Relationship between Selected Micronutrient Concentrations, Total Antioxidant Status, Pain Severity, and the Image of 1H MR Spectroscopy in Degenerative Spine Disease: A Case-Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and the Control Group Characteristic
2.2. Study Design
2.3. Sample Preparation and Biochemical Analyses
2.4. Statistical Analysis
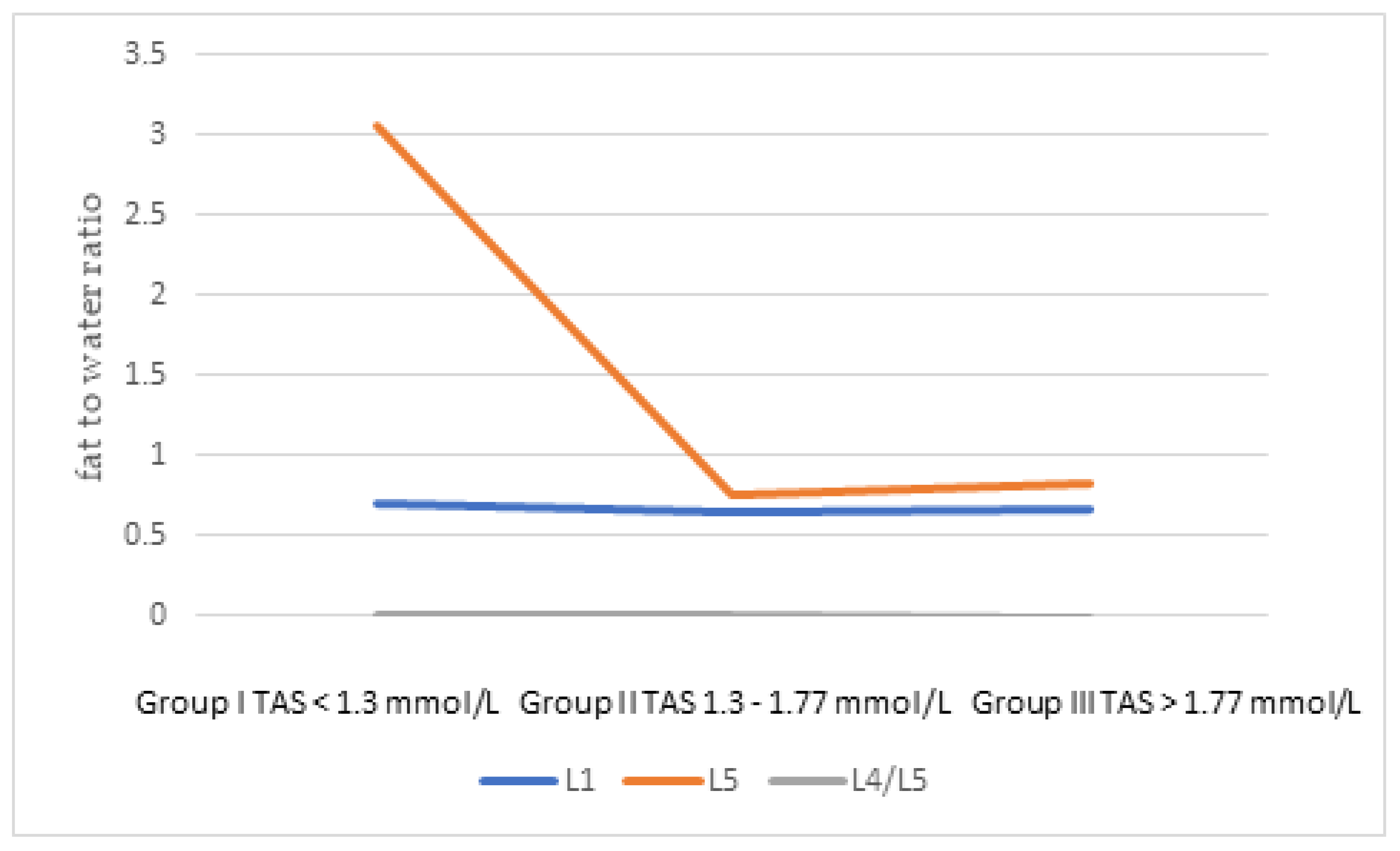
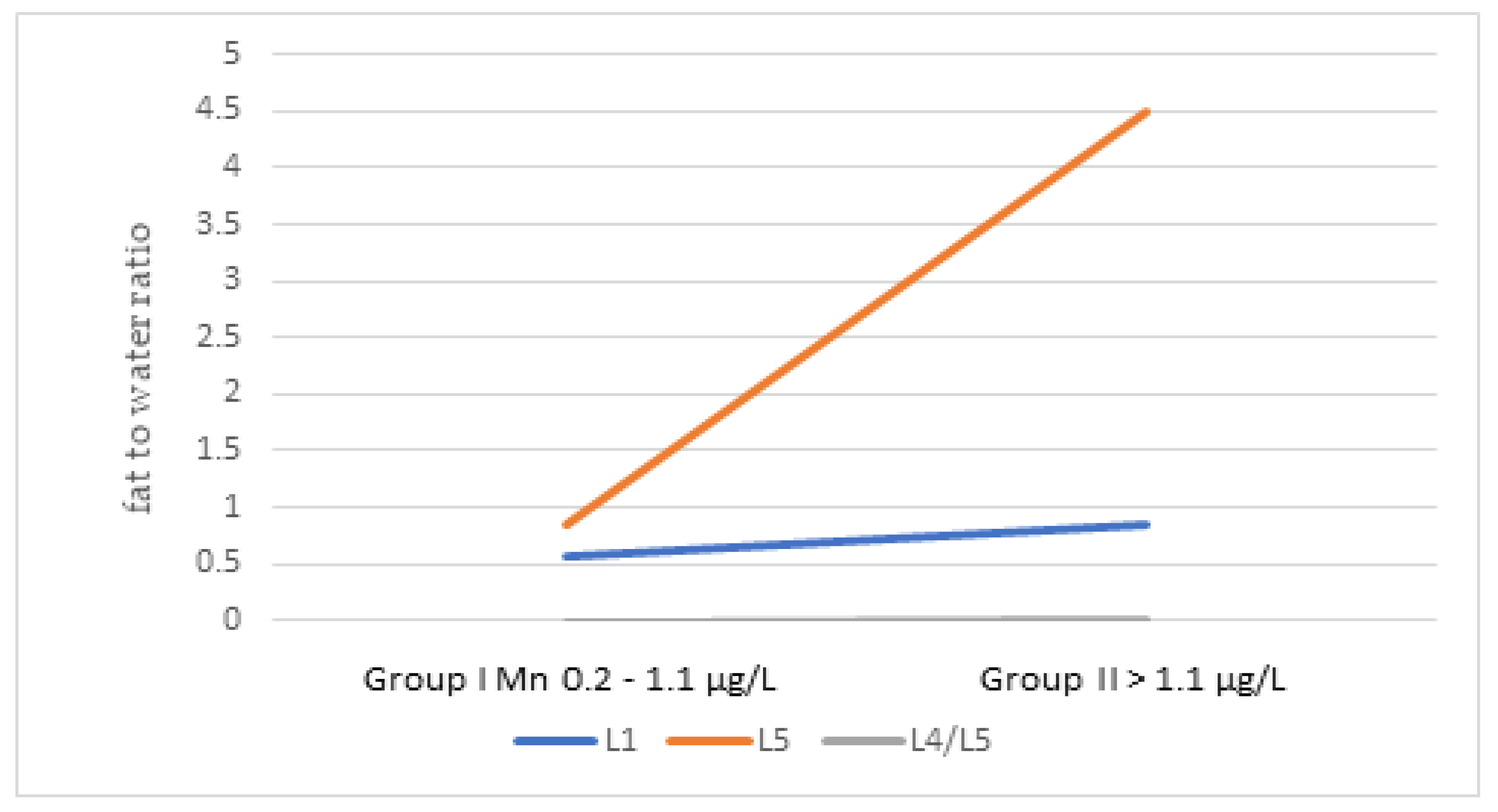
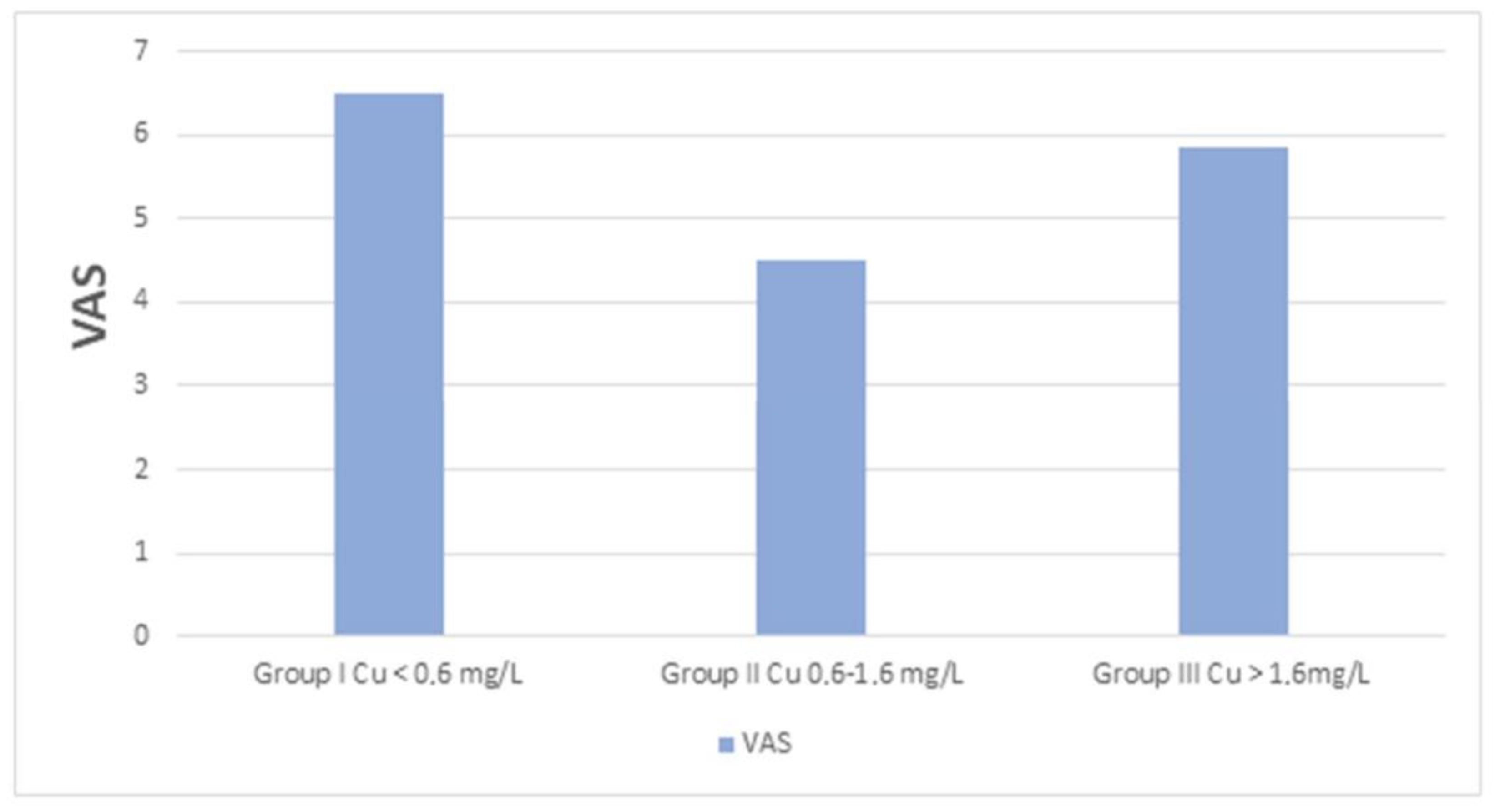
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ravindra, V.M.; Senglaub, S.S.; Rattani, A.; Dewan, M.C.; Härtl, R.; Bisson, E.; Park, K.B.; Shrime, M.G. Degenerative lumbar spine disease: Estimating global incidence and worldwide volume. Glob. Spine J. 2018, 8, 784–794. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman-Górska, I. Reumatologia Kliniczna; Wydawnictwo Lekarskie PZWL: Warsaw, Poland, 2008; pp. 995–1006. [Google Scholar]
- Menezes-Reis, R.; Bonugli, G.P.; Dalto, V.F.; da Silva Herrero, C.F.P.; Defino, H.L.A.; Nogueira-Barbosa, M.H. Association between lumbar spine sagittal alignment and L4-L5 disc degeneration among asymptomatic young adults. Spine 2016, 41, 1081–1087. [Google Scholar] [CrossRef] [PubMed]
- Cheung, K.M.; Karppinen, J.; Chan, D.; Ho, D.W.; Song, Y.Q.; Sham, P.; Cheah, K.S.; Leong, J.C.; Luk, K.D. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine 2009, 34, 934–940. [Google Scholar] [CrossRef] [PubMed]
- Sarzi-Puttini, P.; Atzeni, F.; Fumagalli, M.; Capsoni, F.; Carrabba, M. Osteoarthritis of the spine. Semin. Arthritis Rheum. 2005, 34 (Suppl. 2), 38–43. [Google Scholar] [CrossRef]
- Wróblewska, I.; Bieszcz-Płostkonka, K.; Błaszczuk, J.; Kurpas, D. Efektywność rehabilitacji w chorobach zwyrodnieniowych kręgosłupa. Fam. Med. Prim. Care Rev. 2014, 16, 35–38. (In Polish) [Google Scholar]
- Goode, A.P.; Carey, T.S.; Jordan, J.M. Low back pain and lumbar spine osteoarthritis: How are they related? Curr. Rheumatol. Rep. 2013, 15, 305. [Google Scholar] [CrossRef]
- Gellhorn, A.C.; Katz, J.N.; Suri, P. Osteoarthritis of the spine: The facet joints. Nat. Rev. Rheumatol. 2013, 9, 216–224. [Google Scholar] [CrossRef]
- Suzuki, S.; Fujita, N.; Hosogane, N.; Watanabe, K.; Ishii, K.; Toyama, Y.; Takubo, K.; Horiuchi, K.; Miyamoto, T.; Nakamura, M.; et al. Excessive reactive oxygen species are therapeutic targets for intervertebral disc degeneration. Arthritis Res. Ther. 2015, 17, 316. [Google Scholar] [CrossRef]
- Valavanidis, A.; Vlachogianni, T.; Fiotakis, K. Tobacco smoke: Involvement of reactive oxygen species and stable free radicals in mechanisms of oxidative damage, carcinogenesis and synergistic effects with other respirable particles. Int. J. Environ. Res. Public Health 2009, 6, 445–462. [Google Scholar] [CrossRef]
- Łapaj, Ł.; Markuszewski, J.; Wierusz-Kozłowska, M. Current views on the pathogenesis of osteoarthritis. Chir. Narzadow. Ruchu Ortop. Pol. 2010, 75, 248–260. (In Polish) [Google Scholar]
- Gapys, B.; Raszeja-Specht, A.; Bielarczyk, H. Rola cynku w procesach fizjologicznych i patologicznych organizmu. Diagn. Lab. 2014, 50, 45–52. (In Polish) [Google Scholar]
- Hefnawy, A.E.; El-Khaiat, A.M. The importance of cooper and the effects of its deficiency and toxicity in animal health. Int. J. Live Res. 2015, 5, 1–20. [Google Scholar] [CrossRef]
- Łabądź, D.; Skolarczyk, J.; Pekar, J.; Nieradko-Iwanicka, B. Analysis of the influence of selected elements on the functioning of the bone tissue. J. Educ. Health Sport 2017, 7, 202–209. [Google Scholar]
- Zofkova, I.; Davis, M.; Blahos, J. Trace elements have beneficial, as well as detrimental effects on bone homeostasis. Physiol. Res. 2017, 66, 391–402. [Google Scholar] [CrossRef]
- Kurz, B.; Schunke, J.M. Dietary vitamins and selenium diminish the development of mechanically induced osteoarthritis and increase the expression of antioxidative enzymes in the knee joint of STR/1N mice. Osteoarthr. Cartil. 2002, 10, 119–126. [Google Scholar] [CrossRef]
- Das, A.; Hammad, T.A. Efficacy of a combination of FCHG49 glucosamine hydrochloride, TRH122 low molecular weight sodium chondroitin sulfate and manganese ascorbate in the management of knee osteoarthritis. Osteoarthr. Cartil. 2000, 8, 343–350. [Google Scholar] [CrossRef]
- Mu, S.; Wang, J.; Gong, S. Application of medical imaging based on deep learning in the treatment of lumbar degenerative diseases and osteoporosis with bone cement screws. Comput. Math Methods Med. 2021, 11, 2638495. [Google Scholar] [CrossRef]
- Karcioglu, O.; Topacoglu, H.; Dikme, O.; Dikme, O. A systematic review of the pain scales in adults: Which to use? Am. J. Emerg. Med. 2018, 36, 707–714. [Google Scholar] [CrossRef]
- Yamaguchi, M. Role of zinc in bone formation and bone resorption. J. Trace Elem. Exp. Med. 1998, 11, 119–135. [Google Scholar] [CrossRef]
- Kubaszewski, Ł.; Zioła-Frankowska, A.; Gasik, Z.; Frankowski, M.; Dąbrowski, M.; Molisak, B.; Kaczmarczyk, J.; Gasik, R. Chemometric evaluation of concentrations of trace elements in intervertebral disc tissue in patient with degenerative disc disease. Ann. Agric. Environ. Med. 2017, 24, 610–617. [Google Scholar] [CrossRef]
- Mahmood, N.M.A. Relationship between serum levels of some tracelements, disease duration and severity in patients with knee osteoarthritis. Pharmacol. Pharm. 2015, 6, 489–495. [Google Scholar] [CrossRef]
- Grennan, D.M.; Knudson, J.M.; Dunckley, J.; MacKinnon, M.J.; Myers, D.B.; Palmer, D.G. Serum copper and zinc in rheumatoid arthritis and osteoarthritis. N. Z. Med. J. 1980, 23, 47–50. [Google Scholar]
- Yazar, M.; Sarban, S.; Kocyigit, A.; Isikan, U.E. Synovial fluid and plasma selenium, copper, zinc, and iron concentrations in patients with rheumatoid arthritis and osteoarthritis. Biol. Trace Elem. Res. 2005, 106, 123–132. [Google Scholar] [CrossRef]
- Madej, D.; Borowska, K.; Bylinowska, J.; Szybalska, A.; Pietruszka, B. Dietary intakes of iron and zinc assessed in a select group of the elderly: Are they adequate? Rocz. Panstw. Zakl. Hig. 2013, 64, 97–104. (In Polish) [Google Scholar]
- Migliore, L.; Coppedè, F. Environmental-induced oxidative stress in neurodegenerative disorders and aging. Mutat. Res. 2009, 674, 73–84. [Google Scholar] [CrossRef]
- Tian, W.; Lv, Y.; Liu, Y.; Xiao, B.; Han, X. The high prevalence of symptomatic degenerative lumbar osteoarthritis in Chinese adults: A population-based study. Spine 2014, 15, 1301–1310. [Google Scholar] [CrossRef]
- Su, C.A.; Kusin, D.J.; Li, S.Q.; Ahn, U.M.; Ahn, N.U. The association between body mass index and the prevalence severity, and frequency of low back pain: Data from the osteoarthritis initiative. Spine 2018, 43, 848–852. [Google Scholar] [CrossRef]
- Conforti, A.; Franco, L.; Menegale, G.; Milanino, R.; Piemonte, G.; Velo, G.P. Serum copper and ceruloplasmin levels in rheumatoid arthritis and degenerative joint disease and their pharmacological implications. Pharmacol. Res. Commun. 1983, 15, 859–867. [Google Scholar] [CrossRef]
- Chellan, P.; Sadler, P.J. The elements of life and medicines. Philos. Trans. A Math Phys. Eng. Sci. 2015, 373, 20140182. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, W.; Yao, Q. Copper-based biomaterials for bone and cartilage tissue engineering. J. Orthop. Translat. 2021, 29, 60–71. [Google Scholar] [CrossRef] [PubMed]
- Chaudhri, M.A.; Kemmler, W.; Harsch, I.; Watling, R.J. Plasma copper and bone mineral density in osteopenia: An indicator of bone mineral density in osteopenic females. Biol. Trace Elem. Res. 2009, 129, 94–98. [Google Scholar] [CrossRef]
- Amtage, F.; Birnbaum, D.; Reinhard, T.; Niesen, W.D.; Weiller, C.; Mader, I.; Meyer, P.T.; Rijntjes, M. Estrogen intake and copper depositions: Implications for Alzheimer’s disease? Case Rep. Neurol. 2014, 6, 181–187. [Google Scholar] [CrossRef]
- Satarug, S.; Nishijo, M.; Ujjin, P.; Moore, M.R. Chronic exposure to low-level cadmium induced zinc-copper dysregulation. J. Trace Elem. Med. Biol. 2018, 46, 32–38. [Google Scholar] [CrossRef]
- Lee, J.H. Micronutrient deficiency syndrome: Zinc, copper and selenium. Pediatr. Gastroenterol. Hepatol. Nutr. 2012, 15, 145–150. [Google Scholar] [CrossRef][Green Version]
- Guo, C.H.; Chen, P.C.; Yeh, M.S.; Hsiung, D.Y.; Wang, C.L. Cu/Zn ratios are associated with nutritional status, oxidative stress, inflammation, and immune abnormalities in patients on peritoneal dialysis. Clin. Biochem. 2011, 44, 275–280. [Google Scholar] [CrossRef]
- Giacconi, R.; Costarelli, L.; Piacenza, F.; Basso, A.; Rink, L.; Mariani, E.; Fulop, T.; Dedoussis, G.; Herbein, G.; Provinciali, M.; et al. Main biomarkers associated with age-related plasma zinc decrease and copper/zinc ratio in healthy elderly from ZincAge study. Eur. J. Nutr. 2017, 56, 2457–2466. [Google Scholar] [CrossRef]
- Malavolta, M.; Giacconi, R.; Piacenza, F.; Santarelli, L.; Cipriano, C.; Costarelli, L.; Tesei, S.; Pierpaoli, S.; Basso, A.; Galeazzi, R.; et al. Plasma copper/zinc ratio: An inflammatory/nutritional biomarker as predictor of all-cause mortality in elderly population. Biogerontology 2010, 11, 309–319. [Google Scholar] [CrossRef]
- Ghayour-Mobarhan, M.; Taylor, A.; New, S.A.; Lamb, D.J.; Ferns, G.A. Determinants of serum copper, zinc and selenium in healthy subjects. Ann. Clin. Biochem. 2005, 42 Pt 5, 364–375. [Google Scholar] [CrossRef]
- Fairweather-Tait, S.J.; Bao, Y.; Broadley, M.R.; Collings, R.; Ford, D.; Hesketh, J.E.; Hurst, R. Selenium in human health and disease. Antioxid. Redox Signal. 2011, 1, 1337–1383. [Google Scholar] [CrossRef]
- Wozniak, A.; Napierala, M.; Golasik, M.; Herman, M.; Walas, S.; Piekoszewski, W.; Szyfter, W.; Szyfter, K.; Golusinski, W.; Baralkiewicz, D.; et al. Metal concentrations in hair of patients with various head and neck cancers as a diagnostic aid. Biometals 2016, 29, 81–93. [Google Scholar] [CrossRef][Green Version]
- Aschner, M.; Erikson, K. Manganese. Adv. Nutr. 2017, 8, 520–521. [Google Scholar] [CrossRef]
- Lu, Z.F.; Doulabi, B.; Wuisman, P.I.; Bank, R.A.; Helder, M.N. Influence of collagen type II and nucleus pulposus cells on aggregation and differentiation of adipose tissue-derived stem cells. J. Cell Mol. Med. 2008, 12, 2812–2822. [Google Scholar] [CrossRef]
- Keen, C.L.; Zidenberg-Cherr, S. Manganese. In Present Knowledge in Nutrition, 7th ed.; Ziegler, E.E., Filer, L.J., Eds.; ILSI Press: Washington, DC, USA, 1996; pp. 334–343. [Google Scholar]
- Holley, A.K.; Bakthavatchalu, V.; Velez-Roman, J.M.; St Clair, D.K. Manganese superoxide dismutase: Guardian of the powerhouse. Int. J. Mol. Sci. 2011, 12, 7114–7162. [Google Scholar] [CrossRef]
- O’Neal, S.L.; Zheng, W. Manganese toxicity upon overexposure: A decade in review. Curr. Environ. Health Rep. 2015, 2, 315–328. [Google Scholar] [CrossRef]
- Oulhote, Y.; Mergler, D.; Bouchard, M.F. Sex- and age-differences in blood manganese levels in the U.S. general population: National health and nutrition examination survey 2011–2012. Environ. Health 2014, 13, 87. [Google Scholar] [CrossRef] [PubMed]
- Czajka, A. Wolne rodniki tlenowe a mechanizmy obronne organizmu. Now. Lek. 2006, 75, 582–586. (In Polish) [Google Scholar]
- Andriollo-Sanchez, M.; Hininger-Favier, I.; Meunier, N.; Venneria, E.; O’Connor, J.M.; Maiani, G.; Coudray, C.; Roussel, A.M. Age-related oxidative stress and antioxidant parameters in middle-aged and older European subjects: The ZENITH study. Eur. J. Clin. Nutr. 2005, 59, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Hübner-Woźniak, E.; Okecka-Szymańska, J.; Stupnicki, R.; Malara, M.; Kozdroń, E. Age-related blood antioxidant capacity in men and women. J. Med. Biochem. 2011, 30, 103–108. [Google Scholar] [CrossRef]
| Examined Group n = 90 | Control Group n = 40 | |||
|---|---|---|---|---|
| Age (years) mean ± SD (range) | 48.2 ± 12.7 (21–73) | 45.8 ± 16.0 (21–83) | ||
| Gender | Female 58% | Male 42% | Female 70% | Male 30% |
| BMI (kg/m2) mean ± SD (range) | 28.1 ± 4.1 (20.1–38.3) | 26.2 ± 3.8 (20.7–35.2) | ||
| Smoking cigarettes | Yes 31% | No 69% | Yes 25% | No 75% |
| Examined Group Mean ± SD Min–Max Median (Q1–Q3) | Control Group Mean ± SD Min–Max Median (Q1–Q3) | p Value | |||
|---|---|---|---|---|---|
| Total | Total | ||||
| Zinc (mg/L) | 0.77 ± 0.22 (0.41–2.1) 0.76 (0.64–0.85) | 0.83 ± 0.13 (0.55–1.09) 0.81 (0.74–0.91) | 0.001 * | ||
| F (a) | M (b) | F (c) | M (d) | ||
| 0.74 ± 0.15 | 0.80 ± 0.28 | 0.83 ± 0.13 | 0.85 ± 0.14 | ns | |
| (0.41–1.08) 0.76 (0.64–0.83) | (0.50–2.10) 0.75 (0.63–0.86) | (0.55–1.09) 0.81 (0.74–0.99) | (0.67–1.07) 0.81 (0.74–0.91) | ||
| Smokers (a) | Non-smokers (b) | Smokers (c) | Non-smokers (d) | ||
| 0.81 ± 0.39 (0.41–2.1) 0.74 (0.67–0.88) | 0.75 ± 0.12 (0.53–0.98) 0.77 (0.66–0.83) | 0.87 ± 0.22 (0.55–1.09) 0.92 (0.67–1.07) | 0.79 ± 0.09 (0.56–0.99) 0.79 (0.75–0.86) | ns | |
| Copper (mg/L) | 1.1 ± 0.35 (0.53–2.3) (0.99) (0.88–1.2) | 1.25 ± 0.41 (0.81–2.36) 1.16 (0.92–1.49) | 0.04 * | ||
| F (a) | M (b) | F (c) | M (d) | ||
| 1.21 ± 0.37 (0.75–2.3) 1.13 (0.96–1.33) | 0.94 ± 0.26 (0.53–2) 0.88 (0.81–0.99 | 1.22± 0.39 (0.76–2.3) 1.1 (0.9–1.49) | 1.2 ± 0.48 (0.7–2.36) 1.1 (0.86–1.4) | a vs. b < 0.00001 * | |
| Smokers (a) | Non-smokers (b) | Smokers (c) | Non-smokers (d) | ||
| 1.07 ± 0,35 (0.67–2.03) 0.97 (0.88–1.15) | 1.17 ± 0.34 (0.76–2.22) 1.11 (0.9–1.2) | (1.2 ± 0.39) (0.86–1.78) 1.15 (0.86–1.49) | 1.16 ± 0.39 (0.7–2.31) 1.07 (0.86–1.29) | a vs. b < 0.05 * | |
| Cu/Zn ratio | 1.54± 0.5 (0.35–2.98) 1.48 (1.15–1.81) | 1.56± 0.65 (0.80–3.44) 1.4 (1.12–1.84) | ns | ||
| F (a) | M (b) | F (c) | M (d) | ||
| 1.73 ± 0.5 (0.85–2.98) 1.63 (1.37–2.05) | 1.29 ± 0.39 (0.35–2.17) 1.26 (1.05–1.48) | 1.57 ± 0.61 (0.82–3.32) 1.44 (1.15–1.87) | 1.54 ± 0.76 (0.8–3.49) 1.35 (1.08–1.57) | a vs. b = 0.00006 * | |
| Smokers (a) | Non-smokers (b) | Smokers (c) | Non-smokers (d) | ||
| 1.49 ± 0.58 (0.35–2.78) 1.4 (1.11–1.72) | 1.61 ± 0.45 (0.94–2.98) 1.49 (1.31–1.88) | 1.61 ± 0.96 (0.81–1.32) 1.23 (0.98–2.12) | 1.52 ± 0.55 (0.8–3.11) 1.4 (1.15–1.81) | ns | |
| Selenium (μg/L) | 77.3 ± 21.5 (36.9–189.1) 74.8 (66.3–86.1) | 78.3 ± 14.5 (50.9–112.8) 75.8 (69.8–85.2) | ns | ||
| F (a) | M (b) | F (c) | M (d) | ||
| 78.6 ± 22.7 (48–189.1) 74.6 (66.9–86.1) | (75.4 ± 19.8 (36.9–133.7) 77.6 (64.3–86.4) | 78.1 ± 14 (59.8–112.8) 75.2 (69.7–84.2) | 78.6 ± 16.7 (50.9–106.8) 76.7 (70.5–89.1) | ||
| Smokers (a) | Non-smokers (b) | Smokers (c) | Non-smokers (d) | ||
| 72.6 ± 16.1 (36.9–103.7) 74.1 (60.4–84) | 73.6 ± 15.1 (42.6–104.6) 73.6 (66.5–82.4) | 76.8 ± 9.1 (70.5–94.9) 73.9 (71.2–76.1) | 76.7 ± 12.9 (59.8–112.6) 76 (68.2–83.6) | ||
| Manganese (mg/L) | 1.25 ± 1.28 (0.23–9.76) 1.06 (0.79–1.32) | 1.7 ± 1.98 (0.27–7.91) 0.81 (0.67–1.72) | ns | ||
| F (a) | M (b) | F (c) | M (d) | ||
| 1.19 ± 1.13 (0.22–8.24) 1.06 (0.76–1.28) | 1.34 ± 1.48 (0.36–9.76) 1.04 (0.82–1.36) | 1.35 ± 1.39 (0.27–5.4) 0.77 (0.64–1.03) | 2.43 ± 2.82 (0.58–7.9) 0.94 (0.75–2.1) | ||
| Smokers (a) | Non-smokers (b) | Smokers (c) | Non-smokers (d) | ||
| 1.43 ± 1.44 (0.51–8.24) 1.21 (0.92–1.38) | 1.4 ± 1.51 (0.53–9.76) 1.1 (0.88–1.34) | 1.99 ± 2.64 (0.59–6.71) 0.94 (0.74–1.03) | 1.97 ± 2.21 (0.49–7.91) 0.81 (0.66–2.91) | ||
| Total antioxidant status (mmol/L) | 1.03 ± 0,41 (0.1–2.14) 1.01 (0.71–1.28) | 1.39 ± 0.84 (0.71–3.5) 0.97 (0.88–1.58) | ns | ||
| F (a) | M (b) | F (c) | M (d) | ||
| 0.92± 0.35 (0.1–1.74) 0.97 (0.59–1.17) | 1.18 ± 0.43 (0.62–2.14) 1.12 (0.75–1.4) | 1.1 ± 0.76 (0.51–3.5) 0.82 (0.63–1.04) | 1.45 ± 0.93 (0.87–3.46 1.06 (0.93–1.636) | a vs. b < 0.01 * c vs. d < 0.05 * | |
| Smokers (a) | Non-smokers (b) | Smokers (c) | Non-smokers (d) | ||
| 0.99 ± 0.38 (0.31–1.78) 0.98 (0.71–1.29) | 1.15 ± 0.41 (0.49–2.14) 1.157 (0.86–1.31) | 0.79 ± 0.14 (0.6–0.93) 0.82 (0.7–0.9) | 1.35 ± 1 (0.51–3.5) 0.3 (0.63–1.85) | ns | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jakoniuk, M.; Biegaj, M.; Kochanowicz, J.; Łysoń, T.; Lankau, A.; Wilkiel, M.; Socha, K. Relationship between Selected Micronutrient Concentrations, Total Antioxidant Status, Pain Severity, and the Image of 1H MR Spectroscopy in Degenerative Spine Disease: A Case-Control Study. J. Clin. Med. 2022, 11, 5586. https://doi.org/10.3390/jcm11195586
Jakoniuk M, Biegaj M, Kochanowicz J, Łysoń T, Lankau A, Wilkiel M, Socha K. Relationship between Selected Micronutrient Concentrations, Total Antioxidant Status, Pain Severity, and the Image of 1H MR Spectroscopy in Degenerative Spine Disease: A Case-Control Study. Journal of Clinical Medicine. 2022; 11(19):5586. https://doi.org/10.3390/jcm11195586
Chicago/Turabian StyleJakoniuk, Marta, Magdalena Biegaj, Jan Kochanowicz, Tomasz Łysoń, Agnieszka Lankau, Marianna Wilkiel, and Katarzyna Socha. 2022. "Relationship between Selected Micronutrient Concentrations, Total Antioxidant Status, Pain Severity, and the Image of 1H MR Spectroscopy in Degenerative Spine Disease: A Case-Control Study" Journal of Clinical Medicine 11, no. 19: 5586. https://doi.org/10.3390/jcm11195586
APA StyleJakoniuk, M., Biegaj, M., Kochanowicz, J., Łysoń, T., Lankau, A., Wilkiel, M., & Socha, K. (2022). Relationship between Selected Micronutrient Concentrations, Total Antioxidant Status, Pain Severity, and the Image of 1H MR Spectroscopy in Degenerative Spine Disease: A Case-Control Study. Journal of Clinical Medicine, 11(19), 5586. https://doi.org/10.3390/jcm11195586







