C-Reactive Protein as Predictor for Infectious Complications after Robotic and Open Esophagectomies
Abstract
1. Introduction
2. Materials and Methods
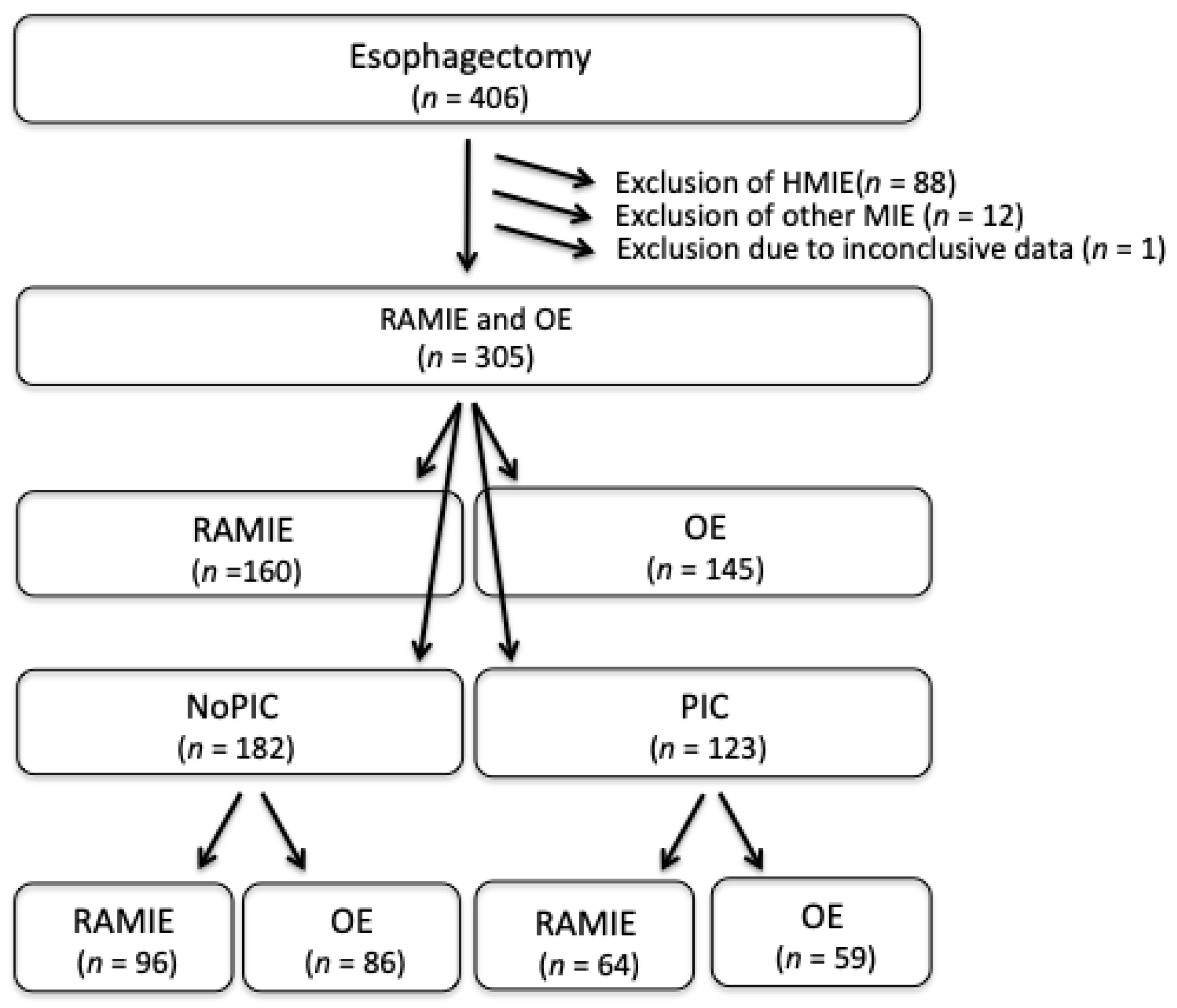
2.1. Patient Cohort
2.2. Treatment Protocol
2.3. Endpoints
2.4. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Postoperative Infectious Complications | ||||
|---|---|---|---|---|
| All (n = 305) | RAMIE (n = 182) | OE (n = 123) | p-Value | |
| PIC (POD10) (yes [n, %]) | 91 [29.8] | 41 [25.6] | 50 [34.5] | 0.09 c |
| PIC (POD30) (yes [n, %]) | 123 [40.3] | 64 [40.0] | 59 [40.7] | 0.90 a |
| Pneumonia (yes [n, %]) | 72 [23.6] | 35 [21.9] | 37 [25.5] | 0.45 a |
| Surgical Side infections (yes [n, %]) | 15 [4.9] | 3 [1.9] | 12 [8.3] | 0.01 c |
| Gastric conduit leakage (yes [n, %]) | 10 [3.3] | 6 [3.8] | 4 [2.8] | 0.63 c |
| Gastric conduit necrosis (yes [n, %]) | 9 [3.0] | 7 [4.4] | 2 [1.4] | 0.12 c |
| Anastomotic leakage (yes [n, %]) | 90 [29.5] | 49 [30.6] | 41 [28.3] | 0.65 c |
| Esophagobronchial Fistula (yes [n, %]) | 15 [4.9] | 10 [6.3] | 5 [3.4] | 0.26 c |
| CDC (yes [n, %]) I II III IV V | 84 [29.5] 3 [1.0] 34 [11.1] 146 [46.1] 14 [4.6] 29 [9.5] | 44 [27.5] 3 [1.9] 15 [9.4] 77 [48.1] 10 [6.3] 11 [6.9] | 40 [27.6] 0 19 [13.1] 64 [44.1] 4 [2.8] 18 [12.4] | 0.14 c |
| Readmission (POD 30) (yes [n, %]) | 33 [10.8] | 14 [8.8] | 19 [13.1] | 0.22 c |
| Recurrence (yes [n, %]) | 81 [26.7] | 38 [23.9] | 43 [29.9] | 0.24 c |
| Death (yes [n, %]) | 90 [29.5] | 56 [35.0] | 93 [64.1] | <0.001 c |
| Follow up (months, [median, range]) | 17.5 (0–144) | 12 (0–106) | 27 (0–144) | <0.001 a |
References
- Ajani, J.A.; Barthel, J.S.; Bentrem, D.J.; D’Amico, T.A.; Das, P.; Denlinger, C.S.; Fuchs, C.S.; Gerdes, H.; Glasgow, R.E.; Hayman, J.A.; et al. Esophageal and esophagogastric junction cancers. J. Natl. Compr. Canc. Netw. 2011, 9, 830–887. [Google Scholar] [CrossRef]
- Franke, F.; Moeller, T.; Mehdorn, A.S.; Beckmann, J.H.; Becker, T.; Egberts, J.H. Ivor-Lewis oesophagectomy: A standardized operative technique in 11 steps. Int. J. Med. Robot. 2021, 17, 1–10. [Google Scholar] [CrossRef] [PubMed]
- van der Sluis, P.C.; Schizas, D.; Liakakos, T.; van Hillegersberg, R. Minimally Invasive Esophagectomy. Dig. Surg. 2020, 37, 93–100. [Google Scholar] [CrossRef]
- Mehdorn, A.S.; Moller, T.; Franke, F.; Richter, F.; Kersebaum, J.N.; Becker, T.; Egberts, J.H. Long-Term, Health-Related Quality of Life after Open and Robot-Assisted Ivor-Lewis Procedures-A Propensity Score-Matched Study. J. Clin. Med. 2020, 9, 3513. [Google Scholar] [CrossRef] [PubMed]
- Heits, N.; Bernsmeier, A.; Reichert, B.; Hauser, C.; Hendricks, A.; Seifert, D.; Richter, F.; Schafmayer, C.; Ellrichmann, M.; Schniewind, B.; et al. Long-term quality of life after endovac-therapy in anastomotic leakages after esophagectomy. J. Thorac. Dis. 2018, 10, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Aselmann, H.; Kersebaum, J.N.; Bernsmeier, A.; Beckmann, J.H.; Moller, T.; Egberts, J.H.; Schafmayer, C.; Rocken, C.; Becker, T. Robotic-assisted total mesorectal excision (TME) for rectal cancer results in a significantly higher quality of TME specimen compared to the laparoscopic approach-report of a single-center experience. Int. J. Colorectal Dis. 2018, 33, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Beeraka, N.M.; Zhang, J.; Reshetov, I.V.; Nikolenko, V.N.; Sinelnikov, M.Y.; Mikhaleva, L.M. Efficacy of da Vinci robot-assisted lymph node surgery than conventional axillary lymph node dissection in breast cancer—A comparative study. Int. J. Med. Robot 2021, 17, e2307. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Zhang, J.; Beeraka, N.M.; Sinelnikov, M.Y.; Zhang, X.; Cao, Y.; Lu, P. Robot-Assisted Minimally Invasive Breast Surgery: Recent Evidence with Comparative Clinical Outcomes. J. Clin. Med. 2022, 11, 1827. [Google Scholar] [CrossRef]
- Egberts, J.H.; Kersebaum, J.N.; Mann, B.; Aselmann, H.; Hirschburger, M.; Grass, J.; Becker, T.; Izbicki, J.; Perez, D. Defining benchmarks for robotic-assisted low anterior rectum resection in low-morbid patients: A multicenter analysis. Int. J. Colorectal Dis. 2021, 36, 1945–1953. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.W.; Wei, P.L.; Chen, C.C.; Kuo, L.J.; Wang, J.Y. Clinical Safety and Effectiveness of Robotic-Assisted Surgery in Patients with Rectal Cancer: Real-World Experience over 8 Years of Multiple Institutions with High-Volume Robotic-Assisted Surgery. Cancers 2022, 14, 4175. [Google Scholar] [CrossRef] [PubMed]
- Mehdorn, A.S.; Richter, F.; Hess, K.; Beckmann, J.H.; Egberts, J.H.; Linecker, M.; Becker, T.; Braun, F. The Role of ICG in Robot-Assisted Liver Resections. J. Clin. Med. 2022, 11, 4175. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, H.; Miyata, H.; Gotoh, M.; Kitagawa, Y.; Baba, H.; Kimura, W.; Tomita, N.; Nakagoe, T.; Shimada, M.; Sugihara, K.; et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann. Surg. 2014, 260, 259–266. [Google Scholar] [CrossRef]
- Zingg, U.; Smithers, B.M.; Gotley, D.C.; Smith, G.; Aly, A.; Clough, A.; Esterman, A.J.; Jamieson, G.G.; Watson, D.I. Factors associated with postoperative pulmonary morbidity after esophagectomy for cancer. Ann. Surg. Oncol. 2011, 18, 1460–1468. [Google Scholar] [CrossRef] [PubMed]
- Rahbari, N.N.; Weitz, J.; Hohenberger, W.; Heald, R.J.; Moran, B.; Ulrich, A.; Holm, T.; Wong, W.D.; Tiret, E.; Moriya, Y.; et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: A proposal by the International Study Group of Rectal Cancer. Surgery 2010, 147, 339–351. [Google Scholar] [CrossRef] [PubMed]
- Kassis, E.S.; Kosinski, A.S.; Ross, P., Jr.; Koppes, K.E.; Donahue, J.M.; Daniel, V.C. Predictors of anastomotic leak after esophagectomy: An analysis of the society of thoracic surgeons general thoracic database. Ann. Thorac. Surg. 2013, 96, 1919–1926. [Google Scholar] [CrossRef] [PubMed]
- Zehetner, J.; DeMeester, S.R.; Alicuben, E.T.; Oh, D.S.; Lipham, J.C.; Hagen, J.A.; DeMeester, T.R. Intraoperative Assessment of Perfusion of the Gastric Graft and Correlation With Anastomotic Leaks After Esophagectomy. Ann. Surg. 2015, 262, 74–78. [Google Scholar] [CrossRef]
- Ikeguchi, M.; Oka, S.; Gomyo, Y.; Tsujitani, S.; Maeta, M.; Kaibara, N. Postoperative morbidity and mortality after gastrectomy for gastric carcinoma. Hepatogastroenterology 2001, 48, 1517–1520. [Google Scholar] [PubMed]
- Lang, H.; Piso, P.; Stukenborg, C.; Raab, R.; Jahne, J. Management and results of proximal anastomotic leaks in a series of 1114 total gastrectomies for gastric carcinoma. Eur. J. Surg. Oncol. 2000, 26, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Alanezi, K.; Urschel, J.D. Mortality secondary to esophageal anastomotic leak. Ann. Thorac. Cardiovasc. Surg. Off. J. Assoc. Thorac. Cardiovasc. Surg. Asia 2004, 10, 71–75. [Google Scholar]
- Babic, B.; Tagkalos, E.; Gockel, I.; Corvinus, F.; Hadzijusufovic, E.; Hoppe-Lotichius, M.; Lang, H.; van der Sluis, P.C.; Grimminger, P.P. C-reactive Protein Levels After Esophagectomy Are Associated With Increased Surgical Trauma and Complications. Ann. Thorac. Surg. 2020, 109, 1574–1583. [Google Scholar] [CrossRef] [PubMed]
- Lin, E.; Calvano, S.E.; Lowry, S.F. Inflammatory cytokines and cell response in surgery. Surgery 2000, 127, 117–126. [Google Scholar] [CrossRef]
- Santonocito, C.; De Loecker, I.; Donadello, K.; Moussa, M.D.; Markowicz, S.; Gullo, A.; Vincent, J.L. C-reactive protein kinetics after major surgery. Anesth. Analg. 2014, 119, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Kokotovic, D.; Burcharth, J.; Helgstrand, F.; Gogenur, I. Systemic inflammatory response after hernia repair: A systematic review. Langenbeck’s Arch. Surg./Dtsch. Ges. Fur Chir. 2017, 402, 1023–1037. [Google Scholar] [CrossRef] [PubMed]
- Gordon, A.C.; Cross, A.J.; Foo, E.W.; Roberts, R.H. C-reactive protein is a useful negative predictor of anastomotic leak in oesophago-gastric resection. ANZ J. Surg. 2018, 88, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Adamina, M.; Steffen, T.; Tarantino, I.; Beutner, U.; Schmied, B.M.; Warschkow, R. Meta-analysis of the predictive value of C-reactive protein for infectious complications in abdominal surgery. Br. J. Surg. 2015, 102, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Munoz, J.L.; Alvarez, M.O.; Cuquerella, V.; Miranda, E.; Pico, C.; Flores, R.; Resalt-Pereira, M.; Moya, P.; Perez, A.; Arroyo, A. Procalcitonin and C-reactive protein as early markers of anastomotic leak after laparoscopic colorectal surgery within an enhanced recovery after surgery (ERAS) program. Surg. Endosc. 2018, 32, 4003–4010. [Google Scholar] [CrossRef] [PubMed]
- Egberts, J.H.; Biebl, M.; Perez, D.R.; Mees, S.T.; Grimminger, P.P.; Muller-Stich, B.P.; Stein, H.; Fuchs, H.; Bruns, C.J.; Hackert, T.; et al. Robot-Assisted Oesophagectomy: Recommendations Towards a Standardised Ivor Lewis Procedure. J. Gastrointest. Surg. Off. J. Soc. Surg. Aliment. Tract 2019, 23, 1485–1492. [Google Scholar] [CrossRef] [PubMed]
- Egberts, J.H.; Stein, H.; Aselmann, H.; Hendricks, A.; Becker, T. Fully robotic da Vinci Ivor-Lewis esophagectomy in four-arm technique-problems and solutions. Dis. Esophagus. 2017, 30, 1–9. [Google Scholar] [CrossRef][Green Version]
- Gisbertz, S.S.; Hagens, E.R.C.; Ruurda, J.P.; Schneider, P.M.; Tan, L.J.; Domrachev, S.A.; Hoeppner, J.; van Berge Henegouwen, M.I. The evolution of surgical approach for esophageal cancer. Ann. N. Y. Acad. Sci. 2018, 1434, 149–155. [Google Scholar] [CrossRef]
- Lewis, I. The surgical treatment of carcinoma of the oesophagus; with special reference to a new operation for growths of the middle third. Br. J. Surg. 1946, 34, 18–31. [Google Scholar] [CrossRef]
- Rice, T.W.; Patil, D.T.; Blackstone, E.H. 8th edition AJCC/UICC staging of cancers of the esophagus and esophagogastric junction: Application to clinical practice. Ann. Cardiothorac. Surg. 2017, 6, 119–130. [Google Scholar] [CrossRef]
- Arnold, M.; Soerjomataram, I.; Ferlay, J.; Forman, D. Global incidence of oesophageal cancer by histological subtype in 2012. Gut 2015, 64, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Booka, E.; Kikuchi, H.; Hiramatsu, Y.; Takeuchi, H. The Impact of Infectious Complications after Esophagectomy for Esophageal Cancer on Cancer Prognosis and Treatment Strategy. J. Clin. Med. 2021, 10, 4614. [Google Scholar] [CrossRef]
- Egberts, J.H.; Welsch, T.; Merboth, F.; Korn, S.; Praetorius, C.; Stange, D.E.; Distler, M.; Biebl, M.; Pratschke, J.; Nickel, F.; et al. Robotic-assisted minimally invasive Ivor Lewis esophagectomy within the prospective multicenter German da Vinci Xi registry trial. Langenbeck’s Arch. Surg./Dtsch. Ges. Fur Chir. 2022, 407, 1–11. [Google Scholar] [CrossRef]
- Gao, Y.B.; Chen, Z.L.; Li, J.G.; Hu, X.D.; Shi, X.J.; Sun, Z.M.; Zhang, F.; Zhao, Z.R.; Li, Z.T.; Liu, Z.Y.; et al. Genetic landscape of esophageal squamous cell carcinoma. Nat. Genet. 2014, 46, 1097–1102. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Yao, H.; Huang, Q.; Lu, H.; Xu, M.; Wu, J. A novel nomogram to predict the risk of anastomotic leakage in patients after oesophagectomy. BMC Surg. 2020, 20, 64. [Google Scholar] [CrossRef] [PubMed]
- Lagergren, J.; Smyth, E.; Cunningham, D.; Lagergren, P. Oesophageal cancer. Lancet 2017, 390, 2383–2396. [Google Scholar] [CrossRef]
- Pennathur, A.; Gibson, M.K.; Jobe, B.A.; Luketich, J.D. Oesophageal carcinoma. Lancet 2013, 381, 400–412. [Google Scholar] [CrossRef]
- Bundred, J.R.; Hollis, A.C.; Evans, R.; Hodson, J.; Whiting, J.L.; Griffiths, E.A. Impact of postoperative complications on survival after oesophagectomy for oesophageal cancer. BJS Open 2020, 4, 405–415. [Google Scholar] [CrossRef]
- Metcalfe, C.; Avery, K.; Berrisford, R.; Barham, P.; Noble, S.M.; Fernandez, A.M.; Hanna, G.; Goldin, R.; Elliott, J.; Wheatley, T.; et al. Comparing open and minimally invasive surgical procedures for oesophagectomy in the treatment of cancer: The ROMIO (Randomised Oesophagectomy: Minimally Invasive or Open) feasibility study and pilot trial. Health Technol. Assess 2016, 20, 1–68. [Google Scholar] [CrossRef]
- Richter, F.; Hendricks, A.; Schniewind, B.; Hampe, J.; Heits, N.; von Schonfels, W.; Reichert, B.; Eberle, K.; Ellrichmann, M.; Baumann, P.; et al. Eso-Sponge(R) for anastomotic leakage after oesophageal resection or perforation: Outcomes from a national, prospective multicentre registry. BJS Open 2022, 6, zrac030. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhong, K.; Guan, Y.; Zhang, H.T.; Zhang, H.; Pan, T.; Pan, J.; Wang, D.J. Evaluation of the significance of interleukin-6 in the diagnosis of postoperative pneumonia: A prospective study. BMC Cardiovasc. Disord 2022, 22, 306. [Google Scholar] [CrossRef] [PubMed]
- Jin, D.; Yuan, L.; Li, F.; Wang, S.; Mao, Y. A novel nomogram predicting the risk of postoperative pneumonia for esophageal cancer patients after minimally invasive esophagectomy. Surg. Endosc. 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- van der Sluis, P.C.; van der Horst, S.; May, A.M.; Schippers, C.; Brosens, L.A.A.; Joore, H.C.A.; Kroese, C.C.; Haj Mohammad, N.; Mook, S.; Vleggaar, F.P.; et al. Robot-assisted Minimally Invasive Thoracolaparoscopic Esophagectomy Versus Open Transthoracic Esophagectomy for Resectable Esophageal Cancer: A Randomized Controlled Trial. Ann. Surg. 2019, 269, 621–630. [Google Scholar] [CrossRef]
- Biere, S.S.; van Berge Henegouwen, M.I.; Maas, K.W.; Bonavina, L.; Rosman, C.; Garcia, J.R.; Gisbertz, S.S.; Klinkenbijl, J.H.; Hollmann, M.W.; de Lange, E.S.; et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: A multicentre, open-label, randomised controlled trial. Lancet 2012, 379, 1887–1892. [Google Scholar] [CrossRef]
- Mariette, C.; Markar, S.R.; Dabakuyo-Yonli, T.S.; Meunier, B.; Pezet, D.; Collet, D.; D’Journo, X.B.; Brigand, C.; Perniceni, T.; Carrere, N.; et al. Hybrid Minimally Invasive Esophagectomy for Esophageal Cancer. N. Engl. J. Med. 2019, 380, 152–162. [Google Scholar] [CrossRef]
- Glatz, T.; Marjanovic, G.; Kulemann, B.; Sick, O.; Hopt, U.T.; Hoeppner, J. Hybrid minimally invasive esophagectomy vs. open esophagectomy: A matched case analysis in 120 patients. Langenbeck’s Arch. Surg./Dtsch. Ges. Fur Chir. 2017, 402, 323–331. [Google Scholar] [CrossRef]
- Mantovani, A.; Allavena, P.; Sica, A.; Balkwill, F. Cancer-related inflammation. Nature 2008, 454, 436–444. [Google Scholar] [CrossRef]
- Zhang, F.; Bu, L.J.; Wang, R.; Da, J.; Ding, J.X.; Peng, W.R. Pretreatment BAN Score Based on Body-mass-index, Albumin and Neutrophil-lymphocyte Ratio Could Predict Long-term Survival for Patients with Operable Esophageal Squamous Cell Carcinoma. J. Cancer 2022, 13, 2768–2774. [Google Scholar] [CrossRef]
- Miarka, L.; Hauser, C.; Helm, O.; Holdhof, D.; Beckinger, S.; Egberts, J.H.; Gundlach, J.P.; Lenk, L.; Rahn, S.; Mikulits, W.; et al. The Hepatic Microenvironment and TRAIL-R2 Impact Outgrowth of Liver Metastases in Pancreatic Cancer after Surgical Resection. Cancers 2019, 11, 745. [Google Scholar] [CrossRef]
- Retsky, M.; Demicheli, R.; Hrushesky, W.J.; Forget, P.; De Kock, M.; Gukas, I.; Rogers, R.A.; Baum, M.; Sukhatme, V.; Vaidya, J.S. Reduction of breast cancer relapses with perioperative non-steroidal anti-inflammatory drugs: New findings and a review. Curr. Med. Chem. 2013, 20, 4163–4176. [Google Scholar] [CrossRef]
- Scarpa, M.; Cavallin, F.; Saadeh, L.M.; Pinto, E.; Alfieri, R.; Cagol, M.; Da Roit, A.; Pizzolato, E.; Noaro, G.; Pozza, G.; et al. Hybrid minimally invasive esophagectomy for cancer: Impact on postoperative inflammatory and nutritional status. Dis. Esophagus 2016, 29, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Zaher, E.H.A.; Ghareeb, W.M.; Fouad, A.M.; Madbouly, K.; Fathy, H.; Vedin, T.; Edelhamre, M.; Emile, S.H.; Faisal, M. Role of the triad of procalcitonin, C-reactive protein, and white blood cell count in the prediction of anastomotic leak following colorectal resections. World J. Surg. Oncol. 2022, 20, 33. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Yang, L.; Huang, Y.; Wang, T.; Sun, X.; Tong, X.; Liu, W.; Yin, Y.; Tao, K.; Zhang, P. Diagnostic accuracy of C-reactive protein and procalcitonin in the early diagnosis of infections after laparoscopic rectal cancer surgery. ANZ J. Surg. 2022. [Google Scholar] [CrossRef]
- Neary, C.; McAnena, P.; McAnena, O.; Kerin, M.; Collins, C. C-Reactive Protein-Lymphocyte Ratio Identifies Patients at Low Risk for Major Morbidity after Oesophagogastric Resection for Cancer. Dig. Surg. 2020, 37, 515–523. [Google Scholar] [CrossRef]
- Barrie, J.; Cockbain, A.; Tsachiridi, M.; Surendrakumar, V.; Maxwell, M.; Tamhankar, A.P. Predicting Delayed Complications After Esophagectomy in the Current Era of Early Discharge and Enhanced Recovery. Am. Surg. 2020, 86, 615–620. [Google Scholar] [CrossRef]
- Booka, E.; Kikuchi, H.; Haneda, R.; Soneda, W.; Kawata, S.; Murakami, T.; Matsumoto, T.; Hiramatsu, Y.; Takeuchi, H. Usefulness of Procalcitonin as a Predictor of Long-Term Prognosis in the Early Postoperative Period after Esophagectomy for Esophageal Cancer. J. Clin. Med. 2022, 11, 3359. [Google Scholar] [CrossRef] [PubMed]
- Bundred, J.; Hollis, A.C.; Hodson, J.; Hallissey, M.T.; Whiting, J.L.; Griffiths, E.A. Validation of the NUn score as a predictor of anastomotic leak and major complications after Esophagectomy. Dis. Esophagus 2020, 33, doz041. [Google Scholar] [CrossRef]
- Noble, F.; Curtis, N.; Harris, S.; Kelly, J.J.; Bailey, I.S.; Byrne, J.P.; Underwood, T.J.; South Coast Cancer, C.-O.-G. Risk assessment using a novel score to predict anastomotic leak and major complications after oesophageal resection. J. Gastrointest. Surg. Off. J. Soc. Surg. Aliment. Tract 2012, 16, 1083–1095. [Google Scholar] [CrossRef]
- Pochhammer, J.; Drozdzynski, J.; Bernsmeier, A.; Kersebaum, J.N.; Laudes, M.; Mehdorn, A.S.; Richter, F.; Schafmayer, C.; Becker, T.; Beckmann, J.H. Low Postoperative Levels of C-Reactive Protein Are an Early Predictor for an Uncomplicated Course After Bariatric Surgery: A Retrospective, Validated Cohort Study. Surg. Laparosc. Endosc. Percutan Tech. 2020, 30, 238–244. [Google Scholar] [CrossRef]
- Liesenfeld, L.F.; Sauer, P.; Diener, M.K.; Hinz, U.; Schmidt, T.; Muller-Stich, B.P.; Hackert, T.; Buchler, M.W.; Schaible, A. Prognostic value of inflammatory markers for detecting anastomotic leakage after esophageal resection. BMC Surg. 2020, 20, 324. [Google Scholar] [CrossRef] [PubMed]
- Findlay, J.M.; Tilson, R.C.; Harikrishnan, A.; Sgromo, B.; Marshall, R.E.; Maynard, N.D.; Gillies, R.S.; Middleton, M.R. Attempted validation of the NUn score and inflammatory markers as predictors of esophageal anastomotic leak and major complications. Dis. Esophagus 2015, 28, 626–633. [Google Scholar] [CrossRef] [PubMed]

| RAMIE (n = 160) | OE (n = 145) | p-Value | |
|---|---|---|---|
| Sex (male [n, %]) | 131 [81.9] | 116 [80.0] | 0.63 b |
| Age (years [mean ± SD]) | 64.0 ± 9.3 | 65.2 ± 10.3 | 0.29 a |
| BMI (kg/m2, [mean ± SD]) | 26.6 ± 4.8 | 26.6 ± 5.2 | 0.97 a |
| Smoking (yes [n, %]) | 57 [35.6] | 45 [31.0] | 0.70 b |
| ASA ≥ 3 (yes [n, %]) | 107 [66.9] | 96 [66.2] | 0.90 b |
| Entity [n, %] | 0.05 b | ||
| Adenocarcinoma | 141 [88.1] | 113 [66.2] | |
| Squamous cell carcinoma | 15 [9.4] | 23 [15.9] | |
| Other | 4 [2.5] | 9 [6.2] | |
| Procedure [n, %] | <0.001 a | ||
| Ivor-Lewis | 146 [88.1] | 108 [75.5] | |
| Transhiatal oesophagectomy | 5 [3.1] | 29 [20.0] | |
| McKeown | 9 [5.6] | 8 [5.5] | |
| Length of surgery (min, [mean ± SD]) | 329.3 ± 74.1 | 293.0 ± 89.5 | <0.010 a |
| Neoadjuvant treatment [n, %] | |||
| Radiotherapy | 44 [27.5] | 25 [17.2] | 0.03 b |
| Chemotherapy | 123 [76.9] | 86 [59.3] | <0.01 b |
| Adjuvant treatment [n, %] | |||
| Radiotherapy | 5 [3.1] | 10 [7.2] | 0.11 b |
| Chemotherapy | 65 [42.2] | 46 [38.7] | 0.55 b |
| PIC (yes [n, %]) | 64 (40.0) | 59 (40.7) | 0.09 b |
| Length of hospital stay (days, [median, range]) | 20.5 (4–112) | 19 (1–171) | 0.59 b |
| Postoperative Infectious Complication until POD 30 | |||
|---|---|---|---|
| NoPIC (n = 182) | PIC (n = 123) | p-Value | |
| Sex (male [n, %]) | 149 [48.9] | 98 [39.7] | 0.63 c |
| Age (years [mean ± SD]) | 64.4 ± 9.9 | 64.8 ± 9.7 | 0.73 a |
| BMI (kg/m2, [mean ± SD]) | 26.2 ± 4.8 | 27.3 ± 5.3 | 0.08 a |
| Smoking (yes [n, %]) | 57 [18.7] | 45 [14.8] | 0.15 c |
| ASA ≥ 3 (yes [n, %]) | 126 [41.3] | 77 [25.3] | 0.23 c |
| Entity [n, %] | 0.56 c | ||
| Adenocarcinoma | 155 [50.8] | 99 [32.5] | |
| Squamous cell carcinoma | 20 [6.6] | 18 [5.9] | |
| Other | 7 [2.3] | 6 [2.0] | |
| Surgical approach [n, %] | |||
| RAMIE | 96 [31.8] | 64 [21.0] | 0.90 c |
| OE | 86 [28.2] | 59 [19.3] | |
| Procedure [n, %] | 0.83 c | ||
| Ivor-Lewis | 153 [50.2] | 101 [33.1] | |
| Transhiatal oesophagectomy | 20 [6.6] | 14 [4.6] | |
| McKeown | 9 [3.0] | 8 [2.6] | |
| Length of surgery (min, [mean ± SD]) | 310.4 ± 81.2 | 314.7 ± 87.3 | 0.66 c |
| Neoadjuvant treatment [n, %] | |||
| Radiotherapy | 38 [12.5] | 31 [10.2] | 0.38 c |
| Chemotherapy | 129 [42.3] | 80 [26.2] | 0.28 c |
| Adjuvant treatment [n, %] | |||
| Radiotherapy | 11 [3.7] | 4 [1.4] | 0.28 c |
| Chemotherapy | 80 [29.3] | 31 [11.4] | <0.001 c |
| Length of hospital stay (days, [median, range]) | 14 (6–58) | 39 (1–171) | <0.001 b |
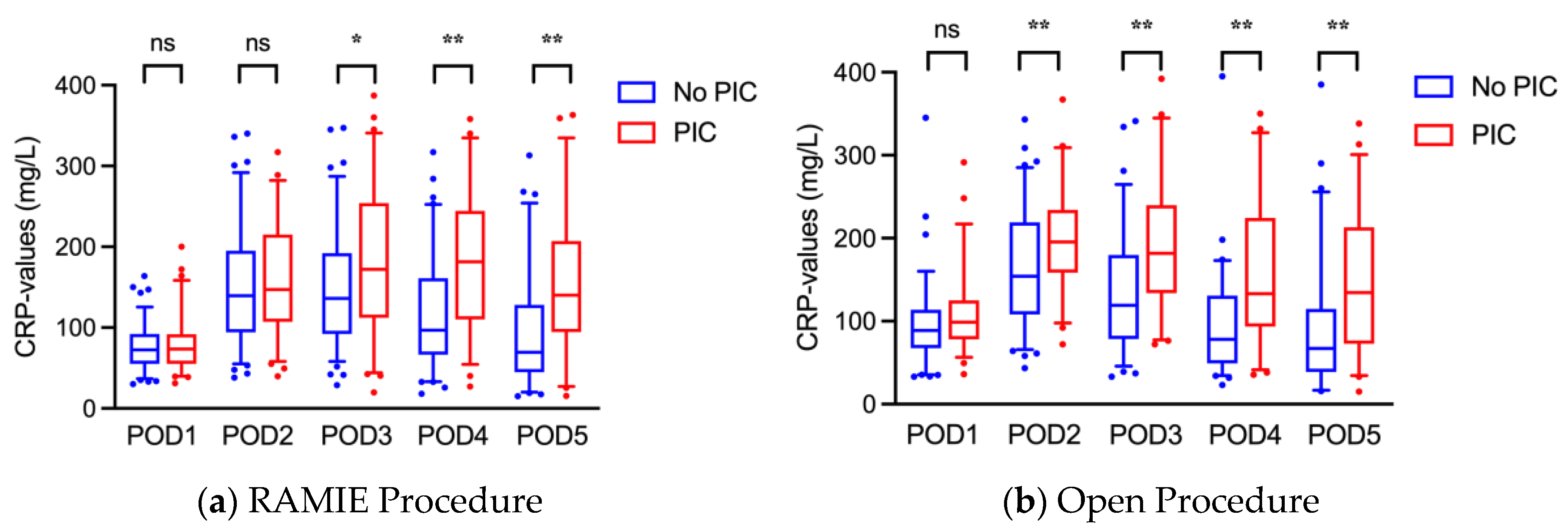
| CRP (mg/L) | NoPIC (n = 182) | PIC (n = 123) | p-Value | PCT (mg/L) | NoPIC (n = 182) | PIC (n = 123) | p-Value |
|---|---|---|---|---|---|---|---|
| POD 1 | 84.5 ± 38.4 | 93.5 ± 42.7 | 0.07 | POD 1 | 1.4 ± 2.9 | 2.1 ± 5.2 | 0.24 |
| POD 2 | 155.5 ± 68.0 | 177.5 ± 69.1 | <0.01 | POD 2 | 1.1 ± 1.7 | 2.8 ± 11.9 | 0.23 |
| POD 3 | 141.1 ± 70.5 | 186.3 ± 84.1 | <0.01 | POD 3 | 0.9 ± 1.2 | 2.4 ± 5.8 | 0.06 |
| POD 4 | 107.0 ± 65.2 | 170.0 ± 84.6 | <0.01 | POD 4 | 1.2 ± 2.6 | 2.9 ± 10.1 | 0.26 |
| POD 5 | 81.9 ± 70.5 | 150.7 ± 86.0 | <0.01 | POD 5 | 1.0 ± 2.2 | 3.6 ± 11.4 | 0.12 |
| POD 2-1 | 70.9 ± 50.9 | 87.3 ± 57.8 | 0.02 | ||||
| POD 3-2 | −15.3 ± 47.4 | 12.7 ± 52.9 | <0.01 | ||||
| POD 4-3 | −37.9 ± 40.9 | −23.4 ± 50.0 | 0.02 |
| Odds Ratio (95% CI) | p-Value | Cut-Off | AUC | NPV | PPV | ||
|---|---|---|---|---|---|---|---|
| RAMIE | POD 4 | 1.01 (1.01–1.02) | <0.01 | 168.0 | 0.73 | 73.9 | 65.2 |
| POD 5 | 1.01 (1.00–1.01) | <0.01 | 70 | 0.70 | 83.7 | 59.3 | |
| OE | POD 4 | 1.01 (1.01–1.02) | <0.01 | 88.3 | 0.74 | 80.4 | 58.9 |
| POD 5 | 1.01 (1.00–1.01) | <0.01 | 142.0 | 0.73 | 71.1 | 78.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Richter, F.; Mehdorn, A.-S.; Fedders, T.; Reichert, B.; Egberts, J.-H.; Becker, T.; Pochhammer, J. C-Reactive Protein as Predictor for Infectious Complications after Robotic and Open Esophagectomies. J. Clin. Med. 2022, 11, 5654. https://doi.org/10.3390/jcm11195654
Richter F, Mehdorn A-S, Fedders T, Reichert B, Egberts J-H, Becker T, Pochhammer J. C-Reactive Protein as Predictor for Infectious Complications after Robotic and Open Esophagectomies. Journal of Clinical Medicine. 2022; 11(19):5654. https://doi.org/10.3390/jcm11195654
Chicago/Turabian StyleRichter, Florian, Anne-Sophie Mehdorn, Thorben Fedders, Benedikt Reichert, Jan-Hendrik Egberts, Thomas Becker, and Julius Pochhammer. 2022. "C-Reactive Protein as Predictor for Infectious Complications after Robotic and Open Esophagectomies" Journal of Clinical Medicine 11, no. 19: 5654. https://doi.org/10.3390/jcm11195654
APA StyleRichter, F., Mehdorn, A.-S., Fedders, T., Reichert, B., Egberts, J.-H., Becker, T., & Pochhammer, J. (2022). C-Reactive Protein as Predictor for Infectious Complications after Robotic and Open Esophagectomies. Journal of Clinical Medicine, 11(19), 5654. https://doi.org/10.3390/jcm11195654






