Insights on the Hydrodynamics of Chiari Malformation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
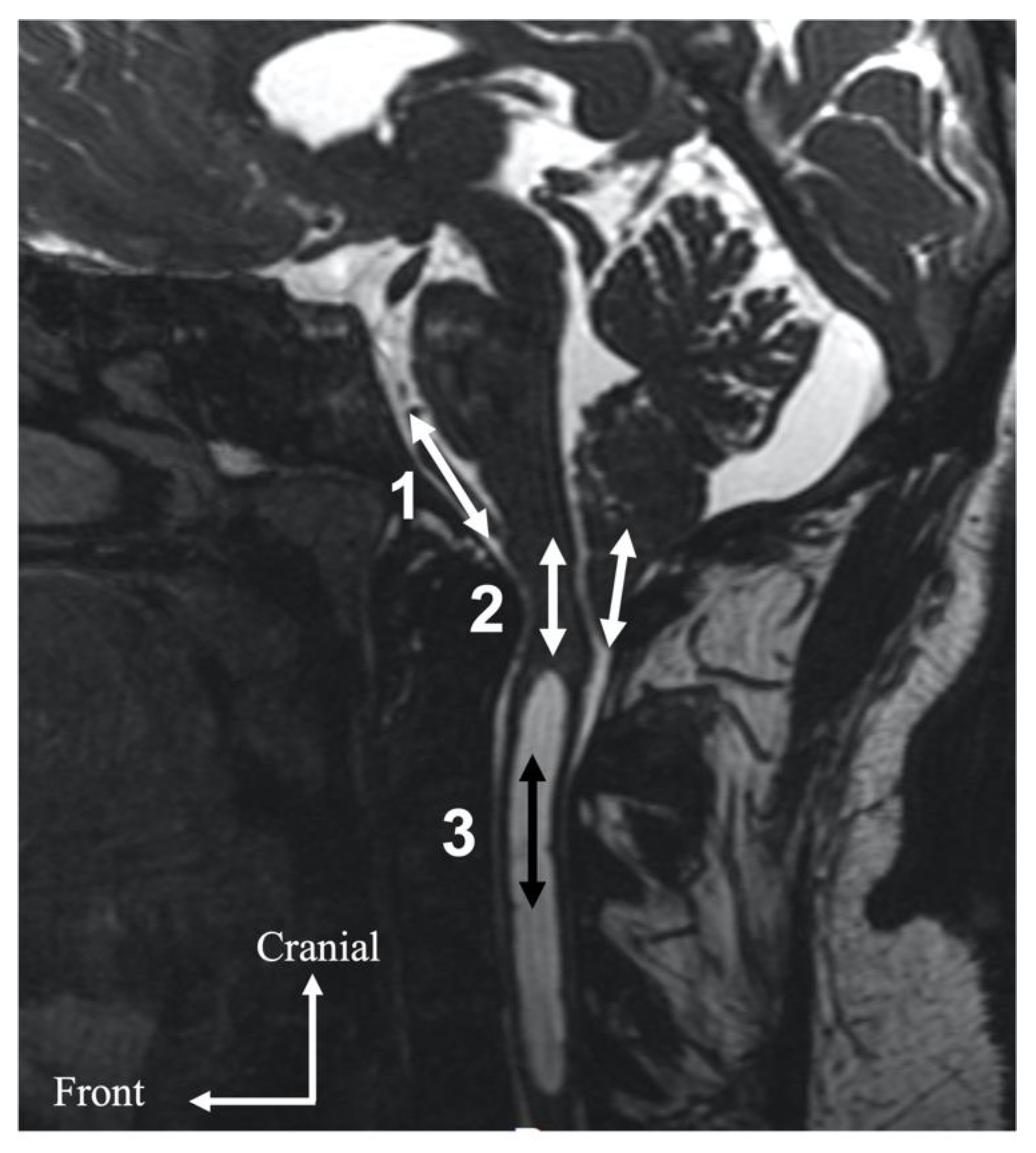
2.2. MRI Acquisition
2.3. Data Analysis
3. Results
3.1. Clinical Effectiveness of Surgery
3.2. Hemodynamics and Hydrodynamics in the Preoperative Period and Evolution after Surgery
4. Discussion
4.1. Preoperative Hemodynamics and Hydrodynamics
4.2. Evolution of Hemodynamic and Hydrodynamic Parameters after Surgery
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barkovich, A.J.; Wippold, F.J.; Sherman, J.L.; Citrin, C.M. Significance of Cerebellar Tonsillar Position on MR. AJNR Am. J. Neuroradiol. 1986, 7, 795–799. [Google Scholar] [PubMed]
- Aboulezz, A.O.; Sartor, K.; Geyer, C.A.; Gado, M.H. Position of Cerebellar Tonsils in the Normal Population and in Patients with Chiari Malformation: A Quantitative Approach with MR Imaging. J. Comput. Assist. Tomogr. 1985, 9, 1033–1036. [Google Scholar] [CrossRef] [PubMed]
- Meadows, J.; Kraut, M.; Guarnieri, M.; Haroun, R.I.; Carson, B.S. Asymptomatic Chiari Type I Malformations Identified on Magnetic Resonance Imaging. J. Neurosurg. 2000, 92, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Ciaramitaro, P.; Garbossa, D.; Peretta, P.; Piatelli, G.; Massimi, L.; Valentini, L.; Migliaretti, G.; Baldovino, S.; Roccatello, D.; Kodra, Y.; et al. Syringomyelia and Chiari Syndrome Registry: Advances in Epidemiology, Clinical Phenotypes and Natural History Based on a North Western Italy Cohort. Ann. Ist. Super. Sanita 2020, 56, 48–58. [Google Scholar] [CrossRef]
- Milhorat, T.H.; Chou, M.W.; Trinidad, E.M.; Kula, R.W.; Mandell, M.; Wolpert, C.; Speer, M.C. Chiari I Malformation Redefined: Clinical and Radiographic Findings for 364 Symptomatic Patients. Neurosurgery 1999, 44, 1005–1017. [Google Scholar] [CrossRef]
- Aiken, A.H.; Hoots, J.A.; Saindane, A.M.; Hudgins, P.A. Incidence of Cerebellar Tonsillar Ectopia in Idiopathic Intracranial Hypertension: A Mimic of the Chiari I Malformation. AJNR Am. J. Neuroradiol. 2012, 33, 1901–1906. [Google Scholar] [CrossRef]
- Lin, W.; Duan, G.; Xie, J.; Shao, J.; Wang, Z.; Jiao, B. Comparison of Results Between Posterior Fossa Decompression with and without Duraplasty for the Surgical Treatment of Chiari Malformation Type I: A Systematic Review and Meta-Analysis. World Neurosurg. 2018, 110, 460–474.e5. [Google Scholar] [CrossRef]
- Klekamp, J. Surgical Treatment of Chiari I Malformation-Analysis of Intraoperative Findings, Complications and Outcome for 371 Foramen Magnum Decompressions. Neurosurgery 2012, 71, 365–380. [Google Scholar] [CrossRef]
- Ciaramitaro, P.; Massimi, L.; Bertuccio, A.; Solari, A.; Farinotti, M.; Peretta, P.; Saletti, V.; Chiapparini, L.; Barbanera, A.; Garbossa, D.; et al. Diagnosis and Treatment of Chiari Malformation and Syringomyelia in Adults: International Consensus Document. Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 2022, 43, 1327–1342. [Google Scholar] [CrossRef]
- Quigley, M.F.; Iskandar, B.; Quigley, M.E.; Nicosia, M.; Haughton, V. Cerebrospinal Fluid Flow in Foramen Magnum: Temporal and Spatial Patterns at MR Imaging in Volunteers and in Patients with Chiari I Malformation. Radiology 2004, 232, 229–236. [Google Scholar] [CrossRef]
- Haughton, V.M.; Korosec, F.R.; Medow, J.E.; Dolar, M.T.; Iskandar, B.J. Peak Systolic and Diastolic CSF Velocity in the Foramen Magnum in Adult Patients with Chiari I Malformations and in Normal Control Participants. AJNR Am. J. Neuroradiol. 2003, 24, 169–176. [Google Scholar]
- Sakas, D.E.; Korfias, S.I.; Wayte, S.C.; Beale, D.J.; Papapetrou, K.P.; Stranjalis, G.S.; Whittaker, K.W.; Whitwell, H.L. Chiari Malformation: CSF Flow Dynamics in the Craniocervical Junction and Syrinx. Acta Neurochir. 2005, 147, 1223–1233. [Google Scholar] [CrossRef]
- Shaffer, N.; Martin, B.; Loth, F. Cerebrospinal Fluid Hydrodynamics in Type I Chiari Malformation. Neurol. Res. 2011, 33, 247–260. [Google Scholar] [CrossRef]
- Alperin, N.; Loftus, J.R.; Oliu, C.J.; Bagci, A.M.; Lee, S.H.; Ertl-Wagner, B.; Green, B.; Sekula, R. Magnetic Resonance Imaging Measures of Posterior Cranial Fossa Morphology and Cerebrospinal Fluid Physiology in Chiari Malformation Type I. Neurosurgery 2014, 75, 515–522. [Google Scholar] [CrossRef]
- Radmanesh, A.; Greenberg, J.K.; Chatterjee, A.; Smyth, M.D.; Limbrick, D.D.; Sharma, A. Tonsillar Pulsatility before and after Surgical Decompression for Children with Chiari Malformation Type 1: An Application for True Fast Imaging with Steady State Precession. Neuroradiology 2015, 57, 387–393. [Google Scholar] [CrossRef]
- Frič, R.; Lindstrøm, E.K.; Ringstad, G.A.; Mardal, K.-A.; Eide, P.K. The Association between the Pulse Pressure Gradient at the Cranio-Cervical Junction Derived from Phase-Contrast Magnetic Resonance Imaging and Invasively Measured Pulsatile Intracranial Pressure in Symptomatic Patients with Chiari Malformation Type 1. Acta Neurochir. 2016, 158, 2295–2304. [Google Scholar] [CrossRef]
- Cushing, H. Studies in Intracranial Physiology & Surgery: The Third Circulation, the Hypophysics, the Gliomas; Milford, H., Ed.; Oxford University Press: Oxford, UK, 1926. [Google Scholar]
- Wilson, M.H. Monro-Kellie 2.0: The Dynamic Vascular and Venous Pathophysiological Components of Intracranial Pressure. J. Cereb. Blood Flow Metab. Off. J. Int. Soc. Cereb. Blood Flow Metab. 2016, 36, 1338–1350. [Google Scholar] [CrossRef]
- Leung, V.; Magnussen, J.S.; Stoodley, M.A.; Bilston, L.E. Cerebellar and Hindbrain Motion in Chiari Malformation with and without Syringomyelia. J. Neurosurg. Spine 2016, 24, 546–555. [Google Scholar] [CrossRef]
- Bapuraj, J.R.; Londy, F.J.; Delavari, N.; Maher, C.O.; Garton, H.J.L.; Martin, B.A.; Muraszko, K.M.; Ibrahim, E.-S.H.; Quint, D.J. Cerebrospinal Fluid Velocity Amplitudes within the Cerebral Aqueduct in Healthy Children and Patients with Chiari I Malformation. J. Magn. Reson. Imaging JMRI 2016, 44, 463–470. [Google Scholar] [CrossRef]
- McGirt, M.J.; Nimjee, S.M.; Fuchs, H.E.; George, T.M. Relationship of Cine Phase-Contrast Magnetic Resonance Imaging with Outcome after Decompression for Chiari I Malformations. Neurosurgery 2006, 59, 140–146. [Google Scholar] [CrossRef]
- Dolar, M.T.; Haughton, V.M.; Iskandar, B.J.; Quigley, M. Effect of Craniocervical Decompression on Peak CSF Velocities in Symptomatic Patients with Chiari I Malformation. AJNR Am. J. Neuroradiol. 2004, 25, 142–145. [Google Scholar] [PubMed]
- Enzmann, D.R.; Pelc, N.J. Cerebrospinal Fluid Flow Measured by Phase-Contrast Cine MR. AJNR Am. J. Neuroradiol. 1993, 14, 1301–1307. [Google Scholar] [PubMed]
- Balédent, O.; Henry-Feugeas, M.C.; Idy-Peretti, I. Cerebrospinal Fluid Dynamics and Relation with Blood Flow: A Magnetic Resonance Study with Semiautomated Cerebrospinal Fluid Segmentation. Investig. Radiol. 2001, 36, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Greitz, D.; Wirestam, R.; Franck, A.; Nordell, B.; Thomsen, C.; Ståhlberg, F. Pulsatile Brain Movement and Associated Hydrodynamics Studied by Magnetic Resonance Phase Imaging. The Monro-Kellie Doctrine Revisited. Neuroradiology 1992, 34, 370–380. [Google Scholar] [CrossRef] [PubMed]
- Bateman, G.A. Vascular Hydraulics Associated with Idiopathic and Secondary Intracranial Hypertension. AJNR Am. J. Neuroradiol. 2002, 23, 1180–1186. [Google Scholar]
- Bradley, W.G., Jr.; Scalzo, D.; Queralt, J.; Nitz, W.N.; Atkinson, D.J.; Wong, P. Normal-Pressure Hydrocephalus: Evaluation with Cerebrospinal Fluid Flow Measurements at MR Imaging. Radiology 1996, 198, 523–529. [Google Scholar] [CrossRef]
- Capel, C.; Baroncini, M.; Gondry-Jouet, C.; Bouzerar, R.; Czosnyka, M.; Czosnyka, Z.; Balédent, O. Cerebrospinal Fluid and Cerebral Blood Flows in Idiopathic Intracranial Hypertension. Acta Neurochir. Suppl. 2018, 126, 237–241. [Google Scholar] [CrossRef]
- Alperin, N.J.; Lee, S.H.; Loth, F.; Raksin, P.B.; Lichtor, T. MR-Intracranial Pressure (ICP): A Method to Measure Intracranial Elastance and Pressure Noninvasively by Means of MR Imaging: Baboon and Human Study. Radiology 2000, 217, 877–885. [Google Scholar] [CrossRef]
- Balédent, O.; Fin, L.; Khuoy, L.; Ambarki, K.; Gauvin, A.-C.; Gondry-Jouet, C.; Meyer, M.-E. Brain Hydrodynamics Study by Phase-Contrast Magnetic Resonance Imaging and Transcranial Color Doppler. J. Magn. Reson. Imaging JMRI 2006, 24, 995–1004. [Google Scholar] [CrossRef]
- Sivaramakrishnan, A.; Alperin, N.; Surapaneni, S.; Lichtor, T. Evaluating the Effect of Decompression Surgery on Cerebrospinal Fluid Flow and Intracranial Compliance in Patients with Chiari Malformation with Magnetic Resonance Imaging Flow Studies. Neurosurgery 2004, 55, 1344–1350. [Google Scholar] [CrossRef]
- Bateman, G.A. The Pathophysiology of Idiopathic Normal Pressure Hydrocephalus: Cerebral Ischemia or Altered Venous Hemodynamics? AJNR Am. J. Neuroradiol. 2008, 29, 198–203. [Google Scholar] [CrossRef] [Green Version]

| Population | Number of Patients |
|---|---|
| Sex ratio (M/F) | 6/15 |
| Age (years) | 41 ± 16 |
| Syrinx | 12 |
| Type of surgery | |
| 9 12 |
| Preoperative | Postoperative | |
|---|---|---|
| Headaches | 14 (67%) | 3 (14%) |
| Dizziness | 5 (24%) | 2 (10%) |
| Instability | 8 (38%) | 1 (5%) |
| Vestibular syndrome | 2 (10%) | 1 (5%) |
| Nystagmus | 4 (19%) | 1 (5%) |
| Ronchopathy | 2 (10%) | 0 |
| Sleep apnea syndrome | 3 (14%) | 0 |
| Paresthesia | 6 (29%) | 2 (10%) |
| Swallowing syndrome | 3 (14%) | 1 (5%) |
| Syringomyelia | No Syringomyelia | p | |
|---|---|---|---|
| SVaqu (μL/CC) | 24 ± 17 | 43 ± 25 | 0.13 |
| SVforamen (μL/CC) | 429 ± 317 | 176 ± 122 | 0.11 |
| SVtonsils (μL/CC) | 313 ± 197 | 332 ± 112 | 0.85 |
| SVcerv (μL/CC) | 458 ± 378 | 391 ± 155 | 0.62 |
| SVvasc (μL/CC) | 1649 ± 492 | 1689 ± 369 | 0.84 |
| AMPvenous (mm3/s) | 5201 ± 2391 | 6080 ± 2661 | 0.44 |
| Correction factor | 1.49 ± 0.4 | 1.19 ± 0.1 | 0.05 |
| Preoperative | Postoperative | p | |
|---|---|---|---|
| SVaqu (μL/CC) | 39 ± 33 | 30 ± 26 | 0.36 |
| SVforamen (μL/CC) | 201 ± 124 | 363 ± 231 | 0.02 |
| SVtonsils (μL/CC) | 323 ± 175 | 194 ± 130 | 0.008 |
| SVcerv (μL/CC) | 434 ± 309 | 398 ± 241 | 0.73 |
| SVvasc (μL/CC) | 1661 ± 433 | 1490 ± 532 | 0.10 |
| AMPvenous (mm3/s) | 5578 ± 2469 | 4576 ± 2084 | 0.008 |
| Correction factor | 1.38 ± 0.3 | 1.20 ± 0.3 | 0.04 |
| SVsyrinx (μL/CC) | 118 ± 86 | 26 ± 28 | 0.03 |
| Variations in the Measurement of the Parameters Studied before and after Surgery (%) | Extradural Approach | Duraplasty | p |
|---|---|---|---|
| SVaqu | 101 ± 24 | 71 ± 35 | 0.21 |
| SVcerv | 145 ± 99 | 106 ± 46 | 0.59 |
| SVforamen | 399 ± 236 | 453 ± 330 | 0.43 |
| SVtonsils | 35 ± 59 | 48 ± 55 | 0.52 |
| SVvasc | 89 ± 22 | 95 ± 29 | 0.26 |
| AMPvenous | 105 ± 18 | 97 ± 52 | 0.78 |
| Correction factor | 86 ± 11 | 65 ± 27 | 0.36 |
| SVsyrinx | 25 ± 35 | 20 ± 30 | 0.70 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capel, C.; Padovani, P.; Launois, P.-H.; Metanbou, S.; Balédent, O.; Peltier, J. Insights on the Hydrodynamics of Chiari Malformation. J. Clin. Med. 2022, 11, 5343. https://doi.org/10.3390/jcm11185343
Capel C, Padovani P, Launois P-H, Metanbou S, Balédent O, Peltier J. Insights on the Hydrodynamics of Chiari Malformation. Journal of Clinical Medicine. 2022; 11(18):5343. https://doi.org/10.3390/jcm11185343
Chicago/Turabian StyleCapel, Cyrille, Pauline Padovani, Pierre-Henri Launois, Serge Metanbou, Olivier Balédent, and Johann Peltier. 2022. "Insights on the Hydrodynamics of Chiari Malformation" Journal of Clinical Medicine 11, no. 18: 5343. https://doi.org/10.3390/jcm11185343
APA StyleCapel, C., Padovani, P., Launois, P.-H., Metanbou, S., Balédent, O., & Peltier, J. (2022). Insights on the Hydrodynamics of Chiari Malformation. Journal of Clinical Medicine, 11(18), 5343. https://doi.org/10.3390/jcm11185343






