Intravenous Magnesium Sulfate Reduces the Need for Antiarrhythmics during Acute-Onset Atrial Fibrillation in Emergency and Critical Care
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
6. Limitations
7. Ethical Statement
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Zwillinger, L. Über die Magnesiumwirkung auf das Herz. Klin. Wochenschr. 1935, 14, 1429–1433. [Google Scholar] [CrossRef]
- Enselberg, C.D.; Simmons, H.G.; Mintz, A.A. The effects of magnesium upon cardiac arrhythmias. Am. Heart J. 1950, 39, 703–712. [Google Scholar] [CrossRef]
- Szekely, P. The Action of Magnesium on the Heart. Br. Heart J. 1946, 8, 115–124. [Google Scholar] [CrossRef][Green Version]
- Boyd, J.C.; Bruns, D.E.; Wills, M.R. Frequency of hypomagnesemia in hypokalemic states. Clin. Chem. 1983, 29, 178–179. [Google Scholar] [CrossRef] [PubMed]
- Tzivoni, D.; Keren, A.; Cohen, A.M.; Loebel, H.; Zahavi, I.; Chenzbraun, A.; Stern, S. Magnesium therapy for torsades de pointes. Am. J. Cardiol. 1984, 53, 528–530. [Google Scholar] [CrossRef]
- Gröber, U.; Schmidt, J.; Kisters, K. Magnesium in Prevention and Therapy. Nutrients 2015, 7, 8199–8226. [Google Scholar] [CrossRef] [PubMed]
- Gilardi, E.; Marsiliani, D.; Nicolo, R.; Petrucci, M.; Torelli, E.; Racco, S.; Di Maurizio, L.; Saviano, L.; Biscione, G.; Giannuzzi, R.; et al. Magnesium sulphate in the Emergency Department: An old, new friend. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 4052–4063. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.M.; Lubitz, S.A.; Sullivan, L.M.; Sun, J.X.; Levy, D.; Vasan, R.S.; Magnani, J.W.; Ellinor, P.T.; Benjamin, E.J.; Wang, T.J. Low Serum Magnesium and the Development of Atrial Fibrillation in the Community. Circulation 2013, 127, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Markovits, N.; Kurnik, D.; Halkin, H.; Margalit, R.; Bialik, M.; Lomnicky, Y.; Loebstein, R. Database evaluation of the association between serum magnesium levels and the risk of atrial fibrillation in the community. Int. J. Cardiol. 2016, 205, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Wang, A. Efficacy of class III antiarrhythmics and magnesium combination therapy for atrial fibrillation. Pharm. Pract. 2012, 10, 65–71. [Google Scholar] [CrossRef]
- Ho, K.M.; Sheridan, D.J.; Paterson, T. Use of intravenous magnesium to treat acute onset atrial fibrillation: A meta-analysis. Heart 2007, 93, 1433–1440. [Google Scholar] [CrossRef] [PubMed]
- Davey, M.J.; Teubner, D. A Randomized Controlled Trial of Magnesium Sulfate, in Addition to Usual Care, for Rate Control in Atrial Fibrillation. Ann. Emerg. Med. 2005, 45, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Rajagopalan, B.; Shah, Z.; Narasimha, D.; Bhatia, A.; Kim, C.H.; Switzer, D.F.; Gudleski, G.H.; Curtis, A.B. Efficacy of Intravenous Magnesium in Facilitating Cardioversion of Atrial Fibrillation. Circ. Arrhythmia Electrophysiol. 2016, 9, e003968. [Google Scholar] [CrossRef] [PubMed]
- Sultan, A.; Steven, D.; Rostock, T.; Hoffmann, B.; Müllerleile, K.; Servatius, H.; Drewitz, I.; Lüker, J.; Meyer, P.; Salukhe, T.; et al. Intravenous administration of magnesium and potassium solution lowers energy levels and increases success rates electrically cardioverting atrial fibrillation. J. Cardiovasc. Electrophysiol. 2012, 23, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Markey, G.C.; Salter, N.; Ryan, J. Intravenous Flecainide for Emergency Department Management of Acute Atrial Fibrillation. J. Emerg. Med. 2018, 54, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.H.; Apostolakis, S. Atrial fibrillation (acute onset). BMJ Clin. Evid. 2014, 2014, 0210. [Google Scholar] [PubMed]
- Alp, N.J.; Bell, J.A.; Shahi, M. Randomised double blind trial of oral versus intravenous flecainide for the cardioversion of acute atrial fibrillation. Heart 2000, 84, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Pohjantähti-Maaroos, H.; Hyppölä, H.; Lekkala, M.; Sinisalo, E.; Heikkola, A.; Hartikainen, J. Intravenous vernakalant in comparison with intravenous flecainide in the cardioversion of recent-onset atrial fibrillation. Eur. Heart J. Acute Cardiovasc. Care 2019, 8, 114–120. [Google Scholar] [CrossRef]
- Donovan, K.D.; Power, B.M.; Hockings, B.E.; Dobb, G.J.; Lee, K.Y. Intravenous flecainide versus amiodarone for recent-onset atrial fibrillation. Am. J. Cardiol. 1995, 75, 693–697. [Google Scholar] [CrossRef]
- Reisinger, J.; Gatterer, E.; Lang, W.; Vanicek, T.; Eisserer, G.; Bachleitner, T.; Niemeth, C.; Aicher, F.; Grander, W.; Heinze, G.; et al. Flecainide versus ibutilide for immediate cardioversion of atrial fibrillation of recent onset. Eur. Heart J. 2004, 25, 1318–1324. [Google Scholar] [CrossRef] [PubMed]
- Kriz, R.; Freynhofer, M.K.; Weiss, T.W.; Egger, F.; Gruber, S.C.; Eisenburger, P.; Wojta, J.; Huber, K.; Koch, J. Safety and efficacy of pharmacological cardioversion of recent-onset atrial fibrillation: A single-center experience. Am. J. Emerg. Med. 2016, 34, 1486–1490. [Google Scholar] [CrossRef]
- Romano, S.; Fattore, L.; Toscano, G.; Corsini, F.; Coppo, A.; Catanzaro, M.; Romano, A.; Martone, A.; Caccavale, F.; Iodice, E.; et al. Effectiveness and side effects of the treatment with propafenone and flecainide for recent-onset atrial fibrillation. Ital. Heart J. Suppl. 2001, 2, 41–45. [Google Scholar] [PubMed]
- Martínez-Marcos, F.J.; García-Garmendia, J.L.; Ortega-Carpio, A.; Fernández-Gómez, J.M.; Santos, J.M.; Camacho, C. Comparison of intravenous flecainide, propafenone, and amiodarone for conversion of acute atrial fibrillation to sinus rhythm. Am. J. Cardiol. 2000, 86, 950–953. [Google Scholar] [CrossRef]
- Capucci, A.; Lenzi, T.; Boriani, G.; Trisolino, G.; Binetti, N.; Cavazza, M.; Fontana, G.; Magnani, B. Effectiveness of loading oral flecainide for converting recent-onset atrial fibrillation to sinus rhythm in patients without organic heart disease or with only systemic hypertension. Am. J. Cardiol. 1992, 70, 69–72. [Google Scholar] [CrossRef]
- Marsiliani, D.; Buccelletti, F.; Carroccia, A.; Gilardi, E.; Silveri, N.G.; Franceschi, F. Natriuretic peptides and atrial fibrillation. Eur. Rev. Med. Pharmacol. Sci. 2010, 14, 855–860. [Google Scholar]
- Savioli, G.; Ceresa, I.F.; Gri, N.; Bavestrello Piccini, G.; Longhitano, Y.; Zanza, C.; Piccioni, A.; Esposito, C.; Ricevuti, G.; Bressan, M.A. Emergency Department Overcrowding: Understanding the Factors to Find Corresponding Solutions. J. Pers. Med. 2022, 12, 279. [Google Scholar] [CrossRef] [PubMed]
- Kotecha, D. Magnesium for Atrial Fibrillation, Myth or Magic? Circ. Arrhythmia Electrophysiol. 2016, 9, e004521. [Google Scholar] [CrossRef] [PubMed]
| p-Value | 14 Non-Cardioverted pts (14.4%) | 83 Cardioverted pts (85.6%) | Variables | MgSO4 Infusion (46 pts) | No MgSO4 Infusion (51 pts) | p-Value |
|---|---|---|---|---|---|---|
| - | - | - | Cardioverted pts | 42 (91.3%) | 41 (80.4%) | p = 0.98 |
| - | - | 27 (32.5%) | Cardioverted before Flecainide infusion | 18 (39.1%) | 9 (17.6%) | p= 0.018 |
| p = 0.43 | 9 (64.3%) | 44 (53%) | Gender (Male) | 29 (63%) | 24 (47.1%) | p > 0.05 |
| p = 0.59 | 64.7 (±12.1) | 66.5 (±10.9) | Age | 64.4 (±11.9) | 67.9 (±10.1) | p = 0.99 |
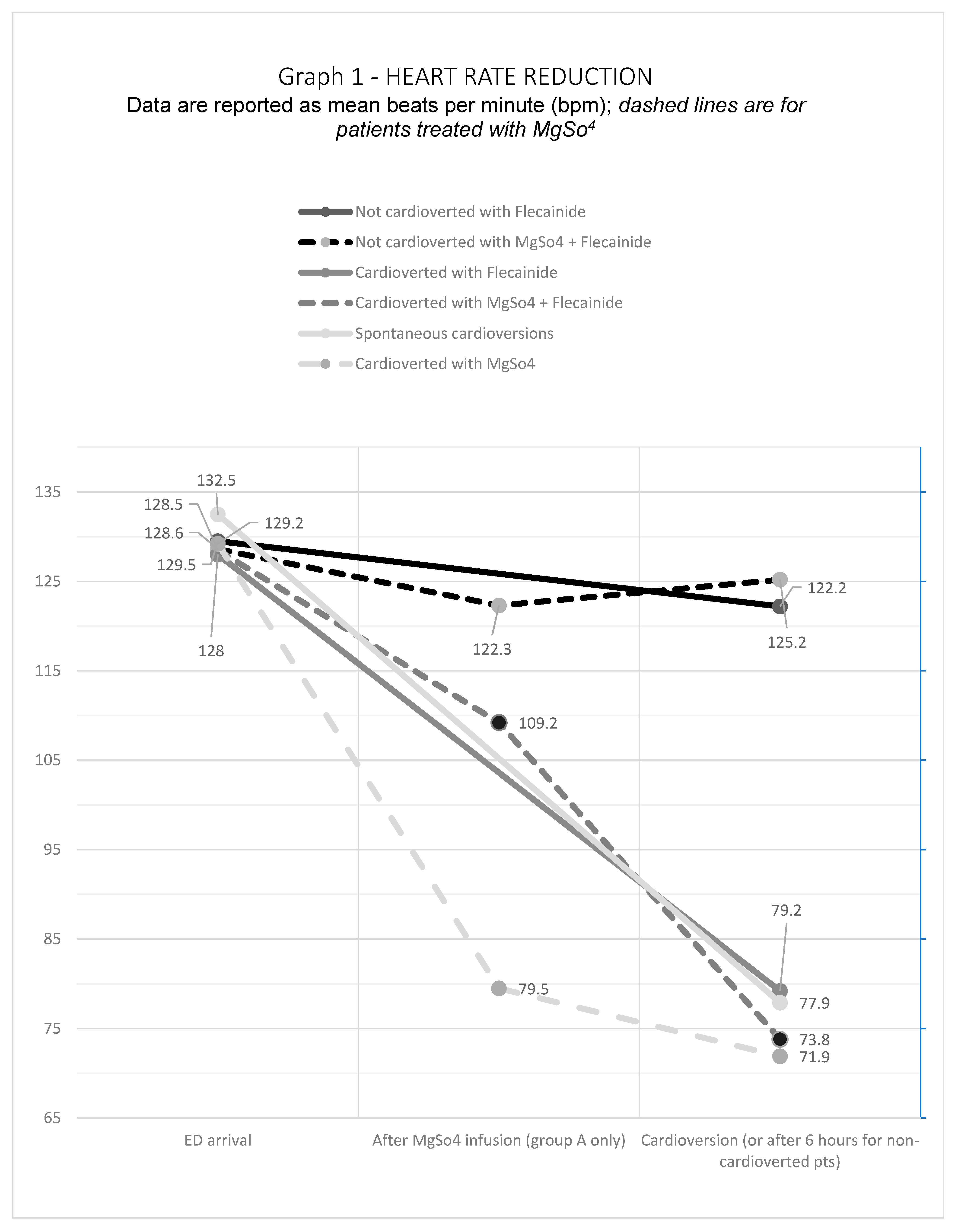
| p = 0.51 | 127.6 (±18.6) | 121.9 (±23.9) | HR at arrival (bpm) | 128.5 (±23.8) | 129.1 (±23.2) | p = 0.99 |
| p < 0.01 | 123.1 (±13.8) after 6 h | 75.7 (±12.2) | HR at cardioversion (bpm) | 77.8 (±19.1) | 87 (±21.7) | p= 0.026 |
| p = 0.37 | 2.1 (±0.2) | 2.1 (±0.1) | Mg pre-Mg (mmol/L) | 2.1 (±0.2) | 2.1 (±0.1) | p = 0.87 |
| - | - | 2.8 (±0.3) | Mg post-Mg (mmol/L) | 2.8 (±0.4) | - | |
| p = 0.32 | 4 (±0.4) | 3.9 (±0.4) | K pre-Mg (mmol/L) | 3.9 (±0.4) | 3.9 (±0.4) | p = 0.93 |
| - | - | 4 (±0.5) | K post-Mg (mmol/L) | 4 (±0.5) | - | |
| p < 0.01 | 2573.6 (±2972.4) | 626.6 (±714.4) | NT-proBNP on arrival (pg/mL) | 971 (±1559.7) | 665 (±644) | p = 0.98 |
| p = 0.95 | 5 (35.7%) | 29 (34.9%) | First AF episode | 20 (43.4%) | 14 (27.4%) | p = 0.09 |
| p = 0.65 | 5 (35.7%) | 37 (44.6%) | Paroxysmal AF | 19 (41.3%) | 23 (45.1%) | p = 0.89 |
| p = 0.68 | 1 (7.1%) | 12 (14.5%) | Diuretics drugs | 6 (13%) | 7 (13.7%) | p = 0.92 |
| p = 1 | 0 | 2 (2.4%) | K-sparing diuretics | 2 (4.3%) | 0 | p = 0.22 |
| p = 0.751 | 3 (21.4%) | 25 (30.1%) | Beta Blockers | 16 (34.7%) | 12 (23.5%) | p = 0.22 |
| p = 0.59 | 2 (14.3%) | 8 (9.6%) | Calcium channel blockers | 2 (4.4%) | 8 (15.6%) | p = 0.09 |
| p = 0.83 | 3 (21.4%) | 20 (24.1%) | Flecainide | 8 (17.4%) | 15 (29.4%) | p = 0.16 |
| p = 1 | 0 | 3 (3.6%) | Propafenone | 2 (4.3%) | 1 (1.9%) | p = 0.49 |
| - | 0 | 0 | Digoxin | 0 | 0 | - |
| p = 1 | 0 | 1 (1.2%) | Amiodarone | 1 (2.1%) | 0 | p = 0.47 |
| p = 0.63 | 2 (14.3%) | 8 (9.6%) | PPI | 7 (15.2%) | 3 (5.8%) | p = 0.13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gilardi, E.; Pomero, F.; Ravera, E.; Piccioni, A.; Santoro, M.C.; Bonadia, N.; Carnicelli, A.; Di Maurizio, L.; Sabia, L.; Longhitano, Y.; et al. Intravenous Magnesium Sulfate Reduces the Need for Antiarrhythmics during Acute-Onset Atrial Fibrillation in Emergency and Critical Care. J. Clin. Med. 2022, 11, 5527. https://doi.org/10.3390/jcm11195527
Gilardi E, Pomero F, Ravera E, Piccioni A, Santoro MC, Bonadia N, Carnicelli A, Di Maurizio L, Sabia L, Longhitano Y, et al. Intravenous Magnesium Sulfate Reduces the Need for Antiarrhythmics during Acute-Onset Atrial Fibrillation in Emergency and Critical Care. Journal of Clinical Medicine. 2022; 11(19):5527. https://doi.org/10.3390/jcm11195527
Chicago/Turabian StyleGilardi, Emanuele, Fulvio Pomero, Enrico Ravera, Andrea Piccioni, Michele Cosimo Santoro, Nicola Bonadia, Annamaria Carnicelli, Luca Di Maurizio, Luca Sabia, Yaroslava Longhitano, and et al. 2022. "Intravenous Magnesium Sulfate Reduces the Need for Antiarrhythmics during Acute-Onset Atrial Fibrillation in Emergency and Critical Care" Journal of Clinical Medicine 11, no. 19: 5527. https://doi.org/10.3390/jcm11195527
APA StyleGilardi, E., Pomero, F., Ravera, E., Piccioni, A., Santoro, M. C., Bonadia, N., Carnicelli, A., Di Maurizio, L., Sabia, L., Longhitano, Y., Saviano, A., Ojetti, V., Savioli, G., Zanza, C., & Franceschi, F. (2022). Intravenous Magnesium Sulfate Reduces the Need for Antiarrhythmics during Acute-Onset Atrial Fibrillation in Emergency and Critical Care. Journal of Clinical Medicine, 11(19), 5527. https://doi.org/10.3390/jcm11195527










