Stress Reduction by Yoga versus Mindfulness Training in Adults Suffering from Distress: A Three-Armed Randomized Controlled Trial including Qualitative Interviews (RELAX Study)
Abstract
1. Introduction
2. Materials and Methods
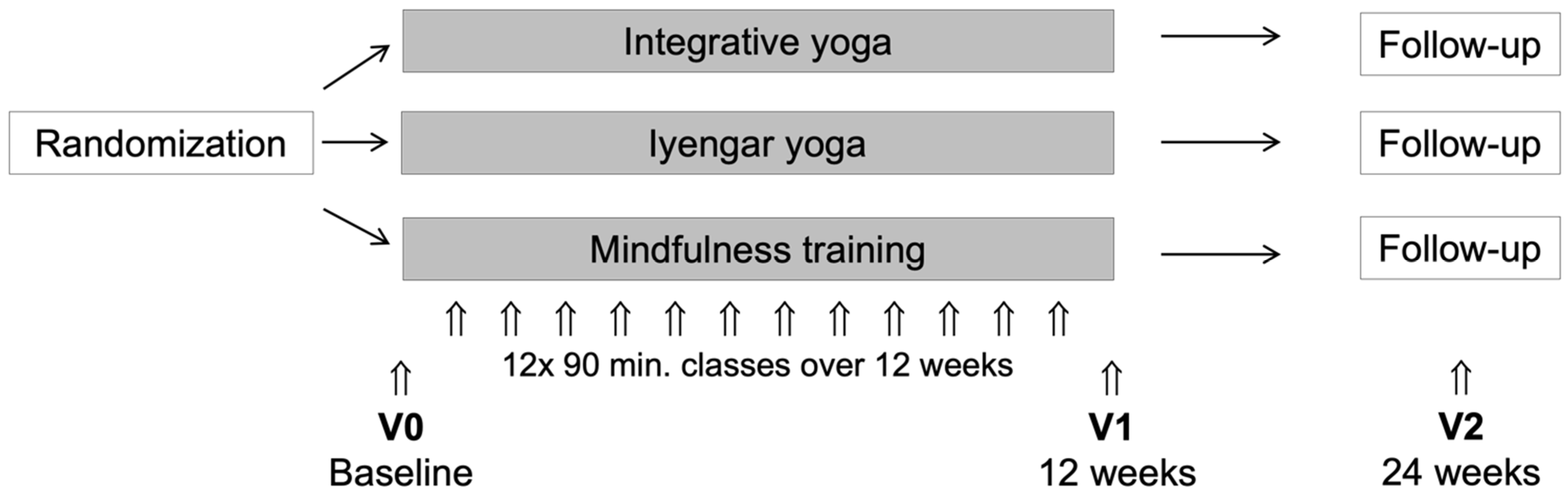
2.1. Study Design
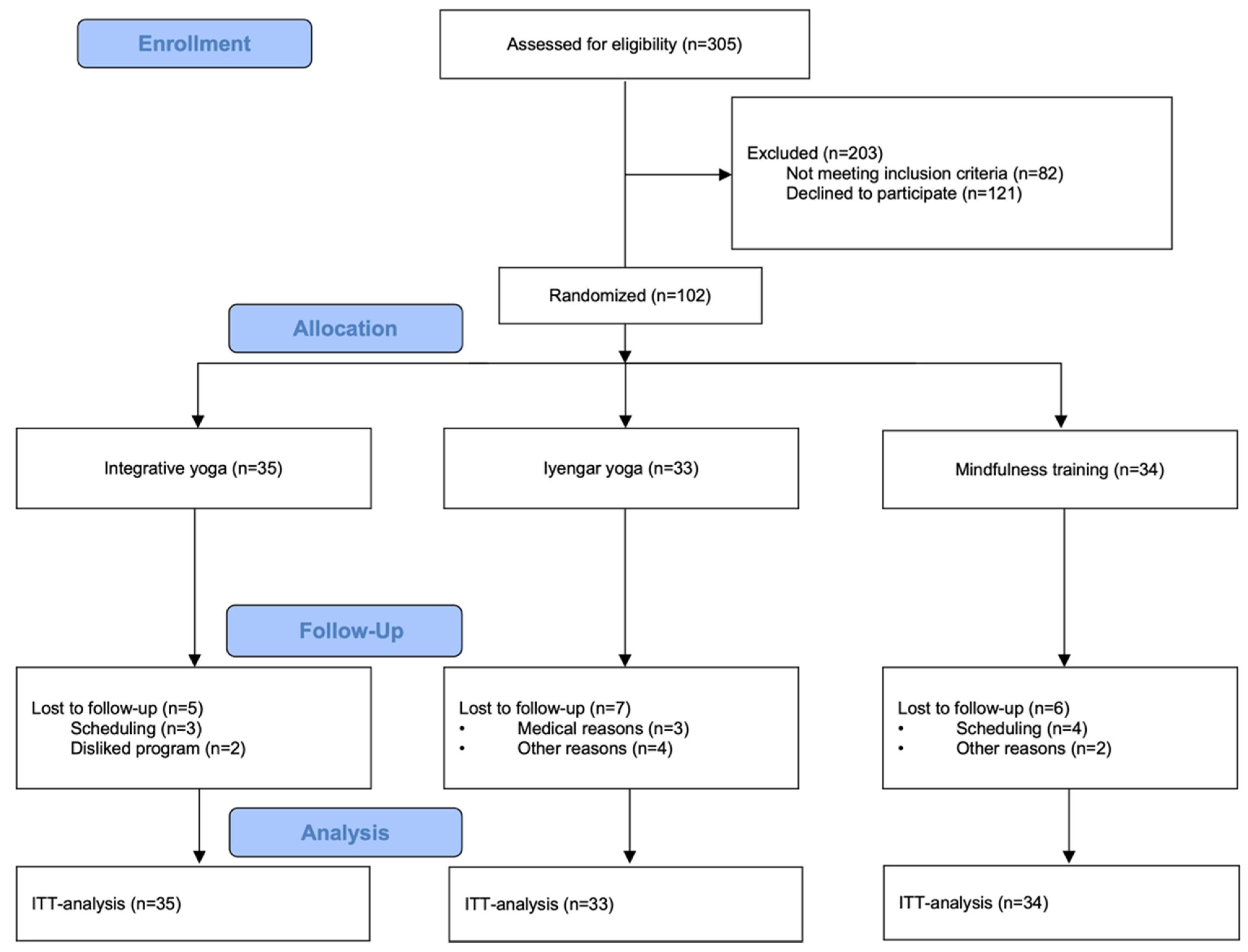
2.2. Recruitment
2.3. Randomization
2.4. Setting
2.5. Interventions
2.5.1. Integrative Yoga
2.5.2. Iyengar Yoga
2.5.3. Mindfulness Training
2.6. Primary Outcome
2.7. Secondary Outcomes
2.7.1. Maslach Burnout Inventory (MBI)
2.7.2. Short Form 36 Health Survey (SF-36)
2.7.3. Beschwerden-Liste/Zerssen Symptom List (B-LR and B-LR’)
2.7.4. Hospital Anxiety and Depression Scale (HADS)
2.7.5. Freiburg Mindfulness Inventory (FMI)
2.7.6. Multidimensional Assessment of Interoceptive Awareness (MAIA)
2.7.7. Self-Regulation Inventory (SRI)
2.7.8. Aspects of Spirituality (ASP)
2.7.9. Hood’s Mysticism Scale (HMS)
2.7.10. Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5)
2.8. Sample Size
2.9. Statistical Methods
2.10. Qualitative Approach
3. Results
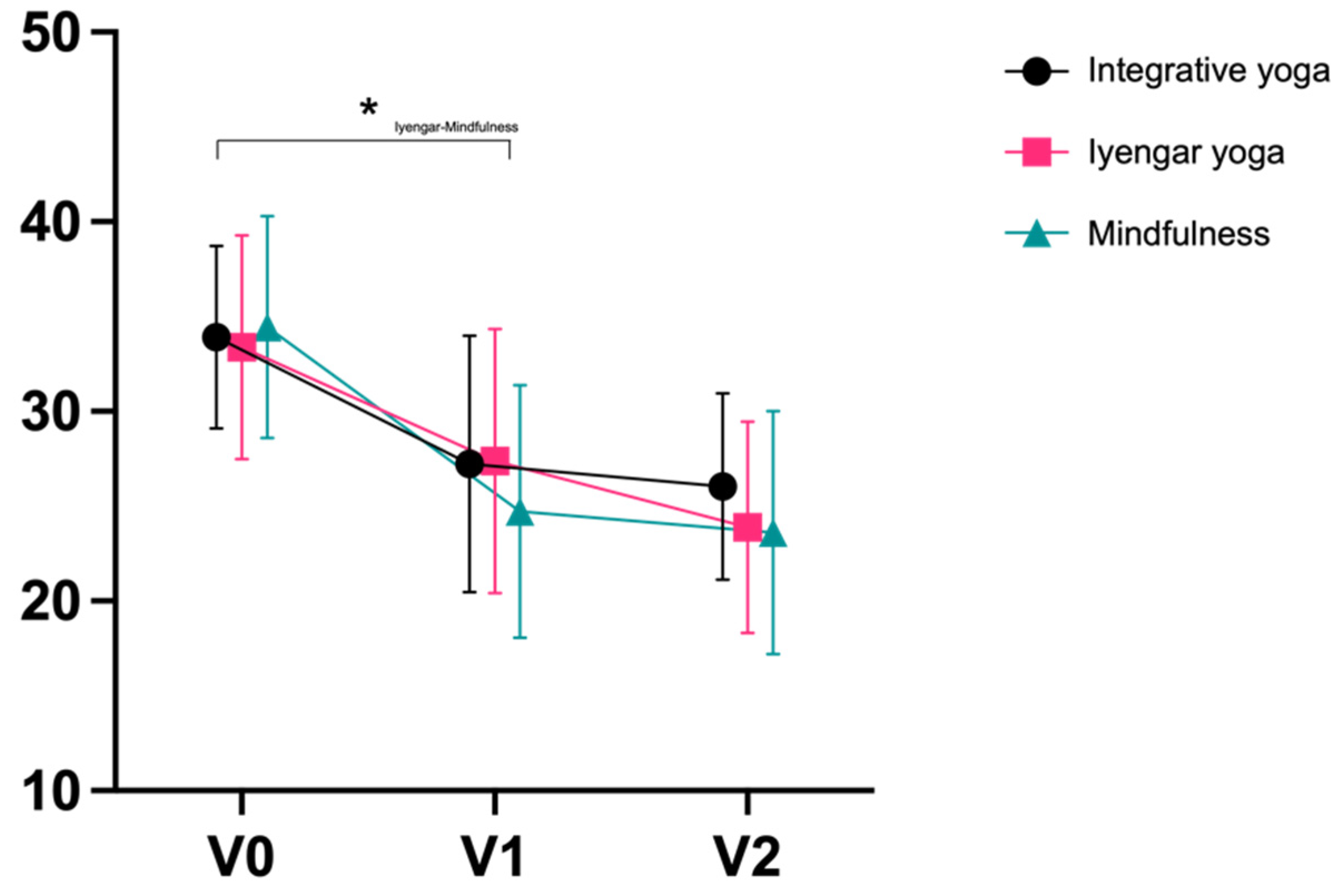
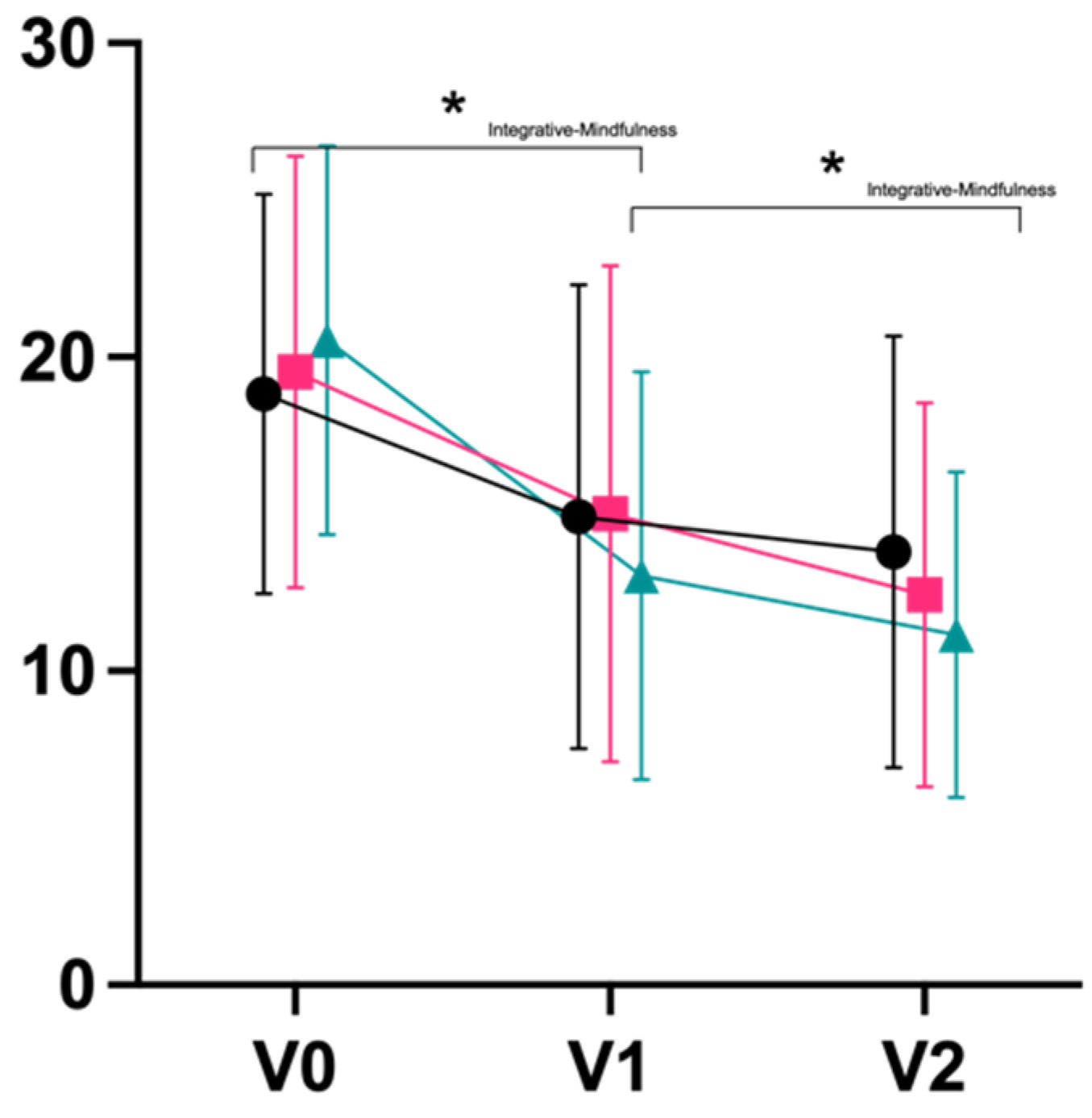
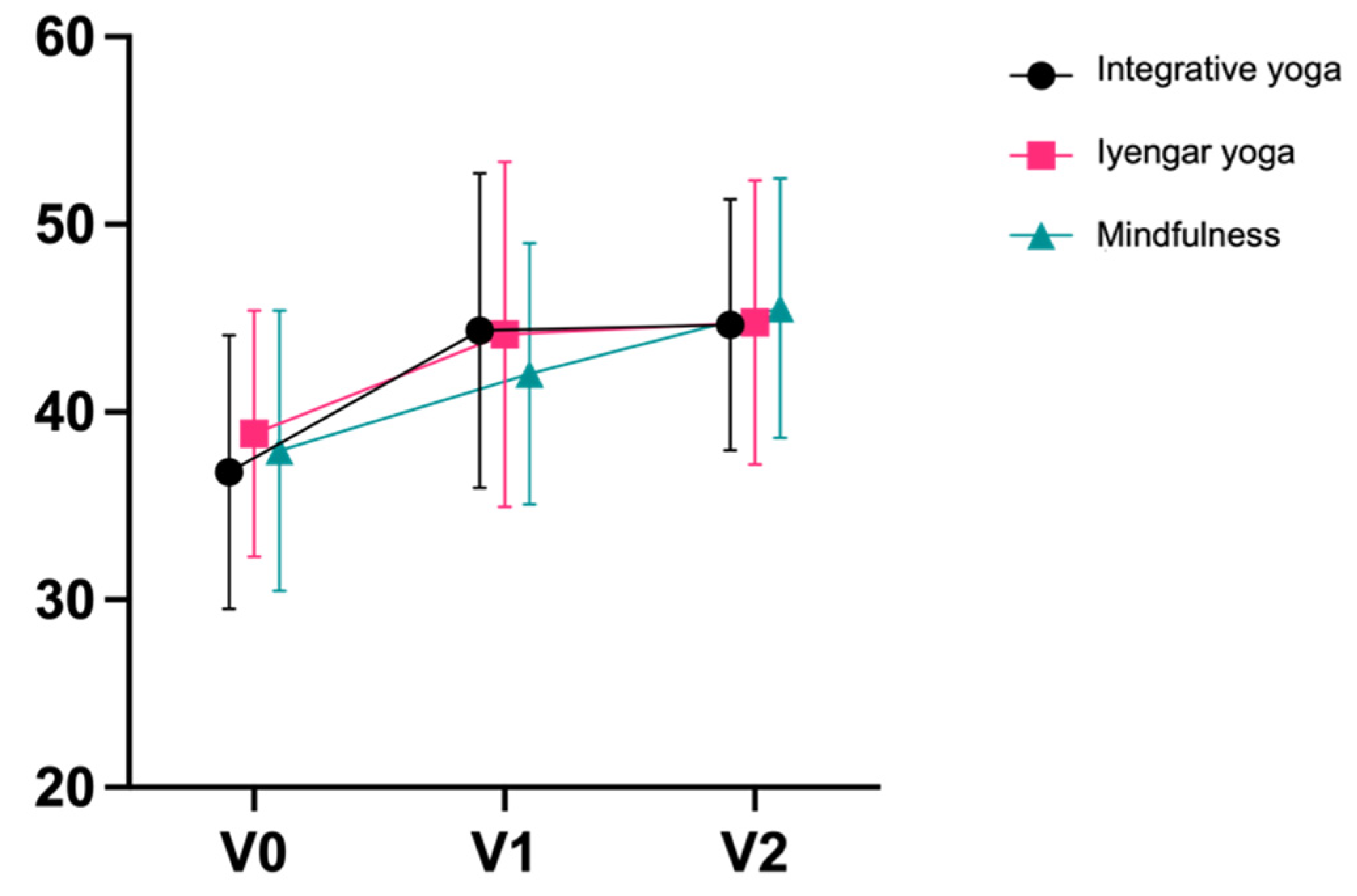
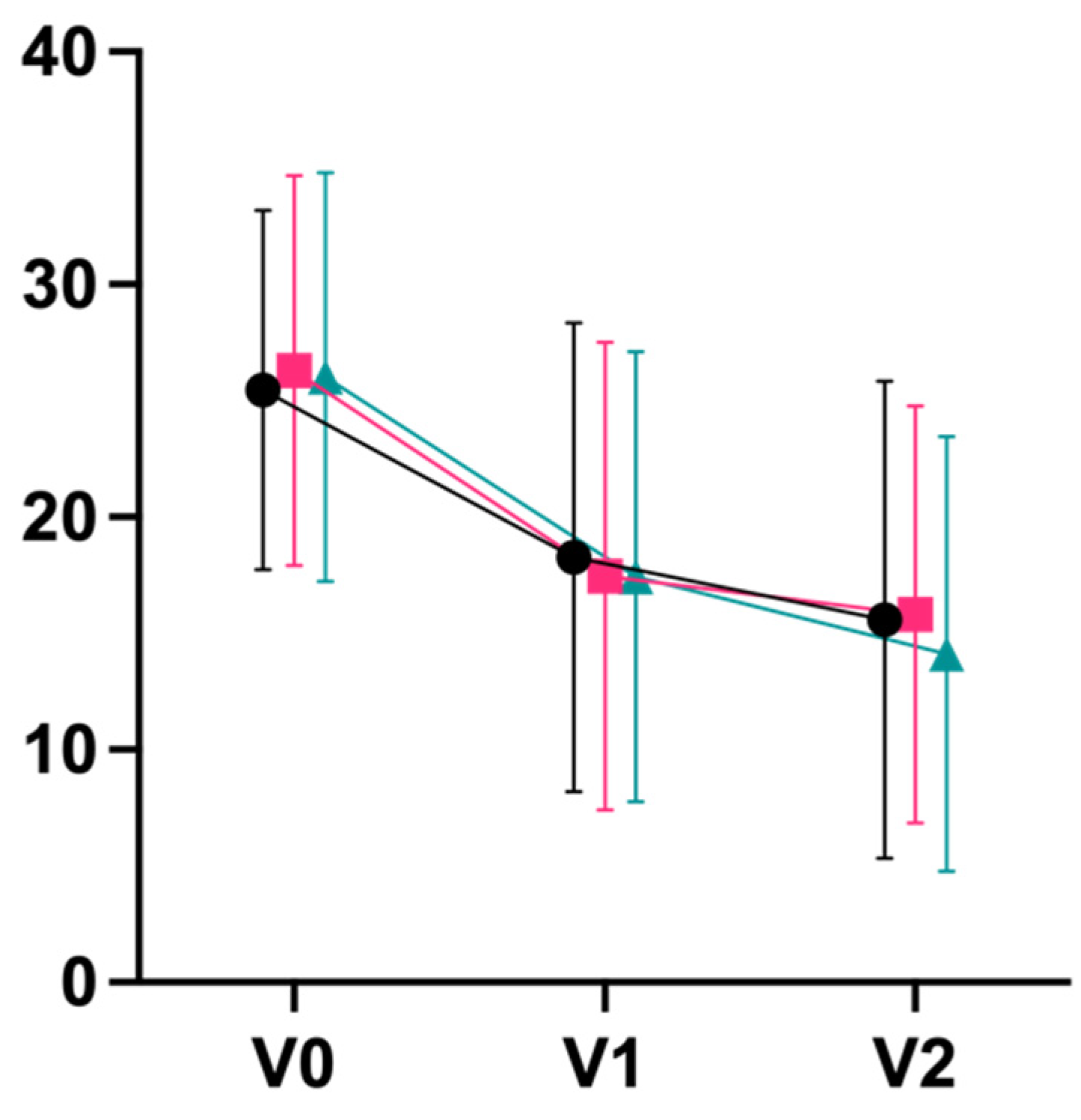
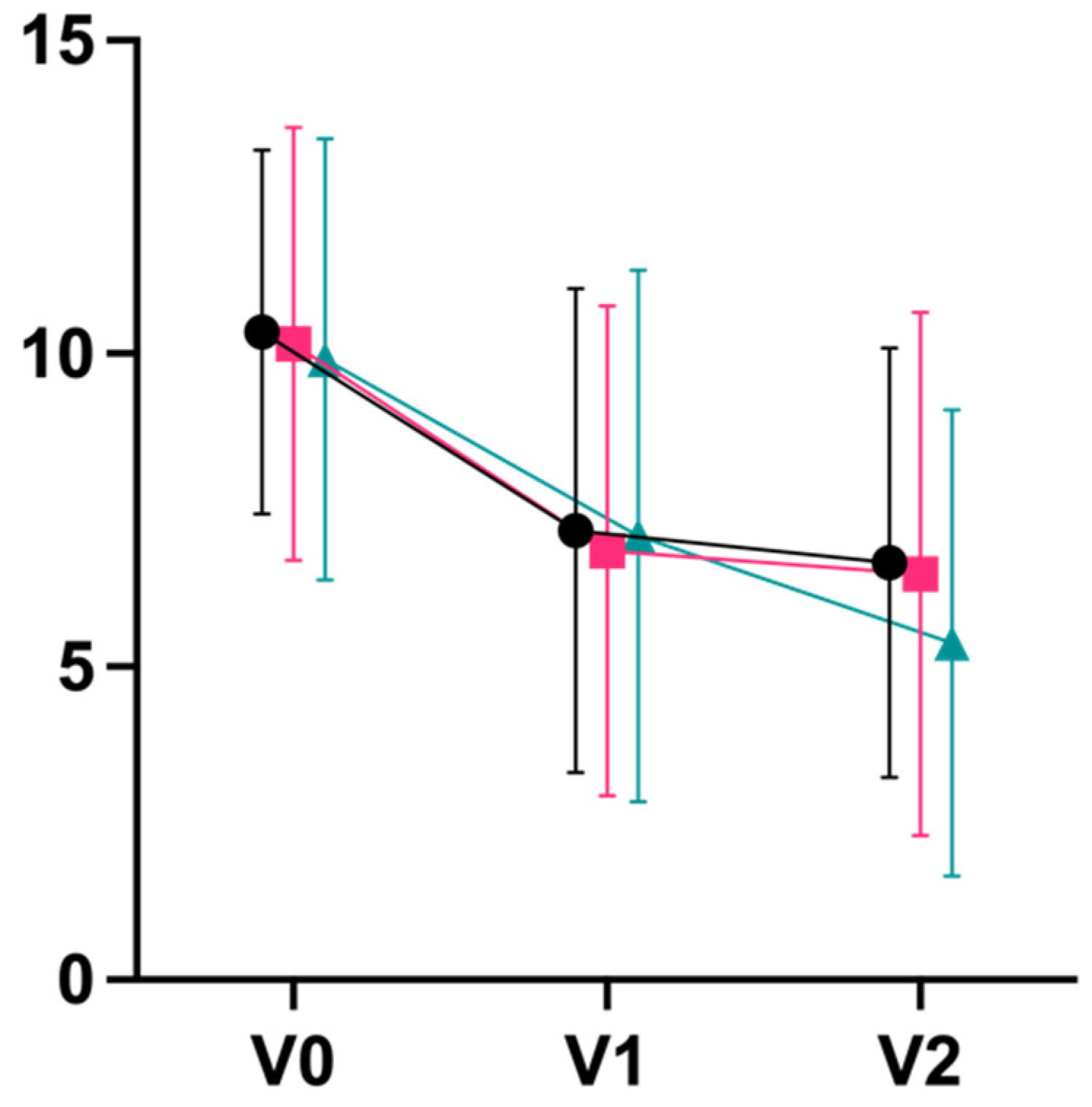
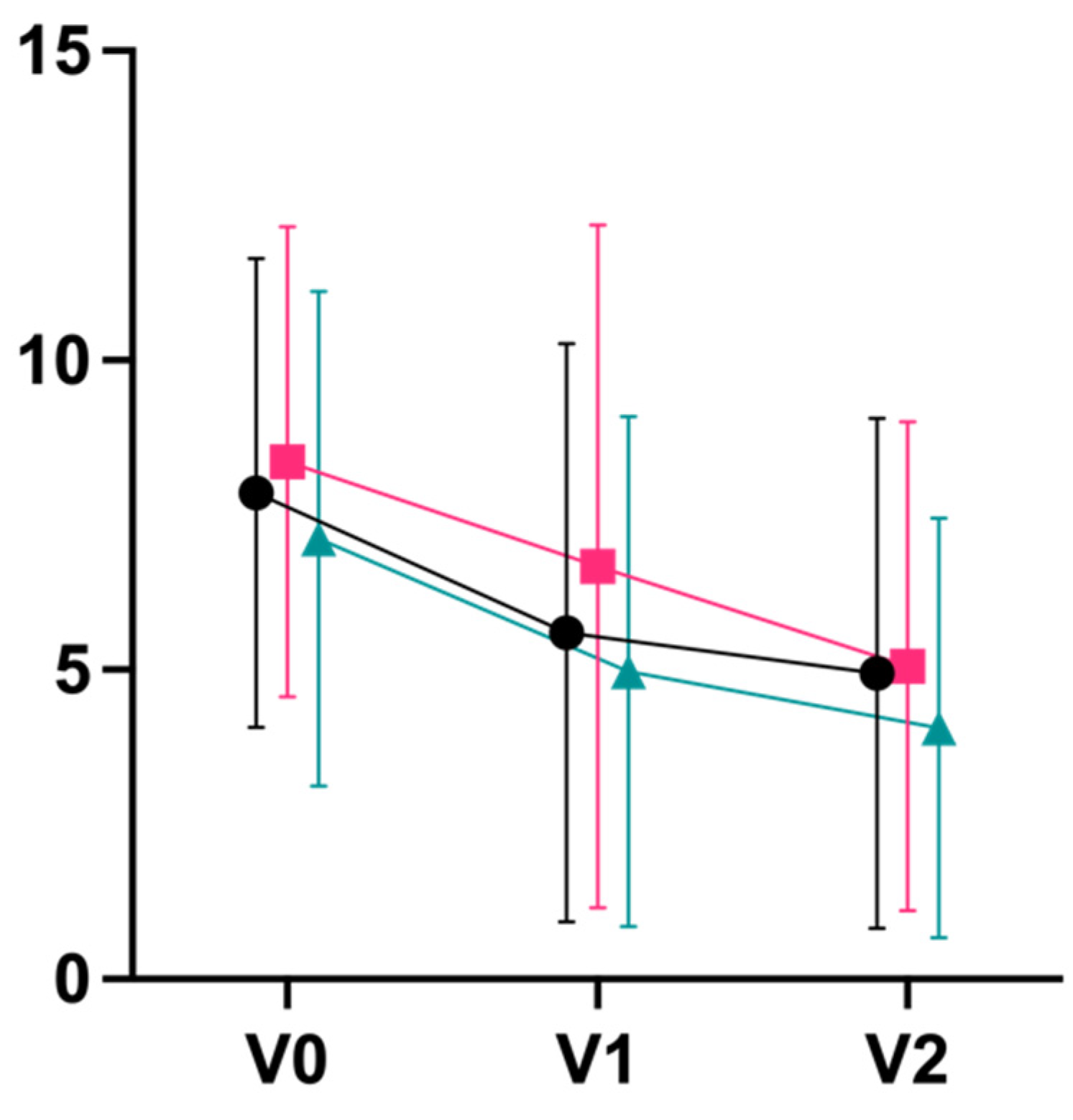
3.1. Quantitative Results
3.2. Qualitative Results
“My daily life is, it went on as it was before, or still is now. But I include an hour for myself.”(Participant 5—Iyengar yoga)
“But a little bit, I have achieved that I allow myself more. […] I have a Jacuzzi in the bathroom, I’ve never used it, for 15 years, […] because I didn’t allow myself that. […] because that was a pampering for me and I’m not allowed to do that. I’ve overcome those little things now and that’s what I do now.”(Participant 6—Mindfulness training)
“Yes, so this mindfulness of what’s happening to me and where I am right now and I’m trying to control that better. […] And now I always try to be aware of how each step is happening, what I’m doing and try not to get distracted. That’s not always successful, but that’s what I try to do.”(Participant 6—Mindfulness training)
“Yes, so a little bit. Not as much as I would have liked, and as I’ve heard with the other women.”(Participant 6—Mindfulness training)
“There were also moments when I really noticed a fundamental change. And where I really became aware that I had done too much to myself before. And one of the greatest moments was when, after a meditation, I stood there on my mat and started to cry and asked my body out loud for forgiveness for what I had done to it for 20 years in the job in which I now work. Nobody had told me to do that, that came from within, and I was very aware of that at that moment, that that came from me. And there were a few things like that then, during the course and even later.”(Participant 2—Mindfulness training)
“You’re not so completely alone in the world, it’s not an exceptional problem, it’s something that a lot of people have.”(Participant 3—Integrative yoga)
3.3. Harms
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ulrich-Lai, Y.M.; Herman, J.P. Neural regulation of endocrine and autonomic stress responses. Nat. Rev. Neurosci. 2009, 10, 397–409. [Google Scholar] [CrossRef]
- Agorastos, A.; Chrousos, G.P. The neuroendocrinology of stress: The stress-related continuum of chronic disease development. Mol. Psychiatry 2021, 27, 502–513. [Google Scholar] [CrossRef] [PubMed]
- Morey, J.N.; Boggero, I.A.; Scott, A.B.; Segerstrom, S.C. Current Directions in Stress and Human Immune Function. Curr. Opin. Psychol. 2015, 5, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Khansari, D.N.; Murgo, A.J.; Faith, R.E. Effects of stress on the immune system. Immunol. Today 1990, 11, 170–175. [Google Scholar] [CrossRef]
- Sahle, B.W.; Chen, W.; Melaku, Y.A.; Akombi, B.J.; Rawal, L.B.; Renzaho, A.M. Association of psychosocial factors with risk of chronic diseases: A nationwide longitudinal study. Am. J. Prev. Med. 2020, 58, e39–e50. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Chronic Diseases and Their Risk Factors: The Nation’s Leading Causes of Death; US Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 1999.
- Selye, H. The Stress of Life; McGraw-Hill Book Company: New York, NY, USA, 1956. [Google Scholar]
- Rosengren, A.; Hawken, S.; Ôunpuu, S.; Sliwa, K.; Zubaid, M.; Almahmeed, W.A.; Blackett, K.N.; Sitthi-amorn, C.; Sato, H.; Yusuf, S. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 953–962. [Google Scholar] [CrossRef]
- Rozanski, A.; Blumenthal, J.A.; Davidson, K.W.; Saab, P.G.; Kubzansky, L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: The emerging field of behavioral cardiology. J. Am. Coll. Cardiol. 2005, 45, 637–651. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Tyrrell, D.A.; Smith, A.P. Negative life events, perceived stress, negative affect, and susceptibility to the common cold. J. Pers. Soc. Psychol. 1993, 64, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Davis, P.A.; Holm, J.E.; Myers, T.C.; Suda, K.T. Stress, headache, and physiological disregulation: A time-series analysis of stress in the laboratory. Headache 1998, 38, 116–121. [Google Scholar] [CrossRef]
- Raison, C.L.; Miller, A.H. When not enough is too much: The role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am. J. Psychiatry 2003, 160, 1554–1565. [Google Scholar] [CrossRef]
- Chrousos, G.P.; Kino, T. Glucocorticoid signaling in the cell. Expanding clinical implications to complex human behavioral and somatic disorders. Ann. N. Y. Acad. Sci. 2009, 1179, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Tsigos, C.; Stefanaki, C.; Lambrou, G.I.; Boschiero, D.; Chrousos, G.P. Stress and inflammatory biomarkers and symptoms are associated with bioimpedance measures. Eur. J. Clin. Investig. 2015, 45, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Janicki-Deverts, D.; Miller, G.E. Psychological stress and disease. JAMA 2007, 298, 1685–1687. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.M.; Rodrigue, S.; Ivers, H. Role of stress, arousal, and coping skills in primary insomnia. Psychosom. Med. 2003, 65, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Rubia, K. The neurobiology of Meditation and its clinical effectiveness in psychiatric disorders. Biol. Psychol. 2009, 82, 1–11. [Google Scholar] [CrossRef]
- Dewa, C.S.; Lin, E.; Kooehoorn, M.; Goldner, E. Association of chronic work stress, psychiatric disorders, and chronic physical conditions with disability among workers. Psychiatr. Serv. 2007, 58, 652–658. [Google Scholar] [CrossRef]
- Esch, T. Health in stress: Change in the stress concept and its significance for prevention, health and life style. Gesundheitswesen 2002, 64, 73–81. [Google Scholar] [CrossRef]
- Meyer, B.; Zill, A.; Dilba, D.; Voermans, S. Entspann Dich, Deutschland!—TK-Stressstudie 2021; Techniker Krankenkasse: Hamburg, Germany, 2021. [Google Scholar]
- Béjean, S.; Sultan-Taïeb, H. Modeling the economic burden of diseases imputable to stress at work. Eur. J. Health Econ. 2005, 6, 16–23. [Google Scholar] [CrossRef]
- Sharma, M.; Rush, S.E. Mindfulness-based stress reduction as a stress management intervention for healthy individuals: A systematic review. J. Evid.-Based Complement. Altern. Med. 2014, 19, 271–286. [Google Scholar] [CrossRef]
- Sharma, M. Yoga as an alternative and complementary approach for stress management: A systematic review. J. Evid.-Based. Complement. Altern. Med. 2014, 19, 59–67. [Google Scholar] [CrossRef]
- Quan, P.; Wang, W.; Chu, C.; Hou, L. Seven days of mindfulness-based cognitive therapy improves attention and coping style. Soc. Behav. Personal. Int. J. 2018, 46, 421–430. [Google Scholar] [CrossRef]
- Bohus, M.; Huppertz, M. Wirkmechanismen achtsamkeitsbasierter Psychotherapie. Z. Für Psychiatr. Psychol. Psychother. 2006, 54, 265–276. [Google Scholar] [CrossRef]
- Snippe, E.; Dziak, J.J.; Lanza, S.T.; Nyklíček, I.; Wichers, M. The shape of change in perceived stress, negative affect, and stress sensitivity during mindfulness-based stress reduction. Mindfulness 2017, 8, 728–736. [Google Scholar] [CrossRef] [PubMed]
- Krampen, G. Entspannungsverfahren in Therapie und Prävention; Hogrefe Verlag: Göttingen, Germany, 2013. [Google Scholar]
- Payne, R.A. Relaxation Techniques; Elsevier: Amsterdam, The Netherlands, 2005. [Google Scholar]
- Segal, Z.; Williams, M.; Teasdale, J. Mindfulness-Based Cognitive Therapy For Depression; Guilford Publications: New York, NY, USA, 2018. [Google Scholar]
- Kachan, D.; Olano, H.; Tannenbaum, S.L.; Annane, D.W.; Mehta, A.; Arheart, K.L.; Fleming, L.E.; Yang, X.; McClure, L.A.; Lee, D.J. Peer reviewed: Prevalence of mindfulness practices in the us workforce: National health interview survey. Prev. Chronic Dis. 2017, 14, E01. [Google Scholar] [CrossRef] [PubMed]
- Simonsson, O.; Fisher, S.; Martin, M. Awareness and experience of mindfulness in Britain. Sociol. Res. Online 2021, 26, 833–852. [Google Scholar] [CrossRef]
- Baer, R.A. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin. Psychol. Sci. Pract. 2003, 10, 125. [Google Scholar] [CrossRef]
- Michalak, J.; Heidenreich, T.; Williams, J.M. Achtsamkeit; Hogrefe Verlag: Göttingen, Germany, 2021; Volume 48. [Google Scholar]
- Eberth, J.; Sedlmeier, P.; Schäfer, T. PROMISE: A model of insight and equanimity as the key effects of mindfulness meditation. Front. Psychol. 2019, 10, 2389. [Google Scholar] [CrossRef]
- Mak, C.; Whittingham, K.; Cunnington, R.; Boyd, R.N. Effect of mindfulness yoga programme MiYoga on attention, behaviour, and physical outcomes in cerebral palsy: A randomized controlled trial. Dev. Med. Child Neurol. 2018, 60, 922–932. [Google Scholar] [CrossRef]
- Gard, T.; Noggle, J.J.; Park, C.L.; Vago, D.R.; Wilson, A. Potential self-regulatory mechanisms of yoga for psychological health. Front. Hum. Neurosci. 2014, 8, 770. [Google Scholar] [CrossRef]
- Rueda, M.R.; Posner, M.I.; Rothbart, M.K. Attentional control and self-regulation. In Handbook of Self-Regulation: Research, Theory, and Applications, 2nd ed.; The Guilford Press: New York, NY, USA, 2004; pp. 284–299. [Google Scholar]
- Kabat-Zinn, J. Full Catastrophe Living; Bantam Dell: New York, NY, USA, 2013. [Google Scholar]
- Nyklíček, I.; Kuijpers, K.F. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: Is increased mindfulness indeed the mechanism? Ann. Behav. Med. 2008, 35, 331–340. [Google Scholar] [CrossRef]
- Tang, Y.-Y.; Ma, Y.; Fan, Y.; Feng, H.; Wang, J.; Feng, S.; Lu, Q.; Hu, B.; Lin, Y.; Li, J. Central and autonomic nervous system interaction is altered by short-term meditation. Proc. Natl. Acad. Sci. USA 2009, 106, 8865–8870. [Google Scholar] [CrossRef] [PubMed]
- Leyland, A.; Rowse, G.; Emerson, L.-M. Experimental effects of mindfulness inductions on self-regulation: Systematic review and meta-analysis. Emotion 2019, 19, 108. [Google Scholar] [CrossRef] [PubMed]
- Maier, S.U.; Makwana, A.B.; Hare, T.A. Acute stress impairs self-control in goal-directed choice by altering multiple functional connections within the brain’s decision circuits. Neuron 2015, 87, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Rogers, M.J. An Examination of a Yoga Intervention and Elementary Student’s Selective Attention and Executive Function in the School Setting. Ph.D. Thesis, University of Kentucky, Lexington, KY, USA, 2016. [Google Scholar]
- Marshall, M.; McClanahan, M.; McArthur Warren, S.; Rogers, R.; Ballmann, C. A comparison of the acute effects of different forms of yoga on physiological and psychological stress: A pilot study. Int. J. Environ. Res. Public Health 2020, 17, 6090. [Google Scholar] [CrossRef]
- Morf, C.C.; Mischel, W. Epilogue: Self-regulation, vulnerability, and implications for mental health. Self Identity 2002, 1, 191–199. [Google Scholar] [CrossRef]
- Shapiro, S.L.; Carlson, L.E.; Astin, J.A.; Freedman, B. Mechanisms of mindfulness. J. Clin. Psychol. 2006, 62, 373–386. [Google Scholar] [CrossRef]
- Gu, J.; Strauss, C.; Bond, R.; Cavanagh, K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin. Psychol. Rev. 2015, 37, 1–12. [Google Scholar] [CrossRef]
- Kuyken, W.; Watkins, E.; Holden, E.; White, K.; Taylor, R.S.; Byford, S.; Evans, A.; Radford, S.; Teasdale, J.D.; Dalgleish, T. How does mindfulness-based cognitive therapy work? Behav. Res. Ther. 2010, 48, 1105–1112. [Google Scholar] [CrossRef]
- Bansal, R.; Gupta, M.; Agarwal, B.; Sharma, S. Impact of short term yoga intervention on mental well being of medical students posted in community medicine: A pilot study. Indian J. Community Med. 2013, 38, 105. [Google Scholar] [CrossRef]
- Bilderbeck, A.C.; Farias, M.; Brazil, I.A.; Jakobowitz, S.; Wikholm, C. Participation in a 10-week course of yoga improves behavioural control and decreases psychological distress in a prison population. J. Psychiatr. Res. 2013, 47, 1438–1445. [Google Scholar] [CrossRef]
- Raghavendra, R.; Nagarathna, R.; Nagendra, H.; Gopinath, K.; Srinath, B.; Ravi, B.; Patil, S.; Ramesh, B.; Nalini, R. Effects of an integrated yoga programme on chemotherapy-induced nausea and emesis in breast cancer patients. Eur. J. Cancer Care 2007, 16, 462–474. [Google Scholar] [CrossRef] [PubMed]
- Satyapriya, M.; Nagendra, H.R.; Nagarathna, R.; Padmalatha, V. Effect of integrated yoga on stress and heart rate variability in pregnant women. Int. J. Gynecol. Obstet. 2009, 104, 218–222. [Google Scholar] [CrossRef]
- Qi, X.; Tong, J.; Chen, S.; He, Z.; Zhu, X. Comparing the Psychological Effects of Meditation- and Breathing-Focused Yoga Practice in Undergraduate Students. Front. Psychol. 2020, 11, 560152. [Google Scholar] [CrossRef] [PubMed]
- Streeter, C.C.; Gerbarg, P.L.; Whitfield, T.H.; Owen, L.; Johnston, J.; Silveri, M.M.; Gensler, M.; Faulkner, C.L.; Mann, C.; Wixted, M.; et al. Treatment of Major Depressive Disorder with Iyengar Yoga and Coherent Breathing: A Randomized Controlled Dosing Study. Altern. Complement. Ther. 2017, 23, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.; Lauche, R.; Langhorst, J.; Dobos, G. Is one yoga style better than another? A systematic review of associations of yoga style and conclusions in randomized yoga trials. Complement. Ther. Med. 2016, 25, 178–187. [Google Scholar] [CrossRef]
- Iyengar, B.K.S. Astadala Yogamala; Allied Publishers: New Delhi, India, 2000. [Google Scholar]
- Michalsen, A.; Jeitler, M.; Brunnhuber, S.; Lüdtke, R.; Büssing, A.; Musial, F.; Dobos, G.; Kessler, C. Iyengar yoga for distressed women: A 3-armed randomized controlled trial. Evid. Based. Complement. Alternat. Med. 2012, 2012, 408727. [Google Scholar] [CrossRef]
- Michalsen, A.; Grossman, P.; Acil, A.; Langhorst, J.; Lüdtke, R.; Esch, T.; Stefano, G.B.; Dobos, G.J. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. Med. Sci. Monit. 2005, 11, Cr555–Cr561. [Google Scholar]
- Woolery, A.; Myers, H.; Sternlieb, B.; Zeltzer, L. A yoga intervention for young adults with elevated symptoms of depression. Altern. Ther. Health Med. 2004, 10, 60–63. [Google Scholar]
- Felver, J.C.; Tipsord, J.M.; Morris, M.J.; Racer, K.H.; Dishion, T.J. The effects of mindfulness-based intervention on children’s attention regulation. J. Atten. Disord. 2017, 21, 872–881. [Google Scholar] [CrossRef]
- Acabchuk, R.L.; Brisson, J.M.; Park, C.L.; Babbott-Bryan, N.; Parmelee, O.A.; Johnson, B.T. Therapeutic Effects of Meditation, Yoga, and Mindfulness-Based Interventions for Chronic Symptoms of Mild Traumatic Brain Injury: A Systematic Review and Meta-Analysis. Appl. Psychol. Health Well-Being 2021, 13, 34–62. [Google Scholar] [CrossRef]
- Whole Medical Systems. In Handbook of Disease Burdens and Quality of Life Measures; Preedy, V.R., Watson, R.R., Eds.; Springer: New York, NY, USA, 2010; pp. 4352–4353. [Google Scholar]
- Satyapriya, M.; Nagarathna, R.; Padmalatha, V.; Nagendra, H. Effect of integrated yoga on anxiety, depression & well being in normal pregnancy. Complement. Ther. Clin. Pract. 2013, 19, 230–236. [Google Scholar] [PubMed]
- Kabat-Zinn, J. Mindfulness-based stress reduction (MBSR). Constr. Hum. Sci. 2003, 8, 73. [Google Scholar]
- Heidenreich, T.; Michalak, J.; Eifert, G. Balance von Veränderung und achtsamer Akzeptanz: Die dritte Welle der Verhaltenstherapie. Psychother. Psychosom. Med. Psychol. 2007, 57, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: Berlin/Heidelberg, Germany, 1984. [Google Scholar]
- Klein, E.M.; Brähler, E.; Dreier, M.; Reinecke, L.; Müller, K.W.; Schmutzer, G.; Wölfling, K.; Beutel, M.E. The German version of the Perceived Stress Scale–psychometric characteristics in a representative German community sample. BMC Psychiatry 2016, 16, 159. [Google Scholar] [CrossRef]
- Schneider, E.E.; Schönfelder, S.; Domke-Wolf, M.; Wessa, M. Measuring stress in clinical and nonclinical subjects using a German adaptation of the Perceived Stress Scale. Int. J. Clin. Health Psychol. 2020, 20, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Enzmann, D.; Kleiber, D. Helfer-Leiden: Stress und Burnout in Psychosozialen Berufen; Asanger: Heidelberg, Germany, 1989. [Google Scholar]
- Maslach, C.; Jackson, S.E. Maslach Burnout Inventory: Research Edition; Consulting Psychologists Press: Washington, DC, USA, 1981. [Google Scholar]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory; Scarecrow Education: Lanham, MD, USA, 1997. [Google Scholar]
- Gumz, A.; Erices, R.; Brähler, E.; Zenger, M. Faktorstruktur und Gütekriterien der deutschen Übersetzung des Maslach-Burnout-Inventars für Studierende von Schaufeli et al. (MBI-SS). Psychother. Psychosom. Med. Psychol. 2013, 63, 77–84. [Google Scholar] [CrossRef]
- Büssing, A.; Perrar, K.-M. Die Messung von Burnout. Untersuchung einer deutschen Fassung des Maslach Burnout Inventory (MBI-D). Measuring burnout: A study of a German version of the Maslach Burnout Inventory (MBI-D). Diagnostica 1992, 38, 328–353. [Google Scholar]
- Ellert, U.; Kurth, B.-M. Gesundheitsbezogene Lebensqualität bei Erwachsenen in Deutschland. Bundesgesundheitsblatt-Gesundh.-Gesundh. 2013, 56, 643–649. [Google Scholar] [CrossRef]
- Brähler, E.; Mühlan, H.; Albani, C.; Schmidt, S. Teststatistische Prüfung und Normierung der deutschen Versionen des EUROHIS-QOL Lebensqualität-Index und des WHO-5 Wohlbefindens-Index. Diagnostica 2007, 53, 83–96. [Google Scholar] [CrossRef]
- Zerssen, D.V. Selbstbeurteilungs-Skalen zur Abschätzung des “subjektiven Befundes” in psychopathologischen Querschnitt-und Längsschnitt-Untersuchungen. Arch. Psychiatr. Nervenkrankh. 1973, 217, 299–314. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Palmer, S.C. Hospital Anxiety Depression Scale. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 988–989. [Google Scholar]
- Herrmann, C. International experiences with the Hospital Anxiety and Depression Scale—A review of validation data and clinical results. J. Psychosom. Res. 1997, 42, 17–41. [Google Scholar] [CrossRef]
- Herrmann, C.; Buss, U. Vorstellung und Validierung einer deutschen Version der “Hospital Anxiety and Depression Scale” (HAD-Skala). Ein Fragebogen zur Erfassung des psychischen Befindens bei Patienten mit körperlichen Beschwerden. Description and validation of a German version of the Hospital Anxiety and Depression Scale (HADS): A questionnaire for identifying emotional disorders in physically ill patients. Diagnostica 1994, 40, 143–154. [Google Scholar]
- Herrmann-Lingen, C.; Buss, U.; Snaith, R.P. Hospital Anxiety and Depression Scale–Deutsche Version (HADS-D); Huber: Bern, Switzerland, 2011. [Google Scholar]
- Walach, H.; Buchheld, N.; Buttenmüller, V.; Kleinknecht, N.; Schmidt, S. Measuring mindfulness—The Freiburg Mindfulness Questionnaire. Construction, validation, short version. J. Medit. Med. Res. 2003, 3, 97–98. [Google Scholar]
- Heidenreich, T.; Ströhle, G.; Michalak, J. Achtsamkeit: Konzeptuelle aspekte und ergebnisse zum Freiburger achtsamkeitsfragebogen. Verhaltenstherapie 2006, 16, 33–40. [Google Scholar] [CrossRef]
- Mehling, W.E.; Price, C.; Daubenmier, J.J.; Acree, M.; Bartmess, E.; Stewart, A. The multidimensional assessment of interoceptive awareness (MAIA). PLoS ONE 2012, 7, e48230. [Google Scholar] [CrossRef]
- Valenzuela-Moguillansky, C.; Reyes-Reyes, A.; Gaete, M.I. Exteroceptive and interoceptive body-self awareness in fibromyalgia patients. Front. Hum. Neurosci. 2017, 11, 117. [Google Scholar] [CrossRef]
- Eggart, M.; Todd, J.; Valdés-Stauber, J. Validation of the Multidimensional Assessment of Interoceptive Awareness (MAIA-2) questionnaire in hospitalized patients with major depressive disorder. PLoS ONE 2021, 16, e0253913. [Google Scholar]
- Grossarth-Maticek, R.; Eysenck, H. Self-regulation and mortality from cancer, coronary heart disease, and other causes: A prospective study. Personal. Individ. Differ. 1995, 19, 781–795. [Google Scholar] [CrossRef]
- Grossarth-Maticek, R.A. Gesundheit und Problemlösung Durch Anregung der Selbstregulation; Walter de Gruyter: Berlin, Germany, 2000. [Google Scholar]
- Büssing, A.; Girke, M.; Heckmann, C.; Schad, F.; Ostermann, T.; Kröz, M. Validation of the self regulation questionnaire as a measure of health in quality of life research. Eur. J. Med. Res. 2009, 14, 223–227. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Büssing, A.; Föller-Mancini, A.; Gidley, J.; Heusser, P. Aspects of spirituality in adolescents. Int. J. Child. Spiritual. 2010, 15, 25–44. [Google Scholar] [CrossRef]
- Büssing, A.; Ostermann, T.; Matthiessen, P.F. Distinct Expressions of Vital Spirituality” The ASP Questionnaire as an Explorative Research Tool. J. Relig. Health 2007, 46, 267–286. [Google Scholar] [CrossRef]
- Büssing, A.; Pilchowska, I.; Baumann, K.; Surzykiewicz, J. Aspects of Spirituality in German and Polish Adolescents and Young Adults—Factorial Structure of the ASP Students’ Questionnaire. Religions 2014, 5, 109–125. [Google Scholar] [CrossRef]
- Hood, R.W., Jr.; Morris, R.J.; Watson, P.J. Further factor analysis of Hood’s Mysticism Scale. Psychol. Rep. 1993, 73, 1176–1178. [Google Scholar] [CrossRef]
- Hood, J.; Ralph, W.; Ghorbani, N.; Watson, P.J.; Ghramaleki, A.F.; Bing, M.N.; Davison, H.K.; Morris, R.J.; Williamson, W.P. Dimensions of the mysticism scale: Confirming the three-factor structure in the United States and Iran. J. Sci. Study Relig. 2001, 40, 691–705. [Google Scholar] [CrossRef]
- Streib, H.; Klein, C.; Keller, B.; Hood, R. The Mysticism Scale as a Measure for Subjective Spirituality: New Results with Hood’s M-Scale and the Development of a Short Form. In Assessing Spirituality in a Diverse World; Springer: Berlin/Heidelberg, Germany, 2021; pp. 467–491. [Google Scholar]
- Weathers, F.W.; Litz, B.T.; Herman, D.S.; Huska, J.A.; Keane, T.M. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. In Proceedings of the Annual Convention of the International Society for Traumatic Stress Studies, San Antonio, TX, USA, 24 October 1993. [Google Scholar]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- Sawilowsky, S.S. New effect size rules of thumb. J. Mod. Appl. Stat. Methods 2009, 8, 26. [Google Scholar] [CrossRef]
- Grossman, P. On measuring mindfulness in psychosomatic and psychological research. J. Psychosom. Res. 2008, 64, 405–408. [Google Scholar] [CrossRef]
- Mayring, P. Qualitative Inhaltsanalyse; UVK University-Verlag: Konstanz, Germany, 1994; Volume 14. [Google Scholar]
- Mayring, P. Qualitative Inhaltsanalyse. Handbuch Qualitativer Forschung: Grundlagen, Konzepte, Methoden und Anwendungen; Beltz Verlag: Weinheim, Germany, 1991. [Google Scholar]
- Della Valle, E.; Palermi, S.; Aloe, I.; Marcantonio, R.; Spera, R.; Montagnani, S.; Sirico, F. Effectiveness of workplace yoga interventions to reduce perceived stress in employees: A systematic review and meta-analysis. J. Funct. Morphol. Kinesiol. 2020, 5, 33. [Google Scholar] [CrossRef]
- Saper, R.B.; Lemaster, C.; Delitto, A.; Sherman, K.J.; Herman, P.M.; Sadikova, E.; Stevans, J.; Keosaian, J.E.; Cerrada, C.J.; Femia, A.L. Yoga, physical therapy, or education for chronic low back pain: A randomized noninferiority trial. Ann. Intern. Med. 2017, 167, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Peters, E.; Hübner, J.; Katalinic, A. Stress, Copingstrategien und gesundheitsbezogene Lebensqualität während der Corona-Pandemie im April 2020 in Deutschland. Dtsch. Med. Wochenschr. 2021, 146, e11–e20. [Google Scholar] [CrossRef]
- Matko, K.; Bringmann, H.C.; Sedlmeier, P. Effects of different components of yoga: A meta-synthesis. OBM Integr. Complement. Med. 2021, 6, 1. [Google Scholar]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Characteristic | Total | Integrative Yoga | Iyengar Yoga | Mindfulness |
|---|---|---|---|---|
| Female (%) | 91 (89.2%) | 31 (88.6%) | 28 (84.8%) | 32 (94.1%) |
| Male (%) | 11 (10.9%) | 4 (11.4%) | 5 (15.2%) | 2 (5.9%) |
| Age (SD) | 46.7 (11.5) | 46.0 (11.5) | 48.4 (10.6) | 45.7 (12.5) |
| Highest level of education | ||||
| University (%) | 73 (71.6%) | 25 (71.4%) | 24 (72.7%) | 24 (70.6%) |
| Highschool (%) | 13 (12.7%) | 4 (11.4%) | 4 (12.1%) | 5 (14.7%) |
| Secondary school (%) | 12 (11.8%) | 4 (11.4%) | 3 (9.1%) | 5 (14.7%) |
| No graduation (%) | 4 (3.9%) | 2 (5.7%) | 2 (6.1%) | 0 (0.0%) |
| Employment status | ||||
| Full-time (%) | 39 (38.2%) | 16 (45.7%) | 9 (27.3%) | 14 (41.2%) |
| Part-time (%) | 27 (26.4%) | 7 (20.0%) | 13 (39.4%) | 7 (20.5%) |
| Student/training (%) | 5 (4.9%) | 1 (2.9%) | 1 (3.0%) | 3 (8.8%) |
| Unemployed (%) | 1 (1.0%) | 0 (0.0%) | 0 (0.0%) | 1 (2.9%) |
| Pension (%) | 5 (4.9%) | 2 (5.7%) | 3 (9.1%) | 0 (0.0%) |
| Self-reported monthly income | ||||
| <1000€ (%) | 16 (15.7%) | 8 (22.9%) | 4 (12.1%) | 4 (11.8%) |
| 1001€–1500€ (%) | 13 (12.7%) | 5 (14.3%) | 3 (9.1%) | 5 (14.7%) |
| 1501€–2000€ (%) | 14 (13.7%) | 5 (14.3%) | 7 (21.2%) | 2 (5.9%) |
| 2001€–3000€ (%) | 25 (24.5%) | 10 (28.6%) | 6 (18.2%) | 9 (26.5%) |
| 3001€–4000€ (%) | 7 (6.9%) | 2 (5.7%) | 2 (6.1%) | 3 (8.8%) |
| >4000€ (%) | 4 (3.9%) | 0 (0.0%) | 4 (12.1%) | 0 (0.0%) |
| Not stated | 1 (1.0%) | 1 (2.9%) | 0 (0.0%) | 0 (0.0%) |
| Most common pre-existing conditions 1 | ||||
| Sleep disorder | 29 (28.4%) | 8 (22.9%) | 12 (36.4%) | 9 (26.5%) |
| Neck pain | 28 (27.5%) | 10 (28.6%) | 10 (30.3%) | 8 (23.5%) |
| Back pain | 23 (22.5%) | 5 (14.3%) | 10 (30.3%) | 8 (23.5%) |
| Digestive complaints | 22 (21.6%) | 9 (25.7%) | 6 (18.2%) | 7 (20.6%) |
| Tension headache | 13 (12.7%) | 4 (11.4%) | 4 (12.1%) | 5 (14.7%) |
| Hypertension | 8 (7.8%) | 6 (17.1%) | 1 (3.0%) | 1 (2.9%) |
| Stress (PSS) | ||||
| Score (SD) | 33.91 (4.80) | 33.39 (5.91) | 34.44 (5.84) | |
| Burnout (MBI) | ||||
| Cynicism (SD) | 12.94 (8.79) | 10.33 (6.90) | 12.94 (6.96) | |
| Exhaustion (SD) | 18.83 (6.36) | 19.52 (6.89) | 20.53 (6.19) | |
| Professional Efficacy (SD) | 25.46 (6.22) | 25.48 (6.88) | 24.21 (7.06) | |
| Quality of Life (SF-36) | ||||
| Mental Component Summary (SD) | 36.79 (7.30) | 38.86 (6.56) | 37.94 (7.46) | |
| Physical Component Summary (SD) | 45.74 (6.06) | 44.25 (6.35) | 45.30 (7.22) | |
| Physical Wellbeing (B-LR) | ||||
| Score (SD) | 25.46 (7.72) | 26.30 (8.38) | 26.00 (8.81) | |
| Depression (HADS) | ||||
| Anxiety (SD) | 10.34 (2.91) | 10.15 (3.46) | 9.91 (3.53) | |
| Depression (SD) | 7.86 (3.79) | 8.36 (3.80) | 7.12 (4.00) | |
| Mindfulness (FMI) | ||||
| Score (SD) | 2.28 (0.48) | 2.35 (0.50) | 2.35 (0.37) | |
| Interoceptive body awareness (MAIA) | ||||
| Noticing (SD) | 3.23 (1.06) | 3.21 (0.95) | 3.33 (1.03) | |
| Not-distracting (SD) | 2.06 (0.91) | 1.95 (1.00) | 1.73 (0.65) | |
| Not-worrying (SD) | 2.06 (1.08) | 2.24 (1.21) | 2.15 (0.81) | |
| Attention regulation (SD) | 2.01 (1.00) | 1.95 (1.05) | 1.96 (0.93) | |
| Emotional awareness (SD) | 3.65 (0.92) | 3.08 (1.12) | 3.28 (1.02) | |
| Self-regulation (SD) | 1.99 (0.94) | 1.75 (1.12) | 1.87 (1.05) | |
| Body listening (SD) | 1.80 (0.97) | 1.69 (1.38) | 1.67 (1.13) | |
| Trusting (SD) | 2.51 (1.15) | 2.33 (1.40) | 2.42 (1.18) | |
| Self-regulation (SRI) | ||||
| Score (SD) | 3.35 (0.87) | 3.36 (0.74) | 3.58 (0.76) | |
| Spirituality (ASP) | ||||
| Religious orientation (SD) | 2.10 (0.95) | 1.89 (0.91) | 1.88 (0.93) | |
| Search for wisdom (SD) | 2.24 (0.72) | 2.19 (0.65) | 2.23 (0.70) | |
| Conscious interactions (SD) | 2.86 (0.55) | 2.79 (0.81) | 2.86 (0.67) | |
| Transcendence conviction (SD) | 1.83 (0.97) | 1.68 (0.90) | 1.72 (0.94) | |
| Mysticism (HMS) | ||||
| Introvertive mysticism (SD) | 1.74 (3.51) | 3.18 (3.23) | 2.74 (3.46) | |
| Extrovertive mysticism (SD) | 1.03 (2.29) | 0.91 (2.47) | 1.12 (2.88) | |
| Interpretation (SD) | 2.46 (3.23) | 2.70 (3.57) | 2.65 (3.67) | |
| Posttraumatic stress (PCL-5) | ||||
| Score (SD) | 26.77 (13.80) | 26.03 (13.33) | 27.00 (15.02) |
| n | V0 | V1 | V2 | ΔV0–V1 | d V0–V1 | ΔV0–V2 | d V0–V2 | |
|---|---|---|---|---|---|---|---|---|
| Integrative yoga | 35 | 33.91 ± 4.80 | 27.23 ± 6.77 | 26.03 ± 4.91 | −6.69 ± 6.19 | 1.08 | −7.89 ± 5.60 | 1.41 |
| Iyengar yoga | 33 | 33.39 ± 5.91 | 27.39 ± 6.98 | 23.88 ± 5.58 | −6.00 ± 7.37 | 0.81 | −9.52 ± 6.94 | 1.37 |
| Mindfulness | 34 | 34.44 ± 5.84 | 24.71 ± 6.67 | 23.62 ± 6.43 | −9.74 ± 7.80 | 1.25 | −10.82 ± 8.77 | 1.23 |
| ΔV0–V1 | ΔV0–V2 | |||||||
| F | p | η2 | F | p | η2 | |||
| ANOVA | 2.621 | 0.078 | 0.050 | 1.439 | 0.242 | 0.028 | ||
| ΔV0–V1 | ΔV0–V2 | |||||||
| Post-hoc comparisons | t | p | η2 | t | p | η2 | ||
| Integrative–Iyengar | −0.414 | 0.680 | 0.003 | 1.062 | 0.292 | 0.017 | ||
| Integrative–Mindfulness | 1.795 | 0.077 | 0.045 | 1.653 | 0.104 | 0.039 | ||
| Iyengar–Mindfulness | 2.016 | 0.048 | 0.057 | 0.678 | 0.500 | 0.007 |
| Interview | Intervention | Participations | Gender | Course Period | Age |
|---|---|---|---|---|---|
| 1 | Iyengar yoga | 11/12 | female | January–April | 48 |
| 2 | Mindfulness training | 11/12 | male | January–April | 50 |
| 3 | Integrative yoga | 8/12 | female | January–April | 58 |
| 4 | Integrative yoga | 10/12 | female | January–April | 47 |
| 5 | Iyengar yoga | 7/12 | female | August–November | 64 |
| 6 | Mindfulness training | 11/12 | female | August–November | 63 |
| Changes |
| Everyday life |
| Self-care |
| Psychological changes |
| Somatic changes |
| Change as a process that takes time |
| Course evaluation |
| General evaluation |
| Educational share |
| Course instructor |
| Other |
| Hopes/Fears |
| Lockdown situation |
| Previous experience |
| Future |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fischer, J.M.; Kandil, F.-I.; Kessler, C.S.; Nayeri, L.; Zager, L.S.; Rocabado Hennhöfer, T.; Steckhan, N.; Koppold-Liebscher, D.A.; Bringmann, H.C.; Schäfer, T.; et al. Stress Reduction by Yoga versus Mindfulness Training in Adults Suffering from Distress: A Three-Armed Randomized Controlled Trial including Qualitative Interviews (RELAX Study). J. Clin. Med. 2022, 11, 5680. https://doi.org/10.3390/jcm11195680
Fischer JM, Kandil F-I, Kessler CS, Nayeri L, Zager LS, Rocabado Hennhöfer T, Steckhan N, Koppold-Liebscher DA, Bringmann HC, Schäfer T, et al. Stress Reduction by Yoga versus Mindfulness Training in Adults Suffering from Distress: A Three-Armed Randomized Controlled Trial including Qualitative Interviews (RELAX Study). Journal of Clinical Medicine. 2022; 11(19):5680. https://doi.org/10.3390/jcm11195680
Chicago/Turabian StyleFischer, Jan Moritz, Farid-Ihab Kandil, Christian S. Kessler, Lucas Nayeri, Laura Sophie Zager, Theresa Rocabado Hennhöfer, Nico Steckhan, Daniela A. Koppold-Liebscher, Holger C. Bringmann, Thomas Schäfer, and et al. 2022. "Stress Reduction by Yoga versus Mindfulness Training in Adults Suffering from Distress: A Three-Armed Randomized Controlled Trial including Qualitative Interviews (RELAX Study)" Journal of Clinical Medicine 11, no. 19: 5680. https://doi.org/10.3390/jcm11195680
APA StyleFischer, J. M., Kandil, F.-I., Kessler, C. S., Nayeri, L., Zager, L. S., Rocabado Hennhöfer, T., Steckhan, N., Koppold-Liebscher, D. A., Bringmann, H. C., Schäfer, T., Michalsen, A., & Jeitler, M. (2022). Stress Reduction by Yoga versus Mindfulness Training in Adults Suffering from Distress: A Three-Armed Randomized Controlled Trial including Qualitative Interviews (RELAX Study). Journal of Clinical Medicine, 11(19), 5680. https://doi.org/10.3390/jcm11195680





