Factors Associated with Increased Analgesic Use in German Women with Endometriosis during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
3.1. Demographic Characteristics
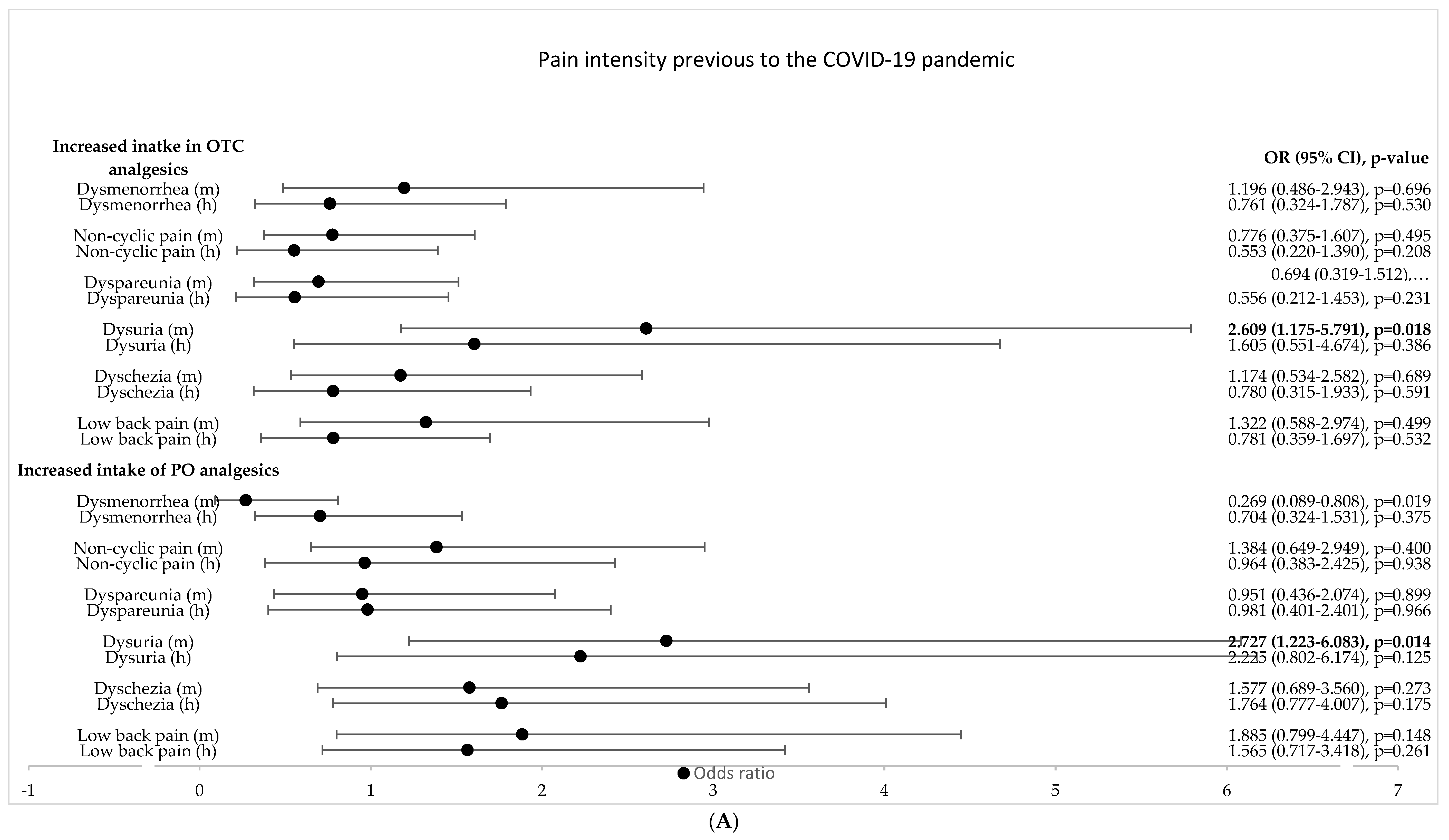
3.2. Identification of Possible Predictors of Increased Intake of OTC and PO Analgesics in Women with Endometriosis
3.3. Identification of Independent Predictors of Increased Intake of Analgesics by Women with Endometriosis
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zondervan, K.T.; Becker, C.M.; Missmer, S.A. Endometriosis. N. Engl. J. Med. 2020, 382, 1244–1256. [Google Scholar] [CrossRef] [PubMed]
- Dückelmann, A.M.; Taube, E.; Abesadze, E.; Chiantera, V.; Sehouli, J.; Mechsner, S. When and how should peritoneal endometriosis be operated on in order to improve fertility rates and symptoms? The experience and outcomes of nearly 100 cases. Arch. Gynecol. Obstet. 2021, 304, 143–155. [Google Scholar] [CrossRef]
- The Practice Committee of the American Society for Reproductive Medicine. Treatment of pelvic pain associated with endometriosis. Fertil. Steril. 2008, 90, 260–269. [Google Scholar] [CrossRef] [PubMed]
- Schwab, R.; Stewen, K.; Kottmann, T.; Theis, S.; Elger, T.; Hamoud, B.H.; Schmidt, M.W.; Anic, K.; Brenner, W.; Hasenburg, A. Determinants of Pain-Induced Disability in German Women with Endometriosis during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 8277. [Google Scholar] [CrossRef] [PubMed]
- Schwab, R.; Anić, K.; Stewen, K.; Schmidt, M.W.; Kalb, S.R.; Kottmann, T.; Brenner, W.; Domidian, J.S.; Krajnak, S.; Battista, M.J.; et al. Pain experience and social support of endometriosis patients during the COVID-19 pandemic in Germany—Results of a web-based cross-sectional survey. PLoS ONE 2021, 16, e0256433. [Google Scholar] [CrossRef] [PubMed]
- Brunes, M.; Altman, D.; Pålsson, M.; Söderberg, M.; Ek, M. Impact of hysterectomy on analgesic, psychoactive and neuroactive drug use in women with endometriosis: Nationwide cohort study. BJOG 2021, 128, 846–855. [Google Scholar] [CrossRef] [PubMed]
- Weaver, J.; Chakladar, S.; Mirchandani, K.; Liu, Z. Surgical and Pharmacological Treatment Patterns in Women with Endometriosis: A Descriptive Analysis of Insurance Claims. J. Women’s Health 2022, 31, 1003–1011. [Google Scholar] [CrossRef] [PubMed]
- Mechsner, S. Endometriosis, an Ongoing Pain—Step-by-Step Treatment. J. Clin. Med. 2022, 11, 467. [Google Scholar] [CrossRef]
- Warzecha, D.; Szymusik, I.; Wielgos, M.; Pietrzak, B. The Impact of Endometriosis on the Quality of Life and the Incidence of Depression—A Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 3641. [Google Scholar] [CrossRef]
- Norman, M.; Razmpour, O.; Olsen, J.M. Women’ s Use of Self-Care Interventions for Endometriosis Pain in the United States. Nurs. Women’s Health 2021, 25, 346–356. [Google Scholar] [CrossRef]
- Breivik, H.; Collett, B.; Ventafridda, V.; Cohen, R.; Gallacher, D. Survey of Chronic Pain in Europe: Prevalence, impact on daily life, and treatment. Eur. J. Pain 2006, 10, 287–333. [Google Scholar] [CrossRef] [PubMed]
- Treede, R.-D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11) Rolf-Detlef. Pain 2018, 160, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Perrot, S.; Citteé, J.; Louis, P.; Quentin, B.; Robert, C.; Milon, J.Y.; Bismut, H.; Baumelou, A. Self-medication in pain management: The state of the art of pharmacists’ role for optimal Over-The-Counter analgesic use. Eur. J. Pain 2019, 23, 1747–1762. [Google Scholar] [CrossRef] [PubMed]
- WHO. The Role of the Pharmacist in Self-Care and Self-Medication: Report of the 4th WHO Consultative Group on the Role of the Pharmacist, The Hague, The Netherlands, 26–28 August 1998; WHO: Geneva, Switzerland, 1998. [Google Scholar]
- Brummett, C.; Waljee, J.; Goesling, J.; Moser, S.; Lin, P.; Englesbe, M.; Bohnert, A.; Kheterpal, S.; Nallamothu, B. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg. 2017, 152, e170504. [Google Scholar] [CrossRef] [PubMed]
- Kapadi, R.; Elander, J. Pain coping, pain acceptance and analgesic use as predictors of health-related quality of life among women with primary dysmenorrhea. Eur. J. Obstet. Gynecol. 2020, 246, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Müller, O.; Neuhann, F.; Razum, O. Epidemiology and control of COVID-19. Dtsch. Med. Wochenschr. 2020, 145, 670–674. [Google Scholar] [PubMed]
- Bundesministerium für Gesundheit. Chronik Coronavirus. 2022. Available online: https://www.bundesgesundheitsministerium.de/coronavirus/chronik-coronavirus.html (accessed on 1 August 2022).
- Schwab, R.; Droste, A.; Stewen, K.; Brenner, W.; Schmidt, M.; Hasenburg, A. Patients’ expectations of preventive measures of medical institutions during the SARS-CoV-2 pandemic in Germany in women with an increased risk of breast and ovarian cancer: A cross-sectional, web-based survey. BMJ Open 2022, 12, e060038. [Google Scholar] [CrossRef]
- Leonardi, M.; Horne, A.W.; Vincent, K.; Sinclair, J.; Sherman, K.A.; Ciccia, D.; Condous, G.; Johnson, N.P.; Armour, M. Self-management strategies to consider to combat endometriosis symptoms during the COVID-19 pandemic. Hum. Reprod. Open 2020, 2020, hoaa028. [Google Scholar] [CrossRef] [PubMed]
- Bourdel, N.; Alves, J.; Pickering, G.; Ramilo, I.; Roman, H.; Canis, M. Systematic review of endometriosis pain assessment: How to choose a scale? Hum. Reprod. Update 2015, 21, 136–152. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63, S240–S252. [Google Scholar] [CrossRef]
- Tait, R.C.; Chibnall, J.T.; Krause, S. The Pain Disability Index: Psychometric properties. Pain 1990, 40, 171–182. [Google Scholar] [CrossRef]
- Löwe, B.; Wahl, I.; Rose, M.; Spitzer, C.; Glaesmer, H.; Wingenfeld, K.; Schneider, A.; Brähler, E. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2010, 122, 86–95. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The Brief Resilience Scale: Assessing the Ability to Bounce Back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Bursac, Z.; Gauss, C.H.; Williams, D.K.; Hosmer, D.W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 2008, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Bursac, Z.; Gauss, C.; Williams, D.K.; Hosmer, D. A purposeful selection of variables macro for logistic regression. SAS Glob. Forum Proc. 2007, 173, 1–5. [Google Scholar]
- Jerez-Roig, J.; Medeiros, L.F.B.; Silva, V.A.; Bezerra, C.L.P.A.M.; Cavalcante, L.A.R.; Piuvezam, G.; Souza, D. Prevalence of Self-Medication and Associated Factors in an Elderly Population: A Systematic Review. Drugs Aging 2014, 31, 883–896. [Google Scholar] [CrossRef] [PubMed]
- De Boer, M.J.; Struys, M.; Versteegen, G.J. Pain-related catastrophizing in pain patients and people with pain in the general population. Eur. J. Pain 2012, 16, 1044–1052. [Google Scholar] [CrossRef]
- Fourquet, J.; Gao, X.; Zavala, D.; Orengo, J.C.; Abac, S.; Ruiz, A.; Flores, I.; Rico, P.; Program, P.H.; Rico, P.; et al. Patients’ report on how endometriosis affects health, work, and daily life. Fertil. Steril. 2010, 93, 2424–2428. [Google Scholar] [CrossRef] [PubMed]
- Carrasco-Garrido, P.; De Andrés, A.L.; Barrera, V.H.; Jiménez-Trujillo, I.; Fernandez-de-las-peñas, C.; Palacios-Ceña, D.; García-Gómez-Heras, S.; Jiménez-García, R. Predictive factors of self-medicated analgesic use in Spanish adults: A cross-sectional national study. BMC Pharm. Toxicol. 2014, 15, 36. [Google Scholar] [CrossRef] [PubMed]
- Puntillo, F.; Giglio, M.; Brienza, N.; Viswanath, O.; Urits, I.; Kaye, A.; Pergolizzi, J.; Paladini, A.; Varrassi, G. Impact of COVID-19 pandemic on chronic pain management: Looking for the best way to deliver care. Best Pract. Res. Clin. Anaesthesiol. 2020, 34, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Ali, O.M.; Debono, V.B.; Anthonypillai, J.; Hapidou, E.G. A Qualitative Study of the Impact of the COVID-19 Pandemic on a Sample of Patients with Chronic Pain. J. Patient Exp. 2022, 9, 23743735221089696. [Google Scholar] [CrossRef]
- Franklin, G.M.; Rahman, E.A.; Turner, J.A.; Daniell, W.E.; Fulton-Kehoe, D. Opioid use for chronic low back pain: A prospective, population-based study among injured workers in Washington state, 2002–2005. Clin. J. Pain 2009, 25, 743–751. [Google Scholar] [CrossRef] [PubMed]
- Rauschert, C.; Seitz, N.; Olderbak, S.; Pogarell, O.; Dreischulte, T.; Kraus, L. Abuse of Non-opioid Analgesics in Germany: Prevalence and Associations Among Self-Medicated Users. Front. Psychiatry 2022, 13, 864389. [Google Scholar] [CrossRef] [PubMed]
- Banks, S.M.; Kerns, R.D. Explaining high rates of depression in chronic pain: A diathesis-stress framework. Psychol. Bull. 1996, 119, 95. [Google Scholar] [CrossRef]
- Jobski, K.; Luque Ramos, A.; Albrecht, K.; Hoffmann, F. Pain, depressive symptoms and medication in German patients with rheumatoid arthritis—Results from the linking patient-reported outcomes with claims data for health services research in rheumatology (PROCLAIR) study. Pharmacoepidemiol. Drug Saf. 2017, 26, 766–774. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental Health and the COVID-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef]
- Schwab, R.; Stewen, K.; Ost, L.; Kottmann, T.; Theis, S.; Elger, T.; Schmidt, M.W.; Anic, K.; Kalb, S.R.; Brenner, W.; et al. Predictors of Psychological Distress in Women with Endometriosis during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 4927. [Google Scholar] [CrossRef]
- Danilov, A.; Danilov, A.; Barulin, A.; Kurushina, O.; Latysheva, N. Interdisciplinary approach to chronic pain management. Postgrad. Med. 2020, 123, 5–9. [Google Scholar] [CrossRef]
- Thornton, L.; Batterham, P.J.; Fassnacht, D.B.; Kay-Lambkin, F.; Calear, A.L.; Hunt, S. Recruiting for health, medical or psychosocial research using Facebook: Systematic review. Internet Interv. 2016, 4, 72–81. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Löwe, B. An Ultra-Brief Screening Scale for Anxiety and Depression: The PHQ–4. J. Psychosom. Res. 2009, 50, 613–621. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The patient health questionnaire-2: Validity of a two-item depression screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Monahan, P.O.; Löwe, B. Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef] [PubMed]




| Increased Intake in OTC Analgesics | Increased Intake in PO Analgesics | ||
|---|---|---|---|
| p-Value | OR (95% CI) | p-Value | OR (95% CI) |
| Duration of reduction in social network ≥15 days (co: <15 days) | |||
| 0.814 | 1.143 (0.376–3.472) | 0.801 | 1.154 (0.380–3.506) |
| n.a. | n.a. | 0.904 | 1.142 (0.134–9.722) |
| Large reduction in social network (co: not at all to moderate reduction in social network) | |||
| 0.490 | 1.308 (0.611–2.799) | 0.033 | 2.681 (1.084–6.633) |
| Perceived reduction in social support during pain experience (co: no reduction in social support) | |||
| 0.185 | 1.550 (0.810–2.966) | 0.010 | 2.375 (1.234–4.571), |
| Pain Characteristics | Dysmenorrhea (cv) | Non-Cyclic Pain (cv) | Dyspareunia (cv) | Dysuria(cv) | Dyschezia (cv) | Low Back Pain (cv) | |
|---|---|---|---|---|---|---|---|
| Global PDI | Correlation coefficient | 0.467 | 0.469 | 0.344 | 0.404 | 0.470 | 0.443 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwab, R.; Stewen, K.; Kottmann, T.; Schmidt, M.W.; Anic, K.; Theis, S.; Hamoud, B.H.; Elger, T.; Brenner, W.; Hasenburg, A. Factors Associated with Increased Analgesic Use in German Women with Endometriosis during the COVID-19 Pandemic. J. Clin. Med. 2022, 11, 5520. https://doi.org/10.3390/jcm11195520
Schwab R, Stewen K, Kottmann T, Schmidt MW, Anic K, Theis S, Hamoud BH, Elger T, Brenner W, Hasenburg A. Factors Associated with Increased Analgesic Use in German Women with Endometriosis during the COVID-19 Pandemic. Journal of Clinical Medicine. 2022; 11(19):5520. https://doi.org/10.3390/jcm11195520
Chicago/Turabian StyleSchwab, Roxana, Kathrin Stewen, Tanja Kottmann, Mona W. Schmidt, Katharina Anic, Susanne Theis, Bashar Haj Hamoud, Tania Elger, Walburgis Brenner, and Annette Hasenburg. 2022. "Factors Associated with Increased Analgesic Use in German Women with Endometriosis during the COVID-19 Pandemic" Journal of Clinical Medicine 11, no. 19: 5520. https://doi.org/10.3390/jcm11195520
APA StyleSchwab, R., Stewen, K., Kottmann, T., Schmidt, M. W., Anic, K., Theis, S., Hamoud, B. H., Elger, T., Brenner, W., & Hasenburg, A. (2022). Factors Associated with Increased Analgesic Use in German Women with Endometriosis during the COVID-19 Pandemic. Journal of Clinical Medicine, 11(19), 5520. https://doi.org/10.3390/jcm11195520






