EBRA Migration Analysis of a Modular, Distally Fixed Stem in Hip Revision Arthroplasty: A Clinical and Radiological Study
Abstract
1. Introduction
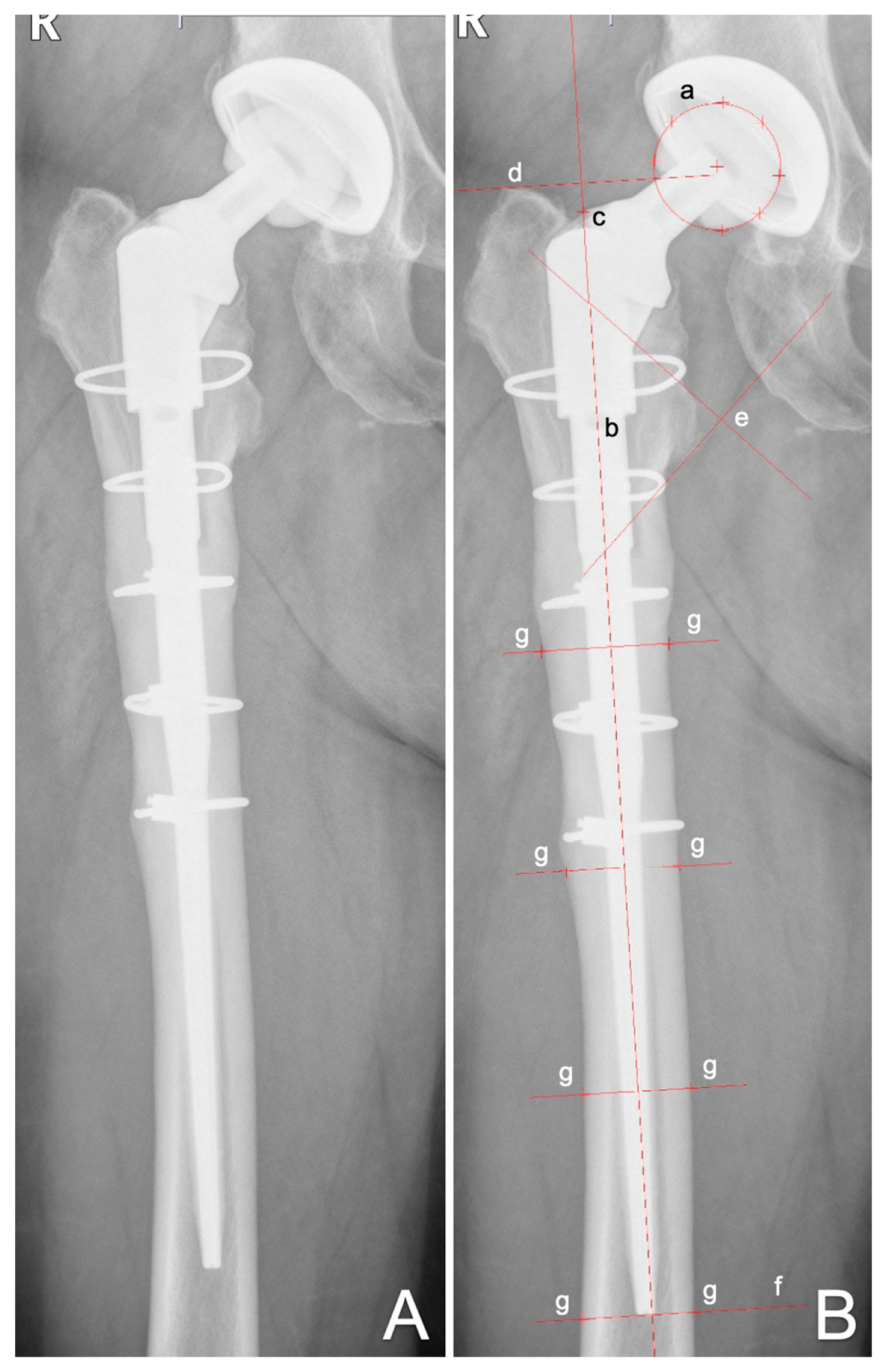
2. Materials and Methods
Statistics
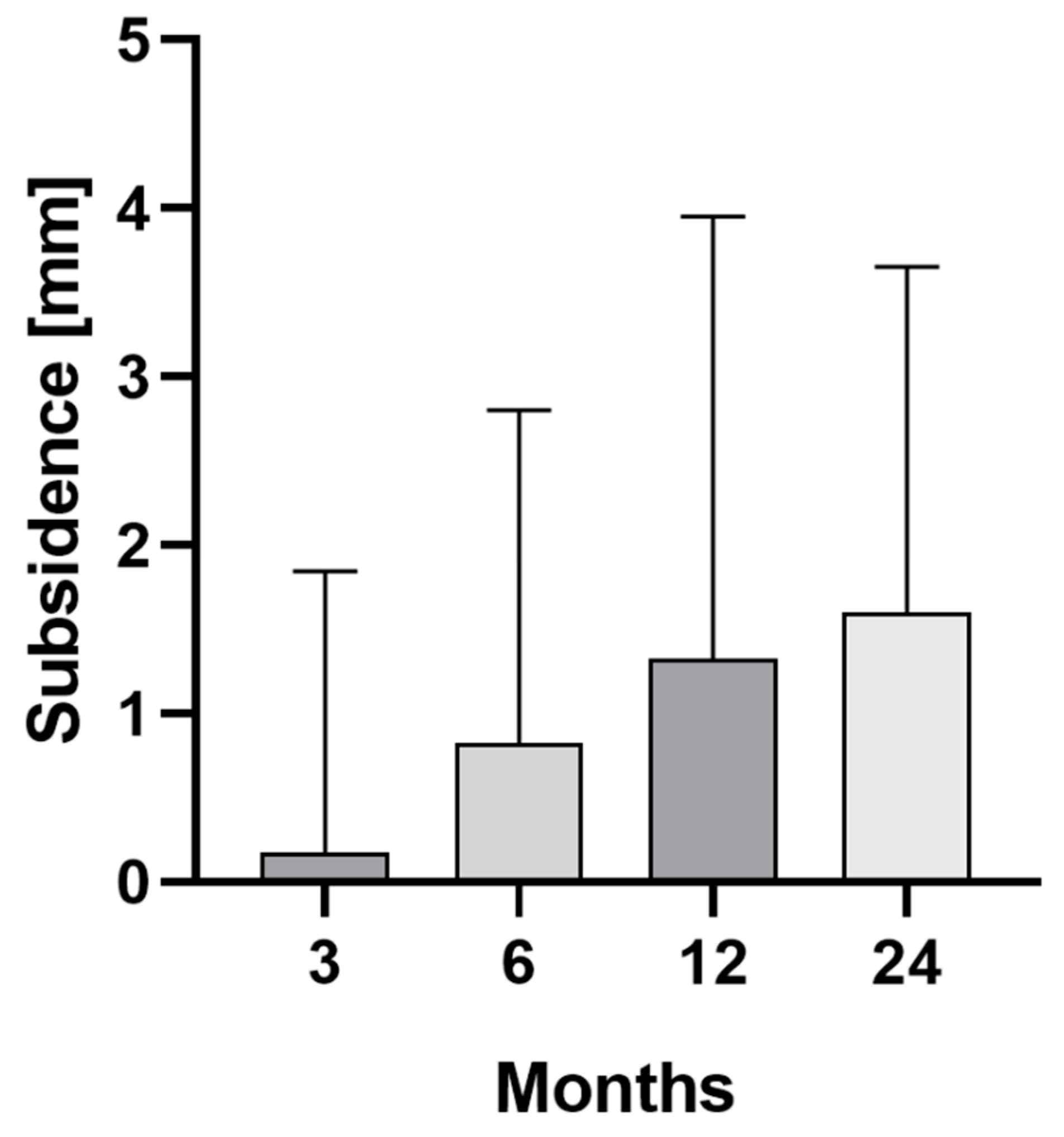
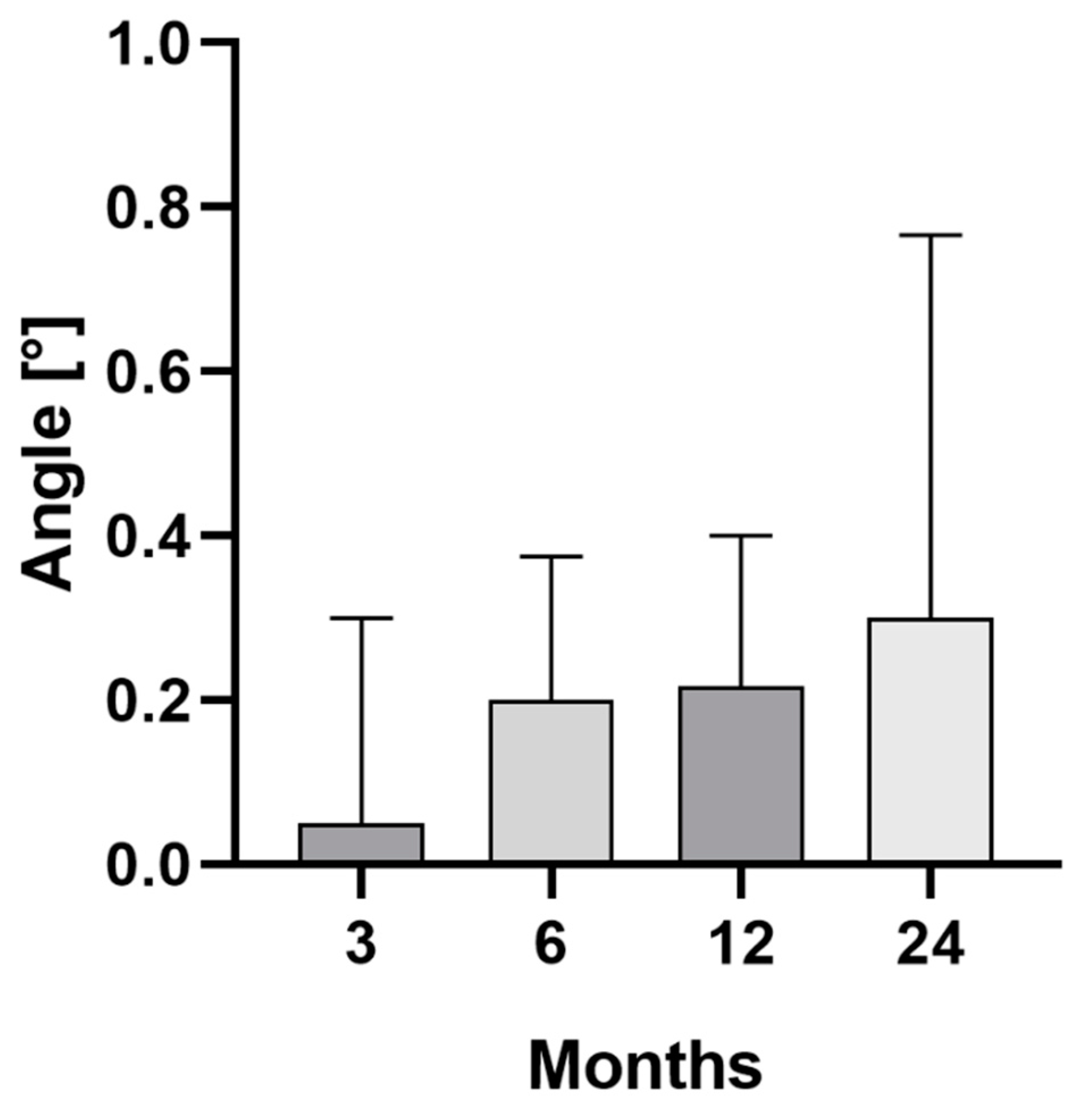
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Joint Surg. Am. 2007, 89, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Pabinger, C.; Lothaller, H.; Portner, N.; Geissler, A. Projections of hip arthroplasty in OECD countries up to 2050. Hip Int. 2018, 28, 498–506. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.M.; Mistry, J.B.; Cherian, J.J.; Elmallah, R.K.; Chughtai, M.; Harwin, S.F.; Mont, M.A. Femoral Component Revision of Total Hip Arthroplasty. Orthopedics 2016, 39, e1129–e1139. [Google Scholar] [CrossRef] [PubMed]
- Sheth, N.P.; Nelson, C.L.; Paprosky, W.G. Femoral bone loss in revision total hip arthroplasty: Evaluation and management. J. Am. Acad. Orthop. Surg. 2013, 21, 601–612. [Google Scholar] [CrossRef] [PubMed]
- Wagner, H. Revision prosthesis for the hip joint in severe bone loss. Orthopade 1987, 16, 295–300. [Google Scholar] [PubMed]
- Kärrholm, J.; Rogmark, C.; Nauclér, E.; Natman, J.; Johanna, V.; Mohaddes, M.; Rolfson, O. Swedish Hip Arthroplasty Register Annual Report 2019. 2019. Available online: https://registercentrum.blob.core.windows.net/shpr/r/VGR_Annual-report_SHAR_2019_EN_Digital-pages_FINAL-ryxaMBUWZ_.pdf (accessed on 14 April 2022).
- Kenney, C.; Dick, S.; Lea, J.; Liu, J.; Ebraheim, N.A. A systematic review of the causes of failure of Revision Total Hip Arthroplasty. J. Orthop. 2019, 16, 393–395. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.A.; Plante-Bordeneuve, P. Early migration and late aseptic failure of proximal femoral prostheses. J. Bone Joint Surg. Br. 1994, 76, 432–438. [Google Scholar] [CrossRef]
- Walker, P.S.; Mai, S.F.; Cobb, A.G.; Bentley, G.; Hua, J. Prediction of clinical outcome of THR from migration measurements on standard radiographs. A study of cemented Charnley and Stanmore femoral stems. J. Bone Joint Surg. Br. 1995, 77, 705–714. [Google Scholar] [CrossRef]
- Kroell, A.; Beaulé, P.; Krismer, M.; Behensky, H.; Stoeckl, B.; Biedermann, R. Aseptic stem loosening in primary THA: Migration analysis of cemented and cementless fixation. Int. Orthop. 2009, 33, 1501–1505. [Google Scholar] [CrossRef]
- Streit, M.R.; Haeussler, D.; Bruckner, T.; Proctor, T.; Innmann, M.M.; Merle, C.; Gotterbarm, T.; Weiss, S. Early Migration Predicts Aseptic Loosening of Cementless Femoral Stems: A Long-term Study. Clin. Orthop. Relat. Res. 2016, 474, 1697–1706. [Google Scholar] [CrossRef]
- Biedermann, R.; Krismer, M.; Stöckl, B.; Mayrhofer, P.; Ornstein, E.; Franzén, H. Accuracy of EBRA-FCA in the measurement of migration of femoral components of total hip replacement. Einzel-Bild-Röntgen-Analyse-femoral component analysis. J. Bone Joint Surg. Br. 1999, 81, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Abrahams, J.M.; Callary, S.A.; Won Jang, S.; Hewitt, J.; Howie, D.W.; Solomon, L.B. Accuracy of EBRA-Cup Measurements after Reconstruction of Severe Acetabular Defects at Revision THR. J. Orthop. Res. 2020, 38, 1497–1505. [Google Scholar] [CrossRef]
- Waldemar Link GmbH & Co KG. MP Reconstruction Prosthesis—Surgical Technique. Available online: http://www.linkhh.com.ua/images/stories/pdf/664_MP_OP.pdf (accessed on 14 April 2022).
- Gruen, T.A.; McNeice, G.M.; Amstutz, H.C. “Modes of failure” of cemented stem-type femoral components: A radiographic analysis of loosening. Clin. Orthop. Relat. Res. 1979, 141, 17–27. [Google Scholar] [CrossRef]
- Krismer, M.; Biedermann, R.; Stöckl, B.; Fischer, M.; Bauer, R.; Haid, C. The prediction of failure of the stem in THR by measurement of early migration using EBRA-FCA. Einzel-Bild-Roentgen-Analyse-femoral component analysis. J. Bone Joint Surg. Br. 1999, 81, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Meermans, G.; Konan, S.; Das, R.; Volpin, A.; Haddad, F.S. The direct anterior approach in total hip arthroplasty: A systematic review of the literature. Bone Joint J. 2017, 99, 732–740. [Google Scholar] [CrossRef] [PubMed]
- Hardinge, K. The direct lateral approach to the hip. J. Bone Joint Surg. Br. 1982, 64, 17–19. [Google Scholar] [CrossRef]
- Kwong, L.M.; Miller, A.J.; Lubinus, P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: A 2- to 6-year follow-up study. J. Arthroplast. 2003, 18 (Suppl. 1), 94–97. [Google Scholar] [CrossRef]
- Girard, J.; Roche, O.; Wavreille, G.; Canovas, F.; Le Béguec, P. Stem subsidence after total hip revision: 183 cases at 5. 9 years follow-up. Orthop. Traumatol. Surg. Res. 2011, 97, 121–126. [Google Scholar] [CrossRef]
- Zheng, K.; Li, N.; Zhang, W.; Zhu, Y.; Zhou, J.; Xu, Y.; Geng, D. Mid- to Long-Term Outcomes of Cementless Modular, Fluted, Tapered Stem for Massive Femoral Bone Loss in Revision Total Hip Arthroplasty. Orthop. Surg. 2021, 13, 989–1000. [Google Scholar] [CrossRef]
- Capone, A.; Congia, S.; Civinini, R.; Marongiu, G. Periprosthetic fractures: Epidemiology and current treatment. Clin. Cases Miner Bone Metab. 2017, 14, 189–196. [Google Scholar] [CrossRef]
- Selvik, G. Roentgen stereophotogrammetric analysis. Acta Radiol. 1990, 31, 113–126. [Google Scholar] [CrossRef] [PubMed]
- Houdek, M.T.; Perry, K.I.; Wyles, C.C.; Berry, D.J.; Sierra, R.J.; Trousdale, R.T. Use of a modular tapered fluted femoral component in revision total hip arthroplasty following resection of a previously infected total hip: Minimum 5-year follow-up. J. Arthroplast. 2015, 30, 435–438. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.J.; Beckman, M.O.; Enocson, A.; Schmalholz, A.; Stark, A. Minimum 5-year follow-up of a cementless, modular, tapered stem in hip revision arthroplasty. J. Arthroplast. 2011, 26, 16–23. [Google Scholar] [CrossRef]
- Patel, P.D.; Klika, A.K.; Murray, T.G.; Elsharkawy, K.A.; Krebs, V.E.; Barsoum, W.K. Influence of technique with distally fixed modular stems in revision total hip arthroplasty. J. Arthroplast. 2010, 25, 926–931. [Google Scholar] [CrossRef]
- Jayasinghe, G.; Buckle, C.; Maling, L.C.; To, C.; Anibueze, C.; Vinayakam, P.; Slack, R. Medium Term Radiographic and Clinical Outcomes Using a Modular Tapered Hip Revision Implant. Arthroplast. Today 2021, 8, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Fink, B.; Grossmann, A.; Schubring, S.; Schulz, M.S.; Fuerst, M. Short-term results of hip revisions with a curved cementless modular stem in association with the surgical approach. Arch. Orthop. Trauma Surg. 2009, 129, 65–73. [Google Scholar] [CrossRef]
- Meding, J.B.; Ritter, M.A.; Keating, E.M.; Faris, P.M. Clinical and radiographic evaluation of long-stem femoral components following revision total hip arthroplasty. J. Arthroplast. 1994, 9, 399–408. [Google Scholar] [CrossRef]
- Schuh, A.; Werber, S.; Holzwarth, U.; Zeiler, G. Cementless modular hip revision arthroplasty using the MRP Titan Revision Stem: Outcome of 79 hips after an average of 4 years’ follow-up. Arch. Orthop. Trauma Surg. 2004, 124, 306–309. [Google Scholar] [CrossRef]
- Sivananthan, S.; Lim, C.T.; Narkbunnam, R.; Sox-Harris, A.; Huddleston, J.I.; Goodman, S.B. Revision Hip Arthroplasty Using a Modular, Cementless Femoral Stem: Intermediate-Term Follow-Up. J. Arthroplast. 2017, 32, 1245–1249. [Google Scholar] [CrossRef]
- Stimac, J.D.; Boles, J.; Parkes, N.; Gonzalez Della Valle, A.; Boettner, F.; Westrich, G.H. Revision total hip arthroplasty with modular femoral stems. J. Arthroplast. 2014, 29, 2167–2170. [Google Scholar] [CrossRef]
- Efe, T.; Schmitt, J. Analyses of prosthesis stem failures in noncemented modular hip revision prostheses. J. Arthroplast. 2011, 26, e7–e12. [Google Scholar] [CrossRef] [PubMed]
- Konan, S.; Garbuz, D.S.; Masri, B.A.; Duncan, C.P. Modular tapered titanium stems in revision arthroplasty of the hip: The Risk and Causes of Stem Fracture. Bone Joint J. 2016, 98 (Suppl. A), 50–53. [Google Scholar] [CrossRef] [PubMed]
- Lakstein, D.; Eliaz, N.; Levi, O.; Backstein, D.; Kosashvili, Y.; Safir, O.; Gross, A.E. Fracture of cementless femoral stems at the mid-stem junction in modular revision hip arthroplasty systems. J. Bone Joint Surg. Am. 2011, 93, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Van Houwelingen, A.P.; Duncan, C.P.; Masri, B.A.; Greidanus, N.V.; Garbuz, D.S. High survival of modular tapered stems for proximal femoral bone defects at 5 to 10 years followup. Clin. Orthop. Relat. Res. 2013, 471, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Buttaro, M.A.; Mayor, M.B.; Van Citters, D.; Piccaluga, F. Fatigue fracture of a proximally modular, distally tapered fluted implant with diaphyseal fixation. J. Arthroplast. 2007, 22, 780–783. [Google Scholar] [CrossRef]
| Number of patients | Female | 26 |
| Male | 36 | |
| Total | 62 | |
| Mean age (years) | 68 (39–89) | |
| BMI (kg/m2) | 28 (19–47) | |
| Cut-to-suture time (min) | 189 (78–428) | |
| Surgical approach | Direct anterior approach | 25 |
| Extended direct anterior approach | 11 | |
| Tensor release | 5 | |
| Lateral approach | 19 | |
| Posterior approach | 6 | |
| Anterolateral approach | 1 | |
| Surgical position | Supine | 61 |
| Lateral | 6 | |
| Preoperative diagnosis | Periprosthetic fracture | 22 |
| Periprosthetic infection | 19 | |
| Aseptic loosening | 17 | |
| Hip dysplasia | 2 | |
| Femoral neck fracture | 2 | |
| Material breakage | 1 | |
| Failed osteosynthesis | 1 | |
| Pathologic fracture | 1 | |
| Osteoarthritis | 1 | |
| Recurrent dislocation | 1 | |
| Vancouver classification | Type B2 | 20 |
| Type B3 | 2 |
| Stem product | MP | 67 (100) |
| Anchoring method | Cementless | 67 (100) |
| CCD angle | 126° | 45 (67) |
| 135° | 12 (18) | |
| n.a. | 10 (15) | |
| Neck length (mm) | 35 | 40 (60) |
| 65 | 17 (25) | |
| n.a. | 10 (15) | |
| Stem length (mm) | 180 | 14 (21) |
| 210 | 28 (42) | |
| 250 | 13 (19) | |
| 290 | 3 (4) | |
| 330 | 1 (2) | |
| n.a. | 8 (12) | |
| Head size (mm) | 28 | 40 (60) |
| 32 | 15 (22) | |
| 36 | 3 (5) | |
| n.a. | 9 (13) | |
| Head material | Biolox | 41 (61) |
| CoCrMo | 15 (22) | |
| n.a. | 11 (17) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blum, P.; Putzer, D.; Neugebauer, J.; Neubauer, M.; Süß, M.; Dammerer, D. EBRA Migration Analysis of a Modular, Distally Fixed Stem in Hip Revision Arthroplasty: A Clinical and Radiological Study. J. Clin. Med. 2022, 11, 5857. https://doi.org/10.3390/jcm11195857
Blum P, Putzer D, Neugebauer J, Neubauer M, Süß M, Dammerer D. EBRA Migration Analysis of a Modular, Distally Fixed Stem in Hip Revision Arthroplasty: A Clinical and Radiological Study. Journal of Clinical Medicine. 2022; 11(19):5857. https://doi.org/10.3390/jcm11195857
Chicago/Turabian StyleBlum, Philipp, David Putzer, Johannes Neugebauer, Markus Neubauer, Markus Süß, and Dietmar Dammerer. 2022. "EBRA Migration Analysis of a Modular, Distally Fixed Stem in Hip Revision Arthroplasty: A Clinical and Radiological Study" Journal of Clinical Medicine 11, no. 19: 5857. https://doi.org/10.3390/jcm11195857
APA StyleBlum, P., Putzer, D., Neugebauer, J., Neubauer, M., Süß, M., & Dammerer, D. (2022). EBRA Migration Analysis of a Modular, Distally Fixed Stem in Hip Revision Arthroplasty: A Clinical and Radiological Study. Journal of Clinical Medicine, 11(19), 5857. https://doi.org/10.3390/jcm11195857







