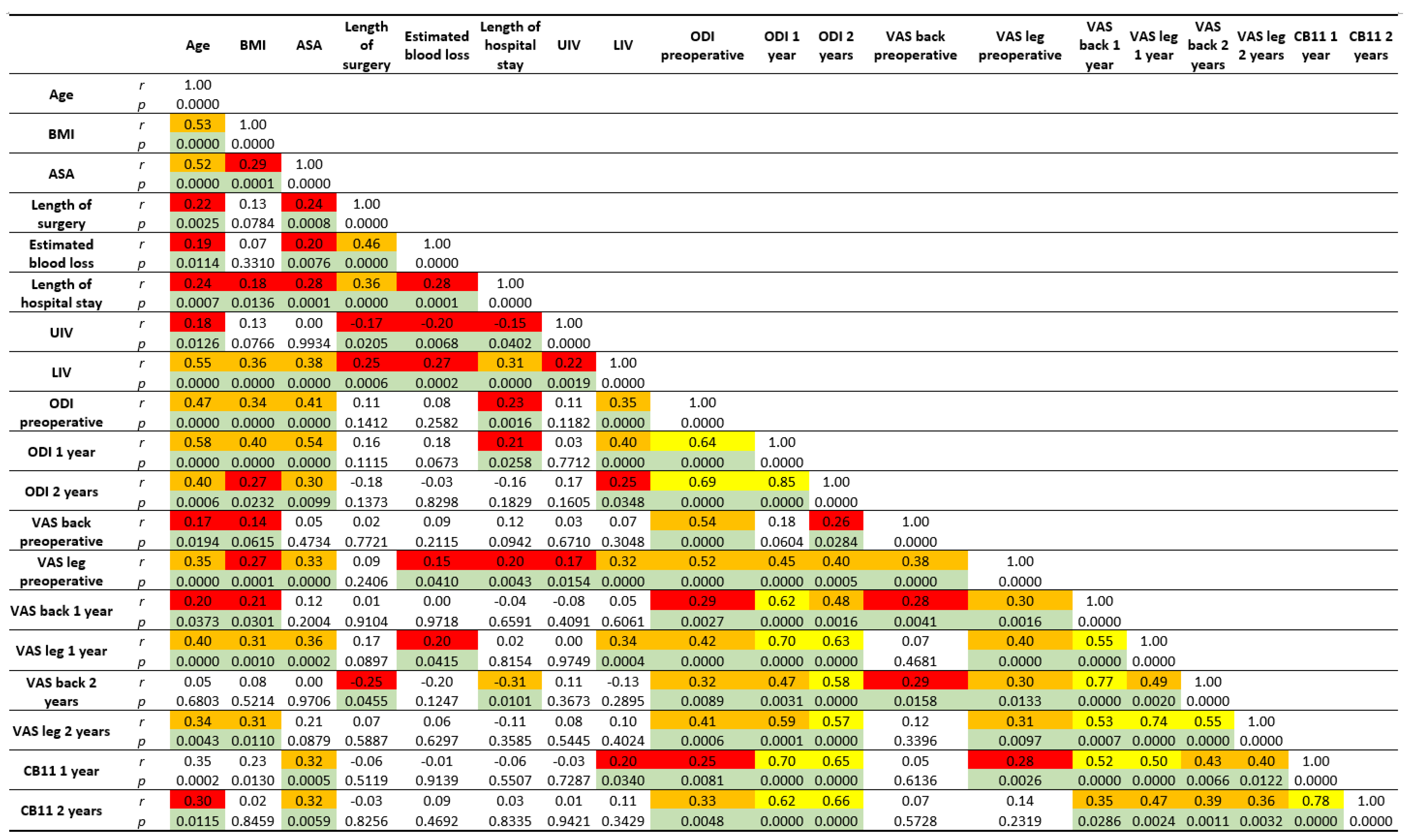
2.3. Statistical Analysis
3. Results
3.1. Patient Recruitment and Demographics
3.2. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoy, D.; Brooks, P.; Blyth, F.; Buchbinder, R. The Epidemiology of low back pain. Best Pract. Res. Clin. Rheumatol. 2010, 24, 769–781. [Google Scholar] [CrossRef] [PubMed]
- Kostuik, J.P.; Bentivoglio, J. The incidence of low-back pain in adult scoliosis. Spine 1981, 6, 268–273. [Google Scholar] [CrossRef]
- Berven, S.; Deviren, V.; Demir-Deviren, S.; Hu, S.S.; Bradford, D.S. Studies in the modified Scoliosis Research Society Outcomes Instrument in adults: Validation, reliability, and discriminatory capacity. Spine 2003, 28, 2164–2169. [Google Scholar] [CrossRef] [PubMed]
- Ogura, Y.; Shinozaki, Y.; Kobayashi, Y.; Kitagawa, T.; Yonezawa, Y.; Takahashi, Y.; Yoshida, K.; Yasuda, A.; Ogawa, J. Impact of sagittal spinopelvic alignment on clinical outcomes and health-related quality of life after decompression surgery without fusion for lumbar spinal stenosis. J. Neurosurg. Spine 2019, 1–6. [Google Scholar] [CrossRef]
- Daniels, A.H.; Reid, D.B.; Tran, S.N.; Hart, R.A.; Klineberg, E.O.; Bess, S.; Burton, D.; Smith, J.S.; Shaffrey, C.; Gupta, M.; et al. Evolution in Surgical Approach, Complications, and Outcomes in an Adult Spinal Deformity Surgery Multicenter Study Group Patient Population. Spine Deform. 2019, 7, 481–488. [Google Scholar] [CrossRef]
- Berjano, P.; Langella, F.; Ismael, M.-F.; Damilano, M.; Scopetta, S.; Lamartina, C. Successful correction of sagittal imbalance can be calculated on the basis of pelvic incidence and age. Eur. Spine J. 2014, 23, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Campagner, A.; Berjano, P.; Lamartina, C.; Langella, F.; Lombardi, G.; Cabitza, F. Assessment and prediction of spine surgery invasiveness with machine learning techniques. Comput. Biol. Med. 2020, 121, 103796. [Google Scholar] [CrossRef]
- Langella, F.; Villafañe, J.H.; Damilano, M.; Cecchinato, R.; Pejrona, M.; Ismael, M.; Berjano, P. Predictive Accuracy of Surgimap Surgical Planning for Sagittal Imbalance: A Cohort Study. Spine 2017, 42, E1297–E1304. [Google Scholar] [CrossRef]
- Bess, S.; Boachie-Adjei, O.; Burton, D.; Cunningham, M.; Shaffrey, C.; Shelokov, A.; Hostin, R.; Schwab, F.; Wood, K.; Akbarnia, B. Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine 2009, 34, 2186–2190. [Google Scholar] [CrossRef] [Green Version]
- Togawa, D.; Hasegawa, T.; Yamato, Y.; Yoshida, G.; Kobayashi, S.; Yasuda, T.; Oe, S.; Banno, T.; Arima, H.; Mihara, Y.; et al. Postoperative Disability After Long Corrective Fusion to the Pelvis in Elderly Patients with Spinal Deformity. Spine 2018, 43, E804–E812. [Google Scholar] [CrossRef]
- Finkelstein, J.A.; Schwartz, C.E. Patient-reported outcomes in spine surgery: Past, current, and future directions. J. Neurosurg. Spine 2019, 31, 155–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gum, J.L.; Carreon, L.Y.; Glassman, S.D. State-of-the-art: Outcome assessment in adult spinal deformity. Spine Deform. 2020, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Langella, F.; Barletta, P.; Baroncini, A.; Agarossi, M.; Scaramuzzo, L.; Luca, A.; Bassani, R.; Peretti, G.M.; Lamartina, C.; Villafañe, J.H.; et al. The use of electronic PROMs provides same outcomes as paper version in a spine surgery registry. Results from a prospective cohort study. Eur. Spine J. 2021, 30, 2645–2653. [Google Scholar] [CrossRef]
- Diebo, B.G.; Varghese, J.J.; Lafage, R.; Schwab, F.J.; Lafage, V. Sagittal alignment of the spine: What do you need to know? Clin. Neurol. Neurosurg. 2015, 139, 295–301. [Google Scholar] [CrossRef]
- Garbossa, D.; Pejrona, M.; Damilano, M.; Sansone, V.; Ducati, A.; Berjano, P. Pelvic parameters and global spine balance for spine degenerative disease: The importance of containing for the well being of content. Eur. Spine J. 2014, 23 (Suppl. 6), 616–627. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.; Valore, A.; Villaminar, A.; Comisso, M.; Balsano, M. Sagittal balance and pelvic parameters--a paradigm shift in spinal surgery. J. Clin. Neurosci. 2013, 20, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Yamato, Y.; Hasegawa, T.; Togawa, D.; Yoshida, G.; Banno, T.; Arima, H.; Oe, S.; Mihara, Y.; Ushirozako, H.; Kobayashi, S.; et al. Rigorous Correction of Sagittal Vertical Axis Is Correlated with Better ODI Outcomes After Extensive Corrective Fusion in Elderly or Extremely Elderly Patients with Spinal Deformity. Spine Deform. 2019, 7, 610–618. [Google Scholar] [CrossRef]
- Yagi, M.; Michikawa, T.; Suzuki, S.; Okada, E.; Nori, S.; Tsuji, O.; Nagoshi, N.; Asazuma, T.; Hosogane, N.; Fujita, N.; et al. Characterization of Patients with Poor Risk for Clinical Outcomes in Adult Symptomatic Lumbar Deformity Surgery. Spine 2021, 46, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [Green Version]
- Mannion, A.F.; Porchet, F.; Kleinstück, F.S.; Lattig, F.; Jeszenszky, D.; Bartanusz, V.; Dvorak, J.; Grob, D. The quality of spine surgery from the patient’s perspective: Part 2. Minimal clinically important difference for improvement and deterioration as measured with the Core Outcome Measures Index. Eur. Spine J. 2009, 18 (Suppl. 3), 374–379. [Google Scholar] [CrossRef] [Green Version]
- Ledonio, C.G.T.; Polly, D.W.; Crawford, C.H.; Duval, S.; Smith, J.S.; Buchowski, J.; Yson, S.C.; Larson, A.N.; Sembrano, J.N.; Santos, E.R.G. Adult Degenerative Scoliosis Surgical Outcomes: A Systematic Review and Meta-analysis. Spine Deform. 2013, 1, 248–258. [Google Scholar] [CrossRef]
- Smith, J.S.; Kelly, M.P.; Yanik, E.L.; Baldus, C.R.; Buell, T.J.; Lurie, J.D.; Edwards, C.; Glassman, S.D.; Lenke, L.G.; Boachie-Adjei, O.; et al. Operative versus nonoperative treatment for adult symptomatic lumbar scoliosis at 5-year follow-up: Durability of outcomes and impact of treatment-related serious adverse events. J. Neurosurg. Spine 2021, 35, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Dinizo, M.; Dolgalev, I.; Passias, P.G.; Errico, T.J.; Raman, T. Complications after Adult Spinal Deformity Surgeries: All Are Not Created Equal. Int. J. Spine Surg. 2021, 15, 137–143. [Google Scholar] [CrossRef]
- Alas, H.; Passias, P.G.; Brown, A.E.; Pierce, K.E.; Bortz, C.; Bess, S.; Lafage, R.; Lafage, V.; Ames, C.P.; Burton, D.C.; et al. Predictors of serious, preventable, and costly medical complications in a population of adult spinal deformity patients. Spine J. 2021, 21, 1559–1566. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.E.; Alas, H.; Pierce, K.E.; Bortz, C.A.; Hassanzadeh, H.; Labaran, L.A.; Puvanesarajah, V.; Vasquez-Montes, D.; Wang, E.; Raman, T.; et al. Obesity negatively affects cost efficiency and outcomes following adult spinal deformity surgery. Spine J. 2020, 20, 512–518. [Google Scholar] [CrossRef]
- Hashimoto, J.; Yoshii, T.; Sakai, K.; Hirai, T.; Yuasa, M.; Inose, H.; Kawabata, A.; Utagawa, K.; Matsukura, Y.; Tomori, M.; et al. Impact of body mass index on surgical outcomes and complications in adult spinal deformity. J. Orthop. Sci. 2021, in press. [CrossRef]
- Khan, J.M.; Basques, B.A.; Harada, G.K.; Louie, P.K.; Chen, I.; Vetter, C.; Kadakia, K.; Elboghdady, I.; Colman, M.; An, H.S. Does increasing age impact clinical and radiographic outcomes following lumbar spinal fusion? Spine J. 2020, 20, 563–571. [Google Scholar] [CrossRef]
- Drazin, D.; Shirzadi, A.; Rosner, J.; Eboli, P.; Safee, M.; Baron, E.M.; Liu, J.C.; Acosta, F.L. Complications and outcomes after spinal deformity surgery in the elderly: Review of the existing literature and future directions. Neurosurg. Focus 2011, 31, E3. [Google Scholar] [CrossRef] [Green Version]
- Lovato, Z.R.; Deckey, D.G.; Chung, A.S.; Crandall, D.G.; Revella, J.; Chang, M.S. Adult spine deformity surgery in elderly patients: Are outcomes worse in patients 75 years and older? Spine Deform. 2020, 8, 1353–1359. [Google Scholar] [CrossRef] [PubMed]
- Lingutla, K.K.; Pollock, R.; Benomran, E.; Purushothaman, B.; Kasis, A.; Bhatia, C.K.; Krishna, M.; Friesem, T. Outcome of lumbar spinal fusion surgery in obese patients: A systematic review and meta-analysis. Bone Jt. J. 2015, 97-B, 1395–1404. [Google Scholar] [CrossRef]
- Pierce, K.E.; Passias, P.G.; Alas, H.; Brown, A.E.; Bortz, C.A.; Lafage, R.; Lafage, V.; Ames, C.; Burton, D.C.; Hart, R.; et al. Does Patient Frailty Status Influence Recovery Following Spinal Fusion for Adult Spinal Deformity?: An Analysis of Patients With 3-Year Follow-up. Spine 2020, 45, E397–E405. [Google Scholar] [CrossRef] [PubMed]
- Scheer, J.K.; Smith, J.S.; Schwab, F.; Lafage, V.; Shaffrey, C.I.; Bess, S.; Daniels, A.H.; Hart, R.A.; Protopsaltis, T.S.; Mundis, G.M.; et al. Development of a preoperative predictive model for major complications following adult spinal deformity surgery. J. Neurosurg. Spine 2017, 26, 736–743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, F.; Firouzabadi, A.; Reitmaier, S.; Zander, T.; Schmidt, H. The shape and mobility of the thoracic spine in asymptomatic adults—A systematic review of in vivo studies. J. Biomech. 2018, 78, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, G.; Boissiere, L.; Larrieu, D.; Bourghli, A.; Vital, J.M.; Gille, O.; Pointillart, V.; Challier, V.; Mariey, R.; Pellisé, F.; et al. Advantages and Disadvantages of Adult Spinal Deformity Surgery and Its Impact on Health-Related Quality of Life. Spine 2017, 42, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Kyrölä, K.; Kautiainen, H.; Pekkanen, L.; Mäkelä, P.; Kiviranta, I.; Häkkinen, A. Long-term clinical and radiographic outcomes and patient satisfaction after adult spinal deformity correction. Scand. J. Surg. SJS 2019, 108, 343–351. [Google Scholar] [CrossRef] [PubMed]
| ICD Diagnosis Codes | |
| 737.30, 737.31, 737.32, 737.34, 737.0, 737.10, 737.12, 737.22, 737.40, 737.41, 737.43, 737.19, 738.5, 737.39 | |
| ICD Procedure Codes | |
| Primary surgery | 81.05, 81.06, 81.08, 81.63, 81.64 |
| Revision surgery | 996.49, V45.4, 996.78, 998.89 |
| Demographic Data | |
|---|---|
| Age (years) | 53.4 ± 16.7 |
| Sex | 149 women (78%), 43 men (22%) |
| BMI (kg/cm2) | 24.2 ± 3.9 |
| Perioperative Data | |
|---|---|
| UIV | C7: 1; T1: 5; T2: 7; T3: 28; T4: 29; T5: 15; T6: 4; T7: 3; T8: 11; T9: 16; T10: 44; T11: 5; T12: 3; L1: 5; L2: 13; L3: 3 |
| LIV | L3: 11; L4: 35; L5: 24; S1: 62; Ilium: 60 |
| Access | Posterior only: 192; postero-anterior: 21; postero-lateral: 38 |
| Curve correction method | SPO: 21; PSO: 13; ALIF: 21; LLIF 38 |
| Length of surgery (min) | 430 ± 150 |
| % EBL | 18 ± 15.3 |
| EBL (mL) | 1264 ± 1073 |
| Length of hospital stay (days) | 8.5 ± 4.5 |
| ODI, VAS and CB11 Overview | ||||
|---|---|---|---|---|
| Preop | 1-year FU | 2-years FU | p (Preop vs. 2-year FU) | |
| ODI | 42.5 ± 20.3 | 26.7 ± 21.4 | 26.8 ± 20.7 | <0.0001 |
| VAS back | 6.8 ± 2.7 | 3.8 ± 3 | 4 ± 3.1 | <0.0001 |
| VAS leg | 4.8 ± 3.7 | 3.4 ± 3.1 | 3.6 ± 3.5 | 0.01 |
| CB11 | - | 0.9 ± 1.1 | 0.9 ± 1.2 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baroncini, A.; Migliorini, F.; Langella, F.; Barletta, P.; Trobisch, P.; Cecchinato, R.; Damilano, M.; Quarto, E.; Lamartina, C.; Berjano, P. Perioperative Predictive Factors for Positive Outcomes in Spine Fusion for Adult Deformity Correction. J. Clin. Med. 2022, 11, 144. https://doi.org/10.3390/jcm11010144
Baroncini A, Migliorini F, Langella F, Barletta P, Trobisch P, Cecchinato R, Damilano M, Quarto E, Lamartina C, Berjano P. Perioperative Predictive Factors for Positive Outcomes in Spine Fusion for Adult Deformity Correction. Journal of Clinical Medicine. 2022; 11(1):144. https://doi.org/10.3390/jcm11010144
Chicago/Turabian StyleBaroncini, Alice, Filippo Migliorini, Francesco Langella, Paolo Barletta, Per Trobisch, Riccardo Cecchinato, Marco Damilano, Emanuele Quarto, Claudio Lamartina, and Pedro Berjano. 2022. "Perioperative Predictive Factors for Positive Outcomes in Spine Fusion for Adult Deformity Correction" Journal of Clinical Medicine 11, no. 1: 144. https://doi.org/10.3390/jcm11010144
APA StyleBaroncini, A., Migliorini, F., Langella, F., Barletta, P., Trobisch, P., Cecchinato, R., Damilano, M., Quarto, E., Lamartina, C., & Berjano, P. (2022). Perioperative Predictive Factors for Positive Outcomes in Spine Fusion for Adult Deformity Correction. Journal of Clinical Medicine, 11(1), 144. https://doi.org/10.3390/jcm11010144








