The Emborrhoid Technique for Treatment of Bleeding Hemorrhoids in Patients with High Surgical Risk †
Abstract
:1. Background
2. Materials and Methods
2.1. Study Design and Study Population
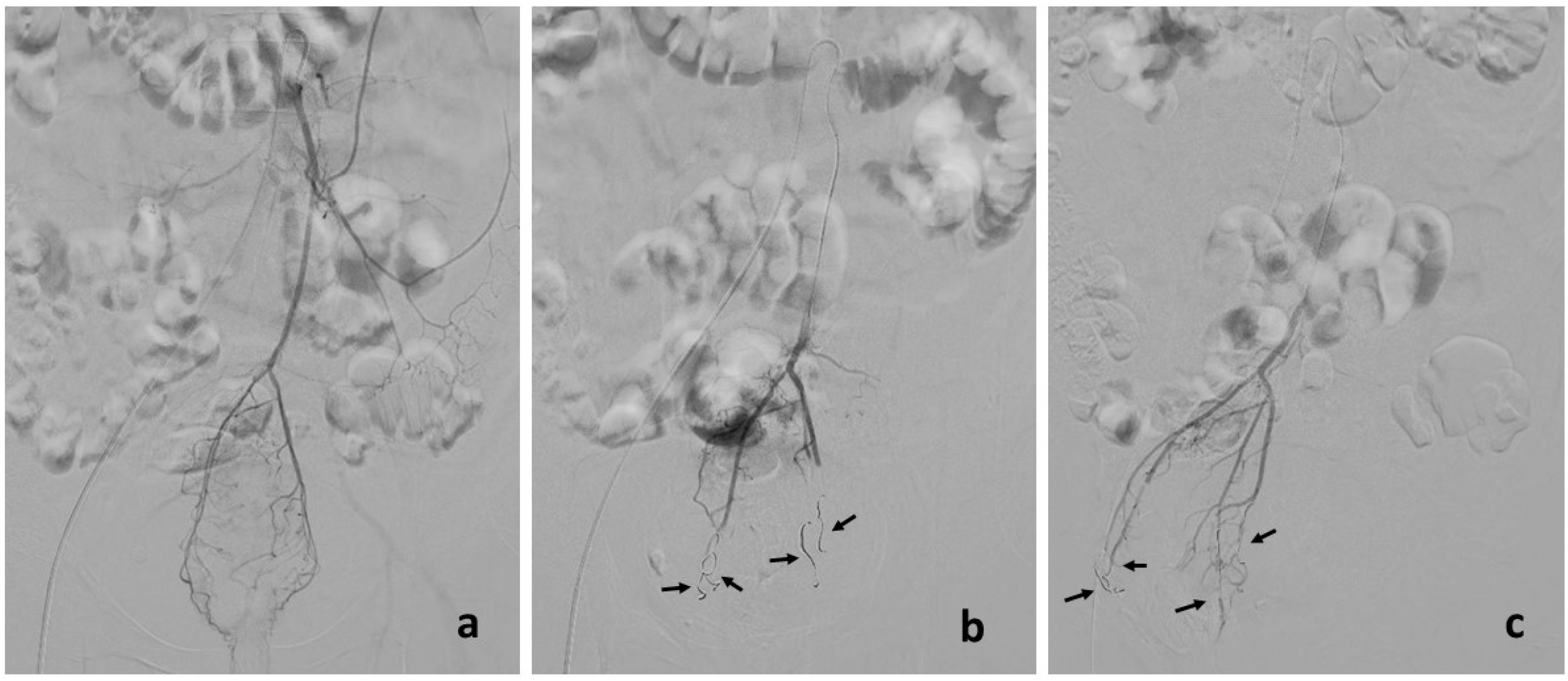
2.2. Treatment
2.3. Endpoints and Definitions
2.4. Statistical Analysis
3. Results
3.1. Patients Characteristics
3.2. Operative and Perioperative Data
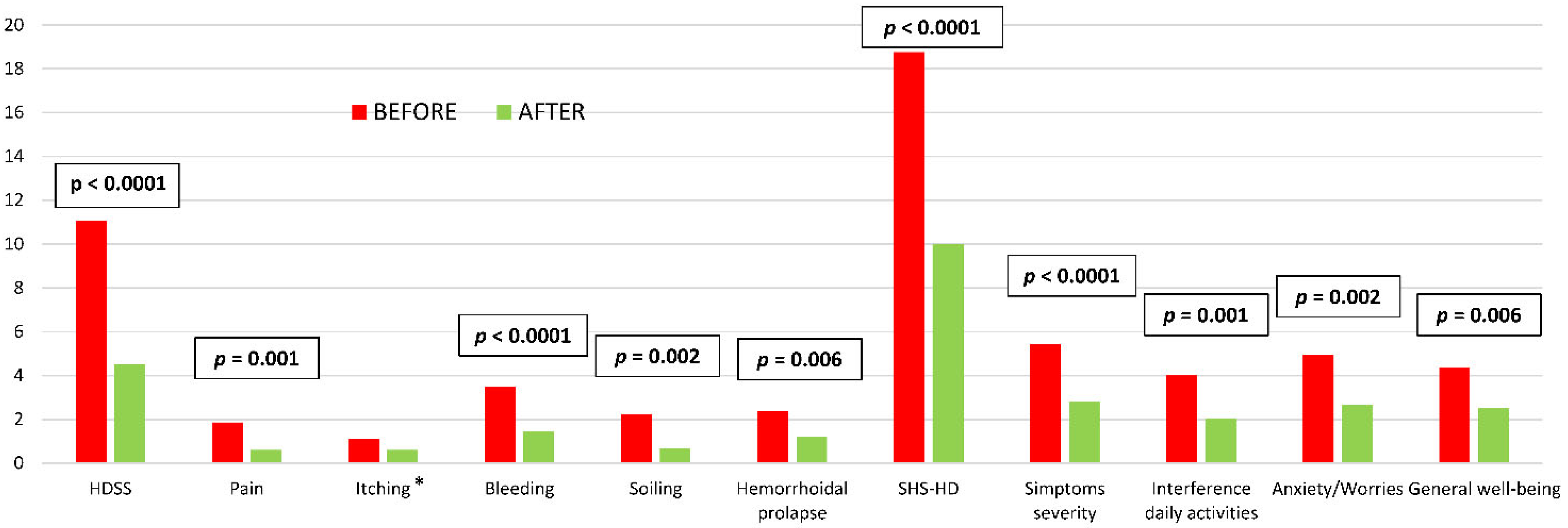
3.3. Middle- and Long-Term Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Perera, N.; Liolitsa, D.; Iype, S.; Croxford, A.; Yassin, M.; Lang, P.; Ukaegbu, O.; van Issum, C. Phlebotonics for haemorrhoids. Cochrane Database Syst. Rev. 2012, 8, CD004322. [Google Scholar] [CrossRef] [PubMed]
- Cengiz, T.B.; Gorgun, E. Hemorrhoids: A range of treatments. Clevel. Clin. J. Med. 2019, 86, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Gallo, G.; Martellucci, J.; Sturiale, A.E.; Clerico, G.; Milito, G.; Marino, F.; Cocorullo, G.; Giordano, P.; Mistrangelo, M.; Trompetto, M. Consensus statement of the Italian society of colorectal surgery (SICCR): Management and treatment of hemorrhoidal disease. Tech. Coloproctol. 2020, 24, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Ratto, C.; Donisi, L.; Parello, A.; Litta, F.; Zaccone, G.; De Simone, V. ‘Distal Doppler-guided dearterialization’ is highly effective in treating haemorrhoids by transanal haemorrhoidal dearterialization. Colorectal Dis. 2012, 14, e786–e789. [Google Scholar] [CrossRef] [PubMed]
- Parello, A.; Litta, F.; De Simone, V.; Campennì, P.; Orefice, R.; Marra, A.A.; Goglia, M.; Santoro, L.; Santoliquido, A.; Ratto, C. Haemorrhoidal haemodynamic changes in patients with haemorrhoids treated using Doppler-guided dearterialization. BJS Open 2021, 5, zrab012. [Google Scholar] [CrossRef]
- Pucher, P.H.; Sodergren, M.H.; Lord, A.C.; Darzi, A.; Ziprin, P. Clinical outcome following Doppler-guided haemorrhoidal artery ligation: A systematic review. Colorectal Dis. 2013, 15, e284–e294. [Google Scholar] [CrossRef]
- Ratto, C.; Campennì, P.; Papeo, F.; Donisi, L.; Litta, F.; Parello, A. Transanal hemorrhoidal dearterialization (THD) for hemorrhoidal disease: A single-center study on 1000 consecutive cases and a review of the literature. Tech. Coloproctol. 2017, 21, 953–962. [Google Scholar] [CrossRef]
- Vidal, V.; Louis, G.; Bartoli, J.; Sielezneff, I. Embolization of the hemorrhoidal arteries (the emborrhoid technique): A new concept and challenge for interventional radiology. Diagn. Interv. Imaging 2014, 95, 307–315. [Google Scholar] [CrossRef]
- Talaie, R.; Torkian, P.; Moghadam, A.D.; Tradi, F.; Vidal, V.; Sapoval, M.; Golzarian, J. Hemorrhoid embolization: A review of current evidences. Diagn. Interv. Imaging. 2022, 103, 3–11. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- Iezzi, R.; Campenni, P.; Posa, A.; Parello, A.; Rodolfino, E.; Marra, A.A.; Ratto, C.; Manfredi, R. Outpatient Transradial Emborrhoid Technique: A Pilot Study. Cardiovasc. Interv. Radiol. 2021, 44, 1300–1306. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services; National Institutes of Health; National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) Version 5. 2017. Available online: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf (accessed on 16 March 2022).
- Rørvik, H.D.; Styr, K.; Ilum, L.; McKinstry, G.L.; Dragesund, T.; Campos, A.H.; Brandstrup, B.; Olaison, G. Hemorrhoidal Disease Symptom Score and Short Health ScaleHD: New Tools to Evaluate Symptoms and Health-Related Quality of Life in Hemorrhoidal Disease. Dis. Colon Rectum 2019, 62, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Simillis, C.; Thoukididou, S.N.; Slesser, A.A.P.; Rasheed, S.; Tan, E.; Tekkis, P.P. Systematic review and network meta-analysis comparing clinical outcomes and effectiveness of surgical treatments for haemorrhoids. J. Br. Surg. 2015, 102, 1603–1618. [Google Scholar] [CrossRef] [PubMed]
- Vidal, V.; Sapoval, M.; Sielezneff, Y.; De Parades, V.; Tradi, F.; Louis, G.; Bartoli, J.M.; Pellerin, O. Emborrhoid: A new concept for the treatment of hemorrhoids with arterial embolization: The first 14 cases. Cardiovasc. Interv. Radiol. 2015, 38, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Eberspacher, C.; Ficuccilli, F.; Tessieri, L.; D’Andrea, V.; Lauro, A.; Fralleone, L.; Mascagni, D. Annoyed with Haemorrhoids? Risks of the Emborrhoid Technique. Am. J. Dig. Dis. 2021, 66, 3725–3729. [Google Scholar] [CrossRef]
- Zakharchenko, A.; Kaitoukov, Y.; Vinnik, Y.; Tradi, F.; Sapoval, M.; Sielezneff, I.; Galkin, E.; Vidal, V. Safety and efficacy of superior rectal artery embolization with particles and metallic coils for the treatment of hemorrhoids (Emborrhoid technique). Diagn. Interv. Imaging 2016, 97, 1079–1084. [Google Scholar] [CrossRef]
- Sun, X.; Xu, J.; Zhang, J.; Jin, Y.; Chen, Q. Management of rectal bleeding due to internal haemorrhoids with arterial embolisation: A single-centre experience and protocol. Clin. Radiol. 2018, 73, 985.e1–985.e6. [Google Scholar] [CrossRef]
- Moggia, E.; Talamo, G.; Gallo, G.; Bianco, A.; Barattini, M.; Salsano, G. Do We Have Another Option to Treat Bleeding Hemorrhoids? The Emborrhoid Technique: Experience in 16 Patients. Rev. Recent Clin. Trials. 2021, 16, 81–86. [Google Scholar]
- Han, X.; Xia, F.; Chen, G.; Sheng, Y.; Wang, W.; Wang, Z.; Zhao, M.; Wang, X. Superior rectal artery embolization for bleeding internal hemorrhoids. Tech. Coloproctol. 2020, 25, 75–80. [Google Scholar] [CrossRef]
- Tradi, F.; Mege, D.; Louis, G.; Bartoli, J.M.; Sielezneff, I.; Vidal, V. Emborrhoïd: Traitement des hémorroïdes par embolisation des artères rectales [Emborrhoid: Rectal arteries embolization for hemorrhoid treatment]. Presse Med. 2019, 48, 454–459. [Google Scholar] [CrossRef]
- Moussa, N.; Sielezneff, I.; Sapoval, M.; Tradi, F.; Del Giudice, C.; Fathallah, N.; Pellerin, O.; Amouyal, G.; Pereira, H.; De Parades, V.; et al. Embolization of the superior rectal arteries for chronic bleeding due to haemorrhoidal disease. Colorectal Dis. 2017, 19, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Venturini, M.; De Nardi, P.; Marra, P.; Panzeri, M.; Brembilla, G.; Morelli, F. Embolization of superior rectal arteries for transfusion dependent haemorrhoidal bleeding in severely cardiopathic patients: A new field of application of the “emborrhoid” technique. Tech. Coloproctol. 2018, 22, 453–455. [Google Scholar] [CrossRef] [PubMed]
- Giurazza, F.; Corvino, F.; Cavaglià, E.; Silvestre, M.; Cangiano, G.; Amodio, F. Emborrhoid in patients with portal hypertension and chronic hemorrhoidal bleeding: Preliminary results in five cases with a new coiling release fashion “Spaghetti technique”. Radiol. Med. 2020, 125, 1008–1011. [Google Scholar] [CrossRef] [PubMed]
- Alves e Sousa, F.; Lopes, P.M.; Mónica, I.B.; Carvalho, A.C.; Sousa, P. Emborrhoid technique performed on a patient with portal hypertension and chronic hemorrhoidal bleeding as a salvage therapy. CVIR Endovasc. 2022, 5, 1–4. [Google Scholar] [CrossRef]
| n(%) | |
| Patients | 21 |
| Ratio M:F | 16:5 |
| Age (years) * | 72.2 (10.9) |
| Comorbidities | |
| Cardiovascular | 18 (85.7) |
| Respiratory | 6 (28.6) |
| Hematological/immunological | 2 (9.5) |
| Mild chronic kidney failure | 5 (23.8) |
| Obesity/dyslipidemia | 17 (81.0) |
| Paraplegia | 1 (4.8) |
| History of smoking/smoker | 10 (47.6) |
| Antiplatelet therapy | 6 (28.6) |
| Anticoagulant therapy | 9 (42.9) |
| Antiplatelet + anticoagulant therapy | 1 (4.8) |
| Previous hemorrhoidal surgery | 6 (28.6) |
| Goligher’s classification | |
| Grade II | 8 (38.1) |
| Grade III | 10 (47.6) |
| Grade IV | 3 (14.3) |
| Flavonoids before embolization | 17 (81.0) |
| Iron therapy before embolization | 10 (47.6) |
| Blood transfusion before embolization | 11 (52.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campennì, P.; Iezzi, R.; Marra, A.A.; Posa, A.; Parello, A.; Litta, F.; De Simone, V.; Ratto, C. The Emborrhoid Technique for Treatment of Bleeding Hemorrhoids in Patients with High Surgical Risk. J. Clin. Med. 2022, 11, 5533. https://doi.org/10.3390/jcm11195533
Campennì P, Iezzi R, Marra AA, Posa A, Parello A, Litta F, De Simone V, Ratto C. The Emborrhoid Technique for Treatment of Bleeding Hemorrhoids in Patients with High Surgical Risk. Journal of Clinical Medicine. 2022; 11(19):5533. https://doi.org/10.3390/jcm11195533
Chicago/Turabian StyleCampennì, Paola, Roberto Iezzi, Angelo Alessandro Marra, Alessandro Posa, Angelo Parello, Francesco Litta, Veronica De Simone, and Carlo Ratto. 2022. "The Emborrhoid Technique for Treatment of Bleeding Hemorrhoids in Patients with High Surgical Risk" Journal of Clinical Medicine 11, no. 19: 5533. https://doi.org/10.3390/jcm11195533
APA StyleCampennì, P., Iezzi, R., Marra, A. A., Posa, A., Parello, A., Litta, F., De Simone, V., & Ratto, C. (2022). The Emborrhoid Technique for Treatment of Bleeding Hemorrhoids in Patients with High Surgical Risk. Journal of Clinical Medicine, 11(19), 5533. https://doi.org/10.3390/jcm11195533







