Is It Possible to Diagnose Preoperatively a Tubal Ectopic Hydatidiform Molar Pregnancy? Description of a Case Report and Review of the Literature of the Last Ten Years
Abstract
:1. Introduction
2. Materials and Methods
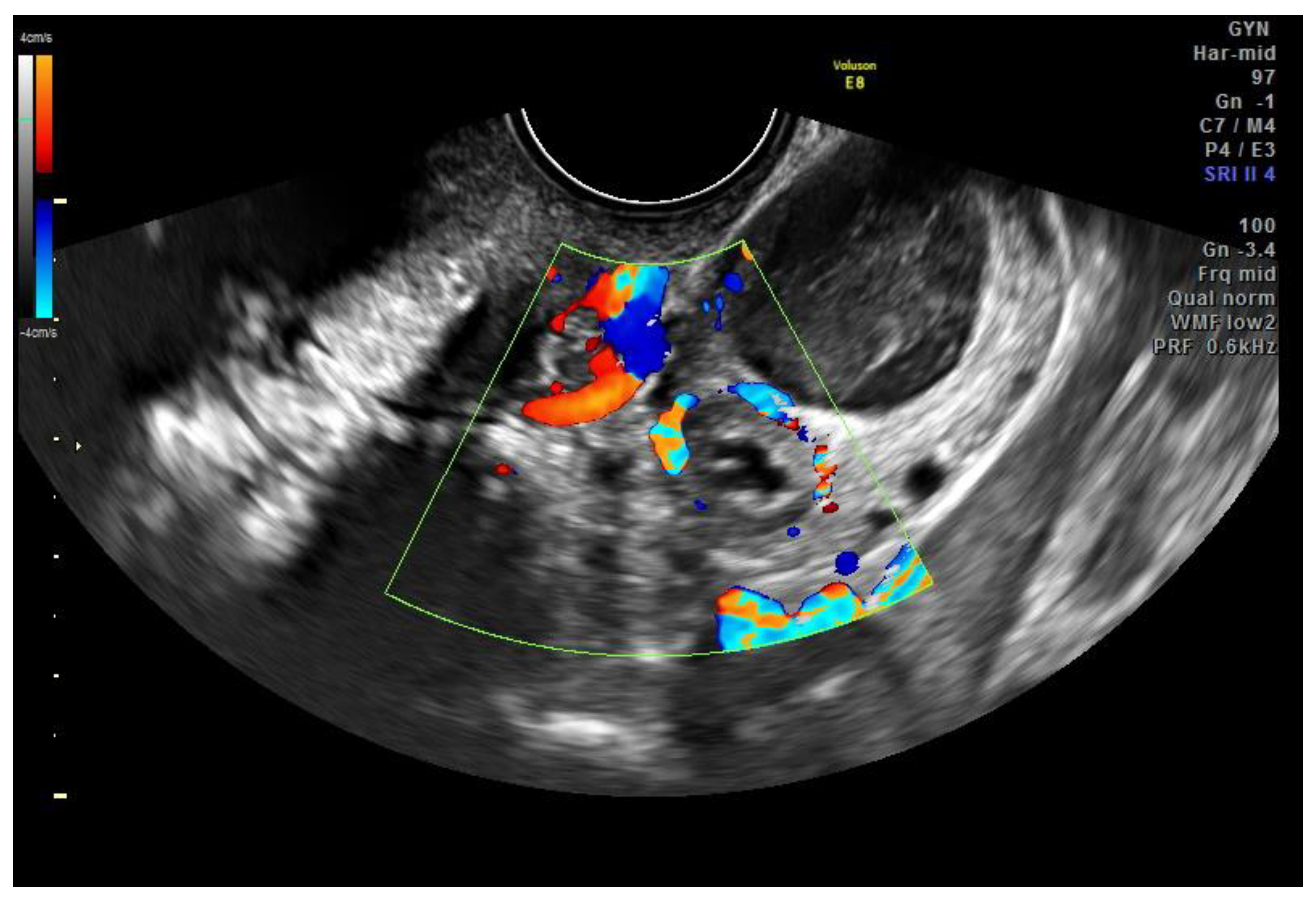
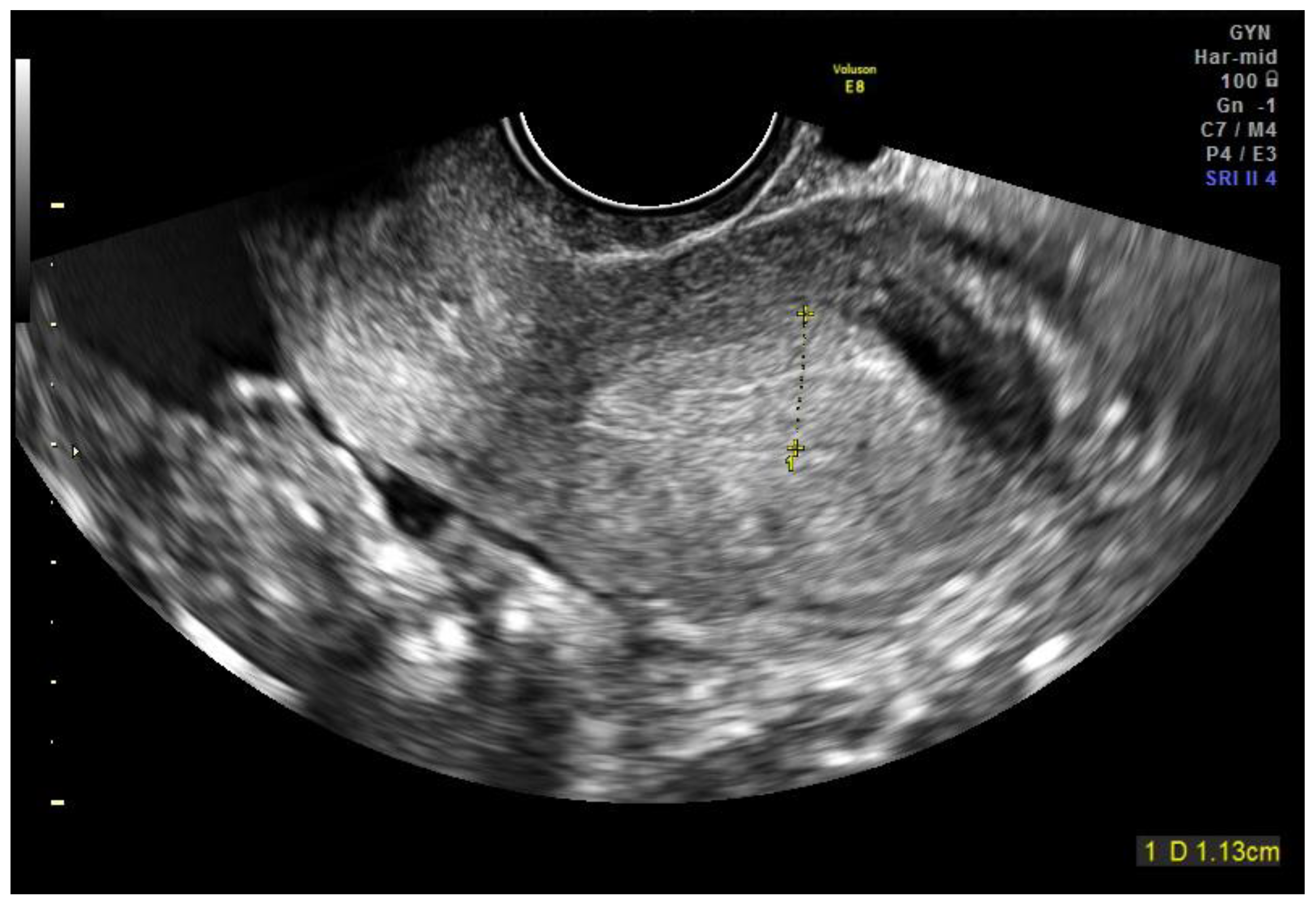
2.1. Case Report
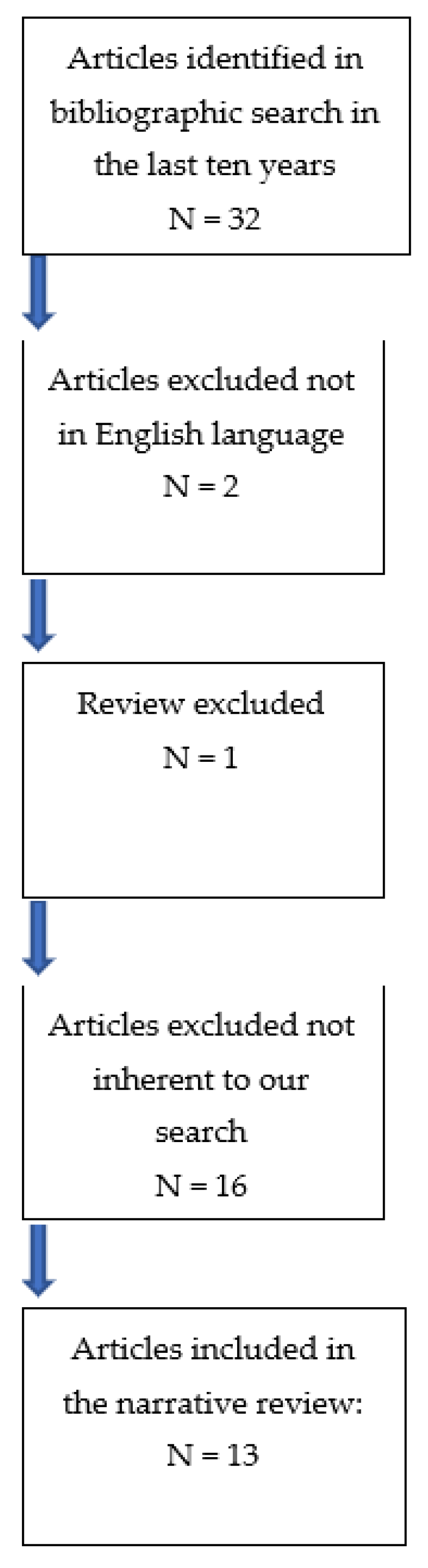
2.2. Review of the Literature
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Seckl, M.J.; Sebire, N.J.; Berkowitz, R.S. Gestational trophoblastic disease. Lancet 2010, 376, 717–729. [Google Scholar] [CrossRef]
- Jacobs, P.A.; Wilson, C.M.; Sprenkle, J.A.; Rosenshein, N.B.; Migeon, B.R. Mechanism of origin of complete hydatidiform moles. Nature 1980, 286, 714–716. [Google Scholar] [CrossRef]
- Depypere, H.T.; Dhont, M.; Verschraegen-Spae, M.R.; Coppens, M. Tubal hydatidiform mole. Am. J. Obstet. Gynecol. 1993, 169, 209–210. [Google Scholar] [CrossRef]
- Smith, H.O. Gestational Trophoblastic Disease Epidemiology and Trends. Clin. Obstet. Gynecol. 2003, 46, 541–556. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Ex-planation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Allen, L.; Dawson, C.; Nascu, P.; Rouse, T. A Molar Pregnancy within the Fallopian Tube. Case Rep. Obs. Gynecol. 2016, 2016, 4367181. [Google Scholar] [CrossRef]
- Siozos, A.; Sriemevan, A. A case of true tubal hydatidiform mole and literature review. BMJ Case Rep. 2010, 2010, bcr0720092123. [Google Scholar] [CrossRef]
- Bousfiha, N.; Erarhay, S.; Louba, A.; Saadi, H.; Bouchikhi, C.; Banani, A.; El Fatemi, H.; Sekkal, M.; Laamarti, A. Ectopic molar pregnancy: A case report. Pan. Afr. Med. J. 2012, 11, 63. [Google Scholar]
- Tulon, B.; Vandana, R.; Subrat, P.; Pallab, S. Ectopic molar pregnancy: A rare entity. J. Reprod. Infertil. 2010, 11, 201–203. [Google Scholar]
- Juan, C.-W. Fallopian tube invasive molar disease. Int. J. Gynecol. Obstet. 2013, 122, 161–162. [Google Scholar] [CrossRef]
- López, C.L.; Lopes, V.G.S.; Resende, F.R.; Steim, J.L.; Padrón, L.; Sun, S.Y.; Júnior, E.A.; Braga, A. Gestational Trophoblastic Neoplasia after Ectopic Molar Pregnancy: Clinical, Diagnostic, and Therapeutic Aspects. Rev. Bras. Ginecol. Obstet. 2018, 40, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Al-Maghrabi, H.; Saleh, D.; Meliti, A. Gestational Trophoblastic Disease Presents as an Ectopic Tubal Pregnancy, a Rare Entity. Case Rep. Obstet. Gynecol. 2019, 2019, 7153170. [Google Scholar] [CrossRef] [PubMed]
- Nakeer, T.; Shahid, M.; Ansari, M.A.; Nakeer, R. Hydatidiform mole presentation as a tubal ectopic pregnancy. J. Coll. Physicians Surg. Pak. 2014, 24 (Suppl. 2), S89–S90. [Google Scholar]
- Beena, D.; Teerthanath, S.; Jose, V.; Shetty, J. Molar Pregnancy Presents as Tubal Ectopic Pregnancy: A Rare Case Report. J. Clin. Diagn. Res. 2016, 10, ED10–ED11. [Google Scholar] [CrossRef] [PubMed]
- Tanha, F.D.; ShirAli, E.; Rahmanpour, H.; Haghollahi, F. Molar Pregnancy Presents as Tubal Ectopic Pregnancy. Int. J. Fertil. Steril. 2011, 4, 184–186. [Google Scholar]
- Mbarki, C.; Jerbi, E.; Hsayaoui, N.; Zouari, F.; Ben Brahim, E.; Oueslati, H. Molar tubal ectopic pregnancy: Report of two cases. J. Obstet. Gynaecol. Res. 2014, 41, 985–988. [Google Scholar] [CrossRef]
- Yakasai, I.; Adamu, N.; Galadanchi, H. Ruptured tubal molar pregnancy. Niger. J. Clin. Pract. 2012, 15, 491–493. [Google Scholar] [CrossRef]
- Zhao, T.; Hou, X.; Su, C.; Wu, Q. Tubal hydatidiform mole treated with salpingotomy: A case report. Clin. Case Rep. 2019, 7, 653–655. [Google Scholar] [CrossRef]
- Charry, R.C.; Figueira, L.M.; García-Barriola, V.; Gomez, C.; Garcia, I.; Santiago, C. Gestational trophoblastic disease in ectopic pregnancy: A case series. J. Reprod. Med. 2006, 51, 760–763. [Google Scholar]
- Gillespie, A.M.; Lidbury, E.A.; Tidy, J.A.; Hancock, B.W. The clinical presentation, treatment, and outcome of patients diagnosed with possible ectopic molar gestation. Int. J. Gynecol. Cancer 2004, 14, 366–369. [Google Scholar] [CrossRef]
- Burton, J.L.; A Lidbury, E.; Gillespie, A.M.; A Tidy, J.; Smith, O.; Lawry, J.; Hancock, B.W.; Wells, M. Over-diagnosis of hydatidiform mole in early tubal ectopic pregnancy. Histopathology 2001, 38, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Sherer, D.M.; Stimphil, R.; Hellmann, M.; Gorelick, C.; Serur, E.; Zigalo, A.; Jain, M.; Abulafia, O. Transvaginal Sonographic Findings of Isolated Intramural Uterine Choriocarcinoma Mimicking an Interstitial Pregnancy. J. Ultrasound Med. 2006, 25, 791–794. [Google Scholar] [CrossRef] [PubMed]
- Rees, H.C.; Paradinas, F.J. The diagnosis of hydatidiform mole in early tubal ectopic pregnancy. Histopathology 2001, 39, 320–321. [Google Scholar] [CrossRef] [PubMed]
- Wells, M. The pathology of gestational trophoblastic disease: Recent advances. Pathology 2007, 39, 88–96. [Google Scholar] [CrossRef]
- Lewis, J.L., Jr. Diagnosis and management of gestational trophoblastic disease. Cancer 1993, 71 (Suppl. S4), 1639–1647. [Google Scholar] [CrossRef]
- Cavoretto, P.; Cioffi, R.; Mangili, G.; Petrone, M.; Bergamini, A.; Rabaiotti, E.; Valsecchi, L.; Candiani, M.; Seckl, M.J. A Pictorial Ultra-sound Essay of Gestational Trophoblastic Disease. J. Ultrasound Med. 2020, 39, 597–613. [Google Scholar] [CrossRef]
- Sebire, N.; Lindsay, I.; Fisher, R.; Savage, P.; Seckl, M.J. Overdiagnosis of Complete and Partial Hydatidiform Mole in Tubal Ectopic Pregnancies. Int. J. Gynecol. Pathol. 2005, 24, 260–264. [Google Scholar] [CrossRef]
- Farrukh, A.; Attia, M.; Furniss, H. Tubal hydatidiform mole: An unexpected diagnosis. J. Obstet. Gynaecol. 2007, 27, 747–748. [Google Scholar] [CrossRef]
| Author, Year | Study Design | Clinical Aspects | US | Treatment | Histological Examination | Follow-Up |
|---|---|---|---|---|---|---|
| Laura Allen et al., 2016 [6] | Case report | 29 years BHCG of 32,000 IU/L. Diagnosis of a miscarriage one month before. Abdominal pain | Right-sided adnexal mass measuring 2.2 × 2.4 × 2 cm, and a fluid collection in the uterus. No evidence of a gestational sac | Salpingostomy and D & C | Partial hydatidiform molar (PHM) pregnancy | Serial monitoring of BHCG level; BHCG = 0 one month after surgery |
| A Siozos et al., 2010 [7] | Case report | β-HCG 3352 IU/L. Vaginal bleeding, abdominal pelvic pain | Left mass adjacent to the left ovary of 2.5 cm. Free fluid in the pouch of Douglas | Mini laparotomy with left partial salpingectomy | Complete molar pregnancy (CHM) | No symptoms 6 weeks later |
| Najoua Bousfiha et al., 2011 [8] | Case report | 32 years BHCG 3454 IU/L. Last menstrual period 6 weeks before. Vaginal bleeding and lower abdominal pain | Irregular echogenic mass in the left adnexa (1.5 cm × 2 cm) | Left laparoscopic salpingectomy | Partial molar pregnancy (PHM) | Weekly quantitative Β-hCG titers until three successive Β-hCG levels were negative. |
| Borahe et al., 2010 [9] | Case report | 30 years Last menstrual period 7 weeks before. Mild vaginal bleeding and pelvic pain | Left tubo-ovarian mass with a live fetus corresponding to 7 weeks and 6 days of gestation with free fluid in the pelvic cavity | Laparotomy left side salpingectomy | Complete molar pregnancy (CHM) and tubal rupture | Weekly follow-up by serum βhCG measurement |
| Chi-Wen Juan 2013 [10] | Case report | 20 years BHCG 6984 mIU/mL. Last menstrual period 8 weeks and 4 days before. Abdominal pain | Empty endometrial cavity with cul-de-sac fluid and a left adnexal mass | Left laparoscopic salpingectomy | Tubal invasive mole and tubal rupture | Weekly quantitative β-hCG titers until 3 successive β-hCG levels were negative |
| Consuelo Lozoya López, et al., 2018 [11] | Case report | 34 years BHCG 12,893 IU/L. Last menstrual period 8 weeks before. Abdominal pain, vomiting, and vaginal bleeding | Left paraovarian mass of 65 × 40 × 35 mm in size, filled with amorphous echoes | Laparotomy left side salpingectomy | Partial molar pregnancy (PHM) with a slight ruptured tube | Elevated hCG levels were detected. MTX was initiated |
| Haneen Al-Maghrabi et al., 2019 [12] | Case report | 39 years BHCG 110.766 mIU/mL. Lower abdominal pain, abdominal distention, and low-grade fever for three days | Right adnexal heterogeneous complex mass (7 × 5 × 5 cm) and an adjacent right ovarian cyst (8 × 7 × 5 cm) with free fluid in the abdomen and pelvis | Laparotomy right salpingo-oophorectomy | Complete molar pregnancy (CHM) and tubal rupture | Follow-up by serum BHCG measurements |
| Tabassum Nakeer et al., 2014 [13] | Case report | 32 years Abdominal pain and vaginal bleeding | Abdominal mass of 1.8 cm near to the left ovary and fluid in cul-de-sac | Laparotomy left side salpingectomy | Partial molar pregnancy (PHM) | |
| Devi Beena et al., 2016 [14] | Case report | 32 years Last menstrual period one and a half months before. Abdominal pain and vaginal bleeding | Right adnexal mass 4 × 3 cm and endopelvic free fluid | Laparotomy right salpingectomy | Complete molar pregnancy (CHM) and tubal rupture | Weekly quantitative β-hCG titers until 3 successive β-hCG levels were negative |
| Fatemeh Davari Tanha et al., 2011 [15] | Case report | 29 years BHCG 15,000 mIU/mL. Vaginal bleeding and pelvic pain | Left adnexal mass of 18 × 28 mm, free fluid in the cul-de-sac. No gestational sac in the uterus | Laparotomy left side salpingectomy | Partial molar pregnancy (PHM) with a slight ruptured tube | Serum beta-HCG titers |
| Chaouki Mbarki et al., 2015 [16] | Case report | 32 years BHCG 40,400 mIU/mL. Last menstrual period 6 weeks before. Abdominal pain and mild vaginal bleeding | A left adnexal mass containing an embryo at 6 weeks of gestation with cardiac activity. No intrauterine gestational sac. Thin endometrium | Left laparoscopic salpingectomy | Partial molar pregnancy (PHM) | Weekly quantitative β-hCG titers until 3 successive β-hCG levels were negative |
| Chaouki Mbarki et al., 2015 [16] | Case report | 37 years BHCG 290,600 mIU/mL. Last menstrual period 7 weeks before. Abdominal pelvic pain | 5 cm left latero-uterine heterogeneous mass, a large pelvic effusion, and no intrauterine pregnancy | Left laparoscopic salpingectomy | Complete molar pregnancy (CHM) and tubal rupture | Weekly quantitative β-hCG titers until 3 successive β-hCG levels were negative |
| IA Yakasai et al., 2012 [17] | Case report | 35 years Last menstrual period 12 weeks before. Abdominal pelvic pain | Well-encapsulated mass in the left adnexa, measuring 79.8 × 50 mm | Laparotomy left side salpingectomy | Complete molar pregnancy (CHM) and tubal rupture | Every 2 weeks quantitative β-hCG titers until 3 successive β-hCG levels were negative |
| Ting Zhao et al., 2019 [18] | Case report | 27 years BHCG 6178 mIU/mL. Last menstrual period 4 weeks before. Abdominal pain | Right adnexal mass measuring 31 × 28 × 18 mm (medium/low echogenic), while no sac was detected in the uterine cavity | Right laparoscopic salpingotomy + 100 mg methotrexate injected into the right mesosalpinx | Complete molar pregnancy (CHM) | Weekly quantitative β-hCG titers until 3 successive β-hCG levels were negative |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Asta, M.; La Ferrera, N.; Gulino, F.A.; Ettore, C.; Ettore, G. Is It Possible to Diagnose Preoperatively a Tubal Ectopic Hydatidiform Molar Pregnancy? Description of a Case Report and Review of the Literature of the Last Ten Years. J. Clin. Med. 2022, 11, 5783. https://doi.org/10.3390/jcm11195783
D’Asta M, La Ferrera N, Gulino FA, Ettore C, Ettore G. Is It Possible to Diagnose Preoperatively a Tubal Ectopic Hydatidiform Molar Pregnancy? Description of a Case Report and Review of the Literature of the Last Ten Years. Journal of Clinical Medicine. 2022; 11(19):5783. https://doi.org/10.3390/jcm11195783
Chicago/Turabian StyleD’Asta, Marco, Nicolò La Ferrera, Ferdinando Antonio Gulino, Carla Ettore, and Giuseppe Ettore. 2022. "Is It Possible to Diagnose Preoperatively a Tubal Ectopic Hydatidiform Molar Pregnancy? Description of a Case Report and Review of the Literature of the Last Ten Years" Journal of Clinical Medicine 11, no. 19: 5783. https://doi.org/10.3390/jcm11195783
APA StyleD’Asta, M., La Ferrera, N., Gulino, F. A., Ettore, C., & Ettore, G. (2022). Is It Possible to Diagnose Preoperatively a Tubal Ectopic Hydatidiform Molar Pregnancy? Description of a Case Report and Review of the Literature of the Last Ten Years. Journal of Clinical Medicine, 11(19), 5783. https://doi.org/10.3390/jcm11195783







