Late Myocardial Infarction and Repeat Revascularization after Coronary Artery Bypass Grafting in Patients with Prior Percutaneous Coronary Intervention †
Abstract
1. Introduction
2. Material and Methods
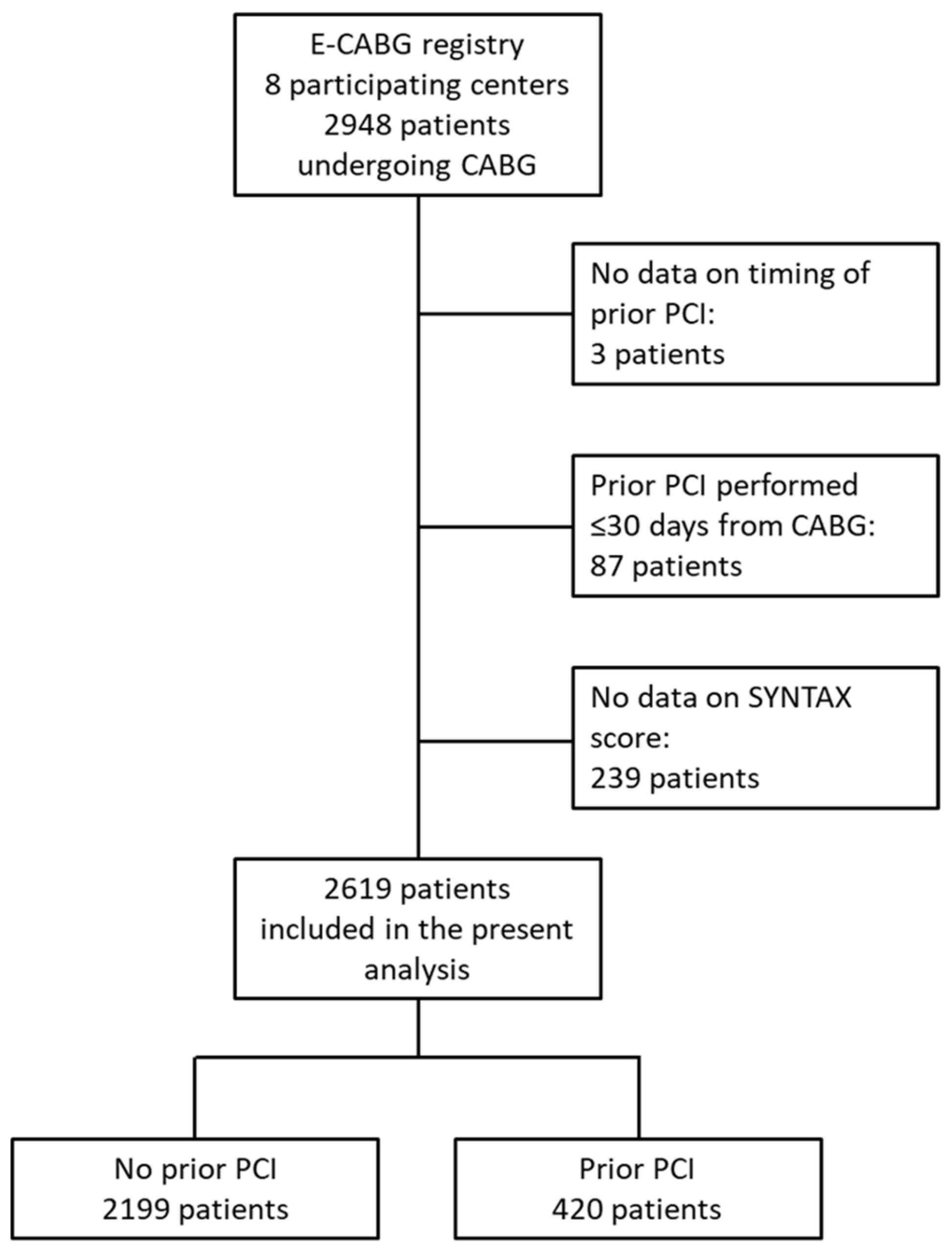
2.1. Patient Population and Data Collection
2.2. Study Cohorts
2.3. Outcomes
2.4. Statistical Analysis
3. Results
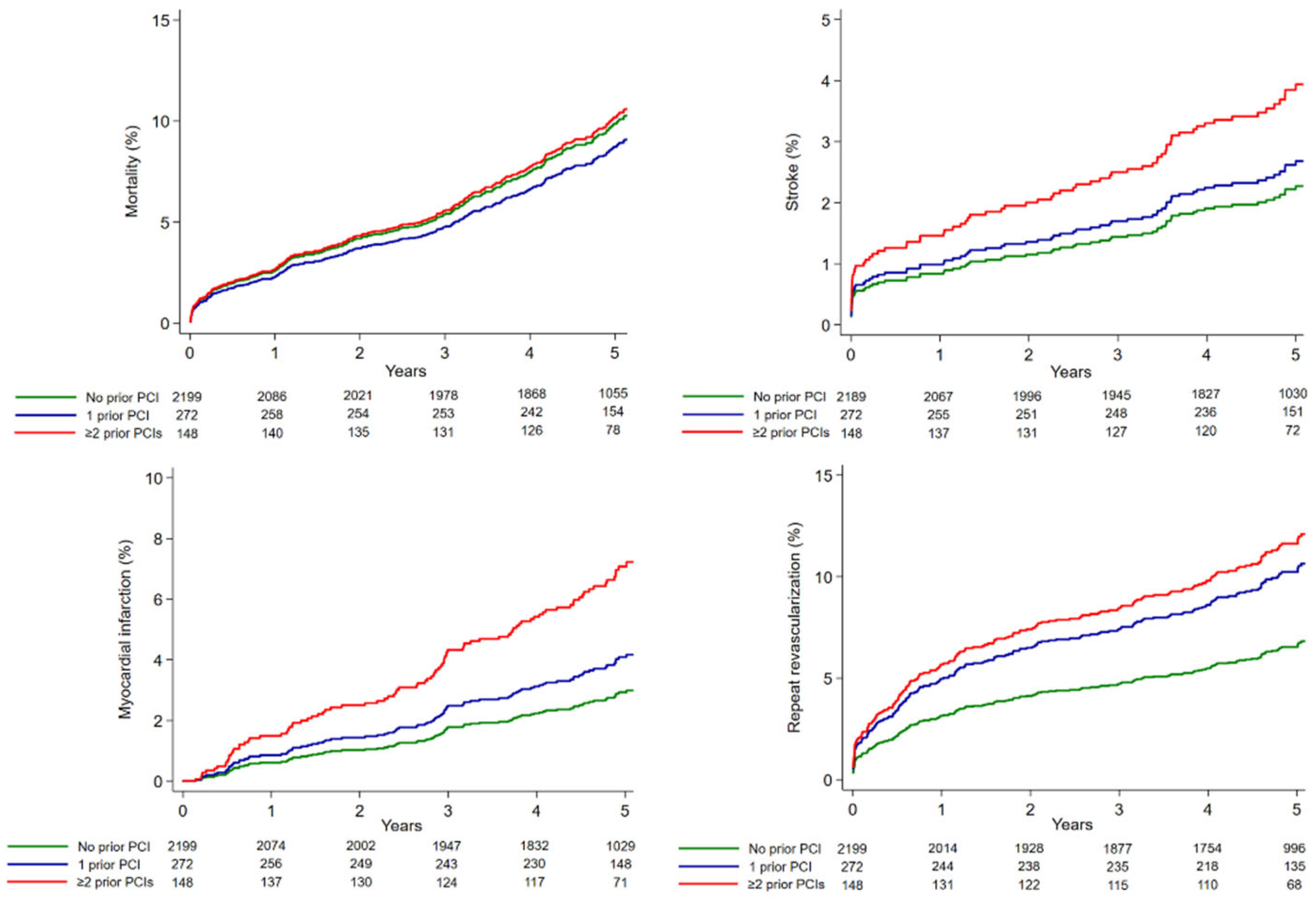
3.1. Outcome According to the Number of Prior PCIs
3.2. Outcome According to the Number of Treated Vessels with PCIs
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mohr, F.W.; Morice, M.C.; Kappetein, A.P.; Feldman, T.E.; Ståhle, E.; Colombo, A.; Mack, M.J.; Holmes, D.R., Jr.; Morel, M.A.; Van Dyck, N.; et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013, 381, 629–638. [Google Scholar] [CrossRef]
- Biancari, F.; Gudbjartsson, T.; Heikkinen, J.; Anttila, V.; Mäkikallio, T.; Jeppsson, A.; Thimour-Bergström, L.; Mignosa, C.; Rubino, A.S.; Kuttila, K.; et al. Comparison of 30-day and 5-year outcomes of percutaneous coronary intervention versus coronary artery bypass grafting in patients aged ≤ 50 years (the Coronary aRtery diseAse in younG adultS Study). Am. J. Cardiol. 2014, 114, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhao, Z.; Yao, J.; Zhao, J.; Hou, T.; Wang, M.; Xu, Y.; Wang, B.; Niu, G.; Sui, Y.; et al. Prior percutaneous coronary intervention and outcomes in patients after coronary artery bypass grafting: A meta-analysis of 308,284 patients. Ther. Adv. Chronic Dis. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Thielmann, M.; Leyh, R.; Massoudy, P.; Neuhäuser, M.; Aleksic, I.; Kamler, M.; Herold, U.; Piotrowski, J.; Jakob, H. Prognostic significance of multiple previous percutaneous coronary interventions in patients undergoing elective coronary artery bypass surgery. Circulation 2006, 114 (Suppl. S1), I441–I447. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Massoudy, P.; Thielmann, M.; Lehmann, N.; Marr, A.; Kleikamp, G.; Maleszka, A.; Zittermann, A.; Körfer, R.; Radu, M.; Krian, A.; et al. Impact of prior percutaneous coronary intervention on the outcome of coronary artery bypass surgery: A multicenter analysis. J. Thorac. Cardiovasc. Surg. 2009, 137, 840–845. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yap, C.H.; Yan, B.P.; Akowuah, E.; Dinh, D.T.; Smith, J.A.; Shardey, G.C.; Tatoulis, J.; Skillington, P.D.; Newcomb, A.; Mohajeri, M.; et al. Does prior percutaneous coronary intervention adversely affect early and mid-term survival after coronary artery surgery? JACC Cardiovasc. Interv. 2009, 2, 758–764. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ueki, C.; Miyata, H.; Motomura, N.; Sakaguchi, G.; Akimoto, T.; Takamoto, S. Previous percutaneous coronary intervention does not increase adverse events after coronary artery bypass surgery. Ann. Thorac. Surg. 2017, 104, 56–61. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hakamada, K.; Sakaguchi, G.; Marui, A.; Arai, Y.; Nagasawa, A.; Tsumaru, S.; Hanyu, M.; Soga, Y. Effect of multiple prior percutaneous coronary interventions on outcomes after coronary artery bypass grafting. Circ. J. 2021, 85, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Fukui, T.; Tanaka, S.; Takanashi, S. Previous coronary stents do not increase early and long-term adverse outcomes in patients undergoing off-pump coronary artery bypass grafting: A propensity-matched comparison. J. Thorac. Cardiovasc. Surg. 2014, 148, 1843–1849. [Google Scholar] [CrossRef] [PubMed][Green Version]
- van den Brule, J.M.; Noyez, L.; Verheugt, F.W. Risk of coronary surgery for hospital and early morbidity and mortality after initially successful percutaneous intervention. Interact. Cardiovasc. Thorac. Surg. 2005, 4, 96–100. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Miguel, G.S.V.; Sousa, A.G.; Silva, G.S.; Colósimo, F.C.; Stolf, N.A.G. Does Prior Percutaneous Coronary Intervention Influence the Outcomes of Coronary Artery Bypass Surgery? Braz. J. Cardiovasc. Surg. 2020, 35, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Nicolau, J.C.; Stevens, S.R.; Al-Khalidi, H.R.; Jatene, F.B.; Furtado, R.H.M.; Dallan, L.A.O.; Lisboa, L.A.F.; Desvigne-Nickens, P.; Haddad, H.; Jolicoeur, E.M.; et al. Does prior coronary angioplasty affect outcomes of surgical coronary revascularization? Insights from the STICH trial. Int. J. Cardiol. 2019, 291, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Stevens, L.M.; Khairy, P.; Agnihotri, A.K. Coronary artery bypass grafting after recent or remote percutaneous coronary intervention in the Commonwealth of Massachusetts. Circ. Cardiovasc. Interv. 2010, 3, 460–467. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sandner, S.; Redfors, B.; Angiolillo, D.J.; Audisio, K.; Fremes, S.E.; Janssen, P.W.A.; Kulik, A.; Mehran, R.; Peper, J.; Ruel, M.; et al. Association of dual antiplatelet therapy with ticagrelor with vein graft failure after coronary artery bypass graft surgery: A systematic review and meta-analysis. JAMA 2022, 328, 554–562. [Google Scholar] [CrossRef] [PubMed]
| Covariates | No Prior PCI 2199 pts | 1 Prior PCI 272 pts | ≥2 Prior PCIs 148 pts | p-Value |
|---|---|---|---|---|
| Baseline risk factors | ||||
| Age (years) | 67.6 ± 9.2 | 65.6 ± 10.0 | 66.9 ± 8.8 | 0.006 |
| Female | 362 (16.5) | 43 (15.8) | 28 (18.9) | 0.615 |
| eGFR (mL/min/1.73 m2) | 76 ± 20 | 76 ± 21 | 75 ± 23 | 0.807 |
| Dialysis | 19 (0.9) | 3 (1.1) | 5 (3.4) | 0.009 |
| Functioning kidney transplant | 6 (0.3) | 1 (0.4) | 0 (0) | 0.712 |
| Anemia | 607 (27.6) | 67 (24.6) | 49 (33.1) | 0.507 |
| Diabetes | 632 (28.7) | 87 (32.0) | 54 (36.5) | 0.028 |
| Recent STEMI | 140 (6.4) | 14 (5.1) | 10 (6.8) | 0.812 |
| Prior stroke/TIA | 145 (6.6) | 22 (8.1) | 11 (7.4) | 0.431 |
| Atrial fibrillation | 183 (8.3) | 15 (5.5) | 22 (14.9) | 0.136 |
| Pulmonary disease | 241 (11.0) | 31 (11.4) | 17 (11.5) | 0.785 |
| Extracardiac arteriopathy | 460 (20.9) | 57 (21.0) | 38 (25.7) | 0.256 |
| Prior cardiac surgery | 7 (0.3) | 4 (1.5) | 5 (3.4) | <0.0001 |
| LVEF ≤ 50% | 666 (30.3) | 81 (29.8) | 47 (32) | 0.793 |
| Critical preoperative state | 225 (10.2) | 22 (8.1) | 11 (7.4) | 0.141 |
| Emergency procedure | 84 (3.8) | 5 (1.8) | 5 (3.4) | 0.292 |
| Indication for surgery | ||||
| In-stent restenosis | - | 60 (22.1) | 78 (53.1) | - |
| Stent thrombosis | - | 6 (2.2) | 8 (5.4) | - |
| Progression of CAD | - | 211 (77.6) | 118 (79.7) | - |
| Left main coronary a. PCI | - | 8 (2.9) | 15 (10.1) | - |
| Any drug-eluting stent | - | 126 (46.3) | 106 (71.6) | - |
| Delay from last PCI (years) | - | 6.6 ± 6.4 | 4.5 ± 4.6 | - |
| No. of diseased vessels | 2.8 ± 0.5 | 2.6 ± 0.6 | 2.6 ± 0.6 | <0.0001 |
| Left main stenosis | 213 (9.7) | 25 (9.2) | 11 (7.4) | 0.381 |
| SYNTAX score | 29 ± 10 | 27 ± 10 | 26 ± 12 | <0.0001 |
| EuroSCORE II (%) | 3.2 ± 4.5 | 3.0 ± 5.0 | 3.6 ± 4.6 | 0.065 |
| Operative data | ||||
| No. of distal anastomoses | 3.0 ± 1.0 | 2.7 ± 0.9 | 2.5 ± 0.9 | <0.0001 |
| CPB time (min) | 89 ± 33 | 84 ± 32 | 88 ± 36 | 0.064 |
| Aortic clamping time (min) | 61 ± 27 | 58 ± 25 | 59 ± 29 | 0.041 |
| Off-pump surgery | 265 (12.1) | 40 (14.7) | 34 (23.0) | <0.0001 |
| BIMA grafting | 518 (23.6) | 75 (27.6) | 16 (10.8) | 0.029 |
| Radial artery graft | 70 (3.2) | 14 (5.1) | 7 (4.7) | 0.097 |
| No Prior PCI 2199 pts | 1 Prior PCI 272 pts | ≥2 Prior PCIs 148 pts | |
|---|---|---|---|
| 30-day mortality | 1.4% | 1.8% | 2.0% |
| Adjusted OR | - | 1.504 (0.547−4.130) | 1.325 (0.342−5.138) |
| 5-year mortality | 12.5% | 9.3% | 14.6% |
| Adjusted HR | - | 0.867 (0.580−1.298) | 0.993 (0.628−1.571) |
| 5-year myocardial infarction | 3.2% | 5.3% | 10.9% |
| Adjusted SHR | - | 1.389 (0.752−2.680) | 2.566 (1.379−4.312) |
| 5-year repeat revascularization | 7.2% | 11.8% | 15.3% |
| Adjusted SHR | - | 1.550 (1.049−2.291) | 1.774 (1.140−2.763) |
| 5-year stroke | 3.0% | 3.0% | 4.8% |
| Adjusted SHR | - | 1.251 (0.596−2.727) | 1.872 (0.874−4.001) |
| 5-year MACCE | 18.8% | 20.5% | 30.2% |
| Adjusted HR | - | 1.188 (0.895−1.578) | 1.383 (0.996−1.920) |
| Covariates | No Prior PCI 2199 pts | 1 Vessel Treated with PCI 271 pts | ≥2 Vessels Treated with PCI 149 pts | p-Value |
|---|---|---|---|---|
| Baseline risk factors | ||||
| Age (years) | 67.6 ± 9.2 | 65.9 ± 9.9 | 66.4 ± 9.0 | 0.011 |
| Female | 362 (16.5) | 44 (16.2) | 27 (18.1) | 0.698 |
| eGFR (mL/min/1.73 m2) | 76 ± 20 | 77 ± 21 | 74 ± 23 | 0.658 |
| Dialysis | 19 (0.9) | 4 (1.5) | 4 (2.7) | 0.026 |
| Functioning kidney transplant | 6 (0.3) | 1 (0.4) | 0 (0) | 0.711 |
| Anemia | 607 (27.6) | 69 (25.5) | 47 (31.5) | 0.634 |
| Diabetes | 632 (28.7) | 84 (31.0) | 57 (38.3) | 0.016 |
| Recent STEMI | 140 (6.4) | 12 (4.4) | 12 (8.1) | 0.955 |
| Prior stroke/TIA | 145 (6.6) | 19 (7.0) | 14 (9.4) | 0.225 |
| Atrial fibrillation | 183 (8.3) | 18 (6.6) | 19 (12.8) | 0.279 |
| Pulmonary disease | 241 (11.0) | 32 (11.8) | 16 (10.7) | 0.887 |
| Extracardiac arteriopathy | 460 (20.9) | 53 (19.6) | 42 (28.2) | 0.141 |
| Prior cardiac surgery | 7 (0.3) | 5 (1.8) | 4 (2.7) | < 0.0001 |
| LVEF ≤50% | 666 (30.3) | 79 (29.2) | 49 (33.1) | 0.691 |
| Critical preoperative state | 225 (10.2) | 21 (7.7) | 12 (8.1) | 0.174 |
| Emergency procedure | 84 (3.8) | 4 (1.5) | 6 (4.1) | 0.389 |
| Indication for surgery | ||||
| In-stent restenosis | - | 8 (3.0) | 6 (4.0) | - |
| Stent thrombosis | - | 64 (23.6) | 74 (50.0) | - |
| Progression of CAD | - | 205 (75.6) | 124 (83.2) | - |
| Left main coronary a. PCI | - | 0 (0) | 23 (15.4) | - |
| Any drug-eluting stent | - | 124 (45.8) | 108 (72.5) | - |
| Delay from last PCI (years) | - | 6.7 ± 6.4 | 4.4 ± 4.4 | - |
| No. of diseased vessels | 2.8 ± 0.5 | 2.6 ± 0.6 | 2.6 ± 0.6 | <0.0001 |
| Left main stenosis | 213 (9.7) | 19 (7.0) | 17 (11.4) | 0.891 |
| SYNTAX score | 29 ± 10 | 27 ± 10 | 26 ± 11 | <0.0001 |
| EuroSCORE II (%) | 3.2 ± 4.5 | 3.0 ± 5.0 | 3.6 ± 4.6 | 0.035 |
| Operative data | ||||
| No. of distal anastomoses | 3.0 ± 1.0 | 2.7 ± 0.9 | 2.5 ± 0.9 | <0.0001 |
| CPB time (min) | 89 ± 33 | 85 ± 32 | 86 ± 35 | 0.054 |
| Aortic clamping time (min) | 61 ± 27 | 59 ± 26 | 57 ± 27 | 0.053 |
| Off-pump surgery | 265 (12.1) | 44 (16.2) | 30 (20.1) | 0.001 |
| BIMA grafting | 518 (23.6) | 74 (27.3) | 17 (11.4) | 0.035 |
| Radial artery graft | 70 (3.2) | 12 (4.4) | 9 (6.0) | 0.041 |
| No prior PCI 2199 pts | 1 Vessel Treated with PCI 271 pts | ≥2 Vessels Treated with PCI 149 pts | |
|---|---|---|---|
| 30-day mortality | 1.4% | 1.5% | 2.7% |
| Adjusted OR | - | 1.165 (0.384−3.532) | 1.937 (0.597−6.290) |
| 5-year mortality | 12.5% | 6.9% | 18.8% |
| Adjusted HR | - | 0.641 (0.408−1.009) | 1.383 (0.918−2.083) |
| 5-year myocardial infarction | 3.2% | 5.3% | 10.8% |
| Adjusted SHR | - | 1.500 (0.831−2.705) | 2.640 (1.497−4.658) |
| 5-year repeat revascularization | 7.0% | 12.4% | 14.1% |
| Adjusted SHR | - | 1.627 (1.115−2.373) | 1.648 (1.029−2.638) |
| 5-year stroke | 3.0% | 2.6% | 5.4% |
| Adjusted SHR | - | 1.063 (0.489−2.310) | 2.215 (1.056−4.646) |
| 5-year MACCE | 18.8% | 18.5% | 33.5% |
| Adjusted HR | - | 1.041 (0.774−1.400) | 1.655 (1.211−2.260) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biancari, F.; Salsano, A.; Santini, F.; De Feo, M.; Dalén, M.; Zhang, Q.; Gatti, G.; Mazzaro, E.; Franzese, I.; Bancone, C.; et al. Late Myocardial Infarction and Repeat Revascularization after Coronary Artery Bypass Grafting in Patients with Prior Percutaneous Coronary Intervention. J. Clin. Med. 2022, 11, 5755. https://doi.org/10.3390/jcm11195755
Biancari F, Salsano A, Santini F, De Feo M, Dalén M, Zhang Q, Gatti G, Mazzaro E, Franzese I, Bancone C, et al. Late Myocardial Infarction and Repeat Revascularization after Coronary Artery Bypass Grafting in Patients with Prior Percutaneous Coronary Intervention. Journal of Clinical Medicine. 2022; 11(19):5755. https://doi.org/10.3390/jcm11195755
Chicago/Turabian StyleBiancari, Fausto, Antonio Salsano, Francesco Santini, Marisa De Feo, Magnus Dalén, Qiyao Zhang, Giuseppe Gatti, Enzo Mazzaro, Ilaria Franzese, Ciro Bancone, and et al. 2022. "Late Myocardial Infarction and Repeat Revascularization after Coronary Artery Bypass Grafting in Patients with Prior Percutaneous Coronary Intervention" Journal of Clinical Medicine 11, no. 19: 5755. https://doi.org/10.3390/jcm11195755
APA StyleBiancari, F., Salsano, A., Santini, F., De Feo, M., Dalén, M., Zhang, Q., Gatti, G., Mazzaro, E., Franzese, I., Bancone, C., Zanobini, M., Tauriainen, T., Mäkikallio, T., Saccocci, M., Francica, A., Rosato, S., El-Dean, Z., Onorati, F., & Mariscalco, G. (2022). Late Myocardial Infarction and Repeat Revascularization after Coronary Artery Bypass Grafting in Patients with Prior Percutaneous Coronary Intervention. Journal of Clinical Medicine, 11(19), 5755. https://doi.org/10.3390/jcm11195755










